We were told it would take about 30 minutes to stabilize Ari and the doctors would be out shortly thereafter to tell us what exactly the issue was. I sat in the window, phone battery dead, and directed all my thoughts and energy to the window behind which I thought that my little girl was fighting for her life. Sergio tried to keep Hugo entertained, but as the afternoon wore on, Hugo became increasingly hungry, tired and stir-crazy- the trifecta of disaster as any parent knows.
Finally, after 3 hours and as Hugo neared an epic meltdown, Sergio went back into the ER, from which we had been forbidden. Two doctors followed him out and, as they saw Hugo, I heard one comment to the other “well, at least they will still have 1 child.”
My stomach dropped and my blood ran cold, and I was convinced that they were going to tell us that my precious baby had died. I felt my heart close up, and I went numb, as I followed behind the doctors, preparing myself to hear those words.
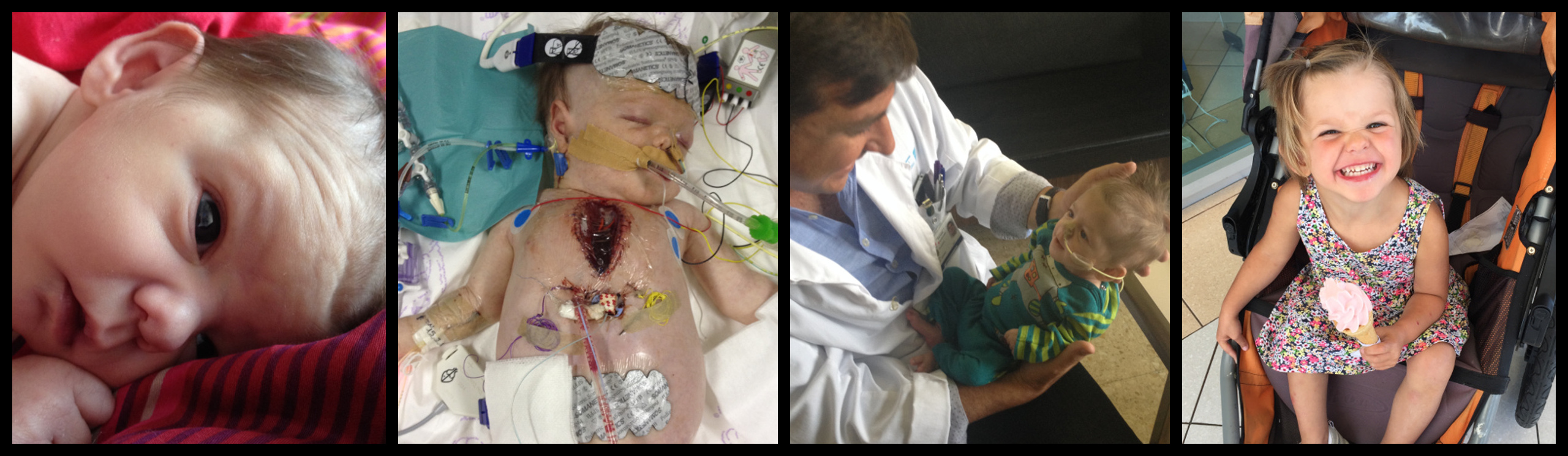
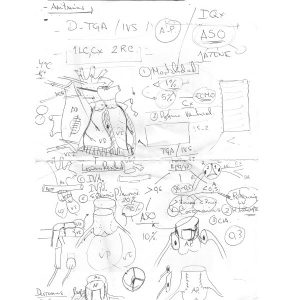
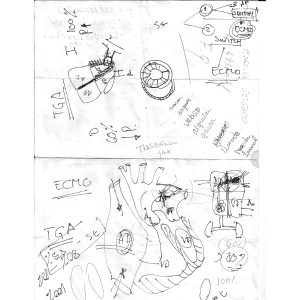
We walked to a small conference room where about 10 doctors were standing around. As we entered, one motioned for us to take a seat, as he also sat down. He immediately began drawing a picture of a heart, and explained to us that Ari had been born with a cardiopathy called “Transposition of the Great Arteries”. He said that normally O2 enters the bloodstream from the lungs, and is then carried to the heart, where the oxygen-rich blood mixes with the oxygen-depleted blood that has arrived to the heart after circulating through the rest of the body. In Ari’s case, The two main conduits, or arteries, into the heart that make that possible were flipped, or transposed. The result was that the blood was not intermingling as it should, and there were effectively 2 parallel and separate tracks in which the O2-rich blood from her lungs continued to circulate through the heart, as the O2-poor blood circulated throughout the rest of her body.
All babies are born with something called a ductus, however, and it is essentially Mother Nature’s safety mechanism to ensure that the lungs have time to function properly for the first time after a baby is born. It is effectively a hole inside the heart between 2 of the heart’s chambers that allows the blood to intermingle, creating a second way in which blood becomes oxygenated immediately after birth. In most cases, however, the ductus shrinks and ultimately closes after a few hours to a few days following birth.
Amazingly, this tiny hole kept Ari alive for nearly 6 weeks. And not only that, she had not shown any of the tell-tale signs of oxygen deprivation (blue tinge in lips and extremities, lethargy, inability to breastfeed). During the course of those 6 weeks, her ductus was shrinking, until finally it measured no more than 2 millimeters, which prompted the episode that resulted in our trip to the ER.
We would later learn that the doctor explaining all of this to us was Dr. Enrique Garcia, the man who would, in very short order, literally have our baby girl’s life in his hands.
Ch. 1: The First 6 Weeks
Ch. 2: To the ER
Ch. 3: The Transfer
Ch. 4: The Diagnosis (this page)
Ch. 5: The Rashkind Procedure
Ch. 6: 8 Weeks in PICU
Ch. 7: Ari’s Arterial Switch
Ch. 8: The End . . . and the Beginning