A RANDOMIZED CLINICAL TRIAL OF REGIONAL CEREBRAL PERFUSION VERSUS DEEP HYPOTHERMIC CIRCULATORY ARREST: FIVE-YEAR FOLLOW-UP FOR NEURODEVELOPMENTAL OUTCOMES IN CHILDREN WITH FUNCTIONAL SINGLE VENTRICLE
Author links open overlay panelMelissaSmith-ParrishSunkyungYuJanetDonohueRichardOhyeEdwardBoveMaryBestCarenGoldberg
University of Michigan Health System, Ann Arbor, MI, USA
Background
Regional cerebral perfusion (RCP) has been endorsed as a method to improve cerebral protection during neonatal aortic arch reconstruction. However, no human study has demonstrated improvement in developmental outcomes with RCP. We aimed to: 1. Compare early school-age (ESA) neurodevelopmental outcomes among children with single ventriclewho underwent the Norwood operation with RCP rather than deep hypothermic circulatory arrest (DHCA), 2. Determine the predictive value of early developmental testing, and 3. Identify additional contributors to ESA development.
Methods
Children enrolled in the RCP randomized controlled trial of infants with single ventricleundergoing the Norwood operation with randomization to aortic arch reconstruction with either RCP or DHCA were included. A comprehensive neuropsychological evaluation was performed at ages 5-8 years with this analysis focusing on the Wechsler Intelligence Scales. Additional candidate predictors were investigated as associated with impaired neurodevelopment with chi square and t tests for categorical and continuous variables respectively.
Results
Forty-one patients returned for ESA follow-up. The overall mean full scale IQ was 93.4 ± 18.8 with a mean verbal IQ of 95.9 ± 17.6, a mean performance IQ of 94.5 ± 19.2, and a mean processing speed IQ of 92.5 ± 15.2. There were no statistical differences between the RCP and DHCA groups. The one year Bayley Scale of Infant Development Psychomotor Development Index (r = 0.68, p<0.0001) and Mental Development Index (r = 0.64, p<0.0001) correlated with the full scale IQ at ESA. Participants with lower socioeconomic status (SES) and those without fetal diagnosis had lower IQ scores. However, SES was higher for those with a fetal diagnosis.
Conclusion
Neurodevelopment is delayed after the Norwood operation without an associated improvement with RCP. Bayley Scale of Infant Development scores at 1 year predict ESA measures, though additional unmeasured factors likely explain a significant portion of ESA developmental outcomes. Fetal diagnosis and higher SES are associated with higher IQ scores, but the mechanism remains unclear as SES is higher among those with fetal diagnosis.
GESTATIONAL AGE AT BIRTH AND OUTCOME AFTER NEONATAL CARDIAC SURGERY: AN ANALYSIS OF THE SOCIETY OF THORACIC SURGEONS CONGENITAL HEART SURGERY DATABASE
Author links open overlay panelSaraPasqualiJohn M.CostelloXiaHeJeffrey P.JacobsKevinHillDavid S.CooperCarl L.BackerMarshallJacobs
Ann & Robert H. Lurie Children’s Hospital of Chicago, Chicago, IL, USA
Background
Earlier gestational age (GA) at birth has been associated with worse outcome in neonates undergoing cardiac surgery, even at 37–38 weeks. However, prior studies have relied on administrative data or examination of single center cohorts. We used clinical registry data to evaluate whether this relationship held true across a large multicenter cohort.
Methods
Neonates <28 days who underwent cardiac surgery (2010–11) in the STS Congenital Heart Surgery Database were included. Multivariable logistic regression was used to evaluate the impact of GA at birth on in-hospital mortality, adjusting for other important patient characteristics (including weight, age and comorbidities), case complexity, and center effects. Post-operative length of stay (PLOS) was also evaluated.
Results
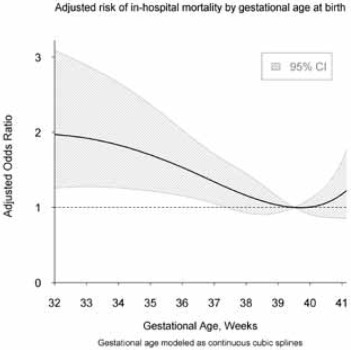
4,784 neonates (92 centers) were included. Compared with an empirically derived 39.5 week GA reference level, birth at or before 37 weeks GA, but not 38 weeks, was associated with significantly higher adjusted mortality (Figure). Adjusted odds ratios (with 95% C.I.) for mortality were 1.53 (1.15–2.03, p=0.003) at 36 weeks, 1.34 (1.05-1.71, p=0.02) at 37 weeks, and 1.16 (0.93–1.45, p=0.19) at 38 weeks. Adjusted PLOS was significantly prolonged for those born at 38 weeks and earlier (all p<0.01).
Conclusions
Optimal outcomes following neonatal cardiac surgery are achieved with birth at 39-40 weeks GA. These data are useful for planning timing of delivery, for counseling, and for risk adjustment in outcomes analyses.
OUTCOMES FOLLOWING PROLONGED EXTRA CORPOREAL MEMBRANE OXYGENATION SUPPORT IN CHILDREN WITH CARDIAC DISEASE: EXTRACORPOREAL LIFE SUPPORT ORGANIZATION REGISTRY STUDY
Author links open overlay panelLauraSchoenebergDeanMerrillPratikSandesaraBarbaraHaneyEricaMolitor-KirschJames O’BrienJrHongyingDaiGeethaRaghuveer
Children’s Mercy Hospital, Kansas City, MO, USA
University of Missouri – Kansas City School of Medicine, Kansas City, MO, USA
Optimal timing for discontinuation of Extra Corporeal Membrane Oxygenation (ECMO) in children with cardiac insufficiency unable to wean from ECMO is ill defined.
Outcomes following prolonged ECMO support (≥14 days) for cardiac insufficiency in children <18 years of age were examined.
We reviewed the International Extracorporeal Life Support Organization data from 1/1/2000-12/31/2011.
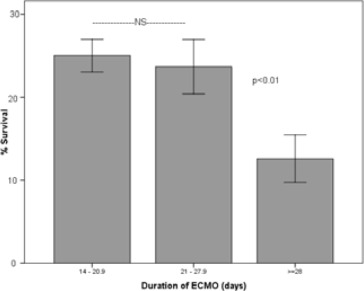
784 prolonged ECMO runs were identified, 177 (23%) survived to hospital discharge, survival decreased further when ECMO lasted ≥28 days (Fig). Compared to non-survivors, survivors were older (median 233vs.39 days, p<0.01), weighed more (16±20vs.8±13 kg, p<0.01), had shorter ECMO duration (20±6vs.22±9 days, p<0.01), and fewer organ complications (median 4vs.3, p<0.01). Those with congenital heart disease had lower survival compared to cardiomyopathy and myocarditis (15%vs.42&52%, p<0.01), single ventricle lesions had worse survival compared to double ventricle (10%vs.18%, p=0.01). 11% (n=89) received cardiac transplant and had better survival than those non-transplanted (53%vs.19%, p<0.01). Pre-ECMO arrest and emergent ECMO placement were not predictors of outcome.
Though 23% survived to hospital discharge, there is a significant attrition and morbidity following prolonged ECMO support for cardiac insufficiency in children. Cardiac transplantation in this cohort is also associated with high mortality. Earlier conversion to other modes of mechanical support as a bridge to transplant is recommended.
VASOACTIVE INOTROPIC SCORE (VIS) IS ASSOCIATED WITH OUTCOME AFTER INFANT CARDIAC SURGERY: A REPORT OF THE PEDIATRIC CARDIAC CRITICAL CARE CONSORTIUM (PC4)
Author links open overlay panelMichaelGaiesHowardJeffriesRobertNieblerSaraPasqualiJanet E.DonohueSunkyungYuRaviThiagarajan
University of Michigan, Ann Arbor, MI, USA
Pediatric Cardiac Critical Care Consortium (PC4), Ann Arbor, MI, USA
Background
Few empirically-derived markers of illness severity exist for pediatric cardiac surgical patients. Vasoactive-inotropic score (VIS), a measure of post-operative cardiovascularsupport, has been associated with morbidity and mortality after infant cardiac surgery in prior single center studies. We evaluated whether this held true in a multi-institutional prospective cohort.
Methods
Consecutive infants (≤1 yr) undergoing cardiac surgery with bypass were enrolled at 4 centers. Doses of vasoactive infusions were recorded for 48 hrs after surgery, converted to integers, and summed to generate hourly VIS. The optimal definition of “high VIS” was determined empirically to be maximum VIS ≥15 in the first 24 hrs. A dichotomous primary outcome was defined a priori as a composite of: hospital or 30-day mortality, cardiac arrest, mechanical circulatory support, dialysis, or neurologic injury. Secondary outcomes included duration of mechanical ventilation and intensive care (ICU) length of stay (LOS). Multivariable logistic regression adjusting for patient factors, operative characteristics, and center effects was performed to test the association between VIS and outcome.
Results
Overall, 391 infants were enrolled including 141 (36%) neonates and 130 (33%) with high VIS. Forty-five (12%) reached the composite endpoint including 19 (5%) deaths. High VIS was independently associated with the composite endpoint [adjusted odds ratio (AOR) 4.0, 95% confidence interval (CI) 1.8-8.9]. This relationship was consistent across age groups and levels of surgical complexity in stratified analyses. High VIS was also independently associated with mortality (AOR 4.7, 95% CI 1.4-15.8) and each of the individual morbidities. Patients with high VIS had greater odds of prolonged mechanical ventilation (AOR 4.3, 95% CI 2.3-8.0) and ICU LOS (AOR 3.2, 95% CI 1.8-5.9).
Conclusions
In this multi-institutional study, VIS was independently associated with mortality and morbidity in infants undergoing cardiac surgery with bypass. We have defined a robust, generalizable metric of cardiovascular support in this population that performs well as a marker of illness severity across centers.
READMISSION WITHIN 30 DAYS OF PEDIATRIC HEART SURGERY: INCIDENCE, RISK FACTORS AND RESOURCE UTILIZATION
Author links open overlay panelSamuel PaulHankeCatherineKrawczeskiBradleyMarinoSamirShahEdmundBerryEileenKingLynnDarbieJamesCnota
Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA
Background
Hospital readmission (RA) is a measure of healthcare quality. Little is known about RA following pediatric heart surgery (PHS). The purpose of this study was to identify: 1) the rate and incurred hospital charges of RA within 30 days of discharge after PHS, 2) factors associated with RA and hospital charges.
Methods
Children 0-17 years of age who underwent PHS between January 1, 2006 and September 30, 2011 were identified by procedural codes within the Pediatric Health Information System database. RA was defined as any admission within 30 days of discharge after PHS. Patients were classified as having 0, 1, or > 1 RA. Charges and RA length of stay are reported. Patient demographics and factors associated with the index PHS hospitalization were analyzed. Factors associated with RA were analyzed by ordinal logistic regression. Log RA charges were analyzed by multivariable generalized linear model.
Results
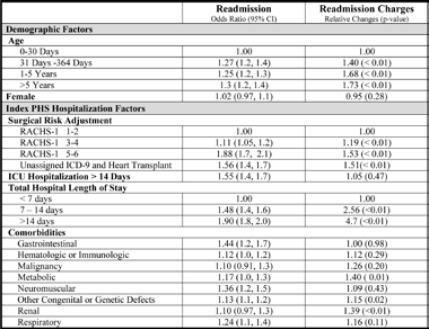
Of 53,105 patients with a PHS discharge from 42 hospitals, 10,667 (20.1%) had at least one RA. Total PHS charges were $498,539,570. Median time from discharge to first RA was 8 (IQR 4, 15) days. Median RA duration was 1 (IQR 1, 4) day. Median charges for RA were $4,272 (IQR $550, $23,887). Table 1 details factors independently associated with RA and RA charges.
VALVE REPLACEMENT WITH AN EXPANDABLE BIOPROSTHETIC VALVE IN NEONATES AND INFANTS
Author links open overlay panelSitaramEmaniFrankPigulaChristopherBairdJamesLockPedro delNido
Boston Childrens Hospital, Boston, MA, USA
Background
Prosthetic options for neonates and infants with valvular heart disease are limited to traditional fixed diameter mechanical and bioprosthetic valves, which require replacement as the child grows. We test the hypothesis that an adjustable externally stented bovine jugular vein graft can be surgically implanted and expanded subsequently in the catheterizationlaboratory as the child grows.
Methods
Externally stented bovine jugular vein graft (Melody) was modified for surgical implantation into the right ventricular outflow tract (RVOT, n=8), aortic (n=1), and mitral positions (n=6). Valves were only partially expanded at surgical implantation with the intention of sequential expansion in the catheterization laboratory with somatic growth. Patients were prospectively followed to determine short-term valve durability and response to balloon expansion.
Results
Median age at valve implantation was 8 months (range 1.6 mo to 6.6 yrs). Median internal diameter of valve at implantation was 12 mm (range 9 to 18 mm). Valvular regurgitation early postopertively was mild or less in the 13/15 patients, and moderate to severe in 2 patients due to technical reasons (excessive trimming of graft in one patient and perivalvar leak following implantation within PTFE tube graft in another). At median follow up of 1.5 years, 2 patients have undergone re-replacement, both considered to be technical failures. Catheter-based valve expansion has been performed in 7 patients (5 RVOT and 2 mitral) at a median interval of 318 days (range 16 days to 748 days) following implantation. Median balloon size at valve expansion was 12 mm (range 12 to 16 mm). Five of 7 patients with mild or less regurgitation prior to balloon expansion continued to demonstrate mild valvular regurgitation following intervention, whereas the regurgitation remained significant in the 2/7 patients with technical failures.
Conclusions
An adjustable stented bovine jugular vein graft is a novel option for neonates and infants who require surgical valve replacement. At short term follow up, valve durability is acceptable. Valve function remains acceptable following catheter-based expansion up to 1.5 years following implantation.
PREGNANCY AFTER FONTAN OPERATION: EARLY AND LATE OUTCOMES
Author links open overlay panelMary M.CanobbioFrankCettaCandiceSilversidesCaroleWarnesJamilAboulhosnJackColman
UCLA ACHD, Los Angeles, CA, USA
The Mayo Clinic, Rochester, MN, USA
Background
The Fontan procedure is the definitive operation for patients with single ventricle physiology. As more women with Fontan operations reach childbearing age, it is important to determine the impact pregnancy has on short and long-term outcomes. The purpose of this multicenter study was to determine outcomes during and after pregnancy in women following Fontan operation.
Methods
A retrospective chart review was performed at 12 North American centers of 45 women who reported a pregnancy after Fontan operation.
Results
There were 71 pregnancies which resulted in 51 (73%) live births (12 spontaneous abortions, 3 therapeutic abortions, 2 fetal demise). Of the live births, the mean gestational age was 34 (range 24-40) weeks and the median birth weight was 2169 gm (760-3572) gms. Thirty-three percent (n=17) of pregnancies were complicated by an adverse maternal cardiac event; including heart failure (n=5), arrhythmias (n=12: atrial 10, ventricular 2). There were no maternal deaths during pregnancy. One woman had a cardiac arrest during delivery, but was successfully resuscitated and discharged to home. Eleven of the adverse cardiac events occurred in the early post partum period and 1 occurring 8 month post-delivery. There was one neonatal death due to prematurity (760 gm infant). Two children were born with CHD (ASD, VSD). Obstetrical events occurred during pregnancy or delivery in 25/48 (52%) and 6 events occurred during the post-partum period. Late follow up was available for 67% (29/45) of the women. The mean follow up time after pregnancy was 7.74years (range 1-23 years). There were 5 late deaths. The mean interval from delivery to death was 12.8 years (range 3-18 years). Cause of death included thromboembolism (n=2), ventricular failure (n=2) and unknown(n=1).
Conclusions
Pregnancy in women with Fontan circulation is associated with risk for the mother and the baby. While there were no maternal deaths during pregnancy in this series, it is unclear from this data if long-term maternal mortality is affected, further prospective and controlled studies are needed to address this issue These findings should form part of preconception counseling in women post-Fontan.
TRANSPLANT-FREE SURVIVAL AND HOSPITALIZATIONS LATE AFTER THE FONTAN PALLIATION
Author links open overlay panelRobert W.ElderNancyMcCabeEmirVeledarAnuragSahuMaanJokhadarBrianKogonMichaelMcConnellWendyBook
Emory University School of Medicine, Atlanta, GA, USA
Background
The Fontan operation is standard palliation for single ventricle heart defects. Outcomes beyond 20 yrs after Fontan palliation are not well known. We describe late outcomes in a cohort of adult patients post-Fontan.
Methods
A chart review of all patients post Fontan who survived to adulthood, seen at Emory since 1998 was performed. Diagnosis, surgical history, cardiac hospitalizations (heart failure, arrhythmia, thromboembolic events, or surgical admissions), death and need for transplantwere obtained. Outcomes were plotted using Kaplan Meier and tested for difference by Fontan type and ventricular morphology.
Results
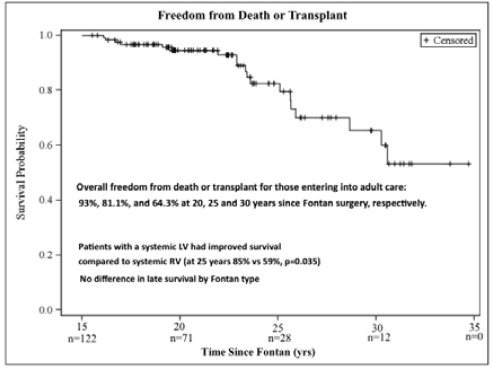
134 patients (57.5% male) were identified (mean age 28.4 yrs [18-55.2], mean time from Fontan completion 21.4 yrs [5.1-34.8]). Ventricular morphological was right (RV) n=31, left (LV) n=98, or equal ventricles n=5. 55 patients had atriopulmonary Fontan (APC), 24 of which were revised, 77 lateral tunnel, 2 extracardiac. 14 patients died, 10 required transplant. Fig. 1shows overall survival. LV patients had improved survival compared to RV (p=0.035), with no differences by Fontan type. Freedom from hospitalization was 69%, 38.6%, and 6.4% at 20, 25 and 30 yrs since Fontan, with no difference by Fontan type or ventricular morphology.
TRANSIENT ELASTOGRAPHY OF THE LIVER FOR NON-INVASIVE ASSESSMENT OF CENTRAL VENOUS PRESSURES AND HEPATIC FIBROSIS IN PATIENTS WITH FONTAN CIRCULATION
Author links open overlay panelFredWuRoshanRazaSarahHarneyChinweikeUkomaduMichaelLandzbergAnne MarieValenteRogerBreitbartMichaelSinghAlexanderOpotowskyKimberleeGauvreauMaureen M.Jonas
Boston Children’s Hospital, Boston, MA, USA
Brigham and Women’s Hospital, Boston, MA, USA
Background
Transient elastography (TE) offers a noninvasive correlate with the degree of hepatic fibrosisusing the liver’s viscoelastic properties. Factors other than fibrosis affect liver stiffness. We sought to determine whether hepatic congestion related to hemodynamics influences liver stiffness measurements (LSM) assessed by TE.
Methods
This was a prospective cohort study of subjects with Fontan circulation undergoing cardiac catheterization with or without liver biopsy. Subjects underwent TE within 5 days before the procedure. Clinical history, hemodynamic and biopsy data, and hepatic biomarkers were collected. Five subjects who previously underwent liver biopsy and TE were also included.
Results
Data were collected on 50 subjects: 45 with hemodynamics, 10 with biopsy. Median age was 13.1y (range 2.4-57.8), and median time since Fontan was 9.9y (range 0.1-32.5). No subject had known hepatitis C. Mean LSM for the entire cohort was 21.4 ± 10.8 kPa. Univariate regression analysis using LSM as a continuous outcome variable is presented in Table 1. LSM is associated with more severe centrilobular fibrosis (p = 0.05). On multiple regression analysis, Fontan pressure (β = 0.901, p = 0.03) and cardiac index (β = −2.703, p = 0.02) were significant predictors of LSM with overall model R2 = 0.206.
Table 1
| n | Regression coefficient | P value | Pearson correlation | |
| Gender (Female) | 50 | 0.751 | 0.81 | – |
| Ventricular morphology (Left) | 50 | 3.396 | 0.27 | – |
| Patent fenestration | 50 | −5.964 | 0.07 | – |
| Age at Fontan (y) | 50 | 0.241 | 0.28 | 0.16 |
| Age at LSM (y) | 50 | 0.275 | 0.01 | 0.35 |
| Time from Fontan to LSM (y) | 50 | 0.481 | 0.003 | 0.41 |
| RA/Fontan pressure (mmHg) | 45 | 0.901 | 0.04 | 0.31 |
| PAWP (mmHg) | 45 | 0.527 | 0.24 | 0.18 |
| MAP (mmHg) | 45 | −0.046 | 0.74 | −0.05 |
| CI (L/min/m2) | 45 | −2.704 | 0.03 | −0.33 |
| PVR (Wood units, indexed) | 40 | 3.409 | 0.03 | 0.34 |
| Systemic arterial 02 saturation (%) | 45 | 0.513 | 0.04 | 0.31 |
| Systemic venous 02 saturation (%) | 45 | 0.026 | 0.89 | 0.02 |
| Platelets (k cell/uL) | 49 | −0.038 | 0.05 | −0.29 |
| AST (U/L) | 28 | −0.202 | 0.27 | −0.22 |
| ALT (U/L) | 28 | −0.028 | 0.90 | −0.03 |
| GGT (U/L) | 21 | 0.092 | 0.06 | 0.42 |
| Albumin (g/dL) | 29 | 5.179 | 0.17 | 0.26 |
| Total protein (g/dL) | 28 | 4.263 | 0.07 | 0.35 |
| Total bilirubin (mg/dL) | 27 | 1.933 | 0.57 | 0.12 |
Conclusions
Higher LSM is associated with unfavorable Fontan hemodynamics and advanced centrilobular hepatic fibrosis. TE may be a useful screening tool for identifying patients who warrant invasive testing.
CLINICAL UTILITY OF LIVER BIOPSY IN ADULTS WITH FONTAN PALLIATION
Author links open overlay panelNancyMcCabeJennyMas-MoyaAlton B.FarrisRobertElderBrianKogonMichaelMcConnellWendyBook
Emory University School of Medicine, Atlanta, GA, USA
Emory University Department of Pathology, Atlanta, GA, USA
Background
Liver fibrosis is a common complication after Fontan palliation for single ventricle heartdefects, but the clinical utility of liver biopsies is unclear. The purpose of this study was to determine if degree of liver fibrosis on biopsy correlates with clinical findings.
Methods
A chart review of adults with Fontan palliation and a liver biopsy at Emory’s Adult Congenital Heart Center was performed (2001-2011). Core liver biopsies were examined using digitally scanned whole slide images of trichrome-stained sections. Portal and lobular fibrosis were quantitated using a positive pixel count algorithm tuned to detect fibrosis. Logistic regression and bivariate correlations were used to examine the relationship between fibrosis and ventricular dysfunction, IVC diameter, clinical features of portal hypertension (defined as ≥2 of the following: platelets <150K, splenomegaly, varices, ascites), and adverse outcomes (death, transplant, or hepatocellular carcinoma [HCC]).
Results
Ten adults were identified (40% female, mean age 31±7 years). Mean time since Fontan was 18.6 years (range: 6-29), 7 had atriopulmonary connection of whom 4 underwent revision, 8 had a systemic left ventricle, 1 had ventricular dysfunction, and mean IVC diameter was 2.1 ± .23 cm. On biopsy, mean portal area was 1.4 × 105 ± 8.7 × 104 um2 and portal % fibrosis was 66% ± 16%. Mean lobular area was 5.9 × 105 ± 2.4 × 105 um2 and lobular % fibrosis was 20% ± 19%. Features of portal hypertension were present in 7, and 3 had an adverse outcome (death=1, transplant=1, HCC=1). No relationship was found between fibrosis and ventricular dysfunction (p=.26-.59), features of portal hypertension (p=.39-.98), or clinical outcomes (p=.14-.98). A strong positive correlation was found between mean portal area and time since Fontan (r= .82, p=.003) and a moderate trending correlation between portal % fibrosis and IVC diameter (r= .59, p=.07).
Conclusion
In adult patients following Fontan palliation, quantitative portal fibrosis by liver biopsyincreases with time since surgery but does not correlate with clinical outcomes. Further evaluation in a larger population is needed to confirm these findings.
EFFECTS OF RACE, ETHNICITY AND GENDER ON SURGICAL MORTALITY FOR HYPOPLASTIC LEFT HEART SYNDROME
Author links open overlay panelPeter N.DeanKimberlyMcHughDiane G.HillmanMark R.ConawayHowardGutgesell
Children’s National Medical Center, Washington, DC, USA
Background
Mortality rates remain high for patients with hypoplastic left heart syndrome (HLHS). There is limited information regarding the effect of race, ethnicity and gender on outcomes for the three palliative procedures for HLHS.
Methods
We examined the effects of race, gender, age at surgery, type of admission and volume on in-hospital mortality for palliative procedures for HLHS between 1998 and 2007 using data from the UHC, an alliance of 116 academic medical centers. Patients were classified as black, Hispanic, white or other. Effects were compared by chi-square analysis and logistic regression.
Results
1729 patients underwent stage 1 palliation (S1P) with a mortality of 28%. Mortality was higher for females (32%, p < 0.05), blacks (30%, p < 0.001), other races (39.5%, p < 0.001), institutions with fewer than 20 procedures (35%, p < 0.0001) and an earlier era (33%, p < 0.0001). No racial differences were seen at the top five volume institutions (overall mortality 18%), but mortality was higher for blacks (32%) and other races (38%) at lower volume institutions (overall mortality 26%, p < 0.001). Mortality was higher for patients discharged home prior to S1P (37%) versus those born at or transferred to the surgical institution (14%, p < 0.001). Blacks were more likely to be discharged home prior to S1P (12% versus 5% of non-black races, p < 0.001). Mortality for stage 2 palliation (S2P) (1224 patients, 5% mortality) was higher for blacks (11%, OR = 2.99, CL = 1.58-5.67) and Hispanics (11%, OR = 3.42, CL = 1.69-6.90) compared to whites. There were no racial differences for stage 3 palliation (S3P) (1032 patients, 4% mortality). Incidence of prematurity at S1P and age at S2P or S3P did not differ among racial groups.
Conclusions
Risk factors for increased mortality at S1P were: female gender, black or other race, lower volume institution, earlier surgical era and discharge prior to diagnosis. Increased mortality in blacks and other races may be explained by higher mortality at non-top five volume institutions and increased percentage of blacks discharged prior to diagnosis. Racial differences at S2P may account for the reported increased mortality in the first year of life for Hispanic patients with HLHS.
CURRENT TRENDS FOR THE DIAGNOSIS AND SURGICAL TREATMENT OF PARTIAL ANOMALOUS PULMONARY VENOUS CONNECTION
Author links open overlay panelUpinderJodhkaCharlesShepardAllisonBradeeRooseveltBryant
University of Minnesota Amplatz Children’s Hospital, Minneapolis, MN, USA
Background
Partial anomalous pulmonary venous connection (PAPVC) is a rare entity seen in 0.4-0.7% of the population. The connections are highly variable, requiring an individualized approach to surgical repair. Each repair has potential associated complications.
Methods
Retrospective chart review of patients who underwent surgical repair of PAPVC between 2002 and 2012. Early results and long-term surgical outcomes after surgical repair of PAPVC at a moderate sized institution were assessed. A variety of modalities were utilized to diagnose each patient, with ultimate confirmation of diagnosis at surgical intervention.
Results
33 consecutive patients were identified with PAPVC. The anomalously connecting veins were right-sided in 28 patients (85%) and left-sided in 5 patients (15%). The most common type of PAPVC was right PAPVC to the superior vena cava in 17 (51%), followed by right PAPVC into the right atrium in 8 (24%), left PAPVC into the vertical vein in 4 (12%), right PAPVC into the inferior vena cava in 2 (6%, both in patients with Scimitar syndrome), and left PAPVC to a left superior vena cava in 1 (3%) patient. The repair strategy over this period of time included single patch repair in 5 (15%), double patch repair in 14 (42%), Warden procedure in 9 (27%), and direct anastomosis in 5 (15%). There was no early or late mortality. Freedom from further cardiac intervention was 88%. There were 3 (9%) patients who developed superior vena cava obstruction and 2 (6%) required intervention. There was 1 (3%) patient with post-operative pulmonary vein obstruction, which required reoperation. One (3%) patient required cardiac transplantation for restrictive cardiomyopathy, which was diagnosed prior to the PAPVC repair. No patients have required pacemaker implantation.
Conclusion
PAPVC is a rare entity requiring a personalized approach to diagnosis and repair. Contemporary surgical treatment of PAPVC is associated with good outcomes and low morbidity.
THE INCIDENCE AND NATURAL HISTORY OF MITRAL REGURGITATION FOLLOWING SURGICAL REPAIR OF TOTAL ANOMALOUS PULMONARY VENOUS DRAINAGE
Author links open overlay panelDianaMageeDevinChetanYasuhiroKotaniJae-SungSonMarkFriedbergChristopherCaldaroneGlenvan ArsdellJohnColesOsamiHonjo
The Hospital for Sick Children, Toronto, Canada
Background
Upon repair of total anomalous pulmonary venous drainage (TAPVD) in children, the left-sided structures face a sudden increase in preload that may alter mitral valve function. We sought to determine the natural history of mitral regurgitation (MR) following TAPVD repair.
Methods
97 patients who underwent TAPVD repair from 2000 to 2012 were reviewed. TAPVD was supracardiac in 50 (52%), cardiac in 17 (18%), infracardiac in 16 (16%), and mixed in 14 (14%). MR was graded as: 0 − None, 1 − Mild, 2 -Moderate, 3 − Severe.
Results
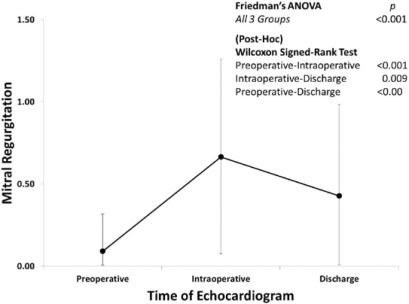
No patient had moderate/severe MR prior to repair. 6 patients (6%) developed moderate MR, 5 (5%) mild-moderate MR, and 24 (25%) mild MR at intraoperative assessment. The 3-year freedom from moderate/severe MR was 88.9%. Of the 62 (66%) patients with postoperative MR, 41 (66%) had functional recovery. Compared to preoperative MR, intraoperative MR worsened, and subsequently improved at discharge, but not to preoperative levels (Fig. 1). None of the patients who developed MR required surgical reintervention. Seven (7%) patients died in the follow-up period but none were due to MR and all 9 patients who developed moderate/severe MR survived. The 3-year freedom from death was 90.4%.
Conclusions
Development of post-operative MR is a relatively common occurrence, although moderate/severe MR is less frequent. The majority of MR improved spontaneously in the postoperative period indicating the functional nature of the mechanism causing MR. Development of MR is not related to mortality.
OUTCOMES AFTER REPAIR OF PARTIAL AND TRANSITIONAL ATRIOVENTRICULAR SEPTAL DEFECTS
Author links open overlay panelJessicaBowmanHaroldBurkhartAdeleGoodloeJosephDearaniSabrinaPhillipsBenjaminEidemFrankCetta
Mayo Clinic, Rochester, MN, USA
Background
Surgical repair of partial atrioventricular septal defects (AVSD) has been successful for over 60 years. Recent data from the Pediatric Heart Network (PHN) show that 31% of patients had moderate/severe left atrioventricular valve regurgitation (LAVVR) at 6 month postoperative. In contrast, previous reports, including data published by our institution, found that only 9% of patients developed more than moderate LAVVR postoperative. Our objective was to determine the long-term outcomes after repair of partial AVSD in the current era and compare those to the PHN data and the earlier experience at our institution.
Methods
Clinical records were reviewed for all patients with partial (including transitional) AVSD who had biventricular repair between 5/1999 and 6/2011 at our institution. Kaplan-Meier method was used to determine survival and potential risk factors were evaluated using Cox proportional hazards models.
Results
Seventy-three patients had repair of partial AVSD during the study time frame. Nineteen (26%) had Down syndrome. Median age at surgery was 9.5 years. Survival at 1-year was 95.1%. Median follow-up was 2.3 years (IQR, 0.3-5.3). At five years postoperative, survival-free of reoperation was 80.1%. Nine patients (12%) required reoperation. Reasons for reoperation included: LAVVR (n=6), LAVV stenosis (n=1), residual ASD (n=1), and relief of LVOTO (n=1). Seven patients (5 within 2 years) developed more than moderate LAVVR with a cumulative incidence of 10.8% by 2 years. None of the patients with Down Syndrome have developed greater than moderate LAVVR. Patient age at surgery (p=0.14) and severity of preop LAVVR (p=0.39) were not identified as statistically significant risk factors for postop LAVVR.
Conclusions
Morbidity and mortality following surgical repair for partial AVSD remain low. The most common reason for reoperation is LAVVR. 10.8% of patients developed more than moderate LAVVR by 2 years postop. These data are in contrast to the PHN data, and our cohort had a longer follow-up period. Additionally, the rate of development of LAVVR was similar in our current cohort when compared to the earlier cohort.
OUTCOMES AND RISK FACTORS FOR MORTALITY IN CHILDREN WITH SINGLE VENTRICLE PHYSIOLOGY WHO ARE SUPPORTED WITH ECMO
Author links open overlay panelDavid J.GoldbergChitraRavishankarRoxanne E.KirschMaryam Y.NaimAntonio R.MottJoseph W.Rossano
The Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Background
Extracorporeal membrane oxygenation (ECMO) is increasingly used in children with single ventricle (SV) anomalies. Our objective is to describe the outcomes and risk factors for mortality in this high-risk group.
Methods
We retrospectively analyzed the Kids’ Inpatient Database (KID) for ECMO use in children ≤ 18 years with SV anomalies for 2000, 2003, 2006, and 2009. The KID is a nationwide sampling of pediatric hospitalizations and is weighted to provide national estimates.
Results
751 children (95% CI 559-943) with SV were supported with ECMO in the four years reported, 87% were infants. Overall mortality was 57% and did not improve over time (2000=52%, 2003=63%, 2006=57%, 2009=55%, p=.66). Compared to children with SV who were not supported with ECMO, those who were supported were more likely to have undergone a cardiac procedure (46% vs. 90%, p<.001) or have an associated diagnosis of arrhythmia (13% vs. 22%, p<.001), cerebrovascular disease (1% vs. 9%, p<.001), heart failure (12% vs. 24%, p<.001), hepatic insufficiency (1% vs. 3%, p<.001), acute renal failure(3% vs. 28%, p<.001), or sepsis (8% vs. 28%, p<.001). For those supported with ECMO, risk factors for mortality by univariate analysis included an associated diagnosis of hepatic insufficiency (mortality 87%, odds ratio 5.2, p=.03) or acute renal failure (mortality 76%, odds ratio 3.3, p<.001). By multivariate analysis only acute renal failure remained as a significant risk factor (odds ratio 3.0, p<.001).
Conclusions
In the four years reported, 43% of children with SV who required ECMO survived although survival did not improve over time. Arrhythmias, heart failure, infection, and end organ dysfunction were more common in SV patients supported with ECMO than those who were not. Acute renal failure was an independent risk factor for mortality. Further studies are needed to identify patients who are most likely to benefit from ECMO support.
PREDICTORS OF MORTALITY IN PEDIATRIC PATIENTS ON VENOUS-ARTERIAL EXTRACORPOREAL MEMBRANE OXYGENATION
Author links open overlay panelRajeshPunnDavidAxelrodStephenRothTheresaTacy
Lucile Packard Children’s Hospital, Stanford University, Palo Alto, CA, USA
Background
Currently, there are no established echocardiographic (echo) or hemodynamic predictors of mortality after venous-arterial extracorporeal membrane oxygenation (ECMO) wean in children. We attempted to determine which echo and hemodynamic measurement predicts mortality.
Methods
Over 2 years, we prospectively assessed 6 echo and 6 hemodynamic variables at 3-5 ECMO flow rates during flow wean. Hemodynamic measurements were: heart rate, inotropic score, arterio-venous oxygenation difference (AV-02), pulse pressure, oxygenation index (OI) and serum lactate. Echo variables included: shortening and ejection fraction, outflow tract Doppler-derived stroke distance (VTI), amount of atrioventricular valve regurgitation, global longitudinal strain (GLS) and global circumferential strain (GCS). Patients were stratified into those who died or needed a transplant (Gr1) and those that did not (Gr2). For each patient, we compared the change within each of these variables between full versus minimum flow for Gr1 versus Gr2 using a paired t-test.
Results
Twenty-one patients were enrolled in the study with an age range of 0.05-15 years. Five had dilated cardiomyopathy while the remaining 16 had structural heart disease with cardiomyopathy. Twelve patients comprised Gr1 with only one heart transplant while 9 who lived constituted Gr2. In Gr1, subjects had a significantly greater increase in AVO2 (31% mean increase, p<0.01) and Ol (43% mean increase, p<0.01) off ECMO compared to full flow but no change in VTI with flow wean. In Gr2, VTI increased significantly (30% mean increase p<0.01) with no change in AVO2 or Ol. GLS was nearly significantly increased off ECMO in Gr2 (p=0.09). Pulse pressure increased significantly in both groups and was not discriminatory (p<0.01).
Conclusions
Failure to augment VTI during ECMO flow wean or an increase in OI and AVO2 portend poor outcomes in pediatric patients. These measurements should be a part of practice standards for patients weaning from ECMO and may discern who will require alternative methods of support. Future studies appear indicated to confirm these findings with a larger sample size.
NEED FOR LATE REINTERVENTIONS IS STRONGLY ASSOCIATED WITH CLASS-3 TECHNICAL PERFORMANCE SCORES (MAJOR RESIDUAL DEFECTS) IN MID AND HIGH COMPLEXITY PROCEDURES
Author links open overlay panelMeenaNathanFrankPigulaHuaLiuKimberleeGauvreauStevenColanMatthewDiOrioFrancisFynn-ThompsonSitaramEmaniChristopherBairdJohnMayerPedro delNido
Children’s Hospital Boston, Boston, MA, USA
Background
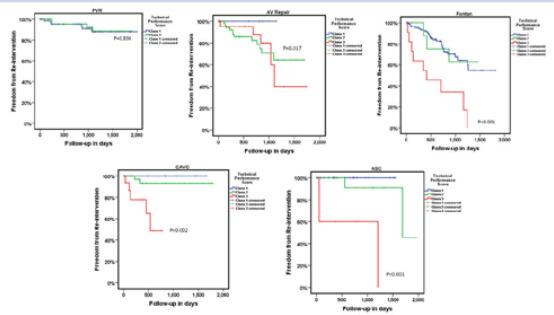
Previous work at our institution, has shown that major residual defects-Class-3 Technical Performance Score (TPS) was associated with more late re-interventions across a range of disease complexity. We hypothesized that this would hold true for specific procedural groups.
Methods
Patients undergoing pulmonary valve replacement (PVR) [low complexity], Fontan [mid complexity], Arterial switch operation (ASO), Aortic valve repair(AVR), complete atrioventricular canal(CAVC) repair [high complexity], from 01/012007 to 09/30/2011 were retrospectively followed. TPS was assigned based on previous methodology as Class-1 (optimal), Class-2 (Minor residual defects), Class-3 (Major residual defects). Length of stay and late (post discharge) re-interventions in anatomic area of repair were analyzed using non parametric methods.
Results
Of 553 patients, 512 had follow-up data. Postoperative median hospital length of stay was significantly higher for class-3 compared to class-1 TPS group in non-neonatal mid/high complexity procedures: AVR (p=0.007), CAVC repair (p>0.001), Fontan (p>0.001). Late reinterventions (Figure 1) was significantly higher for class-3 compared to class-1 TPS group in high complexity procedures such as ASO, CAVC repair and Fontan. Aortic valve repairshad higher rates of re-interventions for both class 2 and 3 TPS.
NOVEL URINARY BIOMARKERS REMAIN ELEVATED YEARS AFTER ACUTE KIDNEY INJURY FOLLOWING CARDIAC SURGERY IN CHILDREN
Author links open overlay panelDavid S.CooperDonnaClaesStuart L.GoldsteinShinaMenonMichaelBennettQingMaCatherineKrawczeski
Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA
Background
Novel urinary biomarkers predict acute kidney injury (AKI) after cardiopulmonary bypass(CPB-AKI). AKI increases risk for future chronic kidney disease (CKD) in adults. We aimed to determine if urinary biomarkers remained chronically elevated in patients (pts) with CPB-AKI (AKI+) vs. without AKI (AKI-).
Methods
We compared CKD clinical/laboratory markers (urine microalbumin/Cr, Schwartz eGFR and blood pressure) and novel urinary biomarkers (uNGAL, uIL-18, uKIM-1 & uL-FABP) in AKI+ (n=19) versus AKI- (n=12) pts 6.8+/− 0.8 yrs (mean) post-CPB. CPB-AKI was defined by the pRIFLE criteria (≥ 50% increase in serum creatinine (sCr) over baseline).
Results
Baseline characteristics between AKI + versus AKI – pts were similar (RACHS-1, CPB time, age at surgery) except for peak sCR (median 0.77 vs 0.48 mg/dL; p=0.02). At follow-up, both cohorts had similar age (7.9 +/− 1.5 vs 7.7 +/− 0.35 yrs). Clinical/laboratory CKD markers were normal in the majority of pts and did not differ between the groups. Urinary biomarker concentrations for AKI + versus AKI – pts are presented in the Table.
Conclusions
In this long term follow-up of children post CPB, we observed 1) persistently elevated uIL-18, uKIM-1 and uL-FABP in AKI + patients, 2) higher uIL-18, uKIM-1 and uL-FABP in AKI + versus AKI – pts and 3) no evidence of classic CKD signs. We suggest novel urinary biomarkers could serve as a more sensitive marker of chronic kidney injury in children who develop post-CPB AKI.
INCIDENCE AND IMPORTANCE OF NEW POSTOPERATIVE RIGHT BUNDLE BRANCH BLOCK AFTER PEDIATRIC ORTHOTOPIC HEART TRANSPLANTATION
Author links open overlay panelJeremy ScottRameyThomasStarcWarrenZuckermanRakeshSinghLindaAddonizioMarcRichmond
Columbia University, New York
Presbyterian/Morgan Stanley Children’s Hospital, New York, NY, USA
Background
Studies have shown right bundle branch block (RBBB) to be the most common (30-70% incidence) ECG abnormality after orthotopic heart transplantation (OHT) in adults, correlating it to higher mean pulmonary artery pressures (PAP) and poorer clinical outcomes. This has not yet been evaluated in pediatric heart transplantation.
Methods
We hypothesized that development of RBBB following pediatric OHT would be associated with higher postoperative mean PAP. A retrospective review was conducted of paired donor and recipient ECGs (24-72 hours post-OHT) and clinical data of all patients who had undergone OHT at our center from 2/5/2000 to 6/13/2011. Students T-test, Mann-Whitney U, Chi-Square and Kaplan-Meier analyses were used as appropriate.
Results
Of 97 pediatric OHT patients, 24 (25%) developed new RBBB and were more likely to be older (11.62 yrs [0.11-17.7yrs] vs. 4.87 yrs [0.5-18.6yrs], p=0.002) and have a higher BSA (1.17m2[0.35-2.07m2] vs. 0.65m2[0.21-1.83m2], p=0.001), with no difference in donor/recipient BSA ratios (p=0.53). There was no association with new RBBB and any intra-transplant factors, including ABO compatibility (p=0.19), crossmatch results (p=0.57), presence of donor downtime (p=0.35), graft ischemic time (p=0.11), cardiopulmonary bypasstime (p=0.35), or elevated donor cardiac enzymes (p=0.62). Development of RBBB was not associated with pre-transplant recipient hemodynamics, including cardiac index (p=0.72), RVEDP (p=0.37), mean PAP (p=0.84), mean RAP (p=0.44), PVRI (p=0.89), or PCWP(p=0.68). Those with new RBBB had lower mean PAP on post-OHT catheterization (6-15 days), both within the normal range (16.4±4.5mmHg vs. 20.2±6.7mmHg, p=0.012). No association was found with any other post-transplant hemodynamic data, evidence of rejection (8% vs. 4%, p=0.68) or ischemia on the first post-op biopsy (25% vs. 22%, p=0.78). New RBBB was not associated with in-hospital mortality (p=0.57), graft survival (p=0.25), or overall mortality (p=0.08).
Conclusion
While the development of RBBB is a common finding in ECGs following pediatric heart transplantation (25%), it is not associated with any known risk factors or clinical outcomes.
DOPPLER FLOW PATTERNS IN THE NEO-AORTA AND RIGHT VENTRICLE-TO-PULMONARY ARTERY SHUNT IN INFANTS WITH SINGLE RIGHT VENTRICLE ANOMALIES: IMPACT ON OUTCOME AFTER INITIAL STAGED PALLIATIONS
Author links open overlay panelPeter C.FrommeltEricGerstenbergerJeanneBaffaWilliamBorderTimothyBradleyStevenColanJessicaGorentzHalehHeydarianJ. BlaineJohnWymanLaiJamiLevineJimmyLuRachelMcCandlessStephenMillerArniNuttingRichardOhyeGailPearsonPierreWong
Meryl Cohen, Medical College of Wisconsin, Milwaukee, WI, USA
Background
A Pediatric Heart Network trial compared outcomes in infants with single right ventricle (RV) anomalies undergoing a Norwood procedure randomized to either modified Blalock-Taussig shunt (MBTS) or right ventricle-to-pulmonary artery shunt (RVPAS). In this cohort, we sought to assess Doppler flow patterns in the neo-aorta and RVPAS as they may provide insight into the physiologic burdens created during initial palliation.
Methods
An echo core lab measured neo-aortic cardiac index (CI), retrograde fraction (RF) in the descending aorta and RVPAS conduit, RVPAS/ neo-aortic systolic ejection time ratio, and systolic/diastolic (S/D) duration ratio early post-Norwood, prior to stage II palliation and at 14 months of age. We examined the association of these Doppler patterns with transplant-free survival, length of ICU/hospital stay after surgeries, and RV functional indices [RV size, ejection fraction (EF), fractional area change, myocardial performance index, and severity of tricuspid regurgitation].
Results
The cohort included 529 subjects with a mean follow-up of 3.0±2.1 years. Neo-aortic CI (8.1±2.7 vs. 4.4±2.0 L/min/m2; p<0.001) and descending aortic RF (45% vs. 4%; p<0.001) were higher in MBTS than RVPAS post-Norwood. RVPAS RF averaged <25% at both interstage intervals. Higher pre-stage II descending aortic RF correlated with decreased RV EF (R=-0.24; p=0.032) at 14 months in MBTS. Higher post-Norwood CI (5.6 vs. 4.4 L/min/m2; p=0.04) and lower S/D ratio (1.40 vs. 1.68; p=0.01) correlated with better interstage transplant-free survival in RVPAS. We found no other associations between outcomes or RV functional status and Doppler flow patterns in either shunt group at any interval.
Conclusion
After the Norwood procedure, infants appear to tolerate significant descending aortic RF (in MBTS) and conduit RF (in RVPAS) with little correlation with transplant-free survival, length of hospital stay, or RV functional indices during the first year. Doppler assessment of neo-aortic cardiac output and S/D duration ratio at the post-Norwood echocardiogram may provide additional non-invasive tools to help identify patients at risk for interstage events after Norwood with RVPAS.
MINIMALLY INVASIVE VIDEO ASSISTED SURGICAL CLOSURE OF ATRIAL SEPTAL DEFECTS: HASTENING RECOVERY USING A SAFE AND EFFECTIVE APPROACH
Author links open overlay panelAnna SabateRotesHaroldBurkhartRakeshSuriMarthaGroganNathanielTaggartHartzellSchaffJosephDearani
Mayo Clinic, Rochester, MN, USA
Background
Minimally invasive video assisted thoracic surgery (VATS), with or without robotic support, permits port-access atrial septal defect closure. We sought to compare the safety and effectiveness of VATS versus conventional median sternotomy (open) in the repair of secundum atrial septal defect (ASD) or patent foramen ovale (PFO).
Methods
Among the 415 consecutive patients undergoing open or VATS ASD/ PFO closure between 1993 and September 2012 (VATS since 2007), 153 patients were compared using 2:1 propensity-matching (n=102 open vs. 51 VATS, respectively). Median age was 43 years (3-71 years) and 67% (n=102) were female. Baseline characteristics including age, gender, body surface area, past medical history of neurologic events, need of patch closure and degree of right ventricular enlargement were similar between the groups.
Results
There were no early deaths in either group. There were no conversions to open sternotomy. Although mean crossclamp time (14±7.6 vs 26±13.2 minutes, p<0.001) and bypass time (32±13.8 vs 61±20.9 minutes, p<0.001) were longer in the VATS group; VATS patients had shorter postoperative ventilation time (7.5±6.4 vs 4.4±2.8 hours, p=0.001) with 62.7% extubated in the operating room; along with shorter intensive care unit stay (26.7±10.8 vs 19.1±9.9 hours, p<0.001) and hospital stay (5.2±1.9 vs 3.5±0.9 days, p<0.001). There were no differences in transfusion requirements, chest-tube drainage, infection, neurologic events or arrhythmias. At early follow-up (mean 1.5 years, maximum 4.2 years) there was no difference in freedom from residual shunt, reintervention, or arrhythmias. Of the 27 patients that underwent VATS ASD/PFO closure for a neurologic event, none had a recurrence.
Conclusions
The use of VATS, with or without robotic assistance, provides a safe, equally effective alternative to conventional sternotomy for ASD/PFO closure. A less invasive port access approach results in shorter ventilation requirements and earlier dismissal from hospital with excellent freedom from recurrent neurologic events.
KOMMERELL DIVERTICULUM SHOULD BE REMOVED WHEN OPERATING SYMPTOMATIC CHILDREN WITH ABERRANT RIGHT SUBCLAVIAN ARTERY (VASCULAR RING)
Author links open overlay panelAlainFraisseCarolineOvaertDeborahLucianoJuliaMitchellBernardKreitmann
AP-HM, Timone Enfants, Marseille, France
Background
Right aortic arch with aberrant left subclavian artery is the most frequent cause of vascular ring. Usual treatment in symptomatic children is ligamentum arteriosus division, leaving the Komerell diverticulum in place with potential risk of residual compression, aneurysmal dilation and dissection or even rupture. Translocation of the aberrant left subclavian artery to the left carotid artery together with removal of the Kommerell diverticulum and division of the ligamentum through a left thoracotomy is currently advocated to avoid those complications.
Results
Between 9/2009 and 8/2011, 13 patients underwent this procedure. Mean age at time of surgery was 7.2 years (median 4.3, range 0.9-18.9), mean weight 25 (median 18, range 8.4-59). All had respiratory symptoms, associated with dysphagia in 5. CT scan and/or MRI had demonstrated the arch anomaly and the dilated Komerell diverticulum in all. Surgery consisted of left postero-lateral thoracotomy followed by arterial ligament division to release compression, diverticulum resection and finally left subclavian artery reimplantation on the left carotid artery. Post-operative complications included transient chylothorax in 4 and phrenic palsy in 1 patient. Mean follow-up reached 8 months (median 2.2, range 0.1-39). Residual symptoms were noted in 3 patients. Echo-Doppler analysis showed a patent left subclavian to carotid artery anastomosis in all but 1 (vessels not seen). Histo-pathologicalanalysis of the resected diverticulum, available in 6 patients, showed cystic medial necrosisand inflammatory tissue in 3, non specific histological findings in 2 and hyperplastic myo-intimal lesions in 1.
Discussion
Translocation of the aberrant subclavian artery together with Komerell diverticulum resection and ligamentum division is a safe and efficient procedure for symptom relief. The observation of profound wall abnormalities such as medial necrosis in the diverticuli that were analyzed encourages us to maintain this strategy.
IMPROVED OUTCOMES WITH PERITONEAL DIALYSIS CATHETER PLACEMENT AFTER CARDIOPULMONARY BYPASS IN INFANTS
Author links open overlay panelDavidKwiatkowskiCatherineKrawczeskiShinaMenonStuartGoldsteinDavidCooper
Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA
Background
Acute kidney injury (AKI) is common in infants after cardiopulmonary bypass (CPB) and is associated with poor outcomes. Peritoneal dialysis (PD) improves outcomes of adults with post CPB AKI, but pediatric data are limited. Since October 2010, we have routinely placed PD catheters (PDC) in the operating room in infants at high risk for AKI. We performed a retrospective matched cohort study to determine if infants receiving PDC would have improved outcomes.
Methods
42 infants with routine PDC placement were each age matched to an infant with similar procedure. Demographic, baseline and outcome data were compared between PDC + and PDC – infants. Our primary outcome was negative fluid balance (FB) on postoperative days 1-3. Secondary outcomes were time to negative FB, electrolyte corrective medications, and time to extubation. Data were compared with McNemar’s, Wilcoxon rank sum, and paired t-tests.
Results
Baseline data did not differ between groups. 25/42 PDC+ infants received PD; 17 were placed to passive drain. PDC+ versus PDC – infants outcomes are presented in the Table. No significant PDC related complications were seen.
Conclusions
PDC use is safe and associated with earlier and more reliably negative FB as well as shorter ventilation and fewer electrolyte corrections in infants at risk for post CPB AKI. Routine PDC use should be considered in high risk infants receiving CPB. Further prospective studies are vital to prove causative effects of PD.
| PDC + | PDC − | p-value | |
| Age | 6 days (3, 9) | 5 days (3, 14) | NS |
| Weight | 3.4 kg (3.0, 3.8) | 3.2 kg (2.5, 3.9) | NS |
| Bypass Time | 164 min (133,194) | 150 min (116,186) | NS |
| Negative Fluid Balance Post-Op Day 1 | 57% | 33% | 0.04 |
| Negative Fluid Balance Post-Op Day 2 | 85% | 61% | 0.01 |
| Negative Fluid Balance Post-Op Day 3 | 67% | 49% | NS |
| Time to Negative Balance | 16 hours (0,24) | 32 hours (24,48) | <0.0001 |
| Time to Extubation | 80 hours (56,128) | 104 hours (48,176) | 0.02 |
| Total Number of Electrolyte Corrective Meds | 1.5 (0,3) | 3 (1,4) | 0.03 |
Percent or median values (25, 75th percentile)
PROFOUND CYTOKINE REMOVAL WITH ULTRAFILTRATION AND MODIFIED ULTRAFILTRATION IN PATIENTS UNDERGOING SURGICAL REPAIR OF CONGENITAL HEART DEFECTS
Author links open overlay panelAlistairPhillipsJianjingXueVincentOlshove
Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA
Background
During cardiopulmonary bypass (CPB) methods to mitigate inflammation are important. Ultrafiltration (UF) and modified UF (MUF) are routinely used during CPB.
Methods
The effluent from UF and MUF, from 41 patients undergoing repair of congenital heart defects on CPB, was evaluate for cytokines. ANOVA analysis was performed p < 0.05 was significant.
Results
Median age (years) 1.72±4.56, mean weight (Kg) 29.7±6.2 kg. 44% had redo sternotomy, mean surgical time of 4:38±1:35 hours and a comprehensive complexity score of 3.8±1.1. Of the patients 51.2% received blood in the operating room.
Conclusions
UF and MUF are effective at reducing cytokines during CPB. MUF seems very important not only for hemo-concentration but also at reducing the cytokine load, and seems important at reducing IL-6 levels.

THE EFFECT OF MODIFIED ULTRAFILTRATION ON ANGIOPOIETINS IN PEDIATRIC CARDIOTHORACIC SURGERY
Author links open overlay panelSeanLangMansoorSyedJamesDziuriaVineetBhandariJohnGiulianoJr.
Yale School of Medicine, New Haven, CT, USA
Background
Cardiopulmonary bypass (CPB) subjects a patient’s blood to hemodilution and nonphysiologic conditions which result in a systemic inflammatory response. Modified ultrafiltration (MUF) counteracts hemodilution, but may also improve outcomes by pro-inflammatory cytokine removal. Vascular growth factors angiopoietin-1 (ang-1) and ang-2 play opposing roles in the capillary leak syndrome seen in patients following cardiac surgery. We hypothesize that the benefits of MUF include the removal of pro-inflammatory mediators, such as ang-2.
Methods
We performed a prospective cohort study. All patients ≤ 18 years of age undergoing cardiac surgery with CPB were offered enrollment. Three serum samples were obtained from each patient: 1. preoperatively, 2. following CPB, and 3. upon intensive care unit (ICU) admission. A final fluid sample from the MUF effluent was also analyzed. Ang-1 and ang-2 levels were determined using sandwich ELISA. The MUF effluent was used to calculate ang-1 and ang-2 percent extraction. The serum sample trends were analyzed by repeated measures ANOVA and paired t tests. The percent extraction was analyzed using the Wilcoxon Signed Rank Test.
Results
To date, 24 subjects have been enrolled. Mean ang-1 levels significantly decreased across all time points (pre CPB 2,987 ± 3,012 ng/ mL, post CPB 1,635 ±1,046 ng/mL, ICU admission 1,036 ± 559 ng/mL; p<0.01). Ang-2 levels were significantly elevated at ICU admission when compared to both pre and post CPB levels (pre CPB 7,425 ± 3,811 ng/mL, post CPB 6,430 ± 3,373 ng/mL, ICU admission 11,126 ± 7914 ng/ mL; p<0.01). There was no significant difference between the mean ang-1 or ang-2 percent extraction within MUF effluent (1.8% ±0.1%, 1.1% ±3.2%, respectively; p=0.34). In addition, the ang-2/1 ratio significantly increased across all time points (3.65 ± 2.41, 5.84 ± 6.58, 16.16 ± 17.87, respectively; p<0.01).
Conclusion
Ang-2/1 ratios significantly increase following CPB in children. The process of MUF removes both ang-1 and ang-2 equally. While data collection is ongoing, our preliminary results suggest that the clinical benefits of MUF cannot be attributed to the removal of larger quantities of ang-2 compared to ang-1.
CONGENITAL HEART DISEASE PATIENTS ARE AT HIGHEST RISK OF RIGHT-SIDED COMPLICATIONS AFTER CARDIAC SURGERY, REGARDLESS THE SIDE OF SURGERY
Author links open overlay panelMark J.SchuuringDavidKoolbergenMarkHazekampPetrSymerskyWimLagrandBarbaraMulderBertoBouma
Academic Medical Center, Amsterdam, The Netherlands
Background
Cardiac surgery relieves symptoms and increases life expectancy in cardiac patients. However, cardiac surgery has risks of complications.
Methods
Adults with congenital (CHD) operated between January 2001 and January 2011 in the Academic Medical Center in Amsterdam were studied. Prevalence of complications in patients with CHD was compared to literature estimates in patients with acquired heart disease (AHD). Data of 412 age and sex matched AHD patients will be available soon.
Results
Data of 412 consecutive CHD patients (age 36 ± 14 years) were studied. Right-sided surgery was performed 122 (30%), left-sided surgery 160 (39%) and both-sided surgery 130 times (31%) times. Patients with CHD suffered more frequently from right ventricular failure (4.4 versus 2%; p < 0.02), pulmonary hypertension (2.4 versus 0.1%; p < 0.01), atelectasis(51.5 versus 30.0%; p <0.01) and pleura effusions (55.8 versus 24.0%; p < 0.01) than patients with AHD. However, patients with CHD suffered less frequently from atrial fibrillation (14.0 versus 51%; p < 0.01), acute coronary syndrome (0.7 versus 3.2%; p < 0.01), acute kidney injury (3.4 versus 7.9%; p < 0.01) and stroke (0.1 versus 2.4%; p < 0.01).
Conclusion
Patients with CHD have more frequent right ventricular failure, pulmonary hypertension, atelectasis and pleura effusions after cardiac surgery than patients with AHD, regardless the side of surgery.
PEDIATRIC RESOURCE EXPENDITURES IN CARDIAC SPECIALTY ENCOUNTERS (PRECISE): DEVELOPMENT OF A COST ADJUSTMENT MODEL FOR CONGENITAL HEART SURGERY
Author links open overlay panelLisaBergersenKimberleeGauvreauJeanConnorMelvinAlmodovarJamesDiNardoJohnTriedmanPujaBankaDionneGrahamSitaramEmaniJohnMayer
Children’s Hospital Boston, Boston, MA, USA
Background
In response to societal pressure to reduce costs and increase value, we sought to develop a methodology to predict cost related to cardiac surgery in congenital heart disease. We combined clinical data from CPT coding and STS registry submissions, rather than administrative claims based metrics such as APR-DRG and CMI, with hospital resource use information.
Methods
Patients undergoing congenital heart surgery at Boston Children’s Hospital were identified in fiscal years 2007 to 2009. Clinical databases, including CPT coding of the primary surgical intervention for the hospitalization, were collected prospectively and linked to total hospital charges for an episode of care. Surgery Cost Categories (SCCs) were developed to group types of surgical procedures using a combination of empiric data and judgment methodology. A multivariable model was built using SCC and additional case characteristics. After accounting for these factors, other determinants of cost following surgery were explored.
Results
In 3 fiscal years 2105 cases were available for analysis. 76 surgical procedure types were categorized in 7 SCCs yielding a grouper variable with an R2 of 47% for the outcome total hospital charges. Explanatory value increased with consideration of patient pre-operative status as determined by age, admission method, and ventilator dependence (R2=59%), and non-cardiac characteristics including weight category, presence of non-cardiac abnormalities, and a genetic syndrome other than trisomy 21(R2=62%). Additional variability in cost for congenital heart surgery was explained with addition of ECMO utilization and greater than one operating room visit during an episode of care (R2=74%).
Conclusions
Combination of clinical data with hospital resource utilization information resulted in a statistically valid predictive model for total hospital costs for congenital heart surgery admissions. This method leads to improved understanding of patients at risk for high resource utilization and could be an important tool for the next generation of institutional reimbursement.
IMPACT REGISTRY: FIRST REVIEW OF COMMUNITY PRACTICE WITH RESPECT TO DEVICE CLOSURE OF ASD AND PDA
Author links open overlay panelJohn W.M.MooreRobertVincentRobertBeekmanLisaBergersenLeeBensonRalfHolzerKathyJenkinsRichardRingelJonathanRomeJimBeachyGerardMartin
Rady Children’s Hospital, San Diego, CA, USA
Introduction
The IMPACT registry captures data on cardiac catheterizations in patients with congenital heart disease. Since inception in January 2011, IMPACT participation has increased to 65 congenital heart centers which have submitted 8889 reports of catheterization. These reports include data specific to ASD and PDA Closures.
Methods
From July 2011 until June 2012, 6834 catheterizations met IMPACT Data Quality Guidelines. Among these, reports of ASD and PDA closures were reviewed including hemodynamicdata, procedural characteristics, and adverse events (AE).
Results
There were 532 (7.8%) ASD closures; median length of stay (LOS) 1.0 day. Indications: RV overload (79.9%), stroke prevention (14.1%), lung disease (2.3%), cyanosis (1.5%), migraine (1.3%). Median Qp/Qs was 1.7; median defect size 12.3 mm. Balloon sizing used in 77.8% (stop flow used in 89.1%). Rim measurement performed in 56.2%. Device implanted in 95%; reason for failure was insufficient rims in 53.9%. Residual shunt >3 mm in 2.7%. AEs included embolization 12 patients (2.3%); 8 retrieved in cath lab, 4 by surgery; arrhythmia requiring medication 4; device malposition or thrombus formation in 3 requiring surgery; tamponade requiring pericardial drainage in 1. Planned cardiac surgery performed in 9 patients; unplanned in 3. There were 472 (6.9%) PDA closures; median LOS < 1 day. Indications: LV overload 58.7%, SBE prevention 34.3%, pulmonary hypertension 7.0%. Median Qp/Qs was 1.4; 60% were conical, 21.5% tubular, 11.7% complex. Device implanted in 97.9%. Residual shunt >3 mm in 1.1%. Pulmonary artery or aortic obstruction in 0.7% and 1.3%. Other AEs: device embolization 6 (1.3%), with cath lab retrieval 5; bleeding needing transfusion 3. Planned cardiac surgery was performed 4; unplanned in1.
Conclusions
Reported success of Device closure of ASD and PDA is high and complication rates are low. Procedural success is lower than expected for ASD device implant. ASD device embolization and malposition were the most common procedural AEs. Device erosion requiring surgery was not reported. PDA device embolization was unusual and did not require surgery. There were no deaths reported.
EFFECT OF FEEDING MODALITY ON GROWTH: A REPORT FROM THE NATIONAL PEDIATRIC CARDIOLOGY QUALITY IMPROVEMENT COLLABORATE
Author links open overlay panelGarickHillNancyRuddPeterBartzDavidHehirMicheleFrommeltJulieSlickerJenaTanemKatherineFrontierKatieTrappQunXiangTaoWangJamesTweddellNancyGhanayem
Children’s Hospital of Wisconsin, Milwaukee, WI, USA
Medical College of Wisconsin, Milwaukee, WI, USA
Background
Achieving adequate growth following stage 1 palliation (S1P) for single ventricle heartdefects often requires supplemental nutrition through enteral tubes. The effect of specific feeding modalities on infant growth remains unclear.
Methods
The National Pediatric Cardiology Quality Improvement Collaborative registry, with data from 47 centers, was queried. Univariate analysis (ANOVA) was used to compare characteristics of patients by feeding modality. Multivariable linear regression was used to study the impact of feeding modality on change in weight for age z-score (WAZ) from S1P discharge to stage 2 palliation (S2P), adjusting for important patient characteristics and post-operative morbidities.
Results
In this cohort of 465 patients, 62% were male and 65% had hypoplastic left heart syndrome. Patients with gastrostomy tubes were older at discharge from S1P and at S2P, and had a shorter interstage period (102 vs. 118 days, p=0.006). Patients in all 5 feeding categories demonstrated improved WAZ score from S1P discharge to S2P. In multivariable analysis, feeding modality was not associated with change in WAZ from S1P discharge to S2P (p=0.72).
Conclusion
Growth during the interstage period from S1P discharge to S2P is not associated with feeding modality. Growth velocity changes during the interstage period may require further investigation given the differences in age at discharge, S2P and interstage length between feeding modalities.
| Results by feeding modality | |||
| Feeding modality (N) | Age at S1P discharge (d) | Age at S2P (d) | Change in WAZ (±SD) |
| Oral only (203) | 35 ± 20 | 157 ± 56 | 0.4 ± 1.2 |
| Oral + nasogastric tube (113) | 31 ± 16 | 146 ± 41 | 0.3 ± 0.9 |
| Nasogastric tube only (63) | 39 ± 32 | 149 ± 49 | 0.5 ± 1.5 |
| Oral + gastrostomy tube (35) | 71 ± 34* | 172±57# | 0.3 ± 0.8 |
| Gastrostomy tube only (51) | 67 ± 26* | 170±57# | 0.3 ± 1.1 |
*
p<0.0001
#
p=0.01
HOSPITAL RESOURCE USE FOR CRITICAL CONGENITAL HEART DEFECT PEDIATRIC ADMISSIONS
Author links open overlay panelRegina MarieSimeoneMatthewOsterCynthia H.CassellBrianArmourMargaret A.Honein
Centers for Disease Control and Prevention, Atlanta, GA, USA
Oak Ridge Institute for Science and Education, Oak Ridge, TN, USA
Background
Some states have implemented newborn screening for critical congenital heart defects(CCHDs). Current healthcare resource use for this population has not been well described. We evaluated hospital resource use among pediatric hospital admissions with CCHDs.
Methods
We analyzed data from the Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project 2009 Kids’ Inpatient Database to estimate pediatric hospital admissions (≤ 20 years), charges and length of stay (LOS). We included admissions with any ICD-9-CM code indicating at least one of 12 CCHD types. We excluded uncomplicated hospital births, CCHD admissions with a chromosomal abnormality, and admissions missing age, charge, or LOS. We examined median charges and LOS for all admissions and those with a CCHD.
Results
Of 7,370,203 pediatric admissions, 4,467,044 met our inclusion criteria, including 25,658 with any CCHD diagnosis. Median charges were about 15 times higher for infants with CCHDs and about three times higher among young adults (age 11–20) compared to all admissions (Table). Median LOS was about three times higher for infants with CCHDs and about 1.5 times higher among young adults compared to all admissions.
Discussion
CCHD admissions represent 0.6% of pediatric admissions and have disproportionately higher charges and longer LOS. Newborn screening for CCHDs could reduce late CCHD diagnosis and might decrease hospital visits, mortality, and morbidity with timely treatment and management.
| All pediatric admissions | Pediatric admissions with a CCHD1 diagnosis | |||||
| Age (Years) | Total hospital stays | Median charges (dollars) for each hospital stay (IQR)2 | Median length of stay (days) for each hospital stay (IQR)2 | Total hospital stays | Median charges (dollars) for each hospital stay (IQR)2 | Median length of stay (days) for each hospital stay (IQR)2 |
| < 1 | 1,765,164 | 5,628 (2,683–17,133) | 2.1 (1.3–3.9) | 16,883 | 83,429 (19,691–221,662) | 6.6 (2.1–17.9) |
| 1–5 | 627,338 | 9,336 (5,218–18,332) | 1.6 (0.7–2.8) | 5,163 | 58,896 (20,013–127,227) | 4.3 (1.6–8.6) |
| 6–10 | 336,623 | 12,842 (6,918–24,570) | 1.8 (0.8–3.4) | 1,410 | 46,899 (19,124–109,922) | 3.1 (1.0–6.0) |
| 11–15 | 420,190 | 14,430 (7,920–27,715) | 2.1 (1.0–4.4) | 1,112 | 46,600 (19,258–94,519) | 3.0 (0.9–5.6) |
| 16–20 | 1,317,729 | 11,288 (6,988–20,000) | 1.9 (1.2–3.0) | 1,090 | 34,268 (14,080–92,791) | 2.9 (1.1–5.5) |
| Total | 4,467,044 | 9,483 (4,614–20,239) | 1.9 (1.1–3.5) | 25,658 | 69,453 (19,331–173,785) | 5.2 (1.8–13.4) |
1 CCHDs (ICD-9-CM) include the 12 primary and secondary targets of current newborn screening practices: hypoplastic left heart syndrome (746.7), pulmonary atresia (746.01), tetralogy of Fallot (745.2), transposition of the great arteries (745.10), tricuspid atresia (746.1), truncus arteriosus (745.0), total anomalous pulmonary venous return (747.41), coarctation of the aorta (747.10), double outlet right ventricle (745.11), Ebstein’s anomaly (746.2), interrupted aortic arch (747.11), single ventricle (745.3).
2 Interquartile Range
THE FINANCIAL IMPACT OF GEOGRAPHY IN PRE- AND POSTNATAL DETECTION OF CRITICAL CONGENITAL HEART DISEASE IN A BROAD REFERRAL AREA
Author links open overlay panelJennieAllenMarkLewinMegVernon
Seattle Children’s Hospital, Seattle, WA, USA
Background
Prenatal detection of critical congenital heart disease (CCHD) is associated with reduced morbidity and mortality. Along with technologic advances, the medical benefits have prompted more rigorous prenatal screening resulting in higher prenatal detection rates of CCHD in some areas. Seattle Children’s Hospital is unique in that we accept referrals from an area over 800,000 square miles including the states of Montana and Alaska, and rural Washington where availability of prenatal screening is variable. There have been no studies analyzing the financial impact of pre- versus postnatal detection of CCHD in our region, important from several viewpoints including that of insurance companies, the government and families.
Objectives
Identify the rate of prenatal detection of CCHD within our referral area and the charges associated with pre- and postnatal detection of CCHD.
Methods
We performed a retrospective study of infants <6mo of age with CCHD referred to our hospital born between 01/09– 01/12. The timing of the diagnosis of CCHD and charges for care were documented based on regional as well as estimated data. Pre-hospital charges (ie. fetal echos, fetal cardiac consults, and emergent transport for infants from outlying areas) and hospital charges were collected. Charges were compared between infants with a pre- and postnatal diagnosis of CCHD from different geographic areas. Data was also collected for specific cardiac lesions such as d-TGA (d-transposition of the great arteries).
Results/Conclusions
The prenatal detection rate of infants referred with CCHD was higher in the Greater Seattle Area (50%) compared to outlying areas (29%). For d-TGA mean prenatal detection charges were $11,866 compared to postnatal charges of $51,547 in outlying areas (p<0.027). The transport charges were the most costly component. Hospital charges were also higher for infants diagnosed after birth from outlying areas compared to those born in Seattle, likely reflecting the severity of illness on presentation. Efforts made to increase prenatal detection of CCHD in outlying areas of our region are likely cost effective and may improve outcomes.
IMPACT OF A SINGLE-VENTRICLE INTERSTAGE HOME MONITORING AND CLINICAL MANAGEMENT PLAN ON INTERSTAGE OUTCOMES AND RESOURCE UTILIZATION
Author links open overlay panelDavid W.BrownPatO’BrienKatie E.CohenMatthewGlynnTerrySaiaKimberleeGauvreauDavidFultonFrankPigulaKathyJenkins
Boston Children’s Hospital, Boston, MA, USA
Background
Dedicated home monitoring programs for infants with single ventricle heart disease (SVD) in the interstage (IS) period between first and second stage palliation are becoming standard of care due to reports of improved somatic growth and IS survival; however, the impact of such programs on resource utilization is unknown.
Methods
We performed a retrospective review of two infant cohorts with SVD who underwent Stage 1 palliation (S1P) at Boston Children’s Hospital and were discharged to home in 2007–2009 without an IS program (Group 1, n=65), or in 2010–2012 (Group 2, n=50) with an IS program that included home monitoring and a standardized clinical assessment and managementplan (SCAMP). Clinical course through bi-directional Glenn (BDG) was compared.
Results
Baseline characteristics were similar, including anatomy (78% hypoplastic left heart syndrome), gestational age (39 weeks), birthweight (3.2 kg), genetic anomalies (9%), pre-operative risk factors (34%), type of S1P, and post-S1P complications (75%). At discharge, age (30 days), 02 saturation (83%), weight/age z score (−1.7) were similar, but all oral feeding was more common in Group 2 (77% vs 89%, p=0.04). Total IS days did not differ (118 vs 123, p=0.85), although at BDG Group 1 had lower 02 (76% vs 80%, p=0.01) and trend toward younger age (152 vs. 171 days, p=0.10). Median number of clinic visits (4), ≥ 1ED visits (36%), and ≥1 unplanned readmissions (37%) did not differ; among those readmitted, the fraction of IS days spent hospitalized trended larger in Group 1. Group 2 had improved IS weight gain (20 vs 23 g/day, p=0.02), larger weight at BDG (6.0 vs 6.2 kg, p=0.02), and trend toward improved weight/age Z scores at BDG (−1.9 vs. −1.3, p=0.09). More required IS cardiac reoperation in Group 1 (10% vs 0%, p=0.03); unplanned interventional catheterizations were similar (31% vs 44%, p=0.67). There were fewer IS deaths in Group 2 (8 vs. 4), though not statistically significant (p=0.76). BDG outcomes were similar.
Conclusions
Infants with SVD followed by an IS SCAMP including home monitoring had improved rates of oral feeding and somatic growth with no increase in inpatient resource utilization, and a reduction in some measures such as reoperation.
RIGHT VENTRICULAR FAILURE IS DIASTOLIC HEART FAILURE AND IS NOT CAUSED BY HYPERTROPHY OR FIBROSIS
Author links open overlay panelMarinus AlexanderBorgdorffBeatrijsBarteldsMichaelDickinsonPaulSteendijkMaartje deVroomenRolfBerger
Center for Congenital Heart Diseases, University Medical Center Groningen, Groningen, The Netherlands
Leiden University Medical Center, Leiden, The Netherlands
Introduction
Right ventricular failure (RVF) is a main determinant of outcome in congenital heart diseasesand pulmonary hypertension. Unfortunately, little is known about its causes. Our aim was to study the pathophysiology of RVF by comparing rats with clinical RVF to rats without clinical RVF, in a model of chronic pressure load.
Methods and Results
Wistar rats were subjected to pulmonary artery banding (1.1mm) and then daily checked for clinical signs of RVF (inactivity, ruffled fur, dyspnea, ascites). Clinical RVF ensued after a period of 52±5 days in 56% of rats. At the onset of clinical RVF (necessitating termination), echocardiography and pressure-volume analysis were performed in those with RVF and in paired compensated rats (noRVF). Pressure load was equal in RVF and noRVF (table). In clinical RVF, cardiac index and TAPSE were lower than in noRVF. RVF rats had pericardial effusion, liver congestion, and dilated right atria, in contrast to noRVF rats. Hemodynamically, RVF rats showed preserved contractility (end systolic elastance), but severe diastolic dysfunction (end diastolic elastance, end diastolic pressure). While RV hypertrophy was equal in both groups, interestingly, myocardial fibrosis was significantly higher in noRVF, which suggests that fibrosis might be protective.
Conclusion
Chronic pressure load is sufficient to induce RVF, but not via excessive hypertrophy or fibrosis. RVF is characterized by diastolic failure, thus improving diastolic function may be the key to treating RVF.
Hemodynamics, hypertrophy and fibrosis
| CON | noRVF | RVF | |
| RV peak pressure (mmHg) | 25±1 | 69±6* | 73±4* |
| Cardiac index (mL/min/g) | 0.32±0.01 | 0.19±0.02* | 0.11±0.02*# |
| TAPSE (mm) | 3.4±0.2 | 2.0±0.2* | 1.2±0.2*# |
| End systolic elastance (mmHg/mL) | 40±3 | 101±21* | 269±77* |
| End diastolic elastance (mmHg/cL) | 19±1 | 114±17* | 323±95*# |
| End diastolic pressure (mmHg) | 1±0 | 3±1* | 6±1*# |
| RV fibrosis ($$) | 5±1 | 29±3* | 16±2*# |
| RV hypertrophy (mg/g) | 0.6±0.1 | 1.4±0.1* | 1.3±0.1* |
Means±SEM.
*
p<0.05 vs CON (n=7).
#
p<0.05 RVF (n=5) vs nonRVF (n=4).
STRAIN BY FEATURE TRACKING PREDICTS CLINICAL OUTCOME IN PEDIATRIC PATIENTS WITH HYPERTROPHIC CARDIOMYOPATHY
Author links open overlay panelBrandonSmithAdamDorfmanSunkyungYuPrachiAgarwalMaryam GhadimiMahaniJimmyLu
University of Michigan, Ann Arbor, MI, USA
Background
In hypertrophic cardiomyopathy (HCM), left ventricular strain by speckle tracking echocardiography is decreased in areas of hypertrophy. Data are not available on strain measurement by feature tracking on cardiovascular magnetic resonance (CMR), or its relation to clinical outcome in pediatric patients.
Methods
This single center, retrospective study included all patients under 21 years with clinical diagnosis of HCM and CMR from 2007-2012, compared to controls with normal left ventricular ejection fraction (LVEF) and no congenital heart disease, left ventricular hypertrophy, or genotype associated with cardiomyopathy. Using a 16-segment model, hypertrophied segments were identified by agreement of two experienced readers blinded to outcome. Strain was evaluated by segment, using feature tracking software (TomTec, Unterschleissheim, Germany), averaged over 16 segments for global radial (GRS) and circumferential (GCS) strain, and compared using repeated measures analysis of variance. The composite outcome was death, non-sustained ventricular tachycardia, or ventricular fibrillation.
Results
Thirty patients with HCM (14.1±3.2 years), with 11 (37%) confirmed by genotype and 24 (80%) with hypertrophy, and 24 controls (15.6±2.8 years) were included. LVEF was higher in HCM patients (65.4±5.8 vs. 59.4±3.0%, p <0.0001), with greater GCS (−29.3±4.6 vs. −26.7±2.7, p=0.01) and similar GRS (61±20 vs. 54±11, p=0.15). However, compared to controls, phenotypic HCM patients had decreased GRS (32.3±5.0 vs. 54.3±3.7, p=0.002) and basal circumferential strain (−22.6±1.5 vs. −26.8±0.9, p=0.03). Phenotype negative HCM patients had greater GRS (69.2±3.5 vs. 54.3±3.7, p=0.01) and GCS (−30.5±0.8 vs. −26.7±0.8, p=0.003) compared to controls. After median follow-up of 1.2 years, 7 patients (23%) with the composite outcome had decreased GRS (median 39.7 vs. 65.4, p=0.01) and a trend toward decreased GCS (median −25.8 vs. −29.6, p=0.06) compared to those without negative outcome.
Conclusions
In pediatric HCM patients, strain by feature tracking may be an important marker of phenotype and clinical outcome. Further study is necessary to evaluate longitudinal changes in this population.
A NOVEL ECHOCARDIOGRAPHIC MEASUREMENT IN PEDIATRIC HEART TRANSPLANT RECIPIENTS WITH DILATED CARDIOMYOPATHY: CAN WE MAXIMIZE THE DONOR SUPPLY?
Author links open overlay panelEuniceHahnWarrenZuckermanMarcRichmondJonathanChenRakeshSinghLindaAddonizio
Columbia University College of Physicians and Surgeons, Division of Pediatric Cardiology, New York, NY, USA
Background
In normal pediatric echocardiograms, the distance from the junction of superior vena cavaand right atrium to inferior vena cava and right atrium (SVC-IVC) is linearly related to height. We examine this relationship in children listed for heart transplant with dilated cardiomyopathy (DCM) compared to a previously defined normal distribution of SVC-IVC in order to maximize potential donor acceptance.
Methods
Measurements of SVC-IVC and left ventricular end-diastolic diameter (LVEDd) in 55 patients (pts) with DCM (age 2 months – 19 years, median 7.8 years) were correlated with height, weight, body surface area (BSA), and BSA0.5. Regression analyses were performed to find the best-fit equation and correlation coefficient. Generalized linear modeling compared DCM to normal SVC-IVC values from 254 pts.
Results
There was a strong linear relationship in DCM pts between SVC-IVC and height (R2=0.84) and a logarithmic relationship to weight (R2=0.80). LVEDd did not correlate to SVC-IVC or any other parameter. In 89% of DCM pts, SVC-IVC was over 2 standard deviations above predicted normal values (mean z-score = 4.3±2.1). Predicted SVC-IVC in DCM pts was different than published norms (p<0.001).
Conclusion
SVC-IVC in pediatric DCM pts, while linearly related to height, is consistently above normal values (figure). When matching pediatric heart recipients to donors, SVC-IVC may help accurately size donor hearts, especially for bicaval anastomosis, and substantially increase the donor pool.

INTERPRETING MEASUREMENTS OF CARDIAC FUNCTION USING VENDOR-INDEPENDENT SPECKLE-TRACKING ECHOCARDIOGRAPHY IN CHILDREN: A PROSPECTIVE, BLINDED COMPARISON WITH CATHETER-DERIVED MEASUREMENTS
Author links open overlay panelSuma PotinyGoudarGirishShiraliShahryarChowdhuryG. HamiltonBakerMarkScheurer
Medical University of South Carolina, Charleston, SC, USA
Background
Adult studies have shown that speckle-derived echo measures of cardiac function correlate with invasive measures of diastolic function, but no such studies have been done in children. Our aim was to compare speckle-derived measures of cardiac function to measurements routinely obtained by cardiac cath in children.
Methods
Echos were performed on the day of cardiac cath. Using Tomtec 2D Cardiac Performance Analysis, longitudinal strain (LS), longitudinal strain rate (LSR), diastolic LSR and ejection fraction for the right and left ventricle (RV and LV) were calculated via speckle-tracking. These were compared to cardiac output and index, dp/dt, ventricular end-diastolic pressure(EDP) and pulmonary capillary wedge pressure(PCWP) by fluid-filled catheters. A blinded observer performed all echo measurements.
Results
Fifty studies were done on 29 patients ages 4 mos to 20 yrs. Their diagnoses included cardiac transplant (48 studies), repaired AV canal (1), and dilated cardiomyopathy (1). RV EDP ranged from 2-22 mm Hg and PCWP ranged from 6-32mmHg. See table below for Results:
| RV EDP | RV dp/dt | |||
| Correlation coefficient | p-value | Correlation coefficient | p-value | |
| RV longitudinal strain | 0.379 | 0.01 | 0.412 | 0.005 |
| RV | ||||
| diastolic | −0.136 | 0.379 | N/A | N/A |
| strain rate | ||||
| RV | 0.065 | 0.675 | −0.143 | 0.356 |
| ejection fraction | ||||
| LV EDP | LV dp/dt | |||
| Correlation coefficient | p-value | Correlation coefficient | p-value | |
| LV global longitudinal strain | 0.588 | 0.04 | −0.653 | 0.02 |
| LV 2-chamber longitudinal strain rate | 0.673 | 0.01 | −0.574 | 0.04 |
| LV global diastolic strain rate | 0.297 | 0.349 | N/A | N/A |
Conclusion
Speckle-derived measures of function have stronger correlation to catheter-derived measures in the LV compared to the RV. LV global LS has the strongest correlation with invasive function measures, whereas diastolic strain did not correlate well with catheter-derived filling pressures in children. Ongoing studies are being performed using micromanometer catheters to confirm our findings.
DIAGNOSTIC ERRORS IN OUTPATIENT ECHOCARDIOGRAPHY IN INFANTS AND YOUNG CHILDREN: THE IMPACT OF PROCEDURAL SEDATION
Author links open overlay panelKenan W.D.SternKimberleeGauvreauGaryPierceyOscarBenavidez
Boston Children’s Hospital, Boston, MA, USA
Massachusetts General Hospital, Boston, MA, USA
Background
Echocardiography is commonly performed in infants and children for evaluation of heart disease. These patients often cannot lie still during an echocardiogram (echo), which may result in incomplete examinations, suboptimal image quality, and diagnostic errors. These errors may possibly be prevented if procedural sedation is used to improve study conditions. We sought to examine study quality measures and diagnostic error in children ≤ 36 months and determine the impact of procedural sedation on these outcomes.
Methods
Echos from 2008-2009 on outpatients ≤ 36 months were reviewed. We collected demographic, image quality concern and study completeness data. Diagnostic errors were identified and categorized by review of the echo images and medical record. Errors were categorized as not preventable (incorrect modality), possibly preventable (preventable with improved technique/conditions) or preventable (image interpretation error).
Results
Among 1515 echos (428 sedated) 15% were incomplete and 49% had image quality concerns. The diagnostic error rate was 7.1%; 11% of errors were not preventable, 63% possibly preventable and 26% preventable. The majority of errors (64%) were in patients with medium/high anatomic complexity. Patients with greater anatomic complexity were more likely to have a sedated echo. Sedated echos had fewer quality concerns (22% vs. 59%) and were less often incomplete (2% vs. 20%), p < 0.001. Diagnostic errors in unsedated echos were more often categorized as possibly preventable/ related to study technique (76% vs. 44%, p < 0.001). In multivariate analysis, errors were increased in medium complexity disease (adjusted odds ratio (AOR) 2.85, p < 0.001), high complexity disease (AOR 4.21, p < 0.001) and pre-intervention echos (AOR 3.37, p < 0.001). Examining possibly preventable errors separately, the use of sedation trended towards an association with lower odds for error (AOR 0.58, p = 0.07).
Conclusion
Quality concerns and incomplete studies are frequent in outpatient echocardiograms in children ≤ 36 months. Procedural sedation improves these measures and is associated with a trend towards a decreased rate of possibly preventable diagnostic errors.
IS MRI SAFE IN PEDIATRIC PATIENTS WITH PACEMAKERS AND EPICARDIAL LEADS: LONG-TERM FOLLOW-UP DATA
Author links open overlay panelWilsonKingJasonGarnreiterThomasPilcherSusanEtheridgePatriciaWhitakerElizabethSaarel
St. Louis University, St. Louis, MO, USA
University of Utah, Salt Lake City, UT, USA
Background
MRI has historically been contraindicated in patients with cardiac pacemakers (PM) due to concerns for circuitry malfunction, rapid pacing, and heating of both the generator and leads. This is a problem given the increasing number of children and adults with PM and the growing number of indications for MRI in cardiac and noncardiac disease. We previously reported that MRI can be performed in patients with a PM and non PM-dependent rhythm with no acute adverse events and no acute change in PM function when the device is temporarily deactivated and patients are carefully monitored. In this study, we evaluated the long-term safety of MRI in pediatric patients with PM, including those with epicardial leads. Pacing thresholds, sensing thresholds, and lead impedance obtained prior to MRI were compared to subsequent PM interrogations and to controls without MRI exposure.
Methods
All patients with PM were entered into a prospective registry at a single pediatric center. Nine patients who had a non-PM dependent rhythm (mean age 13.4±8.7 years) underwent MRI with a 1.5 ? GE scanner between 6/2007 and 12/2010 (4 cardiac, 3 brain, 2 spine). Six had congenital heart disease and 3 had primary arrhythmias. Five patients had epicardialleads. PM included dual chamber (2), atrial (3), and ventricular (4) systems.
Results
No adverse reactions occurred during or immediately after the MRI, and PM settings and function were unchanged immediately after the scan. Patients were followed for a mean of 3.2 years after MRI. No PM failed during the interim. Atrial and ventricular lead sensing, pacing, and impedance did not significantly change, and were not significantly different when compared to controls. Subgroup analysis did not detect any significant pacing, sensing, or impedance changes for patients with either endocardial or epicardial leads.
Conclusion
MRI did not change long-term PM generator function, sensing or pacing thresholds, or lead impedance in our pediatric patients. More data is required to determine the long-term safety of MRI in children with PM including those with epicardial leads.
SILDENAFIL IMPROVES ESTABLISHED RIGHT VENTRICULAR DYSFUNCTION VIA ENHANCEMENT OF DIASTOLIC FUNCTION
Author links open overlay panelMarinus AlexanderBorgdorffBeatrijsBarteldsMichaelDickinsonPaulSteendijkMaartje deVroomenRolfBerger
Center for Congenital Heart Diseases, University Medical Center Groningen, Groningen, The Netherlands
Leiden University Medical Center, Leiden, The Netherlands
Background
Right ventricular (RV) failure is a major determinant of mortality in pulmonary hypertensionor congenital heart diseases. Sildenafil (SIL) benefits the RV when started at the onset of pressure load (prevention). However, it is unknown whether SIL is effective in established RV dysfunction (therapeutic strategy). We assessed the effects of SIL on RV function and fibrosis in a rat model of established RV dysfunction that is not amenable to pulmonary vasodilatory therapy.
Methods
Wistar rats were subjected to pulmonary artery banding (PAB), which results in pressure load-induced RV dysfunction in 4 wks. From week 4 onward, PAB rats were treated with SIL (100mg/kg/d) or placebo (VEH). After 4 (baseline) and 8 wks (end) invasive RV pressure-volume analysis was performed. RV fibrosis was measured as % surface area using Masson-Trichrome staining.
Results
PAB induced RV dysfunction after 4 wks, characterized by decreased ejection fraction (EF: 27±2 vs 47±3%, PAB vs CON, p<0.05). Subsequently started SIL improved EF at 8 wks (43±5 vs 33±3%, SIL vs VEH, p<0.05). This was due to improved diastolic function (end diastolic elastance, end diastolic pressure, see figure) rather than improved contractility (end systolic elastance unchanged). The improvement was accompanied by attenuated fibrosis.
Conclusion
Sildenafil is useful in treating established RV dysfunction via improving diastolic dysfunction. This is clinically important, as many patients present in a progressed stage of RV dysfunction.

STRAIN RATE CORRELATES BETTER THAN TISSUE DOPPLER VALUES IN ESTIMATING VENTRICULAR FILLING PRESSURES IN PATIENTS WITH SINGLE RIGHT VENTRICLES
Author links open overlay panelNaziaHusainJanakiGokhaleLisaNicholsonRalfHolzerCliffordCua
Nationwide Children’s Hospital, Columbus, OH, USA
Background
Increased ventricular end-diastolic pressure (VEDP) is a known risk factor for morbidity and mortality in patients with single ventricle physiology. Tissue Doppler imaging (TDI) analysis has been shown to modestly correlate with direct measurement of VEDP. Myocardial deformation imaging, also known as strain (S) and strain rate (SR) imaging, has not yet been compared to VEDP in this patient population. The goal of this study was to evaluate which of these imaging techniques correlates best with VEDP in patients with single right ventricle (RV) physiology.
Methods
Patients with single RV physiology who underwent simultaneous echocardiography and cardiac catheterization were included in this prospective study. Echocardiographic data included global SRe, global SRa, TDI e’, TDI a’ of the RV free wall, and right atrioventricular valve inflow velocities (E and A wave). E/SRe and E/e’ were calculated. VEDP was obtained from the cardiac catheterization report. Correlations of echocardiographic and catheterization variables were examined using Pearson’s correlation. Receiver operating characteristic curves were used to determine echocardiographic predictive variables for VEDP. P < 0.05 was considered significant.
Results
Twenty two patients were studied (16 hypoplastic left heart syndrome, 5 double outlet right ventricle/tetralogy of Fallot, and 1 unbalanced atrioventricular septal defect). Median age at the time of the catheterization was 11.2 months (range 0–132 months). Mean VEDP was 9.4 + 2.8 mmHg. VEDP correlated significantly with E/SRe ratio (r = 0.87) and with global SRe (r = −0.43). There were no significant correlations between VEDP and TDI measurements. ROC curve analysis using an E/SRe cut off of 1.5 showed 79.2% sensitivity for a VEDP greater than 10.
Conclusions
In patients with single right ventricle physiology, VEDP correlated strongly with strain rate and not with TDI measurements. Strain rate measurements should be used to estimate VEDP in this complex patient population rather than TDI. Clinical implications of this imaging modality need to be further investigated in this population.
CARDIAC HYPERTROPHY IN HUMAN NEWBORNS WITH CONGENITAL HEART DISEASE MODIFIES MATURATIONAL CHANGES IN CARDIAC ENERGY METABOLISM AND NEGATIVELY AFFECTS POSTSURGICAL FUNCTIONAL RECOVERY.
Author links open overlay panelAldaHuaiJayJaswalVictoriaLamIvan R.RebeykaGary D.Lopaschuk
University of Alberta, Edmonton, Canada, University of Pisa, Pisa, Italy
Background
Despite improvements in surgical techniques, ischemia-reperfusion injury (IR) with reduced ventricular functional recovery remains a major predictor of morbidity and mortality among newborns with congenital heart disease (CHD). Modulation of energy substrate metabolism positively affects IR in adult patients undergoing cardiac surgery. However, these findings cannot be extrapolated to newborns with CHD who may undergo obligatory maturational changes. We sought to determine age-related changes in major fatty acid (FA) and carbohydrate metabolism enzymes and their regulation at transcriptional level in human newborns with CHD undergoing corrective surgery. We also determined the difference in maturational changes in patients displaying hypertrophy and its correlation with functional recovery capacity.
Methods
Right ventricular specimens were collected from 59 newborns (age 0-200 days) undergoing surgery. Based on a z-score for right ventricular free wall thickness, patients were stratified as non-hypertrophied (34) or hypertrophied (25). Western blot analysis for major FA and glucose metabolism enzymes, and transcriptional regulatory proteins was performed. Clinical outcomes including post-surgical right and left ventricular functional recovery were also assessed.
Results
Since shortly after birth, neonates displayed an age-related increase in of FA oxidation, and a decrease in carbohydrate oxidative capacity. Hypertrophied hearts displayed an overall reduced expression of key proteins involved in the transcriptional regulation of cardiac energy metabolism at the mitochondrial level, in this way suggesting a vulnerable energetic state. In support with this hypothesis, following surgery, patients displaying hypertrophypresented with a worse ventricular functional recovery. The effects of hypertrophy on clinical outcomes remained significant when entered into multivariate analysis.
Conclusions
In line with animal studies, human newborns with CHD undergo obligatory age-related metabolic maturational changes that are modulated in the setting of hypertrophic response and can be responsible for worse peri-procedural outcomes.
DOPPLER ECHOCARDIOGRAPHY INACCURATELY ESTIMATES RIGHT VENTRICULAR PRESSURE IN CHILDREN WITH ELEVATED RIGHT HEART PRESSURE
Author links open overlay panelGeorgeannGrohPhilipLevyMarkHollandJoshuaMurphyTimothySekarskiGautamSingh
Washington University School of Medicine, St. Louis, MO, USA
Washington University, St. Louis, MO, USA
Background
Doppler echocardiography (DE) is widely used as a surrogate for right heart catheterization(RHC), the gold standard, to assess and monitor elevated right heart pressure in children. However, its accuracy has not been validated in children.
Methods
Simultaneous pressure gradients between right ventricle and right atrium were prospectively assessed by RHC and DE using tricuspid valve regurgitation in 98 consecutive children (age 0-18 yrs, median 5.8 yrs) with 2 ventricle physiology and a wide range of right heart pressures. Subjects were grouped based on RHC measured right ventricular systolicpressure (RVP): group 1 (n=56) with RVP<1/2 systemic systolic blood pressure (SBP) and group 2 (n=42) with RVP >1/2 SBP. Elevated right heart pressure was defined as RVP>1/2 SBP. Correlation and agreement between the methods were assessed using linear regression and Bland-Altman analysis, respectively. Accuracy was predefined as 95% limits of agreement (LOA) ±10mmHg.
Results
Correlation between DE and RHC measured RVP was strong in both groups (group 1: r=0.8, p<0.001; group 2: r=0.77, p<0.001). Agreement between the two methods was good in group 1 (bias 2.5mmHg, 95% LOA +9.4 to −4.5 mmHg), but poor in group 2 (bias −0.68mmHg, 95% LOA +22.8 to −24.2 mmHg) (Figure 1). DE estimated RVP was inaccurate in 2% of subjects in group 1 vs. 33% in group 2.

Conclusion
DE estimates of RVP may often be inaccurate and should not be solely relied upon in the management of children with elevated right heart pressure.
THE IMPACT REGISTRY (IMPROVING PEDIATRIC AND ADULT CONGENITAL TREATMENT): UPDATE AND TRENDS
Author links open overlay panelRobert N.VincentJohnMooreLeeBensonLisaBergersenRalfHolzerKathyJenkinsRichardRingelJonathanRomeJoanMichaels
Gerard Martin, Emory University School of Medicine, Atlanta, GA, USA
Background
IMPACT is a voluntary NCDR registry gathering information on all cardiac catheterizationprocedures in pediatric and adult congenital heart disease patients as well as detailed data on 6 specific interventions.
Methods
This report summarizes the data and trends that we have seen from Jan 2011 through June 2012 for diagnostic catheterizations. For adverse events, the last 4 quarters of data are presented.
Results
The number of sites submitting data increased from 12 to 65. During this period there were 8889 events (cathlab visits) of which 33.2% were for diagnostic catheterizations and 66.8% for specific or multiple interventions. 2,986 candidate procedure records are excluded because they did not meet NCDR data quality thresholds. Diagnostic procedures were performed on 232 newborns (<30 days of age); 750 infants (>=30 days and <=1 yr); 1499 children (>1 yr and <= 18 yr) and 470 adults (>18yr). Procedures were elective (85%), urgent (13%), emergent (2%) or salvage (<1%). Most procedures were performed using general anesthesia (77%). All cause adverse events associated with diagnostic catheterizations (occurring from the onset of the catheterization procedure to discharge) were noted in 11.4% of patients. Adverse events were most common in newborns (16.2%) and infants(4.9%) with children and adults 1.3% each. All cause in hospital mortality was 3.5% for newborns; 4.7% infants; 0.5% children and 0.6% adults.
Conclusions
As the IMPACT registry grows we are gathering data in order to set national benchmarks for diagnostic and certain specific interventional procedures. Future versions of IMPACT will hopefully address risk stratification, attribution of adverse events and long term follow-up of interventions and allow us to create recommendations for catheter intervention based on the data being compiled. Although adverse events as currently reported are not necessarily attributable to the catheterization procedure itself, it is clear that newborns and infants who require a diagnostic catheterization are at risk of adverse events, including death, during their hospital admission.
LOST IN CARE: CAN WE IMPROVE TRANSITION FOR ADULTS WITH CONGENITAL HEART DISEASE IN THE UNITED STATES?
Author links open overlay panelMadhukarKollengodeCurtisDanielsJenneHickeyAliZaidi
Nationwide Childrens’ Hospital, Columbus, OH, USA
The Ohio State University Wexner Medical Center, Columbus, OH, USA
Background
With improved pediatric care there are now more than 1 million adults with congenital heart disease (ACHD) in the U.S. It is well known that loss of care (LC) is linked to poor long term outcomes in ACHD. Previous U.S. studies have investigated LC in a biased population. We sought to describe the major factors leading to LC in a U.S. population of adult patients (pts) with CHD.
Methods
All pts 16-17 yrs. old with CHD seen in 2003 at a free-standing children’s hospital were included, regardless of whether they continued cardiology care. Several methods to contact pts and document long term follow-up were utilized. When found, subjects completed a questionnaire addressing demographics, knowledge of their cardiac defect, and barriers to seeking medical care. Subjects with no documented cardiology follow-up visits (adult, pediatric, or ACHD) since 1/2007 were deemed LC.
Results
Of 197 eligible pts, a total of 74 pts (37.6%) were LC as of 2011. 58 of 197 pts (age 24y ±1.22) completed the survey. Among those LC who were successfully contacted, 46.7% were not receiving any medical follow-up. A higher complexity of CHD (p<0.01) and use of prescription cardiac medications (p<0.001) were associated with an increased likelihood of long term follow-up. Care provided by an ACHD specialist (p<0.001) and focused education regarding the need for specialized long-term care (p<0.003) were associated with improved continuity. Though often cited by pts as a major barrier, lapses in insurance were not a statistically significant reason for LC (p=0.08).
Conclusion
Our study demonstrated, for the first time, that in an unbiased U.S. population over 1/3 of CHD pts have LC from age 16-17 to adulthood. Nearly 1/2 of those do not maintain any medical follow-up. Improved cardiac follow-up was found in those who were followed by an ACHD provider, received directed CHD education, used cardiac medications, and had a higher complexity of CHD. Lower complexity of CHD and a lack of access to specialized ACHD care may be precipitating factors for LC. Improving LC in the U.S. by establishing successful transition in CHD is critical and must be addressed to improve the long-term outcomes for this growing population.
TEEN KNOWLEDGE OF LIFE-LONG CONGENITAL CARDIAC CARE
Author links open overlay panelSusan M.FernandesAmyVerstappenMathieuClairMaryRummellJosephMaresKirstenDummerDeenaBarberStephenCrumbAmiBhattMaryCannobioMasatoTakahashiRobertaWilliamsMichaelLandzberg
Lucile Packard Children’s Hospital, Palo Alto, CA, USA
Boston Children’s Hospital, Boston, MA, USA
Background
National management guidelines recommend that approximately 50% of adult survivors with congenital heart disease (CHD) receive life-long congenital cardiac care (LLCCC) guided in adulthood by an adult congenital heart disease (ACHD) specialist; the number of adults receiving such care appears far less. Inadequate knowledge regarding LLCCC may contribute to care interruption. Given this, we sought to determine the knowledge of adolescents and young adults regarding LLCCC.
Methods
In this multi-center study we administered a survey to patients 13-20 years of age with surgically repaired CHD including: repaired aortic coarctation, repaired tetralogy of Fallot, and those that have undergone arterial switch operation or Fontan procedure. We assessed understanding of their need for LLCCC and type of recommended care providers. Predictors of teen knowledge regarding LLCCC were also assessed.
Results
A total of 201/207 patients approached in the outpatient clinic setting (9 centers) agreed to study participation; median age was 16.2+2.3 years; 60% male. While the need for LLCCC was recognized by 78% of subjects, only 35% recognized that their care should be guided by an ACHD specialist in adulthood. Only 36% of respondents stated that their current cardiology team had spoken to them about LLCCC, but 89% wished to learn more. Older patients were more likely to understand the need for LLCCC than younger patients (16.4+2.3 versus 15.5+2.3, p=0.034). Gender, race, ethnicity, underlying cardiac surgical diagnosis and center of care were not predictive of LLCCC knowledge.
Conclusion
A substantial number of adolescents and young adults with moderate and complex CHD lack knowledge about LLCCC, but most have a desire to learn more about the type of care they will require in adulthood. Transitioning education/assessment ensuring successful transfer to adult-oriented care for this population should emphasize the importance of LLCCC.
UTILIZATION TRENDS OF CONGENITAL HEART DISEASE PATIENTS 10-29 YEARS IN NEW YORK STATE AND CALIFORNIA
Author links open overlay panelRoberta G.Williams
University of Southern California, Los Angeles, CA, USA
Children’s Hospital Los Angeles, Los Angeles, CA, USA
Background
Understanding resource utilization patients with congenital heart disease (CHD) is critical for health care planning. We examined planned vs. emergent (ED) hospitalizations of children and adults with CHD from 2005-2009 in two states, California (CA) and New York State (NYS).
Methods
We obtained a 100% sample of hospitalization data from Healthcare Cost and Utilization Project including State Inpatient Databases in CA and NYS 2005-2009. We calculated total and ED admissions of CHD patients by age groups. We imputed cost for the hospital stays, based on charges and hospital-level charge-to-cost ratios. We normalized the data by population size and calculated annual averages per 100,000 population.
Results
See the table below on the number of annual admissions and cost/100,000 population, CA vs. NYS 2005-2009:
| CA | CA | CA | CA | NYS | NYS | NYS | NYS | |
| Age (years) | 10–14 | 15–19 | 20–24 | 25–29 | 10–14 | 15–19 | 20–24 | 25–29 |
| Non-ED admissions | 16.5 | 15.4 | 10.8 | 11.5 | 25.3 | 23.7 | 19.4 | 20.2 |
| ED Admissions | 4.4 | 6.3 | 7.9 | 8.0 | 3.6 | 5.2 | 6.2 | 6.9 |
| Cost (rounded to $1,000) | $578K | $521K | $359K | $348K | $472K | $435K | $398K | $364K |
Conclusions
A trend for reduction in scheduled admissions and increase in ED admissions begins in adolescence but becomes more marked during the 20’s in both states. Although the total admissions/100,000 population is higher in NYS than CA, cost/year for NYS is less. This may indicate cost savings with pre-emptive care. However, other factors such as practice patterns and structure/availability of services also need to be explored.
DEATH ATTRIBUTABILITY
Author links open overlay panelCarlBackesBugsuOvuncSaroshBatlivalaSthuthiDavidKevinKollinsJonathanRomeLisaBergersenRalfHolzer
Nationwide Children’s Hospital, Columbus, OH, USA
Background
30-day post-procedure mortality is commonly used as a quality outcome metric in surgical (STS) and cardiac catheterization (PCI) registries. It is unclear though, whether this parameter is sufficiently specific to meaningfully capture mortality attributable to cardiac catheterization in patients with congenital heart disease.
Methods
Multi-center cohort study with three participating tertiary referral centers. Source documents (medical records, autopsy data, imaging data) were retrospectively reviewed for patients who died within 30 days of cardiac catheterization performed between 01/2007 and 06/2012. Attributability of death was assigned to each case.
Results
A total of 14,707 cardiac catheterization procedures were performed during the study period. Death occurred within 30 days in 281/14,707 (1.9%) of cases. 88% of cases were emergent or non-elective cases. The median age was 4.2 year (1d-46yr). The median interval between cardiac catheterization and death was 11.2 days (0d-30d). In 159/281 (57%) of cases, cardiac surgery and catheterization occurred within 30 days of each other. Death was likely or probably attributable to the catheterization procedure in 30/281 (11%) of cases. Catheterization related AE eventually resulting in death included primary arrhythmias (n=3), cardiac arrest (n=6), vascular or cardiac trauma (n=9), device related problems (n=1), neurologic injury (n=2), and other AE or hemodynamic compromise within 24 hours following the procedure (n=8). Death was attributable to cardiac surgery in 17%, pre-cath clinical status unrelated to cath or surgery in 26%, post-cath clinical status unrelated to cath or surgery in 28%, and non-cardiac comorbidity in 16%. In 2%, death attributability could not be clearly established.
Conclusions
In a large majority of children with congenital heart disease who die within 30 days of catheterization, the procedure appears not to be a major contributor to mortality. While valuable in other settings, unadjusted 30 day mortality may not be nearly as useful a quality metric for patients with congenital heart disease undergoing cardiac catheterization.
IN-HOSPITAL ARRHYTHMIAS AFTER CONGENITAL HEART SURGERY FOR ADULTS: INCIDENCE AND RISK FACTORS
Author links open overlay panelZelihaKoyakRoel C.A.AchterberghJoris R. deGrootFelixBergerDavid R.KoolbergenMark G.HazekampNico A.BlomBerto J.BoumaBarbara J. MMulder
Academic Medical Center, Asmterdam, The Netherlands
Deutsches Herzzentrum, Berlin, Germany
Background
Little is known about the clinical impact of arrhythmias after surgery for congenital heart disease (CHD) in adults. Therefore, we investigated the prevalence and clinical variables associated with in-hospital arrhythmias after CHD surgery and its impact on clinical outcome.
Methods
Adults with congenital cardiac surgery between January 2009 and December 2011 from 2 referral centres were included. Pre-, intra-, and postoperative data were reviewed retrospectively. Clinical events were defined as cardiovascular death (CVD), heart failure (HF) requiring intravenous diuretics, thrombo-embolic event, endocarditis and permanent pacemaker (PM) implantation
Results
Overall, 419 patients were included (mean age at surgery 38±14 years, 55% male). Arrhythmias occurred in 134 patients (32%) and were supraventricular tachycardia (SVT, 25%), bradycardia (11%) and ventricular tachycardia (VT, 5%). In multivariate analysis age ≥40 years at surgery (OR 2.5, 95% Cl 1.4-4.6, P=0.003), NYHA functional class≥ll (OR 2.4, 95% Cl 1.2-4.7, P=0.009), coronary bypass (CBP) time (OR 1.35/60 minute increase, 95% Cl 1.06-1.82, P=0.019), CK-MB max (OR 1.05 per 10 U/L increase, 95% Cl 1.01-1.09, P=0.021) and significant subpulmonary atrioventriculair valve regurgitation (PAVR) (OR 2.8, 95% Cl 1.2-6.7, P=0.018) were associated with in-hospital arrhythmias. Fifty-nine clinical events occurred in 54 patients (13%) and included permanent PM implantation (5%), HF (3%), CVD (3%), endocarditis (2%), thrombo-embolic event (1%) and other (1%). In-hospital arrhythmias were independently associated with clinical events (OR 7.8, 95% Cl 2.4-25.5, P=0.001) and were driven by bradycardias. However, when PM implantation was not considered as a clinical event, SVTs were associated with a more than two fold increased risk of clinical events (P=0.046).
Conclusion
Arrhythmias are highly prevalent (one out of three) after adult congenital heart surgery. Older and symptomatic patients with significant PAVR at baseline are at risk for in-hospital arrhythmias. In hospital arrhythmias, especially SVTs, are highly associated with worse clinical outcome, whereas bradycardias for permanent PM implantation.
PHACE SYNDROME IS COMMONLY ASSOCIATED WITH UNUSUAL AND POTENTIALLY “SILENT” SEVERE AORTIC ARCH OBSTRUCTION: THE INTERNATIONAL PHACE SYNDROME REGISTRY REVIEW
Author links open overlay panelPeter C.FrommeltMichelle L.BayerDawn H.SiegelKristenHollandIlonaFriedenAlfonsKrolJohannes M.P.J.BreurElenaPopeOrliWargonBeth A.Drolet
Medical College of Wisconsin, Milwaukee, WI, USA
Background
PHACE syndrome is characterized by large infantile hemangiomas of the head and neck associated with anomalies of the brain, heart, cerebral vasculature, eyes, and chest wall. Congenital heart disease (CHD) in PHACE is common but incompletely described. We sought to better characterize CHD in PHACE using a large international registry.
Methods
The medical records of 175 subjects meeting criteria for PHACE syndrome from the PHACE Syndrome International Clinical Registry and Genetic Repository were reviewed to describe associated cardiac and aortic arch pathology.
Results
49/175 (28%) were identified as having cardiac pathology. Coarctation/interrupted aortic arch was most common, found in 27/49 (55%). The coarctation was usually characterized by bizarre long segment transverse arch narrowing with adjacent segments of aneurysmal dilatation, and 16/27 had an associated aberrant origin of a subclavian artery so that both subclavian arteries arose distal to the obstruction. Intervention was performed in 18/27 subjects, and 14/18 procedures occurred after 1 month of age despite severe obstruction at diagnosis, with 3 requiring interposition grafts during infancy. 10/49 (20%) had a right aortic arch, and 5/10 had a vascular ring requiring surgical division. Only 1 subject had a bicuspidaortic valve (without coarctation) and none had mitral valve disease. Superior systemic venous anomalies (bilateral SVC’s or retroaortic innominate vein) were also frequently seen (20%). Intracardiac pathology was less common, with 11 having a VSD (3 requiring surgical closure), 2 tetralogy of Fallot, 1 pulmonary valve stenosis, and 1 tricuspid atresia.
Conclusion
This series provides the most extensive review of PHACE syndrome cardiac pathology and confirms the high risk of significant CHD. Unusual and severe aortic arch pathology is frequent and may be difficult to appreciate clinically because of associated aberrant origin of a subclavian artery. The lack of associated intracardiac findings suggests a primary aortopathy. Cardiac and aortic arch imaging with detailed assessment of arch patency and brachiocephalic origins is required upon diagnosis in all suspected PHACE patients.
LEFT CORONARY ARTERY ANGLE OF TAKEOFF IN PATIENTS WITH TRANSPOSITION OF THE GREAT ARTERIES AFTER ARTERIAL SWITCH OPERATION IS NOT RELATED TO FUNCTION BUT IS RELATED TO LEFT VENTRICULAR MASS: A CMR STUDY
Author links open overlay panelMark A.FogelThomasPawlowskiMarcKellerMatthewHarrisStephenParidonKevinWhitehead
Childrens Hospital of Philadelphia, Philadelphia, PA, USA
Background
Pts with transposition of the great arteries (TGA) may have varied coronary artery patterns; reimplantation during arterial switch operation (ASO) may necessitate acute angles of takeoff from the aortic root impacting left ventricular (LV) performance.
Methods
Retrospective review of CMR scans from 2005–2011 with TGA after ASO with coronary imaging, LV cines & phase contrast velocity mapping. Angle of takeoff measurement of the coronaries were made tangential to the aortic root in 2 orthogonal planes (axial & sagittal); the smaller angle was taken by protocol (see image). Significance = P<0.05.
Results
57 pts, ages 13.8+6.8 yrs were found; 53 had 2 or 3 coronary ostia & 4 had a single coronary artery. Left coronary artery angle of takeoff significantly correlated with indexed LV mass; a lower angle implies a more acute coronary takeoff (see graph). No significant correlations were noted between angle of takeoff of either right, left or single coronary arteries with LV ejection fraction, indexed LV end-diastolic or end-systolic volumes or cardiac index at rest. When pts were divided into those with an angle of takeoff < 450 or > 450, no significant differences in LV function at rest or mass were noted.
Conclusions
Left coronary artery angle of takeoff in pts with TGA after ASO is not related to function at rest but is related to LV mass. This suggests that LV hypertrophy may change the angle of takeoff of the coronaries which may impact LV performance during exercise; a further study is warranted.
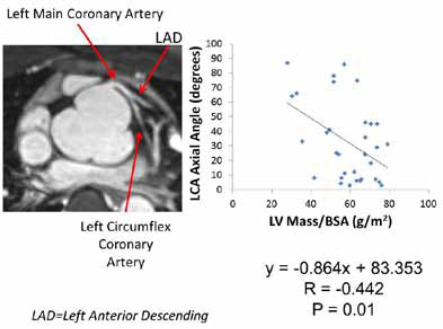
INCIDENCE OF CORONARY ARTERY ANOMALIES IN PULMONARY ATRESIA WITH MAJOR AORTOPULMONARY COLLATERALS
Author links open overlay panelAshokMuralidaranRichardMainwaringV. MohanReddyFrankHanley
Stanford University School of Medicine, Stanford, CA, USA
Background
Pulmonary atresia with Ventricular Septal Defect and Major Aortopulmonary Collaterals (PA/VSD/MAPCA’s) is a complex form of congenital heart disease. Although it has been recognized that coronary artery anomalies are frequently associated with many other conotruncal defects, the incidence of coronary anomalies in PA/VSD/MAPCA’s has not been documented. The purpose of this study was to evaluate the incidence of coronary anomalies in PA/VSD/MAPCA’s.
Methods
64 consecutive patients undergoing their first surgical procedure for repair of PA/VSD/MAPCA’s were included in this study. The coronary artery patterns were documented based on the observations made intra-operatively. These data were then compared to the coronary artery patterns identified at cardiac catheterization.
Results
There were 6 different coronary artery patterns (one normal and five anomalous) observed. 73% had a normal coronary artery pattern, while 27% had an anomalous coronary origin and course. Abnormal coronary artery patterns included:
15% left anterior descending originating from the right coronary artery
5% branch of left comes from right and supplies septum(dual LAD)
3% right coronary originating from left coronary artery
3% branch of right comes from left and supplies free wall
1% right coronary originating from the non-coronary sinus
In addition to these anomalous coronary artery patterns, there were two additional coronary artery abnormalities noted. This included the pulmonary artery arising from the coronary system (n=3) and a MAPCA arising from a coronary (n=2).
Cardiac catheterization corroborated the coronary artery patterns found intra-operatively in 91% of cases. The 9% that did not correlate were all false negatives.
Conclusions
The incidence of anomalous coronary arteries was 27% in PA/VSD/MAPCA’s. An additional 8% had coronary artery abnormalities noted. This incidence of coronary artery anomalies is significantly higher than for most other forms of conotruncal defects. We would emphasize the importance of recognizing these anomalous patterns during placement and/or replacement of conduits from the right ventricle to the reconstructed pulmonary arteries.
LONG-TERM PROGNOSTIC IMPACT OF DOBUTAMINE STRESS ECHOCARDIOGRAPHY IN PATIENTS WITH KAWASAKI DISEASE AND CORONARY ARTERY LESIONS: A 15-YEAR FOLLOW-UP STUDY
Author links open overlay panelNobutakaNotoHiroshiKamiyamaKensukeKarasawaMamoruAyusawaNaokataSumitomoTomooOkada
Nihon University School of Medicine, Tokyo, Japan
Background
Although dobutamine stress echocardiography (DSE) is an established technique for the detection and prognostic stratification of coronary artery disease, the prognostic utility of DSE in adolescents and young adults with Kawasaki disease (KD) and coronary artery lesions (CALs) to predict cardiac events is unknown.
Methods
To determine the prognostic value of DSE involving a 15-year follow-up for predicting cardiac events, 58 patients (pts) (mean age:12.7±4.7 years) at the convalescent stage of KD, including 36 pts with CALs documented by previous coronary angiography and 22 pts with normal coronary artery documented by echocardiography who underwent DSE repeatedly, were reviewed at the initial testing (I) (mean age 13.6±4.4 years) and at a 15-year follow-up (F). Follow-up events were tabulated as cardiac death, nonfatal myocardial infarction, and revascularization.
Results
During a mean follow-up of 14.7 years, there were 8 pts (13.7%) with revascularization(CABG 4 pts, PTCRA 4 pts) and 8 pts (13.7%) with nonfatal myocardial infarction (AMI 1 pt, OMI 7 pts) without any cardiac death. Significant coronary artery disease (CAD) (>70% diameter reduction) was detected in 18 pts (31.0%) at (I), and 24 pts (41.3%) at (F). DSE was positive in 22 pts (37.9%) at (I) and 28 pts (48.2%) at (F). Thus, the sensitivity and specificity of DSE for the detection of CAD were 74 and 95% at (I) and 92 and 96% at (F), respectively. While, no significant difference was observed in wall motion score index (WMSI) at peak stress by DSE between (F) and (I) (1.18±0.14 vs. 1.17±0.15). Five (85%) of 6 pts with false positive DSE (WMSI>1.25) at (I) who all had giant aneurysms (>8 mm) without CAD, developed significant CAD with cardiac events at (F). Cumulative event free survival to 15 years was 25.0% in pts with WMSI>1.25 and 91.7% in pts with WMSI<1.25, respectively. Cox regression analysis showed the grade of peak WMSI(1 to 5) at (I) to be the only independent predictor of future cardiac events (RR:3.28, 95% CI:1.73 to 6.20, p=0.0003).
Conclusions
DSE provided optimal risk stratification and independent prognostic information up to 15 years after the initial testing in pts with KD and CALs regardless of the existence of CAD.
PREVALENCE OF INTRAUTERINE DEMISE IN FETUSES WITH CONGENITAL HEART DEFECTS: 12-YEAR PROGRAMMATIC REVIEW
Author links open overlay panelKatharineBowersAllisonDivanovicJamesCnotaErikMichelfelder
Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA
Background
Congenital heart defects (CHD) are amongst the most common birth defects and impact ∼1% of all babies born in this country. Intrauterine demise (IUFD) in the fetus with CHD is reported to occur at higher rates than the overall population incidence of 6 per 1000 births. As such, fetal CHD is often considered a medical indication for early delivery. However, the advantages of a mature and larger neonate are well described in congenital heart surgery. To inform this risk/benefit discussion, we aim to determine contemporary IUFD rates in the fetus with CHD. We hypothesize that the fetus with isolated CHD is not at increased risk of IUFD.
Methods
We identified all women who underwent fetal echocardiography at our institution from 1998 to 2010. Data was obtained regarding the presence of extracardiac anomalies, confirmed genetic diagnosis, pregnancy outcome and post-natal cardiac diagnosis. Fetuses with minor defects (e.g. small VSDs, isolated LSVC) and complications of twinning (e.g. conjoined twins, twin-twin transfusion syndrome) were excluded. Cardiac diagnoses were grouped into 8 basic categories. Fisher’s exact test was used to compare pregnancy outcome by risk groups.
Results
Out of 500 fetuses with prenatal diagnosis of significant CHD, 21 (%) experienced IUFD, 15 (3%) underwent termination, and 431 (86%) were confirmed live deliveries. 27 (5%) pregnancy outcomes remain unknown. In those fetuses with IUFD, 4 (19%) had a confirmed genetic diagnosis, 11 (52%) had confirmed extracardiac anomalies, and 6(29%) had severe valvar regurgitation (5 Ebstein’s anomaly, 1 tetralogy of Fallot with absent pulmonary valve). Genetic diagnosis remained unknown in 17 cases of IUFD. Extracardiac anomaly (p < 0.000018) and genetic diagnosis (p < 0.003) were associated with IUFD but category of CHD was not.
Conclusion
In isolated fetal CHD without severe valve regurgitation, the risk of IUFD does not exceed that of the general population. As such, early delivery to avoid the risk of IUFD is not indicated for most fetal CHD. These findings inform the ongoing risk/benefit discussion of scheduled delivery in this population.
SHOULD DELIVERY PLANS BE MODIFIED TO DECREASE POSTNATAL RESOURCE UTILIZATION IN INFANTS WITH PRENATALLY DIAGNOSED CONGENITAL HEART DISEASE?
Author links open overlay panelJoyceJohnsonLloydTaniTylerBardsleyL. LuAnnMinichMichaelPuchalskiJanByrneNelangiPinto
University of Utah, Salt Lake City, UT, USA
Background
Prenatally diagnosed infants with congenital heart disease (CHD) who require surgery before discharge often have a delivery plan. We sought to determine the modifiable factors in perinatal management that impact postnatal resource utilization.
Methods
We reviewed infants with prenatally diagnosed CHD (born 8/05 to 12/11) requiring cardiac surgery before discharge. Exclusion criteria: <36 weeks, interventions before cardiac surgery, or transplant evaluation. Multivariate linear regression models were used to determine the impact of demographic and modifiable clinical factors on length of stay (LOS) and hospitalization cost.
Results
Diagnoses (n=126) included single ventricle (60), coarctation (23), pulmonary atresia/stenosis (18), DTGA (11), TAPVR (3), IAA (3), and truncus arteriosus (8). Initial admission to the NICU vs CICU was independently associated with longer ICU LOS (30 vs 22d), total LOS (35 vs 27d), and more days intubated (16 vs 12) after adjusting for RACHS-1, birth weight, syndrome, PGE, delayed sternal closure, infections, and ECMO (Table). Hospital cost, intubation days, and LOS were not affected by day of delivery.
Conclusions
For infants with prenatally diagnosed CHD requiring surgery before discharge, initial admission to the NICU (vs. CICU) is associated with an increase in ICU LOS, total LOS, and days intubated. Prenatal planning for infants with CHD should consider initial place of admission as a modifiable factor to potentially lower resource utilization.
Predictors of Resource Utilization: Multivariate Analysis
| Factor (multivariate analysis) | ICU LOS (days) | Hospital LOS (days) | Length of Intubation (days) | Hospital Cost ($) |
| NICU vs. CICU | +24% (p=0.03) | +19% (p<0.05) | +46% (p=0.002) | +7% (p=0.5) |
| Weekday vs weekend delivery | +10% (p=0.4) | +5% (p=0.6) | −11% (p=0.5) | −4% (p=0.7) |
| RACHS-1 (≥ 5 vs <5) | +11% (p=0.3) | +12% (p=0.2) | +33% (p=0.01) | +27% (p=0.009) |
| PGE dependence | +12% (p=0.4) | +10% (p=0.4) | +8% (p=0.7) | +3% (p=0.8) |
QUALITY IMPROVEMENT IN SCREENING FOR CRITICAL CONGENITAL HEART DISEASE
Author links open overlay panelMatthewOsterKristina W.KuoWilliamMahle
Sibley Heart Center, Children’s Healthcare of Atlanta, Atlanta, GA, USA
Emory University School of Medicine, Atlanta, GA, USA
Background
Unlike other newborn screening programs, screening for critical congenital heart disease(CCHD) with pulse oximetry requires human interpretation of a previously published algorithm, a feature that raises concerns about quality. We hypothesized that a) this method would be prone to error and b) a computer-based tool would lead to a more accurate interpretation of the screening results.
Methods
We performed a randomized crossover study at our institution in 2012 to compare the performance of a paper algorithm vs. a computer-based tool for interpretation of results from screening for CCHD with pulse oximetry. Each of the 102 participants was given 2 sets of 10 screening scenarios and was asked to interpret the results of each scenario as “Pass,” “Fail,” or “Retest.” Unknown to the participants, each set contained 4 “Pass” scenarios, 3 “Fail”, and 3 “Retest.” Healthcare providers with prior experience using pulse oximetry who would be likely to interpret results from such a screening program were eligible. Participants were randomized to use either the paper algorithm or computer-based tool for the first set of 10 scenarios and the alternative method for the second set. We used Wilcoxon rank sum tests to compare the accuracy of interpretation using the 2 methods.
Results
Overall, the subjects answered only 81.6% of the scenarios correctly when manually interpreting the algorithm. This result improved to 98.3% correct when using the computer-based tool (P<0.0001). These differences were most pronounced for the “Fail” scenarios (65.4% for the manual algorithm vs. 96.7% for the computer-based tool, P<0.0001) and the “Retest” scenarios (80.7% for the manual algorithm vs. 98.7% for the computer-based tool, P<0.0001), but were also significant for the “Pass” scenarios (94.1% for the manual algorithm vs. 99.0% for the computer-based tool, P=0.0002).
Conclusions
Use of a manual algorithm for the interpretation of results in screening for CCHD with pulse oximetry may be greatly susceptible to human error. Implementation of a computer-based tool to aid in the interpretation of the results is likely to lead to improved accuracy and quality of any pulse oximetry screening program.
PRENATAL DIAGNOSIS OF CONGENITAL HEART DEFECTS: DOES IT MAKE A DIFFERENCE IN SURVIVAL?
Author links open overlay panelMatthewOsterChristopher H.KimAaron S.KusanoJanet D.CraganPaul B.DresslerAlice H.RougeuxWilliamMahleAdolfoCorrea
National Center on Birth Defects and Developmental Disabilities, CDC, Atlanta, GA, USA
Sibley Heart Center, Children’s Healthcare of Atlanta, Atlanta, GA, USA
Background
While prenatal diagnosis of congenital heart defects (CHDs) has been shown to decrease preoperative morbidity, the impact on survival is unclear. We sought to determine the association of prenatal diagnosis of CHDs by echocardiography with 1-year survival in a large, population-based cohort.
Methods
We identified infants with CHDs in the 1994-2005 Atlanta birth cohort ascertained and classified as critical (Figure) or non-critical by the Metropolitan Atlanta Congenital Defects Program. Among infants with isolated CHDs (no extra-cardiac defects and no chromosomal anomalies), we estimated Kaplan-Meier survival probabilities stratified by prenatal vs. postnatal diagnosis and estimated Cox proportional hazard ratios (HRs) adjusted for gestational age and maternal race/ethnicity.
Results
Of 539,519 live births in the study birth cohort, 4,366 infants had CHDs, of which 3,065 were isolated. Among infants with isolated CHDs, 1-year survival was significantly lower for those with prenatal diagnosis (Figure). The adjusted HR comparing those with prenatal vs. postnatal diagnosis was 1.00 (95% CI: 0.14, 7.35) for the non-critical CHD cohort and 2.54 (95% CI: 1.74, 3.70) for the critical CHD cohort.
Conclusion
Prenatal diagnosis is associated with lower 1-year survival for infants with isolated critical CHDs but no change for those with isolated non-critical CHDs. Varying disease severity within critical CHD subtypes for prenatal vs. postnatal diagnosis might explain this association.

INFLAMMATORY CYTOKINES PREDICT HOSPITAL COURSE AFTER NEONATAL HEART SURGERY
Author links open overlay panelWilliamMahleRitaWillisMatthewStrickland
Children’s Healthcare of Atlanta, Atlanta, GA, USA
Emory University, Atlanta, GA, USA
Cardiac surgery in infants results in a profound inflammatory response secondary to cardiopulmonary bypass (CPB) and the need for blood products. It is not clear how this inflammatory response modulates post-operative course or whether quantification of pro-inflammatory cytokines can aid with risk stratification. In this study, we prospectively assessed a panel of candidate markers to determine the time course for inflammation and the association of specific markers with clinical outcomes defined as intensive care unit length of stay. We obtained pre-operative blood samples from 71 neonates undergoing surgery with CPB and then serially for 5 days following surgery. Numerous interleukins were assayed along with TNF-⊠ and INF gamma. Diagnoses included transposition of the great arteries n=14, hypoplastic left heart syndrome n= 15, 42, other single ventricle defects n= 24, & other two ventricle defects n= 18. Multivariate analysis was performed to determine if inflammatory mediators could independently predict length of stay. Compared to the pre-surgery level, there are statistically significant increases (P < 0.005) at day 1 for six markers: IL 10, IL 13, IL 8, INF gamma, TNF alpha, and IL 6. At 3 days post-op all markers had returned to pre-surgery levels except Il-6 and IL-8, which remained elevated. No marker on the first pre-operative day was independently associated with length of stay. However, IL-8obtained on day 3 following surgery was significantly associated with a prolonged ICU length of stay (p<.001) after adjusting for other covariates. In summary, neonatal heart surgery for complex lesions elicits a broad inflammatory response. This early inflammatory response appears non-specific and does not predict clinical course. Persistence of specific inflammatory mediators such as IL-8 on the 3rd day of surgery, however, provides important prognostic information. As such, IL-8 may serve as a biomarker in this population. Whether strategies targeting specific cytokines can alter clinical course is not known.
ELEVATED LEVELS OF ET-1 IN PULMONARY CIRCULATION AFTER THE FONTAN PROCEDURE
Author links open overlay panelKazuyoshiSaitoKazuhiroWatanabeSayakaOzawaKeiichiHironoNaokiYoshimuraDirkFoellFukikoIchida
University of Toyama, Toyama, Japan
Background
Endothelin-1 (ET-1) is one of the most potent vasoconstrictors produced from various organs and might be involved in many cardiovascular conditions. As far as we know there are no reports about serum levels of ET-1 in pulmonary arteries after the Fontan procedure.
Methods
Study subjects were divided into three groups: 1) Fontan group (11 cases): patients one year-after the Fontan procedure, 2) Glenn group (15 cases): post-operative Glenn procedure patients, 3) Biventricular repair (BVR) group (39 cases): patients who underwent post-operative biventricular repair for congenital heart defects. We assessed various cardiovascular parameters and collected 2-3mls of whole blood samples from the pulmonary artery at the time of post-operative cardiac catheterization. Serum levels of ET-1 were measured using an enzyme-linked immnosorbent assay (ELISA).
Results
1) Concentration of ET-1: The mean serum levels of ET-1 in the Fontan group was significantly higher than in the Glenn (p<0.05) and BVR groups (p<0.01): Fontan group: 1.72+/-1.21, Glenn group: 1.10+/-0.574, BVR group: 0.853+/-0.528 (pg/ml). 2) Hemodynamics of the Fontan group: Serum levels of ET-1 in the Fontan patients were strongly correlated with mean pulmonary artery pressure (mean PAP) (r=0.7797) and ventricular ejection fraction (EF) (r=0.7603).
Conclusions
We report for the first time that patients have elevated levels of ET-1 in the pulmonary circulation after the Fontan procedure and that these are significantly higher than in the Glenn and BVR group patients. Further, the serum levels of ET-1 in the Fontan group patients were strongly correlated with mean PAP and EF, which might indicate that ET-1 in the pulmonary artery influences hemodynamics after the Fontan procedure.
IS SYSTEMIC RIGHT VENTRICULAR FUNCTION BY CARDIAC MRI RELATED TO THE DEGREE OF TRICUSPID REGURGITATION IN CONGENITALLY CORRECTED TRANSPOSITION OF THE GREAT ARTERIES?
Author links open overlay panelMatthew J.LewisJonathanGinnsMarlonRosenbaum
Columbia University, New York, NY, USA
New York Presbyterian Hospital, New York, NY, USA
Background
Patients with congenitally corrected transposition of the great arteries (CCTGA) often develop systemic right ventricular (SRV) dysfunction and systemic tricuspid regurgitation(TR). Studies using echocardiography have suggested a relationship between the degree of TR and SRV dysfunction. However, the geometry of the SRV limits the quantitative assessment of the SRV by echocardiography. Cardiac MRI (CMR) has become the gold standard for volumetric assessment of the SRV. We sought to determine whether there is a relationship between degree of TR and SRV function by CMR.
Methods
We performed a retrospective cohort study evaluating all patients (age ≥18 years) with CCTGA seen at our Adult Congenital Heart Disease Center who underwent CMR between 1/1999 and 11/2012. Patients with tricuspid valve surgery prior to CMR were excluded. TR was quantified by transthoracic echocardiography. A blinded reader reviewed ventricular size, function and mass by CMR for each patient.
Results
Of the 30 patients (37% male), 11 had ≤mild TR (37%) and 19 had ≥moderate TR (63%). Mean age at CMR was 38 years (23-64) and 11 (37%) had associated congenital lesions. Mean SRV ejection fraction for patients with ≥ moderate TR was not significantly different than patients with ≤mild TR (45% vs. 42%, p=0.34). Mean indexed right ventricular end diastolic volume was also not significantly different (128 ml/m2 vs. 130 ml/m2, p = 0.85). Patients with ≥moderate TR were more likely to report dyspnea (46% vs. 0%, p=0.02). However, ≥ moderate TR was not associated with additional congenital lesions, arrhythmiasor decreased left ventricular function by CMR.
Conclusions
In our cohort of patients with CCTGA there was no association between degree of TR and SRV volume or ejection fraction by CMR. Failure to show worsening SRV function or increased volume with greater degrees of TR suggests that degree of TR alone may not fully explain the heterogeneity in SRV function amongst patients with CCTGA.
BACTERIAL ENDOCARDITIS IN PATIENTS WITH ADULT CONGENITAL HEART DISEASE: THE IMPACT OF LESION TYPE AND RECENT VALVE REPLACEMENT SURGERY
Author links open overlay panelDarrenMylotteDinelaRushaniLimingGuoMohammedKaouacheKennethGuoJudithTherrienGiuseppeMartucciAndrewMackieArianeMarelli
McGill Adult Unit for Congenital Heart Disease Excellence, McGill Health Centre, Montreal, Canada
Background
Congenital heart disease (CHD) confers an increased risk of infective endocarditis (IE), though the lesion-specific risk is poorly defined. Furthermore, the contribution of recent valve replacement surgery to IE-risk is unknown.
Methods
We used the Quebec CHD database to extract clinical data on adult CHD patients (18-65 years) diagnosed with IE. Patients were classified according to CHD lesion as follows: cyanotic (tetralogy of Fallot, univentricular heart, complete transposition, truncus arteriosus, hypoplastic left heart); endocardial cushion defects; left-sided (coarctation of the aorta, aortic and mitral stenosis/insufficiency); right-sided (Ebstein anomaly, anomalies of the pulmonary artery/valve); ventricular septal defect; atrial septal defect; patent ductus arteriosus; and other CHD (other or unspecified congenital anomalies). A nested case control study was performed and predictors of IE derived using a logistic regression model. Valve replacement surgery was deemed to be recent if it was performed within 6 months of IE diagnosis. Death within 30-days of diagnosis defined IE-related mortality.
Results
Among 29,137 patients with CHD, 459 (1.58%) developed IE during a follow-up period of 335,683 patient years. The median age of IE diagnosis was 43.6 years (30.9, 54.1). The highest and lowest lesion-specific incidences of IE were observed in patients with left sided lesions (2.89% per 1000 patient years) and patent ductus arteriosus (0.3% per 1000 patient years), respectively. Predictors of IE included: male gender [odds ratio (OR) 1.9: 95% confidence interval (CI) 1.5-2.3; p<0.0001], cyanosis (OR 2.7: 95% CI 1.9-4.0, p<0.0001) and left-sided (OR 3.4: 95% CI 2.6-4.6;p<0.0001) lesions, ventricular septal defect (OR 1.7: 95% CI 1.2-2.4;p=0.002) and recent valve replacement surgery (OR 5.7: 95% CI 2.6-12.5;p<0.0001). Right-sided lesions were not associated with IE (OR 0.9: 95% CI 0.5-1.9;p=0.9). IE-related mortality occurred in 26 patients
(5.7%).
Conclusion
The risk of IE in CHD patients is lesion specific and is greatest in the context of recent valve replacement surgery. Efforts to reduce IE in the CHD population should focus on these high-risk patient groups.
RESECTION OF RIGHT VENTRICULAR OUTFLOW TRACT PATCH DURING PULMONARY VALVE REPLACEMENT IMPROVES RIGHT VENTRICULAR VOLUMES AND EJECTION FRACTION IN PATIENTS WITH TETRALOGY OF FALLOT
Author links open overlay panelDaniel S.O’ConnorJonathanGinnsJanQuaegebeurEmileBachaMarlonRosenbaum
Columbia University Medical Center, New York, NY, USA
Background
Right ventricular (RV) dilatation following Tetralogy of Fallot (ToF) repair is due to both pulmonary regurgitation and the size of the right ventricular outflow tract (RVOT) patch. Recent studies have shown a 28-36% decrease in RV volume following pulmonary valvereplacement (PVR) but no change in RV ejection fraction at one year of follow up. The contribution of the RVOT patch on post-PVR ejection fraction and the role of surgical remodeling during PVR remain controversial. We sought to evaluate the effect of aggressive RVOT patch and scar resection during insertion of a bioprosthetic PVR on RV size and function using cardiac magnetic resonance imaging (MRI).
Methods
Fifty-three ToF patients with chronic pulmonary regurgitation and RV dilatation seen at our adult congenital heart center underwent bioprosthetic PVR from 2001 through 2010. Of those patients, 21 had a cardiac MRI performed both before and after PVR. The operative note was reviewed and 12 patients were identified in whom concomitant resection of the RVOT patch and scar were performed while the remaining 9 patients underwent isolated PVR. MRI volumes and EF were assessed for both groups.
Results
A cardiac MRI was performed 0.87 +/- 0.60 years prior to PVR and 3.1 +/- 2.2 years following PVR on average for both surgical groups. In the PVR and RVOT resection group, RVEDVI and RVESVI decreased substantially following surgery (185cc/m^2 vs. 112cc/m^2; p = 0.013 and 131cc/m^2 vs. 60cc/m^2; p = 0.002) and the RVEF improved dramatically (39% vs. 46%; p < 0.013). In the isolated surgical PVR, RVEDVI and RVESI also improved following surgery (186cc/m^2 vs. 117cc/m^2; p<0.0001 and 102cc/m^2 vs. 71cc/m^2; p=0.006, respectively). RVEF did not change is this surgical group (46% vs. 41%; p=0.057).
Conclusions
Aggressive RVOT resection during pulmonary valve replacement in ToF patients with severely enlarged right ventricles leads to dramatic improvements in RV volumes and EF. The improvement in RVEF differs from prior studies and may be explained by the extensive resection of all non-contracting RV outflow tract tissue as well as late improvement in RVEF post PVR. Whether this approach should be adopted during PVR warrants further study.
ARE LONG-TERM CONSEQUENCES OF PULMONIC REGURGITATION FROM VALVOTOMY SIMILAR TO TETRALOGY OF FALLOT?
Author links open overlay panelMichaelZdradzinskiAtharQureshiRobertStewartGostaPetterssonRichardKrasuski
The Cleveland Clinic, Cleveland, OH, USA
Background
Patients with tetralogy of Fallot (TOF) following complete repair and pulmonic stenosis (PS) after surgical valvotomy often develop significant pulmonic regurgitation (PR) that eventually requires valve replacement (PVR). Though several criteria exist for the timing of PVR in TOF, it is less clear when to intervene in valvotomy patients and whether TOF recommendations can be applied.
Methods
We compared the clinical characteristics, electrocardiograms, imaging studies and invasive hemodynamics of 109 patients (34 PS and 75 TOF) newly referred to a large congenital heart disease clinic for evaluation of PR between 2005 and 2011. Patients with prior PVR or conduit implantation and those with > mild right ventricular outflow narrowing were excluded. Valvular regurgitation was graded echocardiographically from 1 (mild) to 4 (severe). ECG analysis was limited to nonpaced tracings.
Results
The two cohorts were similar in terms of baseline demographics and comorbidities as well as presenting NYHA function class. Time interval from surgery to referral was longer in valvotomy patients (37±10 vs. 32±11 years, p=0.022) and degree of PR was greater by echocardiography (3.2±0.9 vs. 2.4 ±1.6, p=0.004). ECG showed considerably greater QRS width in TOF (150±28 vs. 114±27ms, p<0.001). Echo pulmonary valve gradient was greater for TOF (14±8 vs. 8±3 mm Hg, p<0.001). MRI Right ventricular (RV) ejection fraction (41±11 vs. 49±8%, p=0.001) and left ventricular (LV) ejection fraction (52±10 vs. 59±7%, p=0.002) were considerably lower in TOF. Invasive hemodynamics revealed similar pulmonary artery pressure, right atrial pressure and cardiac index for both groups. 22.1% of the TOF cohort required pacemaker or ICD implantation compared to 2.8% of the valvotomy patients (p=0.011).
Conclusions
Though presenting later than TOF after classic repair, PS valvotomy patients have greater degrees of regurgitation. RV/LV function and QRS width appear less affected, suggesting changes in TOF patients that go beyond the effects of PR. This suggests a need for disease-specific guidelines for intervention in PS valvotomy patients.
FEEDING DYSFUNCTION IS ASSOCIATED WITH GROWTH FAILURE IN PRESCHOOL-AGED SINGLE VENTRICLE PATIENTS
Author links open overlay panelGarickHillAlanSilvermanRichardNoelJulieSlickerAnnScottPeterBartz
Children’s Hospital of Wisconsin, Milwaukee, WI, USA
Medical College of Wisconsin, Milwaukee, WI, USA
Background
Feeding and growth problems present early in infants with single ventricle defects but often remain suboptimal during childhood despite surgical palliation. Maladaptive mealtime behaviors or interactions, known as feeding dysfunction, may contribute to these feeding problems. We sought to determine the prevalence of feeding dysfunction in children with single ventricle defects, identify associated risk factors and determine whether feeding dysfunction is associated with poor growth.
Methods
Patients aged 2-6 years with single ventricle defects presenting to Children’s Hospital of Wisconsin for routine cardiology follow-up were prospectively identified. All patients had completed stage II or stage Ill palliation. Parents of the patients completed 2 validated instruments for assessment of feeding dysfunction; the Mealtime Behavior Questionnaire and the About Your Child’s Eating questionnaire. Demographic and diagnostic data were collected retrospectively from chart review.
Results
Instruments were completed for 56 patients; median age was 39 months. Twenty three (41%) patients had a history of gastrostomy (G) tube placement with 12 requiring current G tube use for at least partial nutritional support. Overall, 28 (50%) patients had some form of feeding dysfunction. Compared to a normal reference population, single ventricle patients had statistically-significant differences in food manipulation (p<0.001), mealtime aggression (p=0.002), choking/gagging/vomiting (p<0.001), resistance to eating (p<0.001) and parental aversion to mealtime (p<0.001). Weight and height for age z-scores were significantly lower in subjects with feeding dysfunction (−0.84 vs. −0.33; p=0.049 and −1.46 vs. −0.56; p=0.001 for weight and height respectively). Current G tube use was the only risk factor identified for feeding dysfunction.
Conclusions
Feeding dysfunction is common in children with single ventricle defects, occurring in 50% of 2-6 year-olds in our cohort. Feeding dysfunction was associated with worse growth parameters. Current G tube use was associated with presence of feeding dysfunction. Outcomes may be improved with early identification of feeding dysfunction.
ASSESSMENT OF THE LIVER IN PATIENTS WITH FONTAN PHYSIOLOGY USING ULTRASONIC SHEAR WAVE ELASTOGRAPHY
Author links open overlay panelShaijaShelbyQinghaiPengRallynRennerLingLiCynthiaScottMarionMeckelburgScott E.FletcherJohnKuglerKim F.DuncanRuben E.Quiros-TejeiraDavid A.DanfordShelbyKutty
University of Nebraska/Children’s Hospital and Medical Center, Omaha, NE, USA
SuperSonic Imagine, Bothell, WA, USA
Background
Liver dysfunction is a recognized complication with the Fontan physiology. We sought to evaluate quantitative ultrasonic measurement of liver stiffness in a Fontan cohort using shear wave elastography (SWE).
Methods
Patients and age-matched controls were prospectively recruited for same day 2D echocardiography and duplex liver ultrasound with SWE. The SWE ultrasound system (SuperSonic Imagine Aixplorer®) and selected transducers (SC6-1, SL15-4) enabled generation of transient shear waves simultaneously with real-time B-mode imaging. Using a Q-box™ plug-in with OsiriX software, stiffness measurements were expressed in terms of Young’s Modulus (kPa). Duplex measurements were made in the celiac and superior mesenteric arteries, and the main portal vein (MPV). These were peak velocities, velocity time integral (VTI), resistive, pulsatility and acceleration indices (RI, PI, AI), MPV flow volume, and MPV and right liver lobe diameters. Comparisons were made with controls and correlations explored between SWE, Duplex and clinical data.
Results
Twenty-seven patients (18 male, 9 female, age 14 ±6 yrs, time since Fontan 11±6 yrs, weight 44±24 kg) and 29 controls (14 male, 15 female, age 14.5±7 yrs, weight 53±20 kg) were studied. It was feasible to obtain measurements in all subjects. Patients had significantly higher SWE values (15.5 vs. 5.2 kPa, p<0.0001) and superior mesenteric arteryRI (8.8 vs. 8.3, p=0.04), while the MPV flow volume (260 vs. 470 ml/ min in controls, p=0.003) and AI (32 cm/s2 vs. 49 in controls, p=0.01) were lower. AI tended to decrease with time since Fontan (P=0.07), but no significant change was seen in SWE or other Duplex indices with age, gender, time since Fontan, VO2 max or ventricular morphology. MPV flow volume and celiac artery RI and PI correlated inversely with SWE.
Conclusion
Fontan physiology is associated with remarkably abnormal liver stiffness, and changes in hepatic vascular flow patterns. SWE measurements are feasible in young patients and the findings are of great concern, but their value in patient management is not established in this cross sectional study. Longitudinal SWE determinations and correlation with liver biopsy findings are planned.
PLEURAL FLUID ACCUMULATION IN CHILDREN WITH UNIVENTRICULAR CONGENITAL HEART DISEASE: THE APPLICATION OF LIGHT’S CRITERIA AFTER THE GLENN AND FONTAN PALLIATION
Author links open overlay panelEnglishFlackYvonneBernardAnupama G.BrixeyRichard W.LightMonroeCarellJr.
Children’s Hospital at Vanderbilt, Nashville, TN, USA
Background
Postoperative pleural effusions contribute to significant morbidity in patients undergoing single-ventricle palliation. Effusions are often attributed to increased central venous pressure, suggestive of transudates. We analyzed postoperative pleural fluid after cavopulmonary anastomosis operations.
Methods
We prospectively enrolled patients prior to Glenn (n=18) or fenestrated Fontan (n=21). Pleural fluid was collected on predetermined postoperative days for the duration of chest tube placement and analyzed for cell counts, total protein, lactate dehydrogenase, triglycerides, and vascular endothelial growth factor (VEGF). Perioperative hemodynamics, surgical variables, chest tube volume, and output duration were collected and compared among patients with and without persistent chest tube drainage beyond 7 days.
Results
The application of Light’s criteria revealed all pleural fluid samples to be exudates. There was no difference in pleural fluid composition, preoperative oxygen saturation, mean pulmonary artery pressures, or pulmonary vascular resistance in Fontan patients with prolonged effusions compared to Fontan patients with effusions </= 7 days in duration.
Conclusions
Persistent pleural effusions after cavopulmonary anastomosis are exudative in nature. To our knowledge this is the first study to analyze the composition of pleural fluid after these operations and suggests a mechanism other than increased central venous pressure.
Baseline hemodynamics and pleural fluid composition (median and IQR) post Glenn and Fontan operation
| Group | Mean pulmonary artery pressure (range) | Pulmonary vascular resistance (units × m⁁2) | Bypass time (minutes) | LDH (U/L) | Triglycerides (mg/dL) | Total protein (g/dL) | VEGF (pg/ml) |
| Glenn (n=18) | 13 mmHg (7–18) | 1.73 (1.41–2.45) | 82 (62–128) | 1003 (746–2187) | 43 (22–61) | 2.87 (2.20–3.48) | 3171 (2493–3510) |
| Fontan (<7d, n=11) | 10 mmHg (7–15) | 1.87 (1.40–2.71) | 101 (93–124) | 727 (534–1083) | 41 (17–55) | 2.58 (2.28–3.00) | 427 (253–963) |
| Fontan (>7d, n=10) | 11mmHg (7–14) | 1.60 (1.21–2.24) | 119 (82–174) | 673 (329–1343) | 77 (48–133) | 2.80 (2.08–3.40) | 429 (230–725) |
ABNORMALITIES IN BONE DENSITY, BONE STRUCTURE AND MUSCLE CROSS-SECTIONAL AREA AFTER FONTAN PALLIATION
Author links open overlay panelCatherineAvitabileJillBrodskyMary B.LeonardKathrynDoddsChristina H.RushElizabethGoldmuntzJackRychikDavidGoldberg
Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Background
Children with single ventricle (SV) physiology after Fontan have multiple risk factors for impaired bone accrual and abnormal body composition. The impact of this circulation on volumetric bone mineral density (BMD), cortical structure, and muscle cross-sectional area (mCSA) has not been evaluated.
Methods
This was a cross-sectional analysis of children with SV physiology after Fontan. TrabecularBMD, cortical BMD, cortical thickness, cortical periosteal circumference, and lower leg mCSA were assessed by tibial peripheral quantitative computed tomography (pQCT). All values were converted to sex- and race-specific z-scores relative to age based on reference data in >650 healthy participants. Z-scores for cortical structure and mCSA were further adjusted for tibia length.
Results
The cohort consisted of 32 subjects; 30 were able to complete pQCT testing. Median (range) age was 9.3 years (5.1-17.6) at a median interval from Fontan of 6.3 years (1.1-16). Fontan subjects had lower mean height z-scores compared to reference participants (−0.58±0.96 vs. 0.25±0.93; p<0.001). Fontan subjects also had lower z-scores for trabecular BMD (−0.90+0.95 vs. 0.02+1.03, p<0.001), cortical BMD (−0.37+1.00 vs. 0.00+1.00, p=0.046), cortical thickness (−0.60+1.00 vs. 0.00+0.96, p<0.001), cortical periosteal circumference (−0.37+0.78 vs. 0.00+0.83, p=0.016), and mCSA (−0.53+1.03 vs.0.00+0.96, p=0.003). In the Fontan cohort, there was a correlation between lower mCSA z-scores and lower cortical periosteal circumference z-scores (R=0.69, p<0.001). Bone and muscle deficits were not associated with age, Fontan characteristics, or parathyroid hormone levels.
Conclusions
Children with SV physiology after Fontan exhibited growth failure as well as significant deficits in volumetric BMD, cortical structure, and mCSA. There was a strong correlation between mCSA and cortical periosteal deficits. Future studies are needed to determine the metabolic and fracture implications of these deficits, and to identify therapies to promote growth, bone development, and normal muscle accrual in this population.
VENTRICULAR MORPHOLOGY OR FENESTRATION STATUS DOES NOT IMPACT EXERCISE CAPACITY IN FONTAN PATIENTS: A STUDY UTILIZING NEAR INFRARED SPECTROSCOPY
Author links open overlay panelRohit SethLoombaRohitRao
Children’s Hospital of Wisconsin/Medical College of Wisconsin Affiliated Hospitals, Milwaukee, WI, USA
Phoenix Children’s Hospital, Phoenix, AZ, USA
Background
Previous studies have demonstrated that fontan patients have decreased exercise capacity when compared to those with normal cardiovascular anatomy. Differences have also been noted within various subgroups of fontan patients, such as morphology of the single ventricleand whether the fontan conduit is fenestrated or not. This study investigates these trends utilizing noninvasive near infrared spectroscopy. It was hypothesized that those with left ventricular morphology and fenestrated fontans would have better exercise and NIRS profiles.
Methods
50 fontan patients and 51 patients with normal cardiovascular anatomy were recruited for this study. NIRS probes were placed to obtain regional oxygen saturation (rSO2) from the brain and kidney. Readings were obtained at 1 minute intervals during rest, exercise, and recovery. A standard Bruce protocol was utilized with a 5 minute recovery period. Average rSO2 for normal vs fontan patients, fenestrated vs unfenestrated fontans, and morphologic left vs right ventricle fontams were graphed to compare trends. Specific change in rSO2 values from the brain and kidney between rest and peak exercise, rest and 2-minutes into recovery, rest and 5-minutes into recovery were then compared using independent t-tests. Similar analysis was then done with respect to the arterial-venous oxygen saturation difference
Results
When comparing normals to fontans, fontan patients had a statistically significant lower duration of exercise (9.3 minutes versus 13.2 minutes, p <0.001). There was no statistically significant difference in rSO2 change or AVO2 at the aforementioned time points. A small oxygen debt was also paid back to the brain in fontan patients after exercise. When comparing fontan patients with and without fenestration, there was no statistically significant difference in exercise time, rSO2 change, or AVO2 difference. When comparing fontan patients with a morphologic left or right ventricle, there were no statistically significant differences either.
Conclusion
Ventricular morphology and fenestration did not affect exercise duration or NIRS trends in exercising Fontan patients.
PRESSURE VOLUME LOOP ANALYSIS IN PATIENTS WITH SINGLE VENTRICLES: COMPARISON OF PRESSURE-VOLUME LOOP AND NON-INVASIVE MEASURES OF SYSTOLIC FUNCTION
Author links open overlay panelShahryarChowdhuryRyanButtsJasonBuckleyAnthonyHlavacekSachinKhambadkoneTain-YenHsiaG. HamiltonBaker
Medical University of South Carolina, Charleston, SC, USA
Background
Non-invasive measurements of systolic function in the single ventricle population are performed using measures whose accuracy and reliability have not been fully assessed. We sought to validate non-invasive measures of systolic function with invasive measures of systolic function derived from pressure-volume loop (PVL) analysis. We hypothesized that non-invasive measures of systolic function would correlate with PVL indices of systolic function in patients with single ventricle physiology.
Methods
During routine cardiac catheterization, PVLs were recorded using conductance catheters (CD Leycom, Netherlands). PVL indices were calculated using single beat methods to avoid instability from load alterations. PVLs were volume calibrated using cardiac magnetic resonance obtained the same day. Echocardiograms were obtained at the time of catheterization. The relationship between PVL and non-invasive measures of systolic function was determined using a Spearman’s correlation analysis.
Results
Ten patients (7 right ventricular dominant, 3 left ventricular dominant) were enrolled. Median age was 3yr (range 3mo to 19yr). Three were enrolled at stage 1, six at stage 2, and two at stage 3 of surgical palliation. MRI ejection fraction (EF) correlated well with end systolicelastance (Ees) (r = 0.73) and dP/dt max (r = 0.71). The single atrioventricular valve annular plane systolic excursion (SAPSE) correlated well with Ees (r = 0.69). Fractional area change (FAC) correlated well with dP/dt max (r = 0.93) and stroke work/end-diastolic volume (r = 0.65). Myocardial performance index, isovolumic acceleration, and 3D-echo derived EF did not correlate with PVL measures.
Conclusion
This study represents the first-ever validation of systolic echocardiographic indices to invasive PVL indices in a single ventricle population. We demonstrated MRI derived EF and echocardiographic derived FAC and SAPSE showed the best correlation with PVL indices. Our results support the use of these non-invasive measures as accurate indices of systolic function in single ventricle patients. Further validation of noninvasive indices with PVL analysis is warranted in this population.
FACTORS ASSOCIATED WITH SYSTEMIC-PULMONARY ARTERIAL COLLATERAL FLOW IN SINGLE VENTRICLE PATIENTS WITH CAVO-PULMONARY CONNECTIONS
Author links open overlay panelAndrew C.GlatzNeilHarrisonAdamSmallYoavDoriMatthewGillespieMatthewHarrisMarkFogelJonathanRomeKevinWhitehead
Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Background
Systemic-pulmonary arterial collateral flow (CollF) is common in single ventricle pts with cavo-pulmonary connections (CPC), although associations with CollF are not well understood. We previously described a method to quantify CollF by cardiac magnetic resonance imaging (CMR). We sought to identify factors associated with CollF in a large cross-section of patients with CPC.
Methods
A retrospective chart review of events from birth to study CMR was performed for all CPC pts who had CollF quantified. CollF as a % of aortic flow (CollF/Ao) was defined as the primary outcome variable.
Results
CollF measured in 96 superior CPC (SCPC) and 52 total CPC (TCPC) pts at 2.6 ± 1.1 and 4.5 ± 1.8 yrs of age (2.1 ± 1.1 and 1.7 ± 1.6 yrs after last CPC) was 33.5 ± 11.1% and 35.6 ± 14.7% of aortic flow. Significant associations existed between various peri-operative/clinical factors and CollF/Ao (see Table). In SCPC pts, CollF/Ao was higher in pts with a prior BT shunt (35 ± 12 v. 29 ± 8%, p=0.009). CollF/Ao was higher in pts with fenestrated TCPC (37 ± 15 v. 26 ± 12%, p=0.04). A multivariate model with chest tube days, ventilator days after TCPC, 02 sat at SCPC discharge, bypass time at TCPC, heterotaxy, and TCPC fenestration (all p<0.04) accounted for 59% of the variance in CollF/Ao.
Conclusions
These data support hypotheses that perioperative morbidity and pleural inflammation play a role in CollF development; that CollF affects pulmonary blood flow and ventricular volumeloading; and that CollF may affect outcomes after TCPC.
Factors Associated with CollF/Ao in Cavo-Pulmonary Connection Patients
Factors Associated with CollF/Ao in Cavo-Pulmonary Connection Patients
| SCPC cohort (n=96) | TCPC cohort (n=52) | |||||||
| Risk factor | Median/Mean | Range/SD | rho | p | Median/Mean | Range/SD | rho | p |
| Total ICU duration (days) | 17.5 | 2–261 | 0.29 | 0.008 | 22 | 6–154 | 0.44 | 0.003 |
| Total hospital duration (days) | 33.5 | 5–342 | 0.33 | 0.002 | 39 | 16–180 | 0.55 | 0.0001 |
| Total chest tube duration (days) | 3 | 0–54 | 0.24 | 0.02 | 8 | 2–84 | 0.34 | 0.02 |
| TCPC ventilator days | 0 | 0–109 | 0.4 | 0.004 | ||||
| Total ventilator days | 2 | 0–144 | 0.29 | 0.008 | 3.5 | 0–117 | 0.29 | 0.05 |
| 02 saturation at SCPC discharge (%) | 80.8 | 3.75 | 0.19 | 0.06 | 80.7 | 4 | 0.31 | 0.03 |
| End-diastolic volume (cc/m2) | 92.2 | 31.5 | 0.2 | 0.046 | 80.5 | 20.1 | 0.41 | 0.04 |
| Cardiopulmonary bypass time at TCPC (min) | 74.6 | 25.5 | 0.35 | 0.01 | ||||
A RETROSPECTIVE COHORT OF 100 FONTAN CONNECTIONS: RELATIONSHIP BETWEEN GEOMETRIC FEATURES AND HEMODYNAMICS OUTCOMES
Author links open overlay panelElaineTangMariaRestrepoChristopherHaggertyLuciaMirabellaKevinWhiteheadJamesBethelMarkFogelAjitYoganathan
Georgia Institute of Technology, Atlanta, GA, USA
Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Background
Fontan connections have complex and patient specific anatomies. Their geometric features can impact the hemodynamic outcomes, such as (1) connection power loss (PL), which has been shown to be related to patient exercise capacity; and (2) unbalanced hepatic flow distribution (HFD) which has been related to an increased risk of pulmonary arteriovenous malformations. In this study, a large-scale anatomic characterization of Fontan connections is performed, and results were correlated with the hemodynamic outcomes.
Methods
100 patient-specific Fontan anatomies were reconstructed from axial cardiac magnetic resonance images. Geometrical parameters analyzed included: vessel diameter, shape factor (minimum / maximum diameter), angles between connecting vessels and caval offset (distance between the superior vena cava and the Fontan pathway (FP)). Computational fluid dynamics simulations were carried out using time-averaged flow boundary conditions (obtained from phase contrast magnetic resonance images) to quantify the resulting PL and HFD. Multiple regressions between the hemodynamic endpoints and the geometric parameters were investigated. P < 0.05 was considered significant.
Results
The connection PL correlated negatively with minimum pulmonary artery (PA) diameter and minimum FP diameter (p < 0.001). Cardiac index was found to have positive significant correlations with FP shape factor (p = 0.004). From multiple regression, it was found that HFD correlated with caval offset (p < 0.001), pulmonary flow distribution (p < 0.001), connection angles (p < 0.001), and PA diameters (p < 0.015).
Conclusions
The dependence of connection PL on minimum PA and FP diameters suggests it is important to correct vessel stenosis at the connection, especially at the FP which can influence cardiac index. Also, caval offset, PA diameters and connection angles together can impact HFD. The knowledge obtained can be useful to design interventional strategies to improve connection hemodynamics in prospective cases.
INCREASED POWER LOSS IN THE TOTAL CAVOPULMONARY CONNECTION IS RELATED TO DECREASED SINGLE VENTRICLE VOLUME
Author links open overlay panelChristopher M.HaggertyLuciaMirabellaJamesBethelKevinWhiteheadMarkFogelAjitYoganathan
Georgia Institute of Technology, Atlanta, GA, USA
Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Background
Single ventricle (SV) lesions are associated with gradual attrition following surgical palliation with the total cavopulmonary connection (TCPC). Abnormalities in ventricular function are frequently noted, particularly diastolic function. We hypothesize that TCPC hemodynamicenergy losses are adversely related to ventricular filling and volumes.
Methods
Cardiac magnetic resonance (CMR) data were retrospectively analyzed for 40 patients. Cine ventricular short axis scans were semi-automatically segmented for all cardiac phases. Ventricular volumes, peak filling rate (PFR), peak ejection rate, and time to PFR were calculated. TCPC geometry was acquired from an axial CMR image stack; relevant flow rates were taken from phase velocity CMR data. TCPC indexed power loss (iPL) was calculated from computational fluid dynamics simulations. Pearson correlations were used to detect relationships between variables, with p<0.05 considered significant.
Results
The Table provides mean results and variable correlates with iPL. End diastolic and end systolic volumes had significant negative correlations with the natural log of iPL; a similar trend for stroke volume was observed. iPL also had a significant relationship to time to PFR (normalized to cycle time).
Conclusions
Indexed TCPC power loss is inversely related with ventricular volumes, particularly end diastolic. High iPL may contribute to diastolic dysfunction and limited preload reserve in SV.
| Parameter | Mean ± SD | Correlation (R) | p-value |
| iPL | 0.040 ± 0.028 | N/A | N/A |
| Age [years] | 13.0 ± 5.0 | 0.15 | NS |
| Body Surface Area [m2] | 1.36 ± 0.42 | 0.25 | 0.11 |
| Cardiac Index [L/min/m2] | 3.1 ± 0.8 | −0.09 | NS |
| Systemic vein flow [L/min/m2] | 2.9 ± 0.8 | −0.21 | 0.20 |
| End Diastolic Volume [mL/m2] | 77 ± 16 | −0.43*† | 0.005 |
| End Systolic Volume [mL/m2] | 35 ± 11 | −0.36*† | 0.023 |
| Stroke Volume [mL/m2] | 42 ± 10 | −0.31† | 0.054 |
| Ejection Fraction [%] | 55 ± 9 | 0.125 | NS |
| Peak Ejection Rate [EDV/s] | 2.9 ± 0.6 | 0.20 | NS |
| PFR [EDV/s] | 2.7 ± 0.7 | −0.10 | NS |
| Time ratio to PFR | 0.20 ± 0.06 | 0.32* | 0.044 |
| Heart Rate [bpm] | 75 ± 16 | 0.11 | NS |
*
p<0.05
†
Correlation with ln(iPL)
THREE-DIMENSIONAL ECHOCARDIOGRAPHIC ASSESSMENT OF THE LONGITUDINAL TRICUSPID VALVE CHANGES ASSOCIATED WITH TRICUSPID REGURGITATION IN HYPOPLASTIC LEFT HEART SYNDROME
Author links open overlay panelTimothyColenShelbyKuttyRichardThompsonChodchanokVijarnsornJeffrey F.SmallhornNee S.Khoo
University of Alberta, Edmonton, Canada, USA
Children’s Hospital and Medical Center, Omaha, NE, USA
Background
Increasing tricuspid regurgitation (TR) is an important risk factor for morbidity and mortality in children with hypoplastic left heart syndrome (HLHS). We have previously identified an association between TV tethering at pre-stage 1 surgical procedure and later TR in HLHS. Leaflet adaptation to tethering forces by leaflet expansion has been demonstrated in animal studies. We hypothesized that TV adaptation to TV tethering and chronic volume load would affect development of TR between stage 1 and stage 2 surgical palliation.
Methods
Infants with HLHS were assessed pre-stage 1 and pre-stage 2 surgical procedures. Two-dimensional echocardiography was used to measure RV fractional area change (FAC), RV sphericity index (SI), RV end-diastolic area (RVEDa – indexed to BSA) and the degree of TR. Three-dimensional echocardiography was used to extract {x, y, z} spatial coordinates to calculate TV leaflet and annulus area, TV tethering and prolapse volumes. Patients were divided into 2 groups, based on degree of TR pre-stage 2, for comparison at each surgical stage, as well as longitudinally between stages.
Results
Of 21 infants, 8 had moderate TR pre-stage 2 (group A) and 13 had mild TR (group B). Each group had similar findings pre-stage 1 with no difference in RV size, function or shape, or in TV size and tethering parameters. On longitudinal assessment from stage 1 to stage 2, both groups showed progressive increase in TV leaflet and annulus area, TV tethering volume, with no change in indexed RV size, FAC or SI. However, at pre-stage 2, group A had larger TV leaflet area (11.1 vs. 9.8 cm2/m2; P=0.05), annulus area (10.3 vs. 8.7 cm2/m2; P<0.05) and perimeter (21.5 vs. 19.4 cm/m2; P=0.09), compared to group B with no significant difference in RV size, shape or function. In Group A TV prolapse volume was also greater (0.10 vs. 0.02 mL/m2; P<0.05) whilst tethering volume was no different
Conclusion
Patients who developed significant TR at pre-stage 2 had an exaggerated increase in TV annulus and leaflet size as well as progressive increase in leaflet prolapse. The potential role of TV maladaptation to early tethering forces in the development of TR in HLHS warrants further investigation.
A COMPARATIVE STUDY OF CARDI-O-FIX SEPTAL OCCLUDER VERSUS AMPLATZER SEPTAL OCCLUDER IN PERCUTANEOUS CLOSURE OF SECUNDUM ATRIAL SEPTAL DEFECTS
Author links open overlay panelMehmetKayaTurkaySaritasYat YinLamAhmetCelebi
Erciyes University School of Medicine, Kayseri, Turkey
Background
We sought to investigate the safety and efficacy of Cardio-O-Fix septal occluder (CSO) in percutaneous closure of atrial septal defects (ASD) as compared to the Amplatzer septal occluder (ASO).
Methods
A consecutive of 351 patients received transcatheter ASD closure with CSO or ASO from July 2004 to October 2010 were studied. The ASDs were divided into simple- (isolated defects<26mm) or complex-types (isolated defect ≥26mm, double or multi-fenestrated defects). The procedures were guided by fluoroscopy and transthoracic or transesophageal echocardiography. Clinical and echocardiographic follow-ups were arranged before discharge, at 1 month and then every 6-month after implantation.
Results
During the study period, 185 (125 males, aged 18.5±15.6 years) and 166 (103 males, aged 21.0±15.7 years) patients attempted CSO and ASO implants, respectively. The CSO group had similar ASD and device sizes, prevalence of complex lesions (17 vs. 16%, p=0.796), procedural times and success rates (97 vs. 96%, p=0.635) as compared to the ASO group. Acute residual shunts were less prevalent in CSO than ASO group and most shunts closed spontaneously at 6-month follow-ups. The average equipment cost per patient was lower in CSO group (US$ 4,100 vs. US$ 5,900, p<0.001). The prevalence of device embolization and atrial arrhythmia (all <2%) were similar in both patient groups.
Conclusion
Transcatheter ASD occlusion with CSO is safe and effective and it appeared to be an attractive alternative to ASO in closing simple-type ASD because of its relatively low cost.
INFLAMMATORY RESPONSE OF BIODEGRADABLE STENTS IN THE DUCTUS ARTERIOSUS IN A NEONATAL PIGLET MODEL
Author links open overlay panelHolly C.DeSenaSurendranath VeeramReddyTre’WelchJianWangJamesRichardsonJosephForbessAlanNugent
UT Southwestern, Dallas, TX, USA
Background
The ductus arteriosus (DA) closes at birth from vasoconstriction and neo-intimal formation. Maintaining a patent DA with a stent is a strategy in congenital heart disease. Metal/nitinol stents in human DA have significant restenosis. DA constriction may influence stent integrity. Data on biodegradable (BD) stent inflammatory response and performance in DA is lacking and this is evaluated using a BD poly-L-lactic acid (PLLA) stent in piglet DA.
Methods
A pregnant sow delivered 7 newborn piglets (1.5-2.68 kg) and they underwent catheterization via the right neck at age 4-12 hours. An angiogram in the descending aortanoted ductal patency. Via a venous line a PLLA stent was delivered to the DA. Aspirin was administered, and at 2 weeks repeat angiography and histology were performed.
Results
The procedure was challenging with 1 DA patent. All DA were crossed with a 0.014” wire and pre-dilated with a 3mm balloon. The stent length complicated delivery but in 4/7 successful placement of 2.5-4.0mm diameter; 15-20mm length was achieved. At 2 weeks (4.8-6.93 kg) repeat angiography revealed all DA were occluded. Histology showed mid portion patency with collapse at the aortic and pulmonary ends. There was mild inflammation with marked smooth muscle proliferation.
Conclusions
The unique characteristics of DA have important implications for BD stent design. The inflammatory response is analogous to metal/ nitinol. Future studies with increased radial strength at proximal and distal ends are planned.
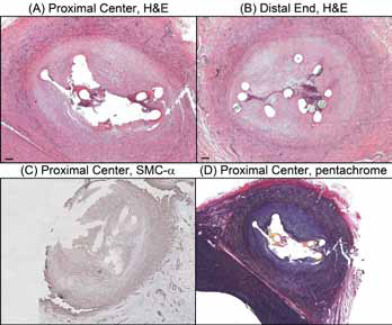
SUCCESFUL TRANSCATHETER THERAPY IN PARTIAL ABNORMAL PULMONARY VENOUS RETURN WITH ADDITIONAL SUPPLY TO LEFT ATRIUM
Author links open overlay panelAlainFraisseDeboraLucianoDanielaLauxJean-ReneLussonSebastienHascoetPascalAmedroCarolineOvaertYounesBoudjemline
La Timone Children’s Hospital, Marseille, France
Necker-Enfants-Malades, Paris, France
Background
Our aim was to report clinical presentation, diagnosis and feasibility of transcatheter therapyin patients with partial abnormal pulmonary venous return (PAPVR) and an additional connection to the left atrium (LA).
Methods
Since 2001, 10 patients(7 girls) from 5 institutions were diagnosed at a median age of 35(1 to 55) years old. Two had a Scimitar syndrome with an additional venous connection of the scimitar vein to the LA whereas 8 had a vertical vein connecting to the left upper pulmonary vein and to the LA. Two patients had an additional aortic coarctation and a secundum atrial septal defect was associated in 3 other cases.
Results
Three patients presented with symptoms whereas there were echocardiographic signs of right ventricle overload in 4 other cases. Diagnosis was confirmed by computed tomodensitometry and cardiac catheterization. Pulmonary artery pressure was normal in all the cases. In 2 patients, transcatheter occlusion of the 2 scimitar veins was successfully performed near their connection to the inferior vena cava with Amplatzer devices, associated with coil-occlusion of anomalous systemic arterial supply. In the other cases, the vertical vein was percutaneously occluded with Amplatzer devices in 5 patients, associated with secundum septal defect closure in 2 cases and aortic coarctation stenting in one patient. Surgical ligation of the vertical vein was performed in one patient. The vertical vein could not be occluded percutaneously in one asymptomatic patient with a restrictive connection to the left atrium and one patient with a severely stenotic bicuspid aortic valve is scheduled for surgery with concomitant ligation of the vertical vein.
Conclusions
In rare cases of PAPVR with an additional connection to the LA, transcatheter therapy can be offered as an alternative to surgery in the majority of the patients.
INCIDENCE, DIAGNOSIS AND OUTCOMES OF CORONARY ARTERY COMPRESSION DURING PERCUTANEOUS PULMONARY VALVE IMPLANTATION
Author links open overlay panelAlainFraisseAnassAssaidiSophieMalekzadeh-MilaniMehulPatelJean-BenoitThamboDamienBonnetLaurenceIserinIssamKammacheYounesBoudjemline
La Timone Children’s Hospitals, Marseille, France
Necker-Enfants-Malades, Paris, France
Background
Coronary compression (CC) may occur during percutaneous pulmonary valve implantation (PPVI) and is potentially life threatening when undiagnosed before right-ventricular outflow tract (RVOT) stenting. We sought to evaluate its incidence, diagnosis and outcome.
Methods
All consecutive patients who underwent transcatheter RVOT treatment from May 2008 to December 2011 in 4 institutions were studied. Baseline demographics, diagnosis and outcomes of CC were reviewed with analysis of risk factors.
Results
CC occurred in 6 out of 100 patients(6%) at a median age of 24(13 to 49) years, with RVOTconduit stenosis as the primary lesion in all cases. The initial congenital heart disease was pulmonary atresia-ventricular septal defect(n=3), complex transposition of the great arteries(n=2) and critical aortic stenosis status-post Ross operation(n=1). The RVOT initial median conduit diameter at surgical implantation was 23(17 to 24) mm and conduit types were homograft(n=3), bioprothesis(n=2) and a pericardial patch(n=1). CC was diagnosed by coronary angiogram during balloon dilation of the RVOT in all cases whereas it was suspected on pre-procedure computed tomography (CT-scan) in only 2 cases. Compression occurred on the left main coronary artery in 5 cases and on a single coronary artery in one patient. No risk factor was found but there was a significantly higher incidence of CC in one of the 4th institutions(p=0.04). CC was well-tolerated and resolved after the balloon was deflated in all the cases. No patients underwent RVOT stenting or PPVI. Surgical conduit replacement was electively performed in 3 patients. Two patients with moderate residual RVOT stenosis are followed. One patient with encephalopathy and respiratory insufficiencydied 9 months after catheterization.
Conclusions
CC is efficiently diagnosed by coronary angiogram during balloon dilation in a small proportion of patients undergoing transcatheter interventions on RVOT. Diagnosis by pre procedure CT-scan is not accurate. No specific risk factors exist. Surgical conduit replacement is indicated when balloon dilation fails to improve the RVOT obstruction.
TECHNICAL CHALLENGES OF ATRIAL SEPTAL STENT PLACEMENT IN FETUSES WITH HYPOPLASTIC LEFT HEART SYNDROME AND INTACT ATRIAL SEPTUM
Author links open overlay panelBrian ThomasKalishWayneTworetzkyCarol B.BensonLouiseWilkins-HaugArielleMizrahi-ArnaudDoff B.McElhinneyJames E.LockAudrey C.Marshall
Boston Children’s Hospital, Boston, MA, USA
Brigham and Women’s Hospital, Boston, MA, USA
Background
Infants born with hypoplastic left heart syndrome and an intact atrial septum (HLHS/IAS) are at high risk for neonatal death, despite maximal postnatal therapy. Prenatal atrial septoplastyby static balloon dilation has been effective in decompressing the left atrium in utero, but several factors have limited the size of septal defects. We attempted to overcome the limitations of balloon septoplasty using transcatheter atrial septal stents.
Methods
The records of the Boston Children’s Hospital/Brigham and Women’s Hospital Fetal Intervention Program were reviewed to identify all fetuses that presented with a diagnosis of HLHS/IAS or severe mitral regurgitation and underwent attempted atrial stent placement.
Results
Nine fetuses between 24 and 31 weeks gestation with HLHS/IAS underwent attempted fetal atrial septal stent placement. A stent was deployed across the atrial septum in five fetuses, with four fetuses demonstrating flow across the stent at the time of intervention. In four cases, stent placement failed due to malposition or embolization, but in three of the four cases, atrial balloon septoplasty at the same in-utero procedure successfully and acutely decompressed the left atrium. There were no maternal complications. There was one fetal demise. The remaining 8 fetuses survived to delivery, but four died in the neonatal period (2 of which had been stented).
Conclusions
Ultrasound-guided atrial septal stent placement is feasible in some fetuses with HLHS/IAS. Visualization of the septum and catheter tip are critical to technical success. Additional experience is necessary to determine the clinical impact of this intervention.
TRANSCATHETER CLOSURE OF SECUNDUM ATRIAL SEPTAL DEFECT WITH DEFICIENT RIMS OTHER THAN THE ANTERO SUPERIOR USING AMPLATZER DEVICES
Author links open overlay panelAlainFraisseAnassAssaidiIssamKammacheJulienManciniPhlippeAldebertDeboraLucianoCarolineOvaertNicolasMichelGilbertHabib
La Timone Children’s Hospital, Marseille, France
Background
We aimed to assess transcatheter closure for secundum atrial septal defect (ASD) with deficient rims(<5 mm), other than the anterior-superior since it is well demonstrated that deficiency in the rim toward the aorta does not influence the success rate for transcatheter closure.
Methods
Between January 1st, 2008 and october 31, 2012, 236 patients underwent percutaneousclosure of ASD in our institution under transesophageal echocardiography guidance in children and intracardiac echocardiography in adults. We retrospectively analyzed the outcomes of the 48 patients(20%, 29 children) with one or more deficient rim other than the anterior-superior.
Results
The median age and weight were 14(1.1-85) years and 35(8.8-99) Kg, respectively. The deficient rim was the inferior(toward the atrioventricular valves) in 11, the inferior- posterior(toward the inferior vena cava) in 18, the superior-posterior(toward the superior vena cava) in 18, and the posterior (toward the pulmonary veins) in 5 cases. Four out of 48 patients had multiple rim deficiency. Transcatheter closure was successfully performed in 42(87%) cases with a median Amplatzer Septal Occluder device size of 28(10 to 40) mm. A modified method of implantation(sizing balloon technique) was used in 39 patients(81%). In 6 patients(5 children) the ASD could not be closed. Four other children(8%) experienced device embolization few hours after transcatheter closure and underwent surgical ASD closure without further complication. By Fisher’s exact test, deficiency of the inferior-posterior rim was associated with failure or embolization(P = 0.003) and there was a trend for children to be associated with embolization or failure(p= 0.065).
Conclusions
Transcatheter closure of secundum ASD is safe and effective in the majority of patients with deficient rims with the exception of inferior-posterior rim deficiency.
INTERSTAGE READMISSIONS AFTER THE NORWOOD PROCEDURE: A REPORT FROM THE NATIONAL PEDIATRIC CARDIOLOGY QUALITY IMPROVEMENT COLLABORATIVE
Author links open overlay panelSamuel PaulHankeRobertBeekmanEileenKingLynnDarbieJeffreyAnderson
Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA
Background
The National Pediatric Cardiology Quality Improvement Collaborative (NPC-QIC) captures data regarding interstage (IS) care processes and outcomes after the Norwood operation. The rates of IS hospital readmission, center variation and risk factors for readmission are not known. The purpose of this study was to utilize NPC-QIC data to explore these issues.
Methods
NPC-QIC registry data between 2009 and 2012 were analyzed for all patients who underwent stage 2 palliation or experienced an IS mortality. Outcomes included any IS readmission with length of stay > one day. To adjust for varying IS duration we calculated: 1) IS Readmission Rate (IRR) = Total # readmissions/total # IS days, and 2) IS Readmission Hospitalization Fraction (IHF) = Total # readmitted hospital days/total # IS days. Independent risk factors were evaluated for any readmission, IRR and IHF, and included patient specific factors (e.g. initial palliation) and discharge processes. IRR and IHF were compared using Kruskal-Wallis tests. Chi-square tests were used to compare rates.
Results
Of 344 infants, 190 (55%) had at least one IS readmission. Cyanosis (24.3%) and feeding problems (23.3%) were the most common indication for readmission. IS mortality was 10.4% for patients with no readmissions, and 7.9% for patients with any readmissions (p=0.42).
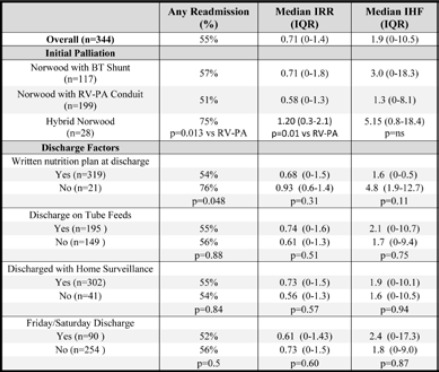
Conclusions
IS Readmissions are frequent. Hybrid stage 1 palliation and absence of a written nutrition plan at discharge are independent risk factors for increased IS readmissions.
EARLY EXTUBATION FOLLOWING INFANT HEART SURGERY
Author links open overlay panelWilliam T.MahleNikhilChananiMichaelWolf
Children’s Healthcare of Atlanta, Emory University, Atlanta, GA, USA
Background
Some institutions have adopted a strategy of early extubation following heart surgery supposing that this approach might improve outcomes. To date, however, the impact of early extubation on patient outcomes is poorly understood.
Methods
We analyzed the 2011 data from the Virtual PICU system, which is a prospective multicenter registry of intensive care admissions. Data regarding post-operative ventilation for complete repair of 4 index cardiac procedures; 1) tetralogy of Fallot (TOF), 2) isolated coarctation of the aorta (coarct), 3) isolated ventricular septal defect (VSD) and 4) transposition of the great arteries (TGA). Early extubation was defined as extubation in the operating room or within 6 hours of admission to ICU. The relationship early extubation and ICU length of stay was analyzed. Results: In 2011 there were 1918 post-operative admission following 4 index procedures (table). In multivariate analysis early extubation was associated with mean reduction in ICU length of stay of 1.5 days (p=.003) Reintubation within 48hrs of early extubation occurred in 1.5% of subjects and did not differ based upon early extubation.
Conclusions
Early extubation following infant heart surgery is associated with a shorter ICU length of stay and no increase in reintubation rates. Efforts to extend this strategy should be considered.
HOSPITAL COSTS FOR PEDIATRIC HEART SURGERY VARY WIDELY ACROSS INSTITUTIONS
Author links open overlay panelSara K.PasqualiXiaHeMarshallJacobsSamirShahEric D.PetersonMatthewHallJ. WilliamGaynorKevin D.HillKarl F.WelkeJohn E.MayerJeffrey P.JacobsJennifer S.Li
University of Michigan, Ann Arbor, MI, USA
Duke University, Durham, NC, USA
Background
Prior studies of hospital costs for pediatric heart surgery relied on administrative data. Linkage with clinical data allows more detailed case ascertainment, risk adjustment, and assessment of complications and outcomes; and may improve our understanding of variation in resource utilization and mediating factors in this era of rising healthcare costs.
Methods
Clinical data from The Society of Thoracic Surgeons Database were linked to cost data from the Pediatric Health Information Systems Database (2006-10). Center variation in hospital costs, adjusted for patient characteristics, was assessed for 9 operations of varying complexity using Bayesian methods.
Results
12,718 operations (27 centers) were included. Costs increased with case complexity (Table). Wide variation between hospitals in adjusted costs was observed across operations, and was greatest for Tetralogy of Fallot repair (9-fold variation). High volume centers had lower costs for the most complex procedures (arterial switch, truncus, Norwood). Hospitals with longer post-op length of stay (LOS) and higher complication rates had higher costs; these variables explained an average of 28% of the variation in cost (range 5-50%).
Conclusions
Hospital costs vary widely across institutions, and are related in part to differences in LOS and complication rates. Further study of the cost-outcome relationship is needed to develop strategies to reduce resource utilization while optimizing patient outcomes.
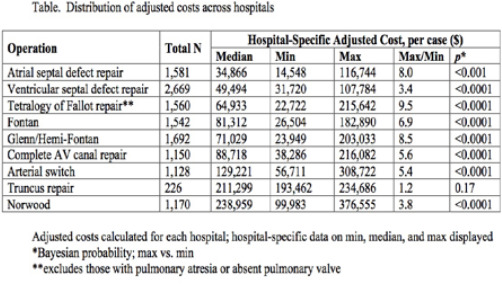
ASSOCIATION BETWEEN TECHNICAL PERFORMANCE SCORES AND NEURO DEVELOPMENTAL OUTCOMES AFTER CONGENITAL CARDIAC SURGERY
Author links open overlay panelMeenaNathanAnjaliSadhwaniKimberleeGauvreauDonnaDonatiJaniceWareAgusMichaelJaneNewburgerFrankPigula
Children’s Hospital Boston, Boston, MA, USA
Background
Technical Performance Score (TPS) has been shown to have a strong association with early and late outcomes after congenital cardiac surgery with higher morbidity and re-intervention in children with TPS of Class 3 (major residual lesions). This study was designed to look at the impact of TPS on neurodevelopmental outcomes (NDO).
Methods
NDO testing at 1 year was offered to families of infants undergoing heart surgery, excluding those with trisomy 21, using Bayley Scale of Infant Development-III-Cognitive, Language and Motor standard scoring. TPS based on discharge echocardiograms are graded as Class 1 (optimal), Class 2 (minor residual) or Class 3 (major residual). Analysis of variance was used to test for association between TPS and NDO.
Results
122 patients underwent NDO testing at median age of 16 months. 21(18%) had single ventricle palliation and 99(82%) had biventricular repair. 32(27%) were in RACHS-1 category 4 to 6. 100 had repair on cardiopulmonary bypass. Table 1summarizes the mean scores across TPS classes with lower scores in class 3. There was no significant difference in NDO scores based on single ventricle or biventricular repair, or RACHS-1 categorization.
Technical Performance Score and Neurodevelopmental Outcomes in Congenital Cardiac Surgery
| TPS | TPS | TPS | ||
| NDO | Class 1 | Class 2 | Class 3 | p value |
| (Mean±SD) n=69 | (Mean±SD) n=34 | (Mean±SD) n=13 | ||
| BSID- Cognitive | 102±17 | 96 ± 17 | 91 ± 18 | p=0.05 |
| BSID- Language | 96 ± 17 | 92 ± 18 | 88 ± 12 | p=0.23 |
| BSID- Motor | 91 ± 15 | 87 ± 18 | 79 ± 19 | p=0.08 |
Conclusion
This data extends the observation that TPS exerts a strong influence on outcomes after congenital heart surgery. Children with significant residual lesions(class3) following repair should be considered at increased risk of ND difficulties and be considered for prompt referral to early intervention programs.
EXTRACARDIAC CONDUIT FONTAN PROCEDURE WITHOUT THE USE OF CARDIOPULMONARY BYPASS: EARLY OUTCOMES
Author links open overlay panelClaudia A.AlgazeV. MohanReddyFrank L.HanleyStanton B.Perry
Stanford University, Palo Alto, CA, USA
Lucile Packard Children’s Hospital, Palo Alto, CA, USA
Background
We compared intensive care unit (ICU) and overall length of stay (LOS), chest tube (CT) duration, days of mechanical ventilation and mortality for non-fenestrated, extracardiac Fontans (NFEF) performed on and off cardiopulmonary bypass (CBP).
Methods
A retrospective review identified 135 patients who underwent NFEF between January 2004 and March 2012. Patients were excluded if they required intracardiac repair which requires CBP. Outcomes were analyzed by adjusted multiple linear regression and propensity scoreweighted regression to reduce bias.
Results
Of the 135 pts, 47 had hypoplastic left heart syndrome, 25 had tricuspid atresia, 16 had atrioventricular septal defect, 15 had double outlet right ventricle, 14 had double inlet left ventricle, 10 had pulmonary atresia with intact ventricular septum, 4 had l-transposition of the great arteries, 2 had d-transposition of the great arteries, and 2 had critical aortic stenosis. CBP was used in 30 patients and avoided in 105 patients. A comparison of adjusted linear regression and propensity score weighted regression results for overall LOS, ICU LOS, days of mechanical ventilation, and CT days is presented in Table 1. Mortality was low in both groups (CBP: 0.07 + 0.05; Off-CBP: 0.01 + 0.01, p =0.06).
Table 1
| Adjusted Linear Regression | Propensity Score Weighted Regression | |||
| Off-Pump Outcome Compared to CBP | p (95% Cl) | Off-Pump Outcome Compared to CBP | p (95% Cl) | |
| Length of Stay | Mean 8 day (+ 3) reduction | p= 0.009 (2 to 14) | Mean 6.4 day (+ 3.4) reduction | p= 0.06 (−.37 to 13) |
| Intensive Care Unit Length of Stay | Mean 2.8 day (+ 1.2) reduction | p= 0.019 (.5 to 5.2) | Mean 2.9 day (+ 1.3) reduction | p= 0.023 (.4 to 5.4) |
| Mechanical Ventilation | Mean 5 day (+ 1.8) reduction | p= 0.008 (1.3 to 8.5) | Mean 4.7 day (+ 2.2) reduction | p= 0.03 (.4 to 9) |
| Chest tube duration | Mean 4 day (+ 2.3) reduction | p= 0.086 (−.56 to 8.42) | Mean 3.7 day (+ 2.2) reduction | p= 0.1 (−.76 to 8) |
Conclusion
The off pump NFEF is associated with significant decreases in ICU and total LOS and in days of mechanical ventilation. Whether this reduction justifies additional surgeries to limit CBP remains unclear.
A PROMPT ARTERIAL SWITCH OPERATION IMPROVES OUTCOMES AND REDUCES COSTS FOR NEONATES WITH TRANSPOSITION OF THE GREAT ARTERIES
Author links open overlay panelBrett R.AndersonAdam J.CiarleglioDenise A.HayesRichardFriedmanEmileBacha
Columbia University/NewYork Presbyterian-Morgan Stanley Children’s Hospital, New York, NY, USA
Background
Arterial switch operation (ASO) is now the standard of care for neonates with dextrotransposition of the great arteries (TGA). With widespread availability of prostaglandins and balloon septostomy, timing of surgery has become largely discretionary. Little is known about the effects of age at operation on either clinical outcomes or costs of management. Our aim was to examine the impact of timing of surgery during the first month of life on major morbidity or mortality and on hospital reimbursement for term infants with uncomplicated TGA.
Methods
We conducted a retrospective cohort study of term infants with simple TGA, with or without ventricular septal defect (VSD), admitted to our institution at < 5 days of age, from Jan 1, 2003 to July 1, 2012. Children with major co-morbid conditions were excluded. Clinical and financial records were obtained, and univariable and multivariable analyses performed to determine the effects of age at operation on major morbidity (arrest, ECMO, delayed sternal closure, systemic infection, necrotizing enterocolitis, seizure, stroke, reoperation and readmission) or mortality and on hospital reimbursement.
Results
141 children met inclusion criteria. One child died preoperatively on day of life zero, while awaiting balloon septostomy. 140 children underwent ASO. Reimbursement data was available for children through Jan 1, 2012 (n = 131). Mortality was 1.4% (n = 2). An additional 24% (n = 33) experienced a major morbidity. Median hospital costs were $61,000 in 2012 dollars ($25,000 – $549,000), with a median length of stay of 13 days (5-122). Median age at operation was 5 days (1-18; 98% at < 12). For every day later that surgery was performed, the odds of major morbidity or mortality increased by 21% (3-43%; P = 0.020) and costs increased by 7% (4-9%; P < 0.001), after considering the effects of inflation, sex, birth weight, date, transfer, weekend admission, insurance, surgeon, balloon septostomy, bypass and cross-clamp times, and the presence of VSD, left ventricular outflow tract or arch obstruction, or abnormal coronary anatomy.
Conclusions
Delay in surgical correction of TGA, with or without VSD, significantly increases morbidity and healthcare costs.
LIFETIME PREVALENCE OF CONGENITAL HEART DISEASE IN THE GENERAL POPULATION IN 2010
Author links open overlay panelMohammedKaouacheRalucaIonescu-IttuAndrewMackieArianeMarelli
McGill Adult Unit for Congenital Heart Disease Excellence, McGill University Health Center, Montreal, Canada
Background
There is a paucity of data to estimate the number of people living with congenital heart disease (CHD) in the general population. The most recent estimates were for the years 2000-2005 when increasing CHD prevalence was documented in adults and children. Our goal was to provide current estimates of life-time CHD prevalence.
Methods
Using a unique identifier assigned at birth, the Quebec CHD database contains 28 years of longitudinal data on all those born with CHD from 1983-2010. The database was created by fusing claims-data from inpatient, outpatient and death registry sources. Published algorithms to identify CHD diagnoses (ICD 9-10) were applied. Severe CHD was defined as tetralogy of Fallot, truncus arteriosus, transposition complexes, endocardial cushion defects, and univentricular hearts. All remaining lesions were classified as other CHD. We used a latent class Bayesian model that combines case definitions from multiple data sources including physician billing, hospitalization and surgical data to obtain point and interval estimates of CHD prevalence.
Results
We identified 108,726 CHD patients from 1983 to 2010. We estimated the prevalence of CHD detected in the first year of life at 8.16 per 1000 live-births (95% CI 7.90, 8.43) from 1998-2005. In 2010, the prevalence estimates in children and adults (95% CI) were 11.85 /1000 (11.43, 12.30) among children and 6.07 /1000 (5.97, 6.17) among adults. The prevalence estimates of severe lesions were 1.76 /1000 (1.68, 1.84) among children and 0.64 /1000 (0.61, 0.67) among adults.
Conclusions
We report data on life-time prevalence of CHD in the general population. Birth prevalence rates are comparable to those published by the Centers for Disease Control in the United States. In 2010, the prevalence of CHD in adults was 6.07 per 1000 corresponding to a 50% increase compared to the year 2000. These results should help inform the generation of contemporary estimates of the number of people living with CHD in the United States and other industrialized nations.
CARDIOVASCULAR SURGERY FOR ADULT CONGENITAL HEART DISEASE: VARIATION IN USE OF SPECIALTY-CARE CENTERS
Author links open overlay panelSusan M.FernandesLisaChamberlainStaffordGradyJonathanMayoAlexanderOptowskyLee M.SandersPaul H.Wise
Stanford University, Palo Alto, CA, USA, CA, USA
Background
2008 ACC/AHA Guidelines for the management of adults with congenital heart disease(CHD) recommend cardiac surgery for moderate/complex CHD be performed in an adult CHD (ACHD) center (Ctr). Given this, we sought to determine the proportion and predictors of ACHD cardiac surgery performed at ACHD Ctrs.
Methods
This study used California’s Office of Statewide Health Planning and Development discharge database to perform a retrospective population analysis of ACHD cardiac surgery (>21 years of age) in California (CA) between 2000 and 2009. Center type (ACHD Ctr vs. non-ACHD Ctr) was defined based on a national, volunteer clinical directory. We examined the relationship between Ctr type and mortality, length of stay (LOS), and hospital charges.
Results
There were 5,811 ACHD cardiac surgeries performed in CA between 2000-2009. Only 28% of hospital discharges; 37% of moderate/complex discharges were from ACHD Ctrs. There was no difference in hospital mortality by Ctr type (ACHD ctr=0.6% vs non-ACHD Ctr=0.9%, p=0.125). Median LOS was longer in ACHD Ctrs [6 days (IQR 4-8) vs 5 days (IQR 4-8), p=0.045]. Median total charges were lower for ACHD Ctrs [$127,712 (IQR $83,439-$196,426) vs $138,081 (IQR $89,967-$200,969), p=0.0033] as well as the hospital charges per day ($21,477 [IQR $15,337-$30,572] vs $24,155 (IQR $16,465-$33,455), p<0.0001]. In multivariate analysis, after controlling for disease complexity, the following factors were independently associated with a lower odds of having surgery in an ACHD Ctr: private insurance [AOR 0.61, 95% Cl (0.53-0.70), p=0.004), Hispanic ethnicity [AOR 0.85, 95% Cl (0.72-0.99), p<0.0001] and having >3 medical co-morbidities [AOR 0.75, 95% Cl (0.62-0.92), p=0.0017].
Conclusion
There is profound variation in utilization of ACHD Ctrs in CA. Most ACHD cardiac surgeries are being performed in non-ACHD Ctrs, where expenses and co-morbidity are higher. In addition, non-clinical and clinical factors appear to play an important role in hospitalization patterns of ACHD patients in CA. Understanding these factors is essential in planning for the care needs of this population.
PREDICTING OUTCOMES USING THE HEART FAILURE SURVIVAL SCORE IN ADULTS WITH CONGENITAL HEART DISEASE
Author links open overlay panelElaine Y.LinHillel W.CohenJacobJohnsonAdaStefanescuAmi B.BhattGeorge K.Lui
Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY, USA
Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA
Background
Adults with congenital heart disease (CHD) face increased risk for morbidity and mortality as they age, but few prognostic models exist. This study aims to assess whether the Heart Failure Survival Score (HFSS) which risk stratifies patients for heart transplantation predicts outcomes in adults with CHD.
Methods
This retrospective study identified 146 of 407 patients with moderate or complex CHD who underwent cardiopulmonary exercise test and had all the HFSS parameters at Montefiore Medical Center in Bronx, NY and Massachusetts General Hospital in Boston, MA from 2009 and 2012. HFSS components (coronary disease, interventricular conduction delay, systemic ventricular ejection fraction (EF), resting pulse, sodium, mean arterial pressure, peak VO2) were collected. Risk strata are defined as low (>8.10), medium (7.2-8.09), and high risk (≤7.19). Death, transplant or ventricular assist device (VAD), arrhythmias, non-elective cardiovascular (CV) hospitalizations, and the composite were studied. HFSS was calculated based on published algorithms. Associations between HFSS and each outcome were calculated.
Results
The cohort had a mean age of 34 years, peak VO2 of 21.5 mL/kg/min, and HFSS of 10.4. Follow-up averaged 166 days for death. There were 4 deaths, no transplants or VADs, 55 arrhythmias, 104 CV hospitalizations (in 40 patients), and 73 composites. One patient was medium risk by HFSS; the rest were low risk. Lower mean HFSS was observed for those with versus those without outcome: death (9.5 ± 0.95 vs. 10.4 ± 0.83, p = 0.04), arrhythmias (10.1 ± 0.87 vs. 10.5 ± 0.79, p = 0.003), CV hospitalizations (10.1 ± 0.74 vs. 10.5 ± 0.86, p = 0.006), and composites (10.1 ± 0.83 vs. 10.6 ± 0.78, p < 0.001). All outcomes occurred in low risk patients so that sensitivity and positive predictive value of medium risk was 0 for each outcome.
Conclusion
Although the HFSS was significantly associated with outcomes, medium and low risk strata failed to further risk stratify, making this model inadequate for prognosticating CHD patients, whose heterogeneous pathophysiology differs from that of the general heart failure population. Further studies are warranted to provide accurate prognosis in adults with CHD.
BLOOD BORNE BACTERIAL INFECTIONS OCCURRING IN PATIENTS WITH PERCUTANEOUSLY IMPLANTED BIOPROSTHETIC PULMONARY VALVE: A SINGLE CENTER EXPERIENCE
Author links open overlay panelJonathanBuberLisaBergersenJamesLockKimberleeGauvreauMichaelLandzbergAnne MarieValenteAudreyMarshall
Boston’s Childrens Hospital, Boston, MA, USA
Background
Percutaneous pulmonary valve implantation (PPVI) using a stent-based bioprosthetic valve is utilized as an alternative to surgery in selected patients. Cases of systemic infections in Melody valve-implanted patients have been reported, yet the incidence and associated risk factors have not been studied in a large cohort.
Methods
Between 2007 and 2012, 149 consecutive patients with congenital heart disease underwent percutaneous Melody valve implantation at Boston Children’s Hospital. Predictor variables collected at baseline and follow up included demographic, clinical, echocardiographic and procedure-related variables factors. Our primary outcome was the occurrence of blood borne bacterial infection treated with >4 weeks of antibiotic therapy, as identified within the database as an adverse event, or by medical record review.
Results
Two patients died of non-infectious causes in the immediate post procedural period. The remaining 147 patients, of whom 59% had Tetralogy of Fallot, had a mean age at implantation of 21.5 years. During a median follow up of 19 months (range: 1 to 63), 14 patients experienced an outcome event (9.5%, 95% Cl 5.3%-15%). Of these, 5 (5 of 147, 3.5%) were diagnosed with endocarditis affecting the Melody valve, necessitating valve explantation in one patient, the others were treated medically. Two patients without known valve involvement died at the time of the event. The median procedure to infection time was 15 months (range 1 to 56). In univariate analysis, the following patient and anatomical characteristics were associated with the occurrence of bacterial infection: male gender, history of prior endocarditis, in situ stents in the right ventricular outflow tract prior to valve placement, and presence of outflow tract irregularities at the implant site.
Conclusions
In Our cohort, 9.5% of patients who underwent PPVI with a Melody valve were subsequently treated for a systemic bacterial infection. The infections occurred between 1 and 56 months after implant, and 5 had confirmed involvement of the valve. Our findings suggest that patient and anatomical factors may be associated with systemic bacterial infection after PPVI.
AORTIC DISTENSIBILITY INDEPENDENTLY PREDICTS EXERCISE CAPACITY IN ADULTS WITH REPAIRED CONOTRUNCAL DEFECTS
Author links open overlay panelMarkusSchwerzmannPascalSchmidheinyKerstinWustmannAndreasWahlJean-PierrePfammatterAlexanderKadner
Congenital Cardiac Center, University of Bern, Inselspital, Bern, Switzerland
Background
: Histological structural abnormalities of the medial aorta are common in adults with conotruncal defects. Using cardiac magnetic resonance imaging (MRI), we documented a decreased distensibility of the ascending aorta in these repaired adults compared to controls. We hypothesize that impaired aortic distensibility increases the afterload burden for the subaortic ventricle and compromises cardiac output during exercise.
Methods
Exercise capacity was assessed by cardiopulmonary exercise testing in 26 adults with d-TGA and an atrial switch procedure, and 35 adults with repaired TOF, and analyzed in relation to the patients’ characteristics, the ejection fraction of the subaortic ventricle, and the ascending aortic distensibility.
Results
The mean age of adults with repaired TOF was 29 ± 10.6 years, and 23.4 ± 7.4 years in adults with d-TGA (p=0.026). Absolute exercise capacity did not differ between both groups nor the percentage of predicted peakVO2 (76 ± 27% and 73 ± 20, p=0.638). In a multivariate regression analysis with age, gender, type of congenital defect, body surface area, subaortic ejection fraction and aortic distensibility as predictors of peakVO2, the only independent predictors of exercise capacity were gender and aortic distensibility (Table 1)
Conclusions
Impaired aortic distensibility predicts exercise capacity in adults with repaired conotruncal defects, independent of the subaortic ejection fraction.
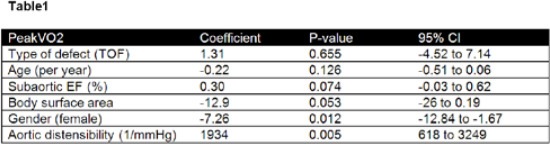
PRENATAL ECHOCARDIOGRAPHIC INDICES PREDICT COARCTATION OF THE AORTA
Author links open overlay panelDongngan T.TruongNelangiPintoMichaelPuchalski
University of Utah, Salt Lake City, UT, USA
Background
Coarctation of the aorta (CoAo) is difficult to diagnose prenatally. Recent studies have focused on transverse arch, isthmus, and isthmus/ductal size as potential predictors of postnatal CoAo. Accurate diagnosis is important for appropriate delivery plans. We sought to determine additional prenatal echocardiographic predictors of postnatal CoAo requiring intervention.
Methods
We studied consecutive fetuses followed prenatally at a regional referral center for concerns of CoAo based on right/left heart size discrepancy from 8/06 to 6/12. Fetuses with additional major heart defects were excluded. Maternal and infant demographics, fetal echos, and post-natal outcomes were examined. The primary outcome was intervention for CoAo prior to hospital discharge after birth. The association of prenatal predictors was examined with univariate logistic regression analysis.
Results
The study group included 58 fetuses, with 110 fetal echos. 47% of infants had CoAo and underwent surgical repair. On the first fetal echo, smaller mitral valve Z score (OR 0.56, P=0.01), smaller aortic valve Z score (OR 0.40, P=0.001), smaller ascending aorta Z score (OR 0.60, P=0.043), larger pulmonary to aortic valve ratio (OR 23.89, P=0.005), and smaller isthmus to ductal ratio (OR <0.01, P=0.009) were associated with postnatal CoAo intervention. On the final echo prior to delivery, only aortic valve Z score (OR 0.38, P=0.003), ascending aorta Z score (OR 0.46, P=0.005), and pulmonary to aortic valve ratio (OR 16.19, P=0.03) were associated with CoAo. Discrepancy in mitral and tricuspid valve size, transverse arch Z score, and right/left ventricular size were not predictive.
Conclusions
Aortic measurements are strongly associated with the need for CoAo repair, but no single fetal echocardiographic index is accurately predictive. Pulmonary to aortic valve ratio, which is easily determined on fetal echo, may increase clinical accuracy in predicting CoAo prenatally if used in a combined algorithm of echo parameters.
MIXED AORTIC valve DISEASE IN THE YOUNG: INITIAL OBSERVATIONS
Author links open overlay panelAllison C.HillStevenColanDavidBrownKimberleeGauvreauPedro delNidoJamesLockRahulRathod
Children’s Hospital Boston, Boston, MA, USA
Background
The natural history and results of surgical intervention in mixed aortic valve disease (MAVD) in children are unknown. We hypothesized that surgery for MAVD would improve valve function, decrease left ventricular end diastolic volume (LV EDV), decrease LV mass, and preserve systolic function.
Methods
Clinical and testing data for 90 patients with at least both moderate aortic stenosis and aortic regurgitation were analyzed retrospectively. A novel MAVD score (= aortic valve gradient * LV EDV z-score) was created.
Results
Half had been managed medically and half had aortic valve surgery, with median age for surgery at 13 years. LV EDV and mass were elevated in both groups (LV EDV z-scores 2.5 ± 1.6 and 3.5 ± 2.5 respectively; LV mass z-scores 3.4 ± 1.9 and 4.2 ± 2.1 respectively). LV mass volume ratio (MVR) and ejection fraction were normal in both groups. Early diastolicpulsed-Doppler mitral inflow (E)/early diastolic tissue Doppler velocity (E’) z-score indicated the presence of diastolic dysfunction in both the medical and surgical groups (3.5 ± 4.2, 3.9 ± 2.5 respectively). LV end diastolic pressure (EDP) was correlated with age (r = 0.4, p = 0.05) and LV MVR (r = 0.4, p = 0.05) but not MAVD score (r = −0.1, p = 0.48). On 6-12 month postoperative echocardiograms for surgical patients, aortic valve gradients and aortic regurgitation were significantly improved (aortic valve gradient improved from 65 ± 17 to 28 ± 18mmHg, p = 0.01; aortic regurgitation grade decreased from median of moderate to mild, p < 0.01). LV EDV was normal 6-12 months. LV mass was significantly improved (p < 0.01). Diastolic dysfunction did not change significantly after surgery. The presence of symptoms did not correlate with any measured parameter; however those with symptoms preoperatively had resolution postoperatively.
Conclusions
MAVD is primarily an iatrogenic disease, caused by intervention on diseased aortic valves in neonates and children. Despite significant diastolic dysfunction, systolic function is invariably preserved and symptoms are not correlated with aortic valve function or LV EDP. Current surgical practice preserves LV mechanics and results in short term improvement in valve function and symptoms.
INTRAUTERINE EXPOSURE TO MATERNAL DIABETES IS ASSOCIATED WITH INCREASED AORTIC STIFFNESS IN EARLY AND LATE INFANCY
Author links open overlay panelHalima AadamAlhashemiTimothyColenAkikoHiroseNajlaAlrajaaSandraDavidgeWinnieSavardMichaelSticklandVenuJainLisaHornberger
University of Alberta, Edmonton, Canada
Background
Infants of mothers with diabetes (IDM), the most common complication of pregnancy, have an increased risk of adult cardiovascular disease (CVD) later in life. IDMs have been shown to have increased aortic intimal-medial thickness in the neonatal period which may contribute to or be a precursor of CVD. Experimental models also suggest the intrauterine diabetic environment structurally and functionally alter the aorta of affected offspring. We sought to determine if there is evidence of increased aortic stiffness, a feature of CVD in adults with diabetes, in IDM in infancy.
Methods
Diabetic pregnancies were recruited prospectively to examine the role of diabetes in fetal cardiovascular programming. For this aspect of the study, their infants were evaluated at 3-6 weeks (early infancy) and at 6-12 months (late infancy) by echocardiography for assessment of aortic stiffness and the findings were compared to those of healthy infants from uncomplicated pregnancies. Pulse wave velocity (PWV) was calculated as {D/(T2-T1)}; where D was the distance of blood flow through the arch; T1 the time measured from QRS to onset of ascending and T2, the onset of descending aortic systolic flow.
Results
Thirty three maternal-infant pairs were assessed including 13 IDMs and 20 controls. Five IDMs had assessments both in early and later infancy. No statistical difference was observed in age at exam, BSA and systolic blood pressure between IDMs and controls. Hemoglobin A1C (HbA1) of the diabetic mothers during pregnancy ranged from 5.7 to 9.6 (median 7.4±1.1). Aortic PWV were significantly higher among IDMs compared to control (mean 5.7±2.25 M/s vs 3.7 ± 1.2M/s respectively, p=0.008). Interestingly, data for the paired IDM group showed that PWV only increased in late DM (7.2 ±1.1) compared with early DM (5.8 ±1.8) (p=0.04) In addition, IDM PWV in this small cohort tended to correlate positively with maternal HbA1C (r=0.56, p=0.04).
Conclusion
IDM have evidence of increased aortic stiffness in early infancy, which may increase later in infancy and may relate to maternal glycemic control. The pathogenic mechanisms responsible for increased aortic stiffness and its relevance to adult CVD requires further investigation.
EVALUATION OF MID-TERM OUTCOMES IN COARCTATION OF THE AORTA MANAGED IN THE RECENT ERA
Author links open overlay panelSusan F.SaleebDanyalThaverKimberleeGauvreauAudreyMarshallDavidFulton
Children’s Hospital Boston, Boston, MA, USA
Background
Coarctation of the aorta (CoA) has long term sequelae of systemic hypertension, premature cardiovascular disease and death. We sought to determine possible risk factors for such outcomes in the recent era of CoA management.
Methods
Performed by retrospective chart review of patients with isolated CoA (other hemodynamically significant lesions excluded) who had surgical or catheterization (cath) procedure from 1998-2010, with viewable diagnostic echocardiogram, and minimum 1 yr post-procedural follow up.
Results
Median age at diagnosis of CoA for the 83 subjects was 0.03 yr (−0.4-29.0) with follow-up of 9.7 yr (1.1-31.0). Median age of initial procedure was 0.04 yr (0.0-16.9, surgical n=66) compared to 12.5 yr (0.1-29.3, cath n=17). At last follow up, median upper to lower extremity BP gradient was −3 (−30 to 38), Doppler uncorrected gradient was 20 (0-37), and cath peak-peak gradient was 4 mm Hg (0-35, n=28). Hypertension (HTN), pre-HTN, or HTN on exercise stress test was present in 25% at median 9.4 yr (5.5-29.0) and was associated with older age of diagnosis (7.1 vs. 0.02 yrs, p <0.001), first procedure ≥6 mos vs. <6 mos of age (27.6% vs. 7.4%, p=0.02), elevated blood pressure (BP) percentile at diagnosis (95±13 vs. 82±20, p=0.002), and increased left ventricular (LV) mass z-score at diagnosis (2.6±1.3 vs. 0.7±2.0, p=0.002). Median cath measured LV end diastolic pressure (n=30) was 12 mm Hg (6-19) at a median age of 11.4 yr (0.1-30.3). Increased LV end diastolic pressure was not related to LV systolic dysfunction, HTN, or age at first procedure. LV mass z-score >2 was present in 7 of 75 patients (9%) at last follow up (median 0.29, range −2.08 to 2.67). A single procedure was performed in 70%, 2 in 24%, and 3 in 6%. Re-intervention was less common with lower initial BP gradient (35±17 vs. 44 ± 16, p=0.05) and was not related to size at initial procedure or arch measurements. Though not statistically significant, fewer re-interventions occurred if age at initial procedure <6 mos vs. ≥6 mos (25.9 vs. 37.9%, p=0.32).
Conclusions
At mid-term follow up of current CoA management, HTN and diastolic dysfunction are common and may contribute to early morbidity and mortality associated with CoA.
INTERMEDIATE TERM OUTCOMES IN PATIENTS WITH INTERRUPTED AORTIC ARCH
Author links open overlay panelMichaelO’ByrneLauraMercer-RosaHuaqingZhaoXuemeiZhangRonnTanelBradleyMarinoAmyCassedyMarkFogelJackRychikWeiYangStephenParidonElizabethGoldmuntz
Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Background
Studies of outcome following repair of interrupted aortic arch (IAA) have focused on mortality and rate of re-intervention. We sought to investigate the clinical status of subjects following IAA repair.
Methods
A cross-sectional assessment of subjects with IAA was performed, with genetic testing, electrocardiogram, cardiac magnetic resonance imaging, cardiopulmonary exercise testing, functional status and health-related quality of life (HRQOL) questionnaires (CHQ50 and PCQLI respectively). Review of their medical history provided retrospective information on the incidence of cardiac re-intervention and utilization of medical care.
Results
Twenty-one subjects aged 11.6+/- 3.6 years with IAA were enrolled. The prevalence of 22q11.2 deletion was 67%. All underwent single stage operative repair. Re-intervention rates were 38% on the left ventricular outflow tract, 33% for the aortic arch, and 24% for both. Left ventricular ejection fraction was 71.7+/-5.8%. Percent predicted maximal oxygen consumption (68+/-18%) and forced vital capacity (71+/-15%), as well as maximal work (76+/-22), were diminished compared to published age and gender norms (p<0.0001). Functional status (p=0.0002 for transformed physical, p=0.0063 for transformed psychosocial) and HRQOL (total score) were diminished relative to historical controls with repaired mild congenital heart disease (p <0.0001) and those with Fontan operations (p=0.0179). Subjects demonstrated frequent utilization of both inpatient and outpatient resources including hospitalizations, non-cardiac operations, subspecialty visits, and medications.
Conclusion
Patients with IAA demonstrate persistent co-morbid disease, with frequent cardiac intervention, and deficits in exercise performance, functional status, and HRQOL.
MIDAORTIC SYNDROME: 30-YEAR EXPERIENCE WITH MEDICAL, ENDOVASCULAR AND SURGICAL MANAGEMENT
Author links open overlay panelDiegoPorrasDebroahSteinMichaelFergusonGulraizChaudryAhmadAlomariKhashayarVakiliSteven J.FishmanJamesLockHeung B.Kim
Boston Children’s Hospital, Boston, MA, USA
Background
Midaortic syndrome (MAS) is associated with severe hypertension, which can be refractory to medical management and associated with significant morbidity and mortality.
Methods
We describe our 30-year experience with multidisciplinary management of patients with MAS.
Results
Fifty-three patients were included with a median age at presentation of 6.7 (birth – 28.7) years. All patients underwent medical management and 35 patients (66%) underwent invasive management (percutaneous techniques: 21; surgical techniques: 5; both: 9). At most recent follow-up, the majority of the patients (67%) were normotensive. The median duration between the time of presentation and achievement of blood pressure control was 5.7 (0.4–21.1) years. The median number of anti-hypertensive medications was 1 (0–5). Percutaneous interventions were acutely successful in decreasing the gradient across the obstruction and % luminal stenosis. However, freedom from reintervention was only 58% at 1 year and 33% at 5 years. Freedom from reintervention after a surgical procedure was longer: 83% at 1 year and 72% at 10 years.
Conclusions
A multidisciplinary management strategy, which couples comprehensive medical management with catheter-based and surgical interventions, can lead to adequate blood pressure control and preservation of end-organ function in the majority of patients with MAS.
SPECTRUM OF CONGENITAL HEART DISEASE AND OUTCOMES IN CHILDREN WITH TURNER SYNDROME: A SINGLE-CENTER EXPERIENCE
Author links open overlay panelJonathan W.CramerPippaSimpsonPeterBartzStevenZangwill
Medical College of Wisconsin, Milwaukee, WI, USA
Children’s Hospital of Wisconsin, Milwaukee, WI, USA
Background
Turner syndrome (TS) is a common genetic abnormality that affects 1 in 2500. Despite the known association between TS and congenital heart disease (CHD), the outcomes following surgical repair have not been well described. We reviewed the spectrum of CHD associated with TS within our center and provide outcomes following aortic coarctation (CoA) repair or staged palliation of hypoplastic left heart syndrome (HLHS).
Methods
The records of patients diagnosed with TS at Children’s Hospital of Wisconsin from 1999–2011 were reviewed. Those patients with TS and CoA or HLHS were then selected and compared against all non-TS patients undergoing like repairs.
Results
Of the 173 patients with TS, 77 (44.5%) were found to have CHD, with left sided obstructive lesions being the most common. However, the spectrum of CHD was wide and included systemic and pulmonary venous abnormalities as well as coronary arteries abnormalities. 21 TS patients were compared to all non-TS patients with isolated CoA undergoing repair during a similar time period. TS patients were statistically more likely to receive a subclavian flap repair, have a longer aortic cross clamp time and have a longer length of hospital stay following repair. Between age matched (age < 60 days) cohorts, the incidence of subclavian flap repair was not statistically different but both aortic cross clamp time and postoperative length of stay remained longer in the TS cohort. In long term follow up (8.8 +/- 9.1yrs) 17% of TS patients had residual hypertension, but no patient required re-intervention and there were no deaths. Finally, amongst 4 patients with HLHS, 3 died within the first year, compared to our previously published 93% survival for standard risk single ventricle patients.
Conclusions
We conclude that the spectrum of CHD seen with TS is not restricted to left sided obstructive heart lesions and included both arterial and venous abnormalities. Additionally, patients with TS undergoing surgical CoA repair may have a more challenging early peri-operative course, but their long term outcomes are similar to their non-TS peers. Finally, the combination of TS and HLHS remains a very challenging population with generally poor survival.
THE EFFECT OF ANGIOTENSIN-CONVERTING-ENZYME INHIBITORS ON THE RATE OF ASCENDING AORTA DILATION IN PATIENTS WITH BICUSPID AORTIC VALVES
Author links open overlay panelScott W.GatlinTraciLeongMatthewOsterMaanJokhadarWilliamMahle
Emory University, Atlanta, GA, USA
Background
Bicuspid aortic valve (BAV) is associated with progressive dilation of the aorta that can lead to dissection. Based on data from other form of aortopathy some have suggested that angiotensin-converting-enzyme inhibitors (ACEI’s) can decrease the rate of dilation of the ascending aorta. We sought to determine if ACEI’s reduce the rate of aortic dilation in adolescents and young adults with BAV.
Methods
A retrospective cohort study of adolescents and young adults with BAV (n = 142) seen at our institution from 2000 to 2011 was performed. Clinical data were reviewed and ascending aorta measurements were taken in serial echocardiograms. Linear regression was used to determine whether ACEI use was associated with a slower rate of growth in the ascending aorta Z score.
Results
Of the 142 subjects, 37 used ACEI’s and 105 did not. ACEI use was practitioner dependent. At initial measurement the mean age was 17.6 years and the mean ascending aorta Z score was 3.6. The median duration of follow-up was 27 months with a range of 6 to 75 months. The study groups were comparable in terms of age, body surface area, and length of follow up. There were differences between the groups in sex, initial ascending aorta size, and degree of aortic insufficiency. The treatment group had a higher percentage of males (84% versus 65%), larger initial ascending aorta z scores (4.5 versus 3.2), and a higher percentage of moderate aortic insufficiency (32% versus 9.5%). The mean rate of change in Z score per year was 0.005 for the treatment group and 0.1 for the control group. Use of ACEI was not significantly associated with change in Z score, p value 0.38.
Conclusions
ACEI use was not found to significantly alter the rate of aortic dilation in BAV patients in this population. What, if any, role ACEI’s have in the routine care of these patients remains to be determined.
THE PREVALENCE OF ARRHYTHMIAS DURING EXERCISE TESTING IN CHILDREN
Author links open overlay panelReenaGhoshGregory J.GatesMylesSchillerChristineWalshRobertPassLynnNappoScottCeresnak
The Children’s Hospital at Montefiore – Albert Einstein College of Medicine, Broxn, NY, USA
Background
Exercise testing is commonly performed in children for evaluation of cardiac disease. There are few data on the prevalence and types of arrhythmias observed during exercise testing in children.
Methods
A retrospective review of all patients < 21 years of age undergoing exercise testing at our center from 2008–2012 was performed. Patient demographics, hx of arrhythmias, echo findings, exercise data, arrhythmias during testing and interventions required were recorded. Chisquare was used for dichotomous variables, ANOVA for continuous data. P < 0.05 was considered significant.
Results
1,037 tests were performed in 916 patients. Mean age was 14 ± 4 years, 537 (55%) were male, 281 (27%) had congenital heart disease (CHD), 178 (17%) had a hx of a prior arrhythmia or rhythm disorder, and 17 (2%) had a pacemaker. Testing was on the treadmill in 677 (65%), the bike in 360 (35%), and with cardio-pulmonary assessment in 400 (40%). The main indications for testing were: Chest pain/palpitations 319 (31%), CHD 281 (27%), arrhythmia hx 148 (14%), and syncope 108 (10%). The most common forms of CHD were: TOF 54 (5.2%), single ventricle 49 (4.7%) and aortic valve dx 36 (3.5%). 291 (28%) patients had a rhythm disturbance during the procedure, the most common being PVCs in 192 (19%) and PACs 53 (5%). Clinically important arrhythmias were noted in 34 (3%) patients and included: 19 (1.8%) increasing ectopy with exercise, 5 (0.5%) VT, 5 (0.5%) second degree AV block, 3 (0.3%) SVT, and 2 (0.2%) AFIB. All arrhythmias spontaneously resolved and none of the patients required cardioversion or acute anti-arrhythmic therapy. Variables associated with the development of a clinically relevant arrhythmia included: severe left ventricular (LV) dysfunction on echo (p<0.001) and a prior history of a documented arrhythmia or arrhythmia disorder (e.g. LQTS, p<0.001). There were no complications or adverse events related to testing.
Conclusions
A total of 29% of children developed a rhythm disturbance during exercise testing and 3% were clinically important. Severe LV dysfunction and a history of documented arrhythmia or arrhythmia disorder were associated with the development of a clinically important arrhythmia in children.
LONG TERM MORTALITY IN LOW RISK ADULT PATIENTS WITH CONGENITAL LONG QT SYNDROME: LIFE INSURANCE CONSIDERATIONS
Author links open overlay panelClaireZhangIlanGoldenbergValentinaKutyifaScottMcNittBronislavaPolonskyChristineTompkinsWojciechZarebaArthurMoss
University of Rochester Medical Center, Rochester, NY, USA
Background
To date most risk stratification studies in long QT syndrome (LQTS) have focused on identifying high-risk subjects. Current data on the long-term clinical course of low-risk adult LQTS patients are limited.
Methods
Patients in this study were from the Rochester-based LQTS Registry. We hypothesized that long-term survival of LQT1-2 patients with QTc <500ms and no cardiac symptoms before age 20 (n=523) would be similar to that of their unaffected genotype-negative family members (n=1134). Kaplan-Meier and Cox proportional hazards regression analyses were the statistical techniques utilized.
Results
The low-risk LQTS study group comprised 27% of genetically confirmed LQTS Registry patients alive at age 20. The cumulative probability of all-cause mortality to age 65 was similar between the low-risk LQTS group and the genotype-negative control group (4.3% and 4.4%, respectively at age 65; p=0.49 for overall difference [Figure 1]). Multivariate analysis showed no significant difference in the risk of all-cause mortality between the two groups (HR = 0.94; 95% CI 0.52-1.69, p=0.82). Similar results were seen in females, males, LQT1, and LQT2 subjects. LQTS females had a lower mortality risk than males (HR = 0.59; 95% CI 0.38-0.93, p=0.02), particularly after age 50.
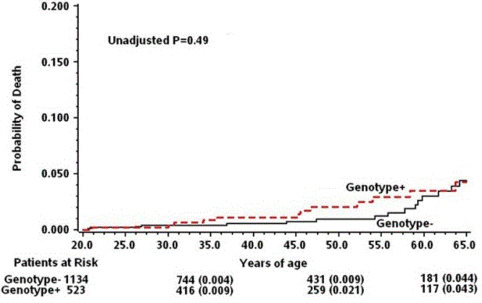
Conclusion
We identified low-risk, adult LQTS patients with a 45-year survival similar to unaffected family members. These low-risk LQTS patients should qualify for normal, age-related life insurance.
A COST-EFFECTIVE APPROACH TO RADIOFREQUENCY CATHETER ABLATION OF LEFT-SIDED ACCESSORY PATHWAYS IN YOUNG PATIENTS WITH WOLFF-PARKINSON-WHITE SYNDROME: A NOVEL THREE CATHETER TECHNIQUE
Author links open overlay panelChristine A.CaponeScott R.CeresnakLynnNappoGregory J.GatesRobert H.Pass
The Children’s Hospital at Montefiore Albert Einstein College of Medicine, Bronx, NY, USA
Background
Ablation is the treatment of choice for WPW in children. With increased concern regarding healthcare costs, efforts to reduce cost while maintaining quality are paramount. We present a novel 3-catheter approach to the ablation of left-sided accessory pathways (AP) in children with WPW.
Methods
A retrospective review from 2008 to 2012 of pts < 21 yrs with WPW who underwent a 3-catheter RF ablation of a left-sided AP (ablation, RV apical, and coronary sinus decapolar catheters). This 3-catheter group was compared to an age and gender matched control group who underwent a standard 5-catheter RF ablation for the treatment of left-sided WPW or concealed AP. Demographics, ablation outcomes and costs were compared between groups.
Results
28 pts met inclusion criteria with 28 control pts. The groups did not differ in gender, age, weight, or BSA (Table 1). Locations of the AP on the mitral annulus were similar between the groups. All pts were ablated transseptally. 28/28 in the 3 catheter group (100%) and 27/28 (96%) controls were acutely successfully ablated. No complications were encountered. There was no difference in procedural time, time to loss of AP conduction, or # of RF applications (Table 1). The catheter cost using 3-catheters was $1940 versus $2620 for the controls, yielding a savings of $680/case.
| Table 1 | 3-Catheter Group (N=28) | 5-Catheter Group (N=28) | P value |
| Gender | 18m, 10f | 18m, 10f | |
| Age (years) | 13.5 ± 3.4 | 12.8 ± 4.4 | 0.53 |
| Weight (kg) | 53.2 ± 19.2 | 52.2 ± 26.8 | 0.88 |
| BSA (m2) | 1.52 ± 0.34 | 1.43 ± 0.47 | 0.38 |
| Time to Loss of AP (sec) | 2.6 ± 2.1 | 2.0 ± 1.1 | 0.18 |
| Number of RF Applications | 7.6 ± 7.0 | 7.1 ± 9.0 | 0.80 |
| Procedure Time (min) | 110 ± 59 | 125 ± 55 | 0.30 |
| Acute Success | 28/28 (100%) | 27/28 (96%) | 0.31 |
Conclusion
Ablation in pts with WPW and a left-sided AP can be performed using 3 rather than the conventional 4-5 catheter approach with similar efficacy and safety while offering significant cost savings.
QRS PROLONGATION DOES NOT PREDICT MALIGNANT VENTRICULAR ARRHYTHMIAS AND SUDDEN DEATH IN PATIENTS FOLLOWING NEONATAL TETRALOGY OF FALLOT REPAIR
Author links open overlay panelBenjamin R.BlevinsNehaJoshiMaullyShah
The Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Background
A QRS duration on the resting ECG of ≥180 milliseconds (msec) has been previously reported to be the most sensitive predictor of life-threatening ventricular arrhythmias after tetralogy of Fallot (TOF) repair. The significance of QRS duration in predicting malignant ventricular arrhythmias and sudden death after neonatal TOF repair has not been previously described.
Methods
A retrospective observational study of children undergoing TOF repair in the first month of life at a single free-standing children’s hospital between 1991 and 2010 who survived to hospital discharge and had at least 12 months of follow-up was undertaken. Subject data were reviewed including demographic data, electrocardiograms, and clinical course.
Results
The study population included 111 subjects accounting for 968 person years of follow-up time. Median QRS duration was 118 msec (IQR: 90-140 msec). Sudden death occurred in 4 subjects (3.6%) with all-cause mortality of 13.5% (n=15). The most recent QRS duration in those subjects who died suddenly (92.0+/-39.4 msec 95% CI: 29.3-154.7) was not significantly different from those who did not (116.9+/-29.5 msec 95% CI: 111.2-122.5 msec p=0.104). A QRS duration greater than or equal to the study population median was not associated with increased rate of sudden death (Fisher’s exact test p = 0.096). QRS duration did increase significantly with follow-up time (p<0.001 r2: 0.242 beta: 2.7).
Conclusion
Prolonged QRS duration did not predict sudden death or malignant ventricular arrhythmiasin subjects who underwent neonatal repair of tetralogy of Fallot. Investigation of other risk factors is warranted in the current era of surgical repair of TOF.
COMPARISON OF VARIOUS FORMULAS FOR DETERMINATION OF THE QTC INTERVAL IN INFANTS AND CHILDREN LESS THAN SIX YEARS OLD
Author links open overlay panelDerekPhan
Harbor-UCLA, Los Angeles, CA, USA
Background
Determination of the heart rate corrected QT interval (QTc) is the basis for accurate ECG diagnosis of long QT syndrome (LQTS). The various commonly used formulas for heart rate correction have not been systematically evaluated in infants and young children.
Methods
Digital recordings of standard 12-lead ECGs were obtained from 702 children ≤ 6 years old with hearing loss who participated in a study of ECG screening for LQTS. The RR and QT intervals were digitally measured with a 4X zoom, each by 2 independent reviewers. QT intervals were then corrected for heart rates by use of the Bazett, Fridericia, Hodges, and Framingham formulas. QTc intervals (y-axis) were plotted against RR intervals (x-axis), and slopes of regression lines were compared. The closer the slope is to zero, the better heart rate correction across different heart rates.
Results
The mean age of the subjects was 2.3±1.7 years, with 230 (33%) <1 year. Heart rates ranged from 76 to 188 bpm (123±19).
| Formula | Mean QTc | QTc Standard Deviation (SD) | Slope of QTc-RR Regression | QTc 2 SD above mean |
| Bazett | 412 | 18 | 0.0046 | 448 |
| Fridericia | 366 | 19 | 0.125 | 403 |
| Hodges | 401 | 17 | −0.128 | 435 |
| Framingham | 289 | 26 | 0.291 | 342 |
For infants <1 year old, Bazett Formula also achieved the most consistent heart rate correction across heart rates ranged from 99 to 188 bpm (139±17), with near zero slope in QTc-RR plot (−0.01). The mean QTc by Bazett formula was 412±19 ms, and 2SD threshold 450 ms
Conclusions
The Bazett formula provided the best heart rate correction formula across a wide range of heart rates in infants and young children. The upper limit of QTc 450 ms remains the statistical threshold for consideration of a diagnosis of the prolonged QTc in infants and young children
VARIABLE INTERMEDIATE OUTCOME IN TOF IS EXPLAINED IN PART BY 22Q11.2 DELETION STATUS
Author links open overlay panelLauraMercer-RosaMarkFogelStephenParidonJackRychikRonnTanelWeiYangHuaqingZhaoElizabethGoldmuntz
The Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Background
Patients with tetralogy of Fallot (TOF) experience variable outcome though the determinants are incompletely understood. We sought to investigate the mechanisms underlying such variability by studying the clinical status of children and adolescents with TOF and the contribution of 22q11.2 deletion (22q11.2DS) to outcome.
Methods
Cross sectional study of TOF patients 8 to 18 years who underwent research-based genetic testing, cardiac magnetic resonance (CMR), exercise stress test (EST) and review of medical history.
Results
We studied 165 patients (12.3 3.1 years), of which 30 had 22q11.2DS (18%), 65% were male, 84% Caucasian and 73% (120) received a transannular patch. For the whole group, by CMR the right ventricular (RV) ejection fraction was 608% (36-82), pulmonary regurgitant fraction 3417% (0-63) and RV end-diastolic volume 11439 (43-222) cc/m2. On EST, predicted maximum oxygen consumption (VO2) for age and gender was 7616 % (28-121). The 22q11.2DS and ND groups were comparable in age, gender, size, pulmonary valveanatomy, age at surgical repair and operative approach. Despite comparable RV function and degree of pulmonary regurgitation, on EST the 22q11.2DS had lower % predicted: Forced Vital Capacity (61.5 16 vs. 80.5 14, p< 0.0001); VO2 (6117 vs. 8012, p<0.0001); and Work (6418 vs. 8622, p=0.0002). Compared to the ND, the 22q11.2DS had more hospitalizations (cardiac + non-cardiac) (6.6 [5; 10] vs. 3 [2; 5], p<0.0001), saw more specialists (3.5 [2; 9] vs. 0 [0; 12], p<0.0001) and used >1 medication (67 vs. 42%, p <0.001).
Conclusions
We demonstrate that genotype may explain some of the clinical variability seen in TOF, in particular with respect to resource utilization and significant differences in exercise performance. This study also provides data on an intermediate aged TOF population with relatively preserved ventricular function despite significant pulmonary insufficiency in the years preceding adult disease.
CHROMOSOMAL REARRANGEMENTS IN PATIENTS WITH CONGENITAL CARDIAC DEFECTS: A META-ANALYSIS REVEALS NOVEL POTENTIAL CRITICAL REGIONS INVOLVED IN HEART DEVELOPMENT
Author links open overlay panelThorThorssonS.SowJ.LevineWWRussellN.El-KashlamJeffreyInnisS.ZoellnerMarkRussell
University of Michigan, C.S Mott Children’s Hospital Congenital Heart Center, Ann Arbor, MI, USA
Background
Congenital cardiac defects (CCD) represent the most common group of birth defects, estimated at 8 per 1000 births. Genetic characterization of patients and families with cardiac defects has identified a number of genes required for heart development. Yet, mutations affecting known genes still account for only a small fraction of CCD suggesting that many more genes and developmental mechanisms remain to be identified. This study aimed at identifying novel loci containing genes critical for human cardiac development using duplication/deletion mapping.
Methods
We reviewed 766 described cases of patients with significant chromosomal rearrangements who were determined to have a chromosomal abnormality. Patients with multiple or whole chromosomal defects were excluded. Patients with overlapping deletions and/or duplications were grouped to identify regions potentially involved in heart development.
Results
36 chromosomal regions were identified in which 5 or more patients had overlapping rearrangements and 99 loci were affected in 2-4 patients with overlapping rearrangements. Of the former group, 9 of 36 loci involve genes (NKX2-5, GATA4, TBX1, GJA5, TAB2, NOTCh2, HAND2, CHD7, EHMT1) known to be involved in heart development, 9 involved deleted regions previously proposed to be involved in heart development, and 18 were novel loci or loci not strongly associated with cardiac defects. Of the 99 loci affected in 2-4 patients, only 11 involved loci were known or suspected to be associated with congenital heart defects. The 22q13.2 locus was further refined based on a new microdeletion to restrict the number of candidate genes to BIK and PACSIN2 which may represent a novel candidate gene/genes for CCD.
Conclusions
Duplication/deletion mapping of chromosomal rearrangements associated with CCD will provide an important roadmap for genome-wide sequencing and genetic mapping strategies to identify novel genes critical for heart development. The variable incidence of cardiac defects across loci suggests a dependence on genetic and/or environmental modifiers to determine the penetrance and phenotypic expression of the observed variations in the copy number of the candidate genes.
THE ECHOCARDIOGRAPHY “BOOT CAMP”: A NOVEL APPROACH TOWARD ACHIEVING BASIC PEDIATRIC IMAGING COMPETENCY
Author links open overlay panelShirazMaskatiaCarolynAltmanShaineMorrisAntonioCabrera
Section of Pediatric Cardiology, Baylor College of Medicine, Texas Children’s Hospital, Houston, TX, USA
Background
Dynamic training schedules introduce novel challenges to medical specialty training programs that require manual dexterity.
Objectives
To examine the effect of a 3-day, intensive pediatric echocardiography course (Boot Camp) on self-efficacy in performing an echocardiogram and in the acquisition and short-term retention of basic echocardiogram knowledge and skills for first-year pediatric cardiology fellows (CF).
Methods
The Boot Camp consisted of hands-on structured practice guided by sonographers and cardiology faculty, didactic lecture and reading. Pre-boot camp experience was assessed via an experience score (EXP). Outcome measures included written pre- and post-Camp exams, a performance based test (PBT), pre- and post-Camp self-efficacy assessments, and number of echocardiograms performed in the first 3 months of fellowship.
Results
Six CFs completed the Boot Camp. Two of the six CFs reported EXP of 2/10, whereas the remainder reported EXP of 0/10. PBT scores ranged from 68-99/147. All six CFs reported pre-Camp self-efficacy scores of 21/147 (minimum score), compared to median post-Camp scores of 82/147 (49-94/147) (p=0.01). Scores on the written exam improved from median of 16/29 (11-18) to 23.5/29 (22-28/29) (p=0.01) There was no difference in outcome measures between those with EXP>0 and those with EXP=0. CFs who completed the Boot Camp completed 28 independent echocardiograms (median 4 per CF) during the first 3 months of fellowship, increased from 5 independent echocardiograms (median 1 per CF) by CFs the year prior to institution of the Boot Camp (p=0.030)
Conclusions
The echocardiography Boot Camp improves self-efficacy in performing an echocardiogram and the acquisition and short-term retention of skills and knowledge required to perform a pediatric echocardiogram. Further areas of study include the effects of the Boot Camp on echocardiography quality and on diagnostic accuracy.
PATIENTS WITH A SYSTEMIC RIGHT VENTRICLE: WHO ARE AT RISK OF CLINICAL EVENTS?
Author links open overlay panelTeun van derBomMichielWinterMaartenGroeninkHubertVliegenPetronellaPieperArievan DijkGertjanSieswerdaJolienRoos-HesselinkAeilkoZwindermanBarbaraMulderBertoBouma
Academic Medical Center, Amsterdam, The Netherlands
Background
In patients with a congenitally corrected transposition of the great arteries or atrially corrected transposition of the great arteries, the systemic right ventricle worsen slowly over time. Worsening is often accompanied by clinical events, such as clinical heart-failure or the development of arrhythmia. However, there are large differences in the occurrence and onset of these events. We aimed to identify which patients are most likely to experience clinical events.
Methods
At baseline, all participants of the valsartan trial underwent regular electrocardiography, 24-hour ambulatory electrocardiography, echocardiography, cardiopulmonary exercise testing, and cardiovascular magnetic resonance imaging or multi-row detector computed tomography in those with pacemakers. Clinical events comprised death, tricuspid regurgitation requiring invasive treatment, ventricular and supraventricular arrhythmia, and worsening heart failure. A Cox proportional hazards analysis was used to assess determinants of event-free survival.
Results
A total of 88 patients with a mean age of 33 years, 65% men and 28% ccTGA were included. During a median of 4.3 years 31 patients (35%) experienced 50 clinical events; an annual risk of 13%. Peak exercise systolic blood pressure (HR 0.86, p=0.02) and right ventricular end-diastolic volume measured by means of CMR (HR 1.20, p<0.0001) were the strongest determinants of clinical events. The combination of these determinants resulted in a negative predictive value for clinical events during 4 years of 96%. These determinants (ROC 0.88) were superior to echo-and electrocardiographic predictors (ROC 0.70).
Conclusions
Patients with a systemic right ventricle have a high annual risk of clinical events. Patients with a peak exercise systolic blood pressure above 180mmHg and patients with only moderately dilated right ventricles had a very low risk of clinical events and might be considered for biannual clinical follow-up, whereas current guidelines recommend annual follow-up.
SIX-YEAR EXPERIENCE WITH A LUMENLESS PACING LEAD IN PEDIATRICS AND CONGENITAL HEART DISEASE
Author links open overlay panelJason MichaelGarnreiterPatriciaWhitakerThomasPilcherSusanEtheridgeElizabethSaarel
University of Utah, Salt Lake City, UT, USA
Background
Pediatric and congenital heart disease (CHD) patients requiring permanent pacing present unique challenges, including need for long duration of implant, small size, and structural abnormalities. A novel 4.1 Fr lumenless catheter delivered pacing lead (Model 3830, Medtronic, Inc, Minneapolis, MN) has proven useful in short term studies in this population. We report long-term experience with this lead.
Methods
Retrospective review of patients with a 3830 lead implanted at a single pediatric center from 2005 to 2011. Data were collected prospectively in a registry from time of implant. Data were compared to a similar control population of patients with a model 1488 lead (St. Jude Medical, Minneapolis, MN).
Results
A total of 193 patients with 198 model 3830 leads (125 atrial, 73 ventricular) were enrolled. CHD was present in 121 patients (63%). Age and weight at implant were 16.6 ± 8.5 years and 51.7 ± 23.5 kg. Length of follow up was 26 ± 19 months (range 0 [[Unable to Display Character: –]] 73). At implant, mean atrial sensing was 2.76 ± 1.26 mV and capture threshold was 0.61 ± 0.34 V at 0.5 ms. Implant ventricular lead sensing was 9.21 ± 4.52 mV and threshold was 0.5 ± 0.3 V at 0.5 ms. These values remained stable over time, and there were no significant differences in impedance, sensing, or thresholds compared to the 101 leads in the 1488 control group. Implant complications were rare in both groups. Long term complications were seen in 4% of the 3830 leads, and 16% of controls. Eight 3830 leads required extraction. Of note, all were fully extracted without complications using only manual traction. There were 3 deaths in each group. One death in the control group occurred during lead extraction. No other deaths were lead related.
Conclusion
This is the largest study to date reporting long term performance of the 3830 lead in pediatricand CHD patients. During 6 years of use this lead has demonstrated excellent efficacy, a low rate of complications and straightforward extractability relative to a control population with traditional pacing leads.
INTESTINAL LOCATION OF NECROTIZING ENTEROCOLITIS AMONG INFANTS WITH CONGENITAL HEART DISEASE
Author links open overlay panelClifford L.CuaJenniferAldrinkKathleenNicholLisaNicholsonCorrinCozzi
Nationwide Children’s Hospital, Columbus, OH, USA
Background
Infants with congenital heart disease (CHD) are at increased risk for developing necrotizing enterocolitis (NEC). Pathophysiology of NEC among infants with CHD is largely unknown although an alteration in intestinal blood flow remains a leading theory. Previous reports of NEC in non-CHD patients have documented primarily small intestinal involvement in preterm infants (< 37 weeks) versus primarily colonic involvement in full-term infants (> 37 weeks). Predominant location of NEC in CHD patients has not been previously described. Goal of this study was to determine if differences exist in the location of NEC in infants with CHD versus those without CHD.
Methods
Retrospective cohort study was performed on patients who underwent a surgical explorationfor NEC between1/2000 to 12/2011. The presence or absence of CHD was noted via echocardiograms. Surgical and/or pathology reports were reviewed to identify the location of NEC. NEC involvement was separated into small intestine, large intestine, ileocecal, NEC totalis, and multi-segment. T-tests and Chi square were used for analysis. P < 0.05 was considered significant.
Results
One hundred sixty-seven patients met inclusion criteria (149 non-CHD, 18 CHD). Non-CHD patients had significantly lower gestational age (28 + 4 vs. 34 + 5 weeks), birth weight (1178 + 58 vs. 2106 + 252 grams), and age at surgery (21 + 1 vs. 40 + 10 days) compared to CHD patients. CHD infants had a higher percentage of mortality (72% vs 29%). There was no significant difference in location of NEC between non-CHD and CHD patients with the predominant location being small intestine in both (31% vs 33%, respectively). In addition, there was no significant difference in location of NEC between preterm non-CHD patients (n = 137) and full-term CHD patients (n = 9) with the small intestine again being the primary site (34% vs. 44%, respectively).
Conclusions
Despite differences in gestational age between non-CHD and CHD patients, location of NEC in these infants did not differ. This suggests that the pathophysiology of NEC in the CHD population might be more similar to that of the preterm population than previously believed.
UTILIZATION OF AN ELECTRONIC PERSONAL HEALTH RECORD BY ADOLESCENTS AND ADULTS WITH CONGENITAL HEART DISEASE
Author links open overlay panelLinda BradleyTiernanMunzibaKhanAnithaJohnKarenKuehl
Children’s National Medical Center, Washington, DC, USA
Background
We have previously reported on development and implementation of www.followmyheart.org(FMH), a condition specific electronic personal health record (PHR) for patients with congenital heart disease (CHD). We now aim to describe patient utilization of FMH during the first 12 months of enrollment. We hypothesize that patient age and disease severity may correlate with frequency of PHR use.
Methods
All patients >15 years (y) of age seen in the Transition Clinic and Washington Adult Congenital Heart of the were offered enrollment in FMH from February 2011- October 2012. Demographic information (age, ethnicity, gender, educational level) and severity of disease were recorded. Individual patient log ins to FMH were tracked by an imbedded site function. Correlation analysis examined the relationship between demographic sub-groups and disease severity with PHR use.
Results
From February 2011 – October 2012 127 CHD patients > 15 y old registered for FMH; 81 participated in the study. Disease ranged from mild, moderate, to severe with mild patients being significantly younger than those with moderate or severe disease (mean age (SD): 24.0 y (8.5), 29.1 y (10.8), 28.3 y (8.8), p= 0.04). Three patients died and 1 withdrew during the study. Among the 77 remaining patients, there were 523 FMH log ins (range 0-71, mean frequency (SD) of 6.8 (11.2) times per patient per year). Mean frequency of use varied with age (<18 y – 3.0 (4.9), 18–21 y – 4.7 (10.6), >21y 7.9 (11.8), p=0.009). Older age category (>21 y) correlated with increased FMH use (R=0.34, p=0.002) while ethnicity, gender, educational level, and disease severity did not. There was a four-fold increase in rate of FMH use among women who were pregnant (all>21 y) during the study compared to the group as a whole. Patients reported liking the ability to access, share, and print their medical and surgical information and found it most useful in emergency situations.
Conclusions
PHR use among CHD patients was frequent but highly variable. Increased FMH use correlated with older age category but not with severity of disease and often related to acute intercurrent illness or pregnancy.
WHITE MATTER LESIONS ARE NOT ASSOCIATED WITH THE PRESENCE OF RIGHT-TO-LEFT SHUNT
Author links open overlay panelRezaMasoomiRubineGevorgyanWilliamHsuNorikoSalamonJonathanTobis
David Geffen School of Medicine at University of California Los Angeles (UCLA), los Angeles, CA, USA
Background
White matter lesions (WMLs) are prevalent in people who have migraine with or without a right-to-left shunt (RLS) across a patent foramen ovale (PFO). WMLs may also result from paradoxical emboli due to RLS in non-migraineurs. We studied if there is any association between WMLs and RLS by comparing the frequency of WMLs in subjects with a known RLS versus a general population.
Method
464 patients age 20-80 with a PFO had a brain magnetic resonance imaging (MRI) study. The images were interpreted by a radiologist for the presence of WMLs. Patients were divided into two groups based on the presence or absence of migraine. To determine the frequency of WMLs in age matched normal subjects, brain MRI results were reviewed from 2,728 patients, and those with conditions associated with WMLs such as cerebrovascularemergencies, migraine headache, brain tumors, vasculitis and multiple sclerosis were excluded.
Results
In all age groups of non-migraineurs with a RLS, WMLs were not more prevalent compared to age matched controls. Migraineurs with RLS had an increased prevalence of WMLs in age groups 30-39 (21.05% vs. 4.4% p=0.01) and 50-59 (49.15% vs. 21.2% p=0.0008).
The percent frequency of WMLs on MRI per decade:
The percent frequency of WMLs on MRI per decade:
| Age in years | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 |
| RLS w/o migraine % (N) with WMLs | 10% (1) | 4.7% (1) | 13.7% (7) | 23.7%(14) | 35.7%(15) | 30.43%(7) |
| Control % (N) with WMLs | 7.4% (5) | 4.4% (2) | 22.5%(16) | 21.2%(18) | 46.7%(31) | 69.7%(69) |
| p-values | 0.57 | 1 | 0.32 | 0.87 | 0.37 | 0.001 |
Conclusions
In people with RLS due to a PFO who do not have associated migraine headache or aura, there is no increase in the frequency of WMLs on brain MRI compared with an age matched control population. Migraineurs with RLS have a higher frequency of WMLs than age matched controls.
THE RISK OF SUDDEN CARDIAC DEATH IN ADULT CONGENITAL HEART DISEASE: IMPLICATIONS FOR IMPLANTABLE CARDIOVERTER DEFIBRILLATOR THERAPY
Author links open overlay panelZelihaKoyakBarbaraMulderAeilkoZwindermanLouiseHarrisErwinOechslinBertoBoumaCandiceSilversidesWernerBudtsIsabellevan GelderJoris R. deGroot
Academic Medical Center, Amsterdam, The Netherlands, Peter Munk Cardiac Centre, Toronto, Canada
Background
The absolute risk of sudden cardiac death (SCD) is largely unknown in adults with congenital heart disease (CHD). This hampers accurate assessment of the individual patient’s risk of SCD. We developed a risk scoring system to assess the absolute risk of SCD among adults with various CHD.
Methods
Predictors of SCD were previously derived from a case-controlled study and were 1) coronary artery disease, 2) heart failure 3) supraventricular tachycardias, 4) impaired systemic ventricular function, 5) impaired subpulmonary ventricular function, 6) QRS duration≥120ms and 7) QT dispersion≥70ms. We developed a point-based risk scoring system. Points were attributed to each variable depending on the B-coefficient. The calculation of the absolute risk of SCD was based on the number of risk factors present in one single patient and the a priori risk of SCD.
Results
Three risk scores were constructed. Risk score 1 was based on the raw logistic regression coefficients. Risk score 2 was based on the rounded logistic regression coefficients. In risk score 3 one point was attributed to each variable. The C-index was 0.77, 0.77 and 0.76 for risk score model 1, 2 and 3, respectively. The simplified risk score 3 was used to calculate the absolute annual risk of SCD among various defects (Figure 1).
Conclusion
We developed and validated a simplified risk score model to predict the absolute risk of SCD in CHD. This might be useful guiding clinicians in decision making for implantable cardioverter defibrillator therapy.
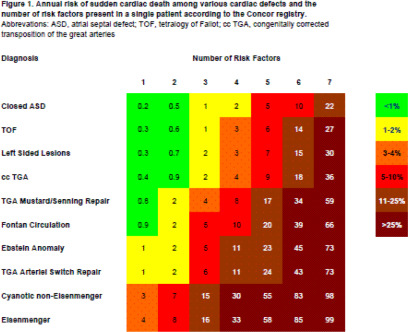
SYSTOLIC ANTERIOR MOTION OF THE ANTERIOR MITRAL LEAFLET AND HYPERTROPHIC CARDIOMYOPATHY: A PREDICTOR OF NON-GENETIC, NON-FAMILIAL DISEASE?
Author links open overlay panelBeth AnnMedfordKristinaHaugaaJohanBosAngelaMillerSteveOmmenBernardGershJonathanJohnsonFrankCettaBenjaminEidemPatrickO’Leary
Michael Ackerman, Mayo Clinic, Rochester, MN, USA
Background
Hypertrophic cardiomyopathy (HCM) is marked by profound phenotypic and genotypic heterogeneity. Systolic anterior motion (SAM) of the anterior mitral leaflet is a classically described feature of HCM but its genetic predilection is unknown.
Methods
Our study cohort consisted of 213 (74 male, mean age 51 ± 167 years) consecutive, unrelated patients referred to Mayo Clinic for evaluation of HCM. All underwent genetic testing for myofilament/sarcomeric HCM (ACTC1, MYBPC3, MYH7, MYL2, MYL3, TNNC1, TNNI3, TNNT2, TPM1). Patients with either a positive genetic test or positive family history of HCM were classified as genetic HCM (G+ HCM) while those with a negative genetic test and a negative family history were called non-genetic HCM (G- HCM). Blinded to the patient’s genetic classification, each echocardiogram was reviewed with particular attention to the maximum left ventricular wall thickness (MLVWT) and LV outflow tract obstruction (LVOTO), septal morphology, and presence of SAM.
Results
Overall, 88 patients (41%) were either mutation positive or had a family history of HCM and therefore considered familial/genetic disease. Compared to G+ HCM patients, those with G- HCM were older at diagnosis (54 ± 16 vs. 47 ± 16 years, p = 0.001), had lower MLVWT (19 ± 5mm vs. 21 ± 5mm, p = 0.02), but had more LVOTO at rest (47 ± 47mmHg vs. 29 ± 41mmHg, p = 0.004). Notably, G-HCM patients were more likely to have the classic HCM finding of SAM compared to G+HCM patients [78/125 patients (62%) vs. 34/88 patients (39%), p=0.001]. Independent of the resting gradient and septal shape, presence of SAM, older age, and decreased MLVWT were predictors of G-HCM (SAM: OR 2.3879; 95%CI1.5235-54.60.02, p=0.0011, Age: OR 1.03; 95%CI 1.01-1.05, p=0.0026, MLVWT: OR 0.93; 95%CI 0.88-0.98, p=0.01).
Conclusions
Independent of septal morphology and the degree of outflow tract obstruction, the presence of one of HCM’s first described echocardiographic findings, SAM, is seen more commonly in HCM patients with a negative genetic test and no evidence for familial disease. This paradoxical observation raises the possibility that a subset of HCM may stem from a primary abnormality involving the mitral valve apparatus.
THE EFFECT OF HIGH DOSE STATINS ON VASCULAR WALL DAMAGE AND CARDIOVASCULAR RISK IN AORTIC COARCTATION
Author links open overlay panelPaulLuiiendiikBertoBoumaJorisVriendHubertVliegenMaartenGroeninkEric DeGrootPetronellaPieperArievan DijkGert-JanSieswerdaGerritVeenAeilkoZwindermanBarbaraMulder
Academic Medical Centre, Amsterdam, The Netherlands
Background
Patients after coarctation repair (CoA) demonstrate an increased cardiovascular risk. Carotidintima-media thickness (CIMT) a reliable marker for atherosclerosis is increased in (CoA). HMG-coA-reductase-inhibitors (statins) have been proven to reduce CIMT and clinical events. The aim of our study was to evaluate the effect of statins on the vascular wall in CoA.
Methods
We designed a multicentre, prospective, randomised, open label trial with blind endpoint (PROBE design) to evaluate the effect of Atorvastatin 80 mg once daily on CIMT progression during 3 year follow-up. The primary endpoint in this study was CIMT measured by B mode ultrasonography. Secondary endpoints were mortality and morbidity due to cardiovascular disease, serum lipids and 24h ambulatory blood pressures.
Results
A total of 130 patients were enrolled (Atorvastatin = 66, No treatment = 64), of which 42 (64%) were on antihypertensive therapy in the statin group versus 42 (65%) in the group without treatment (P = 0.49). There was no significant effect of statin treatment on CIMT progression (treatment effect −0.005, 95%CI, −0.039–0.029; P= 0.76). In neither groups significant CIMT progression was found. Baseline CIMT was significantly higher in hypertensive as compared to normotensive CoA(0.61±0.98 mm vs 0.69± 0.16; P= 0.002). Regression analysis revealed that hypertension (ß = 0.004, P = < 0.001) was the strongest predictor for CIMT progression besides age (ß = 0.043, P = 0.031) and cholesterol (ß = 0.040, P = 0.027). A significant effect of statins on serum total cholesterol levels and serum LDL levels was found. (−0.71, 95% CI, −1.16 – −0.26; P = 0.002 vs −0.66 −1.06 – −0.26; P = 0.001). There was no difference in the remaining secondary outcome measures.
Conclusion
Hypertension is the strongest predictor for CIMT progression in CoA. Treatment with statinsdoes not reduce CIMT progression and secondary outcome measures, despite a decrease in serum total cholesterol and LDL. These findings suggest that the damaging effect of hypertension predominates the effect of statin therapy on the vascular wall. Future trials with anti-hypertensive agents are needed to evaluate the beneficial effect on the vascular wall in CoA.
HIGH RESOURCE USE AMONG ADULT CONGENITAL HEART SURGERY ADMISSIONS IN ADULT HOSPITALS: RISK FACTORS AND ASSOCIATION WITH DEATH AND COMPLICATIONS
Author links open overlay panelAlefiyahRajabaliPriyankaAsraniAmiBhattWeiHeOscarBenavidez
Massachusetts General Hospital, Boston, MA, USA
Background
The adult congenital heart disease population has exceeded the pediatric congenital population with an estimated prevalence of 1.3 million. Adults with congenital heart disease have greater co-morbidities than the general population and accrue significant hospital costs. Defining predictors of high resource use may assist adult hospitals with resource allocation for this growing population. Our objectives include 1) To examine resource use during adult congenital heart surgical admissions in adult hospitals 2) Determine the association of high resource use with complications and mortality and 3) Identify risk factors for high resource use.
Methods and Results
We obtained data from 709 hospitals using the Nationwide Inpatient Sample 2005-2009 and examined Adult Congenital Heart Surgical admissions ages 18–49 years (n=16,231). We defined High Resource Use (HRU) as admissions that exceeded the 90th percentile for total hospital charges; the threshold for HRU was approximately $300,000. Despite representing 10% of admissions, HRU admissions accounted for 68% of total charges. HRU admissions had a higher complication rate than non-HRU (72% vs. 33%, p<0.001) and a higher mortality rate (9.7% vs. 1.8%, P < 0.001). Multivariable analysis demonstrated that HRU is associated with: female gender Adjusted Odds Ratio (AOR) 0.9 (95% confidence interval [Cl] 0.7,1.0); government insurance AOR 2 (95% Cl 1.6, 2.4); weekend admission AOR 1.3 (95% Cl 1, 1.6), emergency admissions AOR 3.9 (95%CI 3.1, 4.8); urgent admissions AOR 2.2 (95% Cl 1.7, 2.9); complications AOR 4.3 (95% Cl 3.4, 5.4); renal failure AOR 1.8 (95%CI 1.5, 2.2); surgical complexity risk category 2 AOR 1.9 (95% Cl 1.1, 3.6); category 3+ AOR 2.3 (95% Cl 1.4, 3.7).
Conclusions
High resource use admissions consumed a disproportionate amount of resources and were associated with higher complication rates and mortality. HRU risk factors included gender, weekend admissions, non-elective admissions, government insurance, increasing surgical complexity, renal failure and complications. Complications, if preventable, may be a target for care improvement strategies to decrease resource use in this population.
HOSPITAL UTILIZATION IN ADULTS WITH SINGLE VENTRICLE CONGENITAL HEART DISEASE AND CARDIAC DYSRHYTHMIAS
Author links open overlay panelRickiFramXinyuTangJamesRobbinsRonnie T.Collins
University of Arkansas for Medical Sciences, Little Rock, AR, USA
Background
Most patients with single ventricle congenital heart disease (SV) are now expected to survive to adulthood. Cardiac dysrhythmias are common in SV and should impact healthcare cost.
Methods
We used nationally distributed data from the 2004 to 2011 Pediatric Health Information System database to identify patients ≥ 18 years of age admitted to the hospital with International Classification of Diseases-9th Revision codes for a diagnosis of either hypoplastic left heart syndrome, tricuspid atresia or single ventricle and a cardiac dysrhythmia. Comparison of hospitalization eras 2004-2007 (A) and 2008-2011 (B) was made using unpaired t-test.
Results
There were 218 SV patients with 297 admissions for a principal diagnosis (PD) of a cardiac dysrhythmia. Mean age was 25.8±6.6 years and mean LOS was 4.4±5.1 days. Total hospital charges were $17,298,027 with mean charge per admission of $58,243±126,375. Mean charge per hospital day was $13,237±24,779. The PD, number of admissions, age, LOS, and hospital charges are shown in Table 1. There was no difference in age or total charges for hospitalization eras. LOS was shorter (p=0.0279) and hospital charges per patient day were higher (p=0.0482) for era B.
Effect of Cardiac Dysrhythmia on Hospitalization in Adults with Single
| Dysrhythmia | Admissions Number (%) | Age (years) Mean+/−SD | Length of Stay (days) Mean+/−SD | Hospital Charges Mean+/−SD |
| Atrial flutter | 148 (50%) | 25.8+/−6.2 | 3.9+/−4.2 | $52,849+/−13,462 |
| Atrial fibrillation | 38 (13%) | 29.3+/−8.1* | 7.1+/−9.9⁁ | $94,870+/−176,298 |
| Sinoatrial node dysfunction | 17 (6%) | 24.0+/−5.6 | 4.0+/−2.4 | $73,501+/−64,177 |
| Complete heart block | 10 (3%) | 26.2+/−9.0 | 3.9+/−2.0 | $84,415+/−21,644 |
| Ventricular tachycardia | 9 (3%) | 22.8+/−4.1 | 6.1+/−4.3 | $57,095+/−70,364 |
| Supraventricular tachycardia | 9 (3%) | 25.2+/−6.9 | 4.4+/−3.8 | $55,659+/−12,523 |
| Other cardiac dysrhythmia | 65 (22%) | 24.8+/−5.9 | 3.9+/−3.3 | $41,861+/−47,855 |
*
indicates p=0.003 compared to cohort; ⁁, p=0.0076 compared to cohort
Conclusions
The cost of hospitalization for adults with SV and cardiac dysrhythmias is significant. Atrial fibrillation occurs in older adults with SV and increases LOS. The LOS for adults with SV and cardiac dysrthymia has decreased with time, however, hospital charges have increased.
HEART RATE RECOVERY PREDICTS CLINICAL WORSENING IN PATIENTS WITH CONGENITAL HEART DISEASE ASSOCIATED PULMONARY ARTERIAL HYPERTENSION
Author links open overlay panelBhuvneshAggarwalKevinMcCarthyReid A.DweikGustavoHeresiAdrianoTonelliOmar A.Minai
Cleveland Clinic Foundation, Cleveland, OH, USA
Background
Slow heart rate recovery (HRR) after exercise has been shown to be a predictor of mortality in patients with chronic cardiopulmonary diseases. The ability of HRR to predict clinical worsening in congenital heart disease associated pulmonary arterial hypertension (PAH) remains unexplored. Our aim was to identify the association of HRR at 1 minute (HRR1) after a 6-minute walk (6MW) test with clinical worsening in patients with congenital heart disease associated PAH.
Methods
All adult patients (N=50) with congenital heart disease associated PAH seen at our institute between August 2009 to September 2011 were included. HRR1 was defined as difference in heart rate between the end of 6MW test and after 1 minute of completion of 6MW test. Clinical worsening was defined as any escalation of drug therapy for PAH, PAH related hospital admission or death. Patients with HRR1 <25/min (N=15) were compared with those who had a HRR1 >25/min (N=35).
Results
Patient groups were comparable in baseline characteristics and hemodynamic variables. Patients with HRR1 <25/min were more likely to have clinical worsening events as compared to patients with HRR1 >25/min [Odds Ratio 7.8; 95% Cl (2-59); p <0.01]. HRR1<25 was associated with shorter time to clinical worsening (TCW) [13 months as compared to 8 months; p <0.01]. Patients with HRR1 <25 also had a significantly lower 6 minute walk distance than the patients with HRR1>25 (1064 feet versus 1449 feet; p <0.01).
Conclusions
HRR1 after the 6MW test is a strong and independent predictor of prognosis in patients with congenital heart disease associated PAH. HRR is a simple tool that can help predict clinical worsening and time to first clinical worsening event in patients with congenital heart disease associated PAH.
PREVALENCE AND CLINICAL CORRELATES OF TYPE OF DYSLIPIDEMIA IN ADULTS WITH CONGENITAL HEART DISEASE
Author links open overlay panelJoshua R.ThomasNasirMushtaqMarkFoxAngelaYetman
Primary Children’s Medical Center, University of Utah School of Medicine, Salt Lake City, UT, USA
University of Oklahoma School of Community Medicine, Tulsa, OK, USA
Background
Overweight and obesity are common in adults with congenital heart disease (ACHD) and relate to adverse outcomes beyond coronary artery disease including increased need for cardiovascular (CV) intervention, arrhythmia, and death. The prevalence of other CV risk factors, specifically dyslipidemia (DLD) in the ACHD population is unknown.
Methods
We sought to assess fasting lipid profiles in a cohort of ACHD patients. Lipid profiles were performed serially on all clinic patients who were fasting and in a non-pregnant state at the time of routine visit. DLD was classified into 5 subtypes as previously described (Table 1). Cross-sectional analysis was performed to evaluate for associations between DLD class and demographic variables.
Results
Two-hundred and twelve patients (41% Female) with a mean age of 34 (19-74) years were identified. Some form of DLD was present in 145(68%) patients. Significant association was found between DLD classification and BMI, as well as diabetes (Table 1). Patients with higher BMI were more likely to have Combined Hyperlipidemia, Low HDL-C, or MetS forms of DLD (OR 1.21 (95%CI 1.104, 1.326) OR 1.103 (95%CI 1.038, 1.173) and OR 1.137 (1.065, 1.214), respectively).
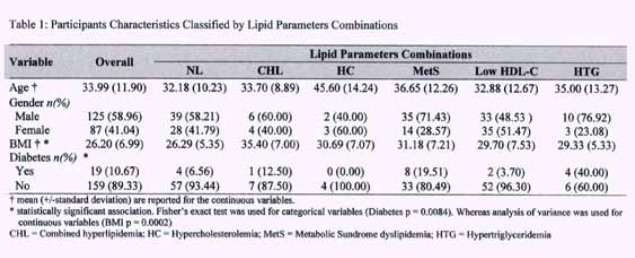
Discussion
Dyslipidemia is common in ACHD patients. These data suggest lipid monitoring as well as appropriate treatment among this population is paramount. Preventative counseling including avoidance of exercise restriction when appropriate should be initiated early.
CORONARY ARTERY OBSTRUCTION AFTER THE ARTERIAL SWITCH OPERATION: IS THERE REALLY A LONG-TERM PROBLEM?
Author links open overlay panelMieke MPDriessenJohannes MPJBreurRoland RJvan KimmenadeGertjan TjSieswerdaFolkert J.MeijboomTimLeiner
Wilhelmina Children’s Hospital & University Medical Center Utrecht, Utrecht, The Netherlands
The Interuniversity Cardiology Institute of the Netherlands, Utrecht, The Netherlands
Introduction
Reimplantation of the coronary arteries in the neo-aortic root is an important part of the arterial switch operation (ASO) for transposition of the great arteries. Postoperative coronary pathology is a potentially lethal complication with incidences reported of 3.3 to 18%. This study evaluates the presence of coronary obstruction and myocardial infarction or left ventricular (LV) dysfunction using multimodality imaging in patients decades after ASO.
Methods
Thirty-two patients after ASO were included. All patients underwent 256-slice computed tomography angiography (CTA). Cardiac magnetic resonance imaging was performed for late gadolinium enhancement (LGE) and measurement of LV ejection fraction (LVEF).
Results
All patients (63% male; mean follow-up 23.5 ± 4.9 yrs) were free of complaints of chest pain or dyspnea. Distribution of coronary artery origins is illustrated in the figure, 7 patients had an unusual coronary anatomy. Calciumscore was 0 in all patients. No coronary stenosis – either of the origo or in the course of the arteries – was seen on CTA. One patient had an interarterial course of the LAD. Seven patients (22%) had a decreased LVEF (<50%), but LGE was not demonstrated in any of the patients.
Conclusions
In contrast to previous reports, the current study found no coronary pathology using CTA in patients up to 33 years after ASO. Although 22% of the patients had a decreased LVEF, coronary obstruction or past myocardial infarction could not be demonstrated by CTA or LGE.
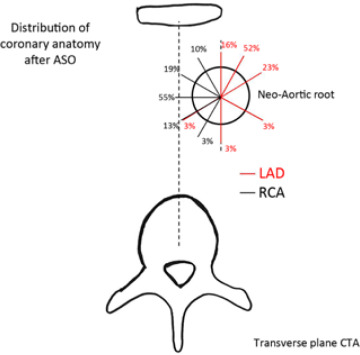
LONG-TERM FOLLOW-UP OF ARTERIAL AND ATRIAL SWITCH OPERATION FOR TRANSPOSITION OF THE GREAT ARTERIES
Author links open overlay panelClaudiaJungeStephanSchoofMechtildWesthoff-BleckReinerBuchhornGerhardZiemerSiegfriedGeyerKambizNorozi
University of Western Ontario, London, Canada, Hannover Medical School, Hannover, Germany
Background
Two decades after surgery for transposition of the great arteries (TGA), the clinical status, cardiac function, cardiorespiratory performance and neurohormonal activity of patients who underwent either atrial switch (Mustard) or arterial switch operation (ASO) were compared. Although cardiac outcomes of patients with TGA after Mustard or ASO have been well described, long term follow up and comparison of these surgical procedures in the adult population is lacking.
Methods
Sixty-two patients with simple TGA, who underwent either Mustard (thirty-four) or ASO (twenty-eight) procedure, have been included. Following the same study protocol, a clinical work up including echocardiography, stress test and blood work was completed for all patients.
Results
Mean age in both groups was comparable: ASO vs. Mustard [20.6 (SD=2.1) vs. 20.6 (SD=3.4) years]. All ASO patients were in NYHA class I, whereas 59% of Mustard patients were in NYHA class II or III. Peak oxygen uptake was higher in ASO patients (% of predicted 80 vs. 69, p<0.01). Compared to healthy individuals, the mean Tei index for systemic ventricle was high in both groups, but this parameter was significantly higher in Mustard than ASO patients [0.60 (SD=0.16) vs. 0.47 (SD=0.14), p<0.01]. The median plasma N-terminal pro brain natriuretic peptide in ASO patients was within the normal range but the Mustard group had significantly higher levels [42 (18–323) vs. 172 (26–1018), p < 0.0001].
Conclusion
Two decades after surgery the clinical status of patients who underwent ASO was better than the status of Mustard patients. This holds in terms of cardiac function, cardiorespiratory performance and neurohormonal activity.
IMPACT OF MEDICAL COMORBIDITIES ON HOSPITALIZATIONS IN ADULTS WITH SINGLE VENTRICLE CONGENITAL HEART DISEASE
Author links open overlay panelRonnie T.CollinsRickiFramXinyuTangJamesRobbins
University of Arkansas for Medical Sciences, Little Rock, AR, USA
Background
Most patients with single ventricle congenital heart disease (SV) are now expected to survive to adulthood. Medical comorbidities are common in SV.
Methods
We used nationally distributed data from 43 pediatric hospitals in the 2004 to 2011 Pediatric Health Information System database to identify patients ≥ 18 years of age admitted to the hospital with International Classification of Diseases-9th Revision codes for a diagnosis of either hypoplastic left heart syndrome, tricuspid atresia or single ventricle. Primary diagnoses (PD), length of stay (LOS) and hospital charges were determined. Interaction of charges with PD and year of admission were examined using one-way analysis of variance.
Results
There were 803 SV patients with 1333 admissions during the study period. Mean age was 24.8±6.2 years (54% male) and mean LOS was 6.8±11.3 days. Total hospital charges were $127 million with mean charge per admission of $95,501±192,068. Mean charge per hospital day was $14,765±16,574. The PD, number of admissions, hospital charges and LOS are shown in Table 1. Hospital charges correlated with PD group (p<0.001). Admission rate remained stable (∼180/year) from 2006 to 2011. LOS decreased (p<0.0308) and hospital charges per day increased across the study period (p<0.001).
Effect of Principal Diagnosis Group on Hospitalization in Adults with Single Ventricles (N=1287)
| Primary Diagnosis Group | Admissions Number (%) | Total Charges (Millions) | Hospital Charges Mean±SD | Length of Stay Mean±SD |
| Cardiovascular | 961 (72%) | $107 | $111,711±201,194 | 7.2±12.2 |
| Gastroenterologic | 86 (6%) | $4.5 | $52,901±91,734 | 6.4±8.2 |
| Infectious disease | 86 (6%) | $5.6 | $64,582±89,262 | 7.5±9.4 |
| Pulmonary | 50 (4%) | $4.9 | $97,889±279,819 | 8.5±12.8 |
| Neurologic & Otolaryngology | 41 (3%) | $0.9 | $24,099±32,795 | 3.1±3.0 |
| Hematology & Oncology | 34 (3%) | $0.9 | $26,909±25,965 | 4.0±4.8 |
| Fluid & Electrolyte | 18 (1%) | $0.3 | $19,141±12,781 | 2.8±2.6 |
| Rheumatologic & Orthopedic | 11 (1%) | $1.2 | $111,792±129,706 | 6.3±5.5 |
*
Indicates groups with ≥10 admissions
Conclusions
The costs of hospitalizations in adults with SV are significant and are impacted by comorbid medical conditions. Hospitalization rates for adults with SV are not increasing, though costs are.
ADULT AND PEDIATRIC CONGENITAL HEART DISEASE HOSPITALIZATIONS IN THE UNITED STATES
Author links open overlay panelJared MartinO’LearySarah deFerrantiOmarSiddiqiMichaelLandzbergAlexanderOpotowsky
Brigham and Women’s Hospital, Boston, MA, USA
Boston Children’s Hospital, Boston, MA, USA
Background
Congenital heart disease (CHD) incidence has remained stable but longevity has improved, resulting in a growing adult CHD population. Previous reports suggested a rise in US CHD hospitalizations from 1998-2005. It is unclear if those trends have continued and whether pediatric CHD admissions have changed in a similar way.
Methods
We identified CHD admissions to US hospitals, 1998-2009 using the Nationwide Inpatient Sample. Diagnostic codes for CHD identified cases, which were classified as simple, complex or unclassified. Sampling weights were used to produce national estimates of annual CHD admissions.
Results
Annual adult CHD hospitalizations increased from 72,656±5,258 in 2005 to 117,483±8994 in 2009 (61.7%;15.4%/year), maintaining the prior trend. There was a 215% increase in adults admitted with CHD from 1998 to 2009 (19.5%/year) while pediatric admissions increased 46.9% (4.3%/year). Admissions for simple, unclassified and complex defects grew at an annual rate of 26.3, 12.2, and 11.2% respectively among adults; for children equivalent figures were 7.0, −1.2 and 4.0%. The Figureshows admissions by year for adults and children stratified by complexity. Adults accounted for 42.2% of CHD admissions in 2009, up from 25.4% in 1998.
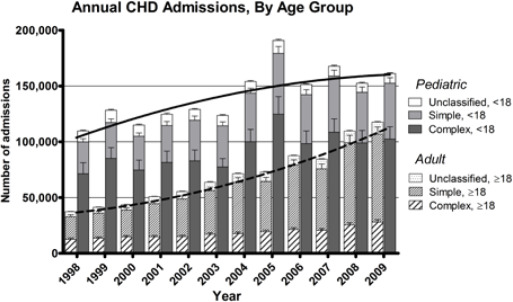
Conclusion
Growth in adult CHD hospitalizations has continued unabated and the number of adult admissions for CHD is approaching that of pediatric. Further research is warranted to effectively care for this emergent population of adults living with CHD.
CARDIOVASCULAR AND GENERAL HEALTH STATUS OF ADULTS WITH TRISOMY 21
Author links open overlay panelSamuel AllenHayesJoshuaThomasJoyceJohnsonAngelaYetman
Primary Children’s Medical Center, University of Utah, SLC, UT, USA
Background
There is a growing population of adults with Trisomy 21 (T21). Little data exists to assist practitioners in counseling patients and caregivers regarding expected long-term outcomes. We sought to assess cardiovascular status, as well as co-morbidities in this patient cohort.
Methods
A retrospective review of the electronic medical databases of 2 medical institutions with widespread coverage of the state was undertaken. Patients with a diagnosis of T21 who had a cardiology clinic visit or echocardiogram during 1995-2012 were identified. Patients of adult age (>21 years) were included. Demographic, surgical, and clinical variables were recorded. Correlates of adverse outcome defined as death, adult onset arrhythmia or heart failure, and adult cardiac surgery were sought.
Results
Ninety-four patients (49% female) with a median age of 30 (21-56) years and body mass index (BMI) of 29.1+7.6 m/kg2 were identified. Congenital heart defects (CHD) requiring surgery in childhood were present in 68 (72%) patients, minor defects in 13 (14%) and no CHD in 13. Of the 81 patients with CHD, 43 had an isolated atrioventricular septal defect(AVSD), 7 isolated tetralogy (ToF), 2 AVSD with ToF, 2 single ventricle, 17 a VSD, and 10 had other defects. Of the 68 patients requiring surgery, definitive repair was performed in only 53 (78%). Adverse outcome was present in 38 (40%). There were 8 adult deaths at a mean age of 41.4+6.2 years. Thirty patients required 2.2 (1-14) hospitalizations for cardiorespiratory disease in adulthood. Of the 53 post-operative patients, 25% required repeat surgery in adulthood. Co-morbidities included hypothyroidism in 42 (45%), dementia in 4 (4%), sleep apnea in 34 (36%), pulmonary hypertension in 37 (39%) and obesity in 36 (38%). Of the 22 (23%) patients developing late arrhythmias, 13 required implantable cardioverter defibrillator or pacemaker. Patients with an adverse outcome had a higher BMI (31.3 vs. 27.8 m/kg2, p=0.03), and were more likely to have pulmonary hypertension (71% vs. 23%, p<0.0001).
Conclusions
Adults with Trisomy 21 are living into their 6th decade and have a high incidence of arrhythmias, need for repeat cardiac surgery, and pulmonary hypertension.
MAJOR AORTOPULMONARY COLLATERAL ARTERY NOMENCLATURE
Author links open overlay panelClaudia A.AlgazeLynn F.PengJeffrey A.FeinsteinV. MohanReddyFrank L.HanleyStanton B.Perry
Stanford University School of Medicine, Palo Alto, CA, USA
Lucile Packard Children’s Hospital, Palo Alto, CA, USA
Background
The anatomic variability in tetralogy of Fallot with pulmonary atresia (PA) or pulmonary stenosis (PS) and major aortopulmonary collateral arteries (MAPCA) makes it difficult to compare outcomes for different therapeutic approaches. We developed a novel anatomy-based classification system and risk score for MAPCA’s.
Methods
A retrospective review identified 128 patients with tetralogy of Fallot/PS or PA/MAPCA with pre-operative angiograms adequate to identify number; origin: transverse aorta, descending aorta (DTA), abdominal aorta, subclavian artery, and coronary artery; type: dual supply, single supply (SS), mixed supply and patent ductus arteriosus; distribution: number and name of bronchopulmonary segments supplied; and stenoses.
Results
We identified 475 MAPCA and 17 patent ductus arteriosus. Each was assigned names using schemes of varying complexity. Using a simple scheme combining origin, type and number of segments supplied (e.g. DTA-SS-3) there are 78 unique names for the 475 MAPCA. With a more complex scheme combining origin, type, number and names of segments supplied (e.g. DTA-SS-3-R1-R2-R6); there are 244 unique names. Once the MAPCA are named, each patient is named by stringing the MAPCA names together. For example, a patient with 3 MAPCA’s (DTA-SS-5, DTA-SS-7, DTA-SS-6) is named DTA-SS-5-DTA-SS-7-DTA-SS-6. Even with this relatively simple scheme, 114/128 patients have unique names. These names are converted to a risk score using a formula with weighted factors for origin, type, number of segments, stenoses and maximum number of segments supplied by largest MAPCA. The 128 patients were divided into 5 groups: 1) only dual supply MAPCA, 2) patients with PS, 3) patients with patent ductus arteriosus and MAPCA, 4) combination of dual, single and mixed supply MAPCA and 5) only SS MAPCA. The risk scores for these 5 groups were 1) 19, 2) 26, 3) 41, 4) 50 and 5) 70.
Conclusion
For the individual patient, these naming schemes give a shorthand way to identify each patient, and ensure all relevant data is obtained pre-operatively. For groups of patients, the names and risk scores provide a way to risk-adjust groups and allow comparison of therapeutic approaches and outcomes.
COMPLICATIONS RELATED TO TRANSHEPATIC VENOUS ACCESS IN CHILDREN WITH CONGENITAL HEART DISEASE: A 12-YEAR SINGLE CENTER EXPERIENCE
Author links open overlay panelAthar M.QureshiLourdesPrietoSharonBradley-SkeltonLarryLatson
The Cleveland Clinic, Cleveland, OH, USA
Background
Children with complex congenital heart disease often have difficult central venous access as a result of prior procedures. In addition, there may a need to preserve their central veins for future cardiac catheterizations or surgeries. In many of these patients (pts.), transhepatic venous access is a vital modality for cardiac catheterizations and central venous access, however significant complications can occur.
Methods
The records of pts. who underwent transhepatic venous access between 6/2000- 10/2012 at The Center for Pediatric and Congenital Heart Disease at The Cleveland Clinic were reviewed. IRB approval was obtained for the study. Transhepatic access was obtained using biplane fluoroscopy in the majority of pts. and ultrasound in 2 pts.
Results
124 transhepatic procedures were performed in 81 pts. during the study period. The diagnoses included single ventricle circulations in 50, pulmonary atresia/VSD in 10, cardiomyopathy in 3, heart transplant in 2 and other complex biventricular circulations in 16 pts. The median weight of the pts.was 6.3 (2.2–94) kg. with a median age of 7 months (2 weeks-35 years). Diagnostic catheterizations were performed in 75, interventions in 39 and central venous line placement in 91 procedures (tunneled catheters n=80, non-tunneled catheters n=11). The median maximum sheath size inserted was 8 (4-14) French. There were 12 (10%) major complications (complete heart block requiring intervention n=6; bleeding requiring intervention and transfusion n=6, with 1 death as a result). Heart blockpersisted in 3 pts. (2 paced for 2 weeks and 1 month; and 1 with recovery 2 days later). Factors such as weight, age and maximum French size of sheath were not associated with complications. Diagnostic and interventional procedures were not associated with more complications compared with procedures involving central venous line placement alone (p= 0.7). There were 24 late deaths unrelated to the transhepatic prodedures.
Conclusions
Transhepatic access is an extremely vital modality of access to the heart and vascular structures in children with complex heart disease. Prevention of complications should focus on minimizing bleeding risks and heart block.
DELAYED SUCCESS OF BALLOON DILATION FOR COEXISTING valvar AND SUPRAVALVAR PULMONARY STENOSIS
Author links open overlay panelJohn JerryParentMarkHoyer
Indiana University School of Medicine, Indianapolis, IN, USA
Background
Balloon pulmonary valvuloplasty (BPV) is the treatment of choice for valvar pulmonary stenosis (PS) in children. Current practice favors surgical repair of moderate, severe, and symptomatic PS when a coexisting supravalvar component (SV) is present. This approach has been derived from the lack of immediate reduction in total pulmonary gradient (TPG) and right ventricular pressures from BPV, as well as adverse events related to the procedure. We evaluated the outcomes of children at a single institution who underwent BPV for PS and SV.
Methods
A retrospective analysis of outcomes in children with PS and SV following BPV was performed. Our cath database was searched for patients undergoing BPV for PS with both valvar and supravalvar components since 2004. Inclusion criteria: age < 19 years and no previous cardiac surgery.
Results
Twenty three patients were identified. Median age at BPV was 0.5 years (IQR 0.3-2). Surgery was avoided in 15/23 (65%) [Group 1] and required in 8/23 (35%) [Group 2] following BPV. Reasons for surgery were: persistent symptoms in 5/8 (63%) and worsening TPG in 3/8 (37%). Median time to surgery following BPV in Group 2 was 0.9 years (IQR 0.2-1.9). Group 1 had a mean baseline peak echo TPG of 60 mmHg (± 12) that decreased to 44 mmHg (± 10) following BPV (p <0.01). TPG by echo decreased further to 21 mmHg (± 13) at 3.6 years (± 2.2) following BPV (p<0.01). Group 2 had a mean baseline peak echo TPG of 68 mmHg (± 17). TPG was unchanged by 1st echo after BPV at 56 mmHg (± 13) and just prior to surgery at 63 mmHg (± 15), (p > 0.10). Mean RV/LV pressure ratio was higher in Group 2 versus Group 1 at baseline (0.89 vs. 0.75, p <0.05) and post-BPV (0.9 vs. 0.64, p<0.05). No adverse events related to BPV were observed.
Conclusions
BPV has minimal acute effect on PS with a SV component, yet long term benefits are achieved in most patients. BPV should be considered first line therapy given its safety and long term effectiveness. Continued close medical follow-up is necessary following BPV. Only those with persistent symptoms, near systemic right ventricular pressures, or worsening TPG should be referred for surgical repair. A higher RV/LV pressure ratio at cath confers a higher risk for future surgical intervention.
OXYGEN CONSUMPTION ASSUMPTIONS ARE INACCURATE IN YOUNG CHILDREN WITH COMPLEX CONGENITAL HEART DISEASE
Author links open overlay panelMichaelSeckelerRusselHirschRobertBeekmanBryanGoldstein
Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA
Background
Oxygen consumption (VO2) is necessary for the determination of blood flow and vascular resistance during cardiac catheterization. Since measurement of VO2 is cumbersome, most catheterization labs forgo VO2 measurement (M-VO2) in favor of an assumed VO2 (A-VO2) derived from predictive equations, with or without modification. We sought to identify factors associated with an inaccurate A-VO2.
Methods
Retrospective review of consecutive anesthetized cardiac catheterization patients with direct measurement of VO2 (CAi0V Airway Module, GE Healthcare) at a large quaternary care children’s hospital. A-VO2 was calculated using the LaFarge equation. A difference between A-VO2 and M-VO2 ≥ 20% was considered clinically relevant and defined an inaccurate A-VO2. Patients were stratified by age (< 3 and ≥ 3 years) as the LaFarge equation has not been validated for < 3 years of age. Factors evaluated included: patient status (outpatient vs. ICU), age, weight, heart rate, hemoglobin and cardiac diagnosis. Groups were compared using ?2 test. Logistic regression was used to identify risk factors for inaccurate A-VO2.
Results
Of the 370 patients analyzed, 234 (63%) were ≥ 3 years and 136 (37%) were < 3 years of age. ICU status and single ventricle anatomy were prevalent overall (16 and 23%, respectively) but more common in the < 3 years cohort (32% for each). A-VO2 was inaccurate more often in subjects < 3 years compared to older subjects (44% vs. 14%, p < 0.001). In subjects ≥ 3 years, multivariate regression identified lower hemoglobin (OR 1.2, p = 0.04) and ICU status (OR 3.5, p = 0.03) as factors predictive of inaccurate A-VO2. In subjects < 3 years, multivariate regression identified higher heart rate (OR 1.04, p = 0.002), ICU status (OR 4.8, p = 0.004) and single ventricle anatomy following stage I palliation (OR 5.4, p = 0.04) as factors predictive of inaccurate A-VO2.
Conclusions
Use of A-VO2 in young patients is frequently inaccurate and may lead to significant errors in determination of blood flow and vascular resistance. Young critically-ill and stage I palliated patients should have VO2 measured to assure accurate Fick calculations.
IMPACT REGISTRY: FIRST REVIEW OF COMMUNITY PRACTICE WITH RESPECT TO AORTIC AND PULMONARY VALVULOPLASTY
Author links open overlay panelJohn W.M.MooreRobertVincentRobertBeekmanLisaBergersenLeeBensonRalfHolzerKathyJenkinsRichardRingelJonathanRomeKristinaMcCoyGerardMartin
Rady Children’s Hospital, San Diego, CA, USA
Introduction
The IMPACT registry captures data on cardiac catheterizations in patients with congenital heart disease. Since inception in January 2011, IMPACT participation has increased to 65 congenital heart centers which have submitted 8889 reports of catheterization. These reports include data specific to Aortic Valvuloplasty(AV) and Pulmonary Valvuloplasty (PV).
Methods
From July 2011 until June 2012, 6834 catheterizations met IMPACT Data Quality Guidelines. Among these, reports of AV and PV were reviewed including hemodynamic data, procedural characteristics, and adverse events (AE).
Results
There were 105 (1.5%) AV; median length of stay (LOS) 1.0 day. Indications: gradient (86.7%), LV dysfunction (6.7%), symptoms (5.7%). Pre-procedure: median gradient was 60 mmHg; 1 or 2+ Al 91 (86.6%), > 2+ Al 7 (6.7%). AV performed in 97.1%. Single balloon used in 93.6%, stabilization in 74.3%. Post- procedure: gradient in single balloon: 40 in 29.0%; 1 or 2+ Al in 83.5%, >2+ Al 15.9%. AEs included arrhythmia in 8 (7.6%), requiring medication 1, cardioversion 2, pacemaker 2; bleeding or other events requiring transfusion 7 (6.7%); tamponade requiring drainage 1. Planned cardiac surgery performed in 3 patients; unplanned 1.
There were 243 (3.6%) PV; LOS 1 day. Indications: gradient (75.3%), RV dysfunction (11.1%), R to L shunting (7%), Symptoms (6.6%). Pre-procedure: median gradient was 47 mmHg, RVp/LVp 0.9. PV performed in 98.8%, Single balloon used in 95.1%, stabilization in 50.8%. Post-procedure: residual gradient in single balloon: 40 in 13.7%; 1 or 2+ PI 89.6%, >2+ PI 9.4%. AEs included arrhythmia in 11 (4.5%), requiring medication 7, cardioversion 2; bleeding or other events requiring transfusion 18 (7.5%); cardiac arrest 2, ECMO 2. Planned cardiac surgery in 11; unplanned 0.
Conclusions
Reported complication rates of AV are relatively low, but in many cases AV resulted in suboptimal gradient relief, (perhaps to avoid increasing Al). PV also has low reported complication rates and appears to have has better efficacy. Progression to > 2+ insufficiency was not a major problem in either group. There were no deaths reported.
IMPACT REGISTRY: FIRST REVIEW OF COMMUNITY PRACTICE WITH RESPECT TO AORTIC AND PULMONARY ARTERY STENTING
Author links open overlay panelJohn W.M.MooreRobertVincentRobertBeekmanLisaBergersenLeeBensonRalfHolzerKathyJenkinsRichardRingelJonathanRomeTraciConnollyGerardMartin
Rady Children’s Hospital, San Diego, CA, USA
Introduction
The IMPACT registry captures data on cardiac catheterizations in patients with congenital heart disease. Since inception in January 2011, IMPACT participation has increased to 65 congenital heart centers which have submitted 8889 reports of catheterization. These reports include data specific to stent implantation for treatment of Coarctation of the Aorta(CoA) and for treatment of Proximal Pulmonary Artery Stenosis
(PA).
Methods
From July 2011 until June 2012, 6834 catheterizations met IMPACT Data Quality Guidelines. Among these, reports of CoA and PA Stenting were reviewed including hemodynamic data, procedural characteristics, and adverse events (AE).
Results
There were 87 (1.3%) cath lab visits for CoA stenting; median length of stay (LOS) 1.0 day. Indications: gradient (43.7%), hypertension (32.2%), LV dysfunction (12.6%), appearance (10.3%). Pre-procedure: median gradient was 28 mmHg. CoA stent implanted in 97.9%. Post procedure: residual gradient: 20 in 2.9%. AEs included bleeding or other events requiring transfusion in 8 (9.3%), arrhythmia requiring medication in 2. Planned cardiac surgery performed in 4 (4.7%) patients; unplanned cardiac surgery in 1.
There were 87 (1.3%) cath lab visits for PA stenting; LOS 1 day. Indications: gradient (31.0%), RV hypertension/dysfunction (16.1%), PA flow discrepancy (24.1%), appearance (25.3%). Pre-procedure: RV/LV 0.6. PA stent implanted in 100%: LPA (71.4%), RPA (28.6%). Side branch jailing occurred in 7 (7.2%), and was intended in 6. AEs included arrhythmia in 3 (3.5%), requiring medication 1, cardioversion 1; bleeding or other events requiring transfusion 5 (5.8%); cardiac arrest 2. Planned cardiac surgery performed in 1 patient; unplanned in none.
Conclusions
Reported success rates of CoA and PA stenting are high and complication rates are low. No catastrophic vessel ruptures were reported, and there were no deaths.
PEDIATRIC RESOURCE EXPENDITURES IN CARDIAC SPECIALTY ENCOUNTERS (PRECISE): DEVELOPMENT OF A COST ADJUSTMENT MODEL FOR CONGENITAL CARDIAC CATHETERIZATION
Author links open overlay panelLisaBergersenKimberleeGauvreauJeanConnorCherylO’ConnellMelvinAlmodovarJamesDiNardoPujaBankaJohnMayer
Audrey Marshall, Children’s Hospital Boston, Boston, MA, USA
Background
To better understand costs related to catheterization for congenital heart disease we sought to develop tools to measure resource utilization.
Methods
A single institution catheterization database with prospectively collected case characteristics was linked to hospital charges related and limited to an episode of care in the catheterization lab (fiscal year 2008-2010). Cath cost categories (CCCs) were developed to group types of cath procedures using a combination of empiric data and judgment methodology. A multivariable model with outcome charges was created using CCC and additional case characteristics.
Results
In 3 fiscal years 3839 cases were available for analysis. 43 cath procedure types were categorized into 7 CCCs yielding a grouper variable with an R2 explanatory value of 72.6%. In the final CCCs, biopsy cases are isolated in the lowest category, CCC 1, and percutaneous pulmonary valve placement alone makes up CCC 7. As shown in Figure 1, the largest proportion of cases is in CCC 2 which includes diagnostic cases without intervention. The final model included CCCs, number of interventions, and cardiac diagnosis, R2=74.2%.
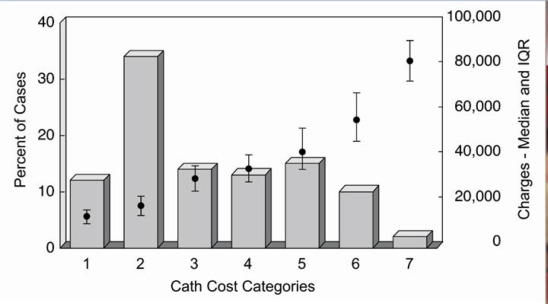
Conclusions
We have developed a catheterization procedure type cost grouper that accounts for the diverse case population encountered in catheterization for congenital heart disease. CCC and our multivariable model could be used to understand financial characteristics of a population at a single point in time, longitudinally, and to compare populations.
ATRIAL TACHYARRHYTHMIAS AFTER PERCUTANEOUS CLOSURE OF LARGE ATRIAL SEPTAL DEFECTS: INCIDENCE AND PREDICTORS
Author links open overlay panelFelipeHernandezLidia deSousaFedericoGimenoJose AntonioBazJose de la TorreHernandezAngelSanchez-RecaldeRosaHernandezFranciscoBosaArmandoBethencourtRobertoBlancoIgnacioCruz-GonzalezJuanRuiz-NodarRomanLezaunJavier GoicoleaRuigomezEduardoOliveira
Hospital 12 de Octubre, Madrid, Spain
Background
Percutaneous closure of atrial septal defects (ASD) is the preferred therapeutic approach in most patients, with high success rates and few complications. However, it is not clear the potential relation between device implant and the development of atrial tachyarrhythmias(AT), specially atrial fibrillation (AF), during follow-up, although a higher incidence has been described in elderly patients.
Methods
The multicenter REPERA registry included retrospectively 449 adult patients who had undergone a percutaneous ASD closure with large devices (>26 mm). All of them had a 12-lead ECG prior to the procedure. AT (or other symptomatic rhythm disturbances) were registered during follow-up.
Results
Mean age was 51±18 years (17-88), 63% female. Persistent AT (AF or atrial flutter) were present at baseline in 60 patients (13%), who where excluded from the analysis. Successful device implant was achieved in 358 out of 389 patients (92%), all of them in sinus rhythmprior to the procedure. Median follow-up has been 3.1 years (1.1-6.4). AT were documented in 33 patients (9.2%, 48% female), 5 cases in the first 24 hours and most of them in the first 3 months (79%). AF was the most common tachyarrhythmia (90%). There were no significant differences between patients with or without arrhythmias in device size (31.3 versus 31 mm) or age (51 versus 50 years). Logistic regression analysis showed that patients over 40 years had a significant higher incidence of AT (p<0.02) during follow-up. No case of advanced atrioventricular block was described.
Conclusions
The incidence of AT in adult patients after percutaneous closure of septal defects with large devices is significant. Most of them appear in the first weeks after the procedure, AF being the most common by far. Age over 40 years is a significant risk factor for the development of AT after device closure of ASD.
PULMONARY VALVE REPLACEMENT IN REPAIRED TETRALOGY OF FALLOT: ARE WE OPERATING EARLIER FOLLOWING RELEASE OF THE AHA/ACC GUIDELINES?
Author links open overlay panelMatthew J.LewisDanielO’ConnorJonathanGinnsMarlonRosenbaum
Columbia University, New York, NY, USA
New York Presbyterian Hospital, New York, NY, USA
Background
The timing of pulmonary valve replacement (PVR) in patients with repaired tetralogy of Fallot(TOF) and significant pulmonary regurgitation (PR) remains controversial. The AHA/ACC guidelines for Adult Congenital Heart Disease released in 2008 provided non-quantitative recommendations for PVR, although recent studies advocate PVR before indexed right ventricular end diastolic volume (RVEDVi) exceeds 160 ml/m2. We sought to determine whether the published ACC/AHA guidelines significantly affected the clinical or imaging characteristics of patients undergoing PVR.
Methods
We conducted a retrospective cohort study evaluating all patients seen at our adult congenital heart disease center (age≥18 years) with TOF who underwent PVR between 1/1/1999 and 6/1/2012. Variables based on prior studies and the AHA/ACC guidelines were defined prior to data acquisition and assessed immediately prior to PVR.
Results
Of 59 patients with TOF who had a PVR at our institution, 35 (59%) were before the release of the guidelines and 24 (41%) were after. All patients had a transthoracic echo upon presentation, and 49 of the 59 patients had a pre-operative cardiac MRI (CMR). All patients had moderate or severe PR. Median time to PVR from initial visit at our institution by log rank-test was significantly higher in the pre-guideline group (p= 0.005). Mean pre-operative right ventricular ejection fraction by CMR was significantly higher in patients who had a PVR after the guidelines (47% vs. 41%, p =0.03), as was pre-operative right ventricular functionby echocardiography (p=0.01). However, pre-operative mean RVEDVi was not significantly different between the pre and post guideline groups (194 ml/m2 vs. 175 ml/m2, p=0.24).
Conclusions
Patients with repaired TOF and significant PR who underwent PVR after the release of the ACC/AHA guidelines had a shorter time to surgery and better right ventricular function by TTE and CMR but no significant difference in degree of right ventricular dilation. Although the guidelines may have had a beneficial impact on time to referral, the absence of quantitative recommendations may explain the lack of reduction in RVEDVi in the post-guideline group.
PREDICTION OF CORONARY ARTERY DISEASE AMONG ADULT CONGENITAL HEART DISEASE PATIENTS USING FRAMINGHAM RISK SCORE
Author links open overlay panelJoshua R.ThomasNasirMushtaqAngelaYetmanMarkFox
Primary Children’s Medical Center, University of Utah School of Medicine, Salt Lake City, UT, USA
University of Oklahoma School of Community Medicine, Tulsa, OK, USA
Background
Risk assessment tools to predict coronary artery disease (CAD), such as the Framingham Risk Score (FRS), have been developed to assess various populations. The FRS evaluates cardiovascular (CV) risk factors including age, gender, BP, smoking status, diabetes, and lipid profile. The CAD risk among adults with congenital heart disease (ACHD) is currently unknown.
Methods
We assessed CAD risk among ACHD clinic patients. Cross-sectional analysis of data was performed. We evaluated the distribution of 10-year risk of CAD as a categorical variable and continuous variable. Ten-year risk of CAD was categorized into three categories (<10%, 10% to 20%, and >20%) and its distribution was examined with gender and age by Fisher’s exact test. For the continuous variable, analysis of variance and student’s t-test were conducted to examine differences in mean CAD risk across gender and age.
Results
Two-hundred and ten patients (41% Female) with a mean age of 34 (19-74) years were identified. The mean 10-year CAD risk for males was 4.64 (+/-3.99) and for females 2.39 (+/-3.18), with statistically significant differences among age and gender (Table 1). In contrast to previously reported data for the general population, there was in increase in the proportion of patients in the >10% risk categories among the ACHD patient population.
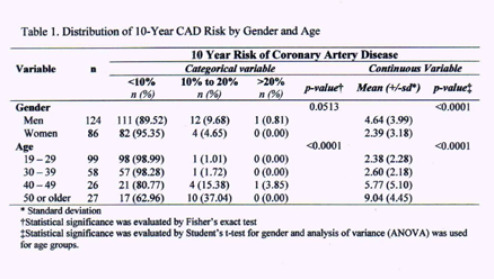
Discussion
Patients in the ACHD population are at a significant risk of CAD. The CV risk factors assessed in the FRS should be evaluated and positively modified among ACHD patients.
OUTCOMES OF CARDIAC RESYNCHRONIZATION THERAPY IN ADULT PATIENTS WITH SURGICALLY REPAIRED TETRALOGY OF FALLOT AND LEFT VENTRICULAR SYSTOLIC DYSFUNCTION
Author links open overlay panelDaneshKellaFaisalMerchantWendyBookJonathanLangbergMichael S.Lloyd
Emory University School of Medicine, Atlanta, GA, USA
Background
Although left ventricular (LV) systolic dysfunction is known to occur in adults with repaired Tetralogy of Fallot (TOF), the benefit of cardiac resynchronization therapy (CRT) in this cohort is not well described.
Methods
We retrospectively identified all patients with repaired TOF and impaired LV ejection fraction(LVEF ≤ 40%) undergoing CRT at our institution (n=10) and divided them into two groups: de novo CRT (Group A, n=6) or upgrade from existing device (Group B, n=4). Echocardiogramswere reviewed at baseline (pre-CRT) and medium-term follow-up (6-12 months).CRT response was defined as a reduction in LVESV ≥ 15% at medium-term follow-up.
Results
For all patients, age at surgical repair was 13.1 ± 16.0 yrs and age at CRT was 44.4 ± 12.5 yrs. Baseline LVEF was 24.0 ± 10.5%, New York Heart Association (NYHA) class 2.9 ± 0.6 and QRS duration 179.1 ± 36.3 msec. Group A demonstrated right ventricular (RV) conduction delay preponderance whereas all patients in Group B was RV paced at baseline. Time to medium-term follow-up was 10.4 ± 5.3 months. Group A showed significant improvements in LVEF, LVEDV and LVESV (Table). Group B also demonstrated a significant improvement in LVEF with favorable trends in LV volumes. Out of 9 patients with complete data at medium-term follow-up, 8 showed evidence of CRT response (Group A: 4/5; Group B: 4/4).
Conclusions
Adults with repaired TOF and LV systolic dysfunction demonstrate significant medium-term response to CRT, even among those with RV conduction delay.
| TABLE | Left ventricle ejection fraction (%) | ||
| Baseline | Medium-term | p | |
| Group A | 21.7 ± 11.3 | 32.0 ± 4.5 | <0.01 |
| Group B | 27.5 ± 9.6 | 42.5 ± 18.5 | 0.05 |
| Left ventricle end-diastolic volume (cc) | |||
| Baseline | Medium-term | p | |
| Group A | 251.5 ± 87.4 | 216.1 ± 86.5 | 0.03 |
| Group B | 272.0 ± 111.3 | 180.8 ± 42.1 | 0.16 |
| Left ventricle end-systolic volume (cc) | |||
| Baseline | Medium-term | p | |
| Group A | 193.7 ± 71.3 | 147.4 ± 55.5 | 0.03 |
| Group B | 228.1 ± 104.1 | 106.6 ± 5.7 | 0.09 |
ABILITY OF THE EUROPEAN SOCIETY OF CARDIOLOGY GUIDELINES TO PREDICT HAEMODYNAMICALLY SIGNIFICANT COARCTATION OF THE AORTA
Author links open overlay panelMikael G.DellborgMarcoAstengoCarolineBerntssonPeterErikssonValeriaFisichella
Dept of Medicine Sahlgrenska University Hospital Ostra, Goteborg, Sweden
Dept of Radiology Sahlgrenska University Hospital, Goteborg, Sweden
Background
In the setting of coarctation of the aorta (CoA), clinical symtoms and signs, exercise testingand imaging techniques help identify patients in need of intervention. Nonetheless, cardiac catheterization is still regarded as the gold standard for the evaluation of haemodynamically significant CoA. According to the European Society of Cardiology Guidelines (ESC), all patients with a non-invasive pressure difference >20 mmHg between upper and lower limbswith arterial hypertension, pathological blood pressure response during exercise, or left ventricular hypertrophy (LVH) should have intervention (class I recommendation, level of evidence C), while hypertensive patients with ≥50% aortic narrowing relative to the aortic diameter at the diaphragm level on imaging, should be considered for intervention (class IIa recommendation, level of evidence C).
Methods
Clinical, imaging and catheterization data of 42 consecutive subjects with CoA suspected to be haemodynamically significant and undergoing cardiac catheterization from October 1998 to November 2011 with complete clinical and catheterization data were reviewed retrospectively. The ability of Class I and IIa recommendations in identifying patients with a peak-to-peak pressure gradient ≥ 20 mmHg at catheterization was tested.
Results
42 cases were analysed, 31 were male (74%); mean age at cath 35.1 ± 4.8 years; 26 (62%) had native CoA; 26 (62%) bicuspid aortic valve; 3 (7%) left ventricular ejection fraction < 55%; 33 (79%) hypertension; 22 (52%) had LVH; and 23 patients (54.8%) had a peak-to-peak pressure gradient ≥ 20 mmHg. Combination of class IC and IIaC recommendations predicted a significant pressure gradient with a sensitivity of 0.87, specificity of 0.37, positive predictive value of 0.62 and a negative predictive value of 0.70. Overall diagnostic accuracy was 0.64.
Conclusions
Current ESCguideline critera to identify patients with CoA needing intervention performed poorly in predicting a significant pressure gradient at catheterisation. Further efforts are needed to develop a reliable noninvasive method to classify patients with CoA, thereby safely reducing the number of diagnostic catheterizations
HYPERTENSION PATTERNS POST AORTIC COARCTATION REPAIR
Author links open overlay panelCarlaCanniffeDavidCelermajerKevinWalsh
Mater Misericordiae Hospital, Dublin, Ireland, Our Ladys Childrens Hospital Crumlin, dublin, Ireland
Background
Up to 55% of patients who have undergone successful aortic coarctation repair develop late systolic hypertension, however the severity and patterns of this complication have not been well characterised.
Methods
All patients who had had coarctation repair and were ≥ 12 years old were eligible for inclusion. Patients had office and 24 hour ambulatory blood pressure (ABP) performed. Reports of recent cardiac imaging and cardiac risk factors were also recorded. Hypertensionwas defined as 24 hour mean BP >135/85mmHg or BP load ≥ 30% (adults) or >95th percentile for age and height (≤ 17years old).
Results
364 patients with a history of repaired aortic coarctation were identified. Those with complex congenital heart disease, a significant residual gradient across their aorta, significant developmental delay and pregnant patients were excluded. 16 patients did not wish to participate, leaving a cohort of 295 patients. To date 148 patients have been prospectively studied. Mean age 28.9 years (range 12-71 years; 65.5% of cohort between 18-39years). 46.2% male. 56.2% had bicuspid aortic valves. 48.9% had been repaired within the first 24 months of life. 43.7% were on prescribed anti-hypertensive medication at the time of enrolment. 27.8% were found to have systolic hypertension on ABP recordings. 26.6% had a blunted nocturnal dip of < 10% and 42.2% had white-coat hypertension. The median age of those with systolic hypertension was 29years (range 12-55 years). Male patients had a higher prevalence of hypertension compared to female patients (p=0.02). There was no significant difference between the age at repair/intervention and the presence of hypertension at follow up. Furthermore when we compared surgery (end to end anastomosis+ subclavian flap, number=98) to percutaneous intervention (Stent, number=34) there was no significant difference in hypertension prevalence at follow up (p=0.8114).
Conclusions
Despite anatomically successful repair of aortic coarctation, both white coat and confirmed hypertension are common in young adult survivors.
EARLY FIRST TRIMESTER FETAL ECHOCARDIOGRAPHY: IDENTIFICATION OF CARDIAC STRUCTURES BY 2D IMAGING AND COLOR DOPPLER FROM SIX WEEKS GESTATION
Author links open overlay panelDarrenHutchinsonAngelaMcBrienLisaHowleyYukaYamamotoAkikoHiroseTerekMotanVenuJainWinnieSavardLisa K.Hornberger
Stollery Childrens Hospital, Edmonton, Canada, University of Alberta, Edmonton, Canada
Background
Early fetal echocardiography (FE), performed at 12-16 weeks gestational age (GA), can be used to screen for fetal heart disease akin to that routinely done in the mid trimester. The effectiveness of very early FE prior to 12 weeks GA for cardiac screening is unclear. We sought to evaluate the efficacy of FE in assessing the fetal heart structure from 6-7 weeks GA.
Methods
From February 2009 we prospectively recruited pregnant women for first trimester FE for a variety of indications including increased nuchal translucency as well as healthy controls. All had 2 dimensional cardiac imaging combined with color Doppler (CD) assessment. Transabdominal scanning was used in all cases with transvaginal scanning used additionally in most cases prior to the 11th week GA (n=92/107, 86%).
Results
227 pregnancies undergoing first trimester FE were included for review. Mean GA at FE was 10+6 weeks (range 6+1 to 13+6 weeks). Significant improvement in image resolution of the fetal heart was gained with every advancing week of gestation. CD assisted with definition of cardiac anatomy at all gestational ages. A four-chambered heart could be identified in 53% of patients in the 8th week GA (n=10/19), improving to 80% (n=36/45) in the 10th week GA and 98% (n=57/58) in the 11th week GA. Both cardiac outflow tracts were imaged on B mode in the minority from 8+0 to 10+6 weeks GA (n=17/70, 24%) but could be imaged in most from 11+0 to 13+6 weeks GA (n=95/119, 80%). CD imaging improved identification of both the outflow tracts to 64% (n=29/45) in the 10th week GA. Crossing of the great vessels, using CD, could be demonstrated in the majority of cases in the 10th week GA (n=25/45, 51%) and improved to 90% in the 11th week GA. The inferior vena cava (IVC) could be identified on B mode imaging as early as 8 weeks GA (n=1/19, 5%). CD improved visualization of the IVC to over 80% from 10 weeks GA. Pulmonary veins were not visualized until after the 11th week GA.
Conclusion
Very early FE, from as early as 8 weeks GA, can be used to assess cardiac structures. The use of CD increases detection of cardiac structures in early FE significantly. Very early FE can be considered as a diagnostic tool in pregnancies with an elevated risk of congenital heart disease.
CHANGES IN CARDIAC SIZE AND FUNCTION IN CHILDREN WITH SINGLE RIGHT VENTRICLE ANOMALIES AFTER NORWOOD-RV REMODELING AFTER THE FIRST YEAR VARIES BY INITIAL SHUNT TYPE
Author links open overlay panelPeter C.FrommeltEricGerstenbergerJamesCnotaMerylCohenJessicaGorentzKevinHillJ. BlaineJohnJamiLevineJimmyLuWilliamMahleRachelMcCandlessLucMertensGailPearsonCarolynSpencerDeepikaThackerIsmeeWilliamsPierreWongJaneNewburger
Medical College of Wisconsin, Milwaukee, WI, USA
Background
We sought to compare changes in right ventricular (RV) size and function after the 1st year and prior to Fontan surgery in children with single RV anomalies enrolled in the Single Ventricle Reconstruction trial who underwent Norwood randomized to a modified Blalock-Taussig shunt (MBTS) vs. right-ventricle-pulmonary-artery shunt (RVPAS).
Methods
We compared the MBTS and RVPAS shunt groups with respect to core-lab echocardiographic indices of RV size and function, tricuspid valve (TV) and neo-aortic valve (NAV) dimensions and function, and aortic arch gradient from protocol exams at 14.3±1.2 months and 33.6±9.6 months (≤ 6 months before planned Fontan).
Results
233 subjects (111 MBTS; 122 RVPAS) had acceptable echoes at both time periods. At 14 months, there was no difference by shunt type for any measure. From the 14 mo to pre-Fontan echo, the MBTS group had stable indexed RV volumes and ejection fraction (EF), while the RVPAS group had significantly increased end-systolic volume (49.1±6.6 to 55±17.8 ml/BSA1.3, p=0.004) and decreased RVEF (44.2±3.1 to 40.9±6.7%, p=0.004). Indexed NAV area was similar in the shunt groups and became significantly smaller from 14 mo to pre-Fontan (z-score 6.8±2.9 to 5.7±2.5, p<0.001 for MBTS; 6.4±3.2 to 5.1±2.9, p<0.001 for RVPAS). Although the NAV remained markedly dilated pre-Fontan, > mild regurgitation was rare (<5%) and similar at both intervals for the 2 shunts. By the pre-Fontan study in both groups, indexed TV area also decreased, nearly normalizing in size (z-score 1.9±2.2 MBTS; 2.1±2 RVPAS). The incidence of ≥moderate TV regurgitation was stable and uncommon (18% at both intervals for both groups). Finally, aortic arch gradients were stable and usually less than 2 m/s pre-Fontan (1.7±0.5 m/s MBTS; 1.8±0.6 m/s
RVPAS).
Conclusion
Initial shunt type at the Norwood procedure influences RV remodeling during the 2nd and 3rd years of life prior to Fontan surgery in survivors with single RV anomalies; longer-term systolic RV function appears to deteriorate after the RVPAS. Encouragingly, NAV and TV size decrease in both shunt groups over time, and both valves continue to function well for most survivors, without progressive regurgitation before the Fontan.
FUNCTIONAL ASSESSMENT BY STRESS EXERCISE IN PATIENTS WITH ANOMALOUS AORTIC ORIGIN OF A CORONARY ARTERY: EXPERIENCE OVER 17 YEARS
Author links open overlay panelSilvana M.LawrenceCarlos M.MeryMuhammad S.KhanAmanda L.TateDiane W.ChenRajeshKrishnamurthyCharles D.Fraser
Baylor College of Medicine, Houston, TX, USA
Texas Children’s Hospital, Houston, TX, USA
Background
Anomalous aortic origin of coronary arteries (AAOCA) is the second most common cause of sudden cardiac death in young athletes and remains a challenging diagnosis with variable clinical and surgical approaches to management. We sought to review our 17-year institutional experience with functional assessment of these patients using stress exercise test.
Methods
Retrospective review of functional assessment by stress exercise, with or without myocardial perfusion, in patients with diagnosis of AAOCA and no other associated major congenital heart defects at our institution from 1995-2012.
Results
A total of 55 patients with AAOCA were identified, 36% female. Stress exercise test was performed in 27 (49%) and myocardial perfusion test (SESTAMIBI) in 14 (25%). ST-T changes were identified in 2 (7.4%) of 27 patients (one underwent surgery) and 3 (11%) had arrhythmias (SVT, second degree AV block and RBBB) during stress test. Of the 16 (29%) patients who underwent surgical intervention, 7 (44%) had SESTAMIBI performed, only one had perfusion abnormalities (anomalous right CA from the left). Of the 39 (71%) patients followed clinically, 7 (18%) had SESTAMIBI performed and only one had perfusion abnormalities (anomalous left CA from the right). All patients had normal systolic function by echocardiography. Follow up stress test was performed in 8 (50%) who underwent surgery (one with ST-T changes) and in 14 (36%) who were followed clinically (all normal). The presence of symptoms did not relate to abnormal findings on stress test. Patients continued to report symptoms after surgery, but no significant ischemic changes were identified on those who underwent functional assessment. Upon median follow up of 2 years, all patients remain alive with no major reported cardiac events.
Conclusions
Functional assessment by stress test with or without myocardial perfusion in patients with AAOCA has a low yield for positive
Results
Management strategies vary even within a single institution. A better understanding of the natural history of AAOCA in the young population and improved surrogate markers of risk are needed to help devise risk stratification and treatment algorithms in these patients.
RISK OF CONGENITAL HEART DISEASE IN RELATIVES OF PROBANDS WITH CONOTRUNCAL CARDIAC DEFECTS: AN EVALUATION OF 1622 FAMILIES
Author links open overlay panelShabnamPeyvandiEitanIngallStacyWoyciechowskiJenniferGarbariniLaura E.MitchellElizabethGoldmuntz
The Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Background
Current risk counseling for conotruncal cardiac defects (CTD) is based on empiric estimates from multiple studies. Sibling risk of congenital heart disease (CHD) is estimated to be 2-3% for lesions such as tetralogy of Fallot (TOF) and lower (1-2%) for transposition of the great arteries (TGA). We examined the risk of CHD in relatives of probands with CTD to assist in counseling practices.
Methods
1,622 probands with CTD and no reported chromosomal or genetic abnormalities were recruited sequentially. A three-generation pedigree was obtained for each proband by a genetic counselor detailing the presence and type of CHD in each family member. Risks and 95% confidence intervals (Cl) were calculated for subgroups of relatives based on degree of relationship and proband gender. In addition, crude odds ratios (OR) and 95% Cl were used to compare risks in subgroups of relatives defined by the proband’s cardiac anatomy, e.g. siblings of probands with normally related (TOF, ventricular septal defect, truncus arteriosus, interrupted aortic arch) versus malpositioned (D- and L- TGA, double outlet right ventricle) great arteries. For pairs of affected relatives, concordance rates were calculated for CTD specifically and for CHD in general.
Results
The risk for any type of CHD in relatives of probands with CTD was 3.3% in siblings (95% Cl: 2.6-4.1), and 1.5% (95% Cl: 1.2-2.1) in a parent, consistent with previous literature. The siblings of male probands had a higher risk (4.3%, 95% Cl: 3.2-5.7) than the siblings of female probands (2.5%, 95% Cl: 1.8-3.4). Risk was higher in siblings for probands with normally related great arteries as compared to probands with malpositioned great arteries (OR 2.5, 95% Cl: 1.4-4.5). When the proband had normally related great arteries, 73% of the affected siblings had a concordant lesion (ie CTD). In contrast when the proband had malposition of the great vessels, only 50% of the affected siblings had a concordant CTD.
Conclusions
These data suggest that risk of CHD is higher in siblings when the proband is male or has normally related great arteries. These data contribute to our understanding of the risk for CHD in the relatives of affected individuals.
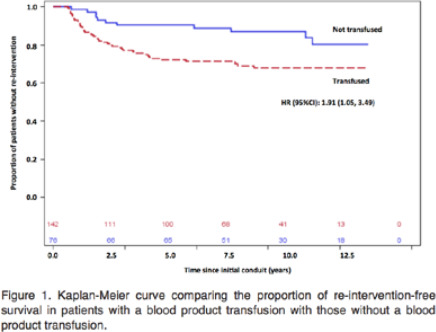
BLOOD TRANSFUSION: A NOVEL CULPRIT OF EARLY GRAFT FAILURE IN CHILDREN?
Author links open overlay panelKenneth Wei QiangGuoArianeMarelliMohammedKaouacheJudithTherrien
McGill Adult Unit for Congenital Heart Disease Excellence, Royal Victoria Hospital, Montreal, Canada
Department of Cardiology, Jewish General Hospital, Montreal, Canada
Background
The attrition of right ventricle to pulmonary artery (RV-PA) conduits has been attributed in part to the body’s immunologic response. We hypothesized that antibodies developed through blood transfusion, directed against the conduits, may result in accelerated degeneration and the need for re-intervention. We sought to analyze the association between transfusion exposure and conduit re-intervention.
Methods
This is a population-based study of the province of Quebec (Canada) with the observation period from January 1, 2000 to March 31, 2010. We included children born between January 1, 2000 to December 31, 2006 who were diagnosed with a cono-truncal anomaly and had an RV-PA conduit. The patients were followed for transfusion exposure and RV-PA re-intervention. Time to re-intervention in those exposed versus non-exposed was analyzed using Cox regression.
Results
There were 590 patients (58% males; median age at first RV-PA conduit was within the 1st year of life) who met the inclusion criteria. Patients who received a blood transfusion at the time of the initial conduit had near double the risk of a re-intervention compared to those who did not (hazard ratio of 1.913; 95% confidence interval, 1.05–3.49; P=0.0345).
Conclusion
In this population-based analysis, prior blood transfusion after the year 2000 was associated with a higher risk of an RV-PA conduit re-intervention. These data support the hypothesis that a blood transfusion mediated immune response may adversely impact conduit longevity.
BLOOD TRANSFUSION: A NOVEL CULPRIT OF EARLY GRAFT FAILURE IN CHILDREN?
Author links open overlay panelKenneth Wei QiangGuoArianeMarelliMohammedKaouacheJudithTherrien
McGill Adult Unit for Congenital Heart Disease Excellence, Royal Victoria Hospital, Montreal, Canada
Department of Cardiology, Jewish General Hospital, Montreal, Canada
Background
The attrition of right ventricle to pulmonary artery (RV-PA) conduits has been attributed in part to the body’s immunologic response. We hypothesized that antibodies developed through blood transfusion, directed against the conduits, may result in accelerated degeneration and the need for re-intervention. We sought to analyze the association between transfusion exposure and conduit re-intervention.
Methods
This is a population-based study of the province of Quebec (Canada) with the observation period from January 1, 2000 to March 31, 2010. We included children born between January 1, 2000 to December 31, 2006 who were diagnosed with a cono-truncal anomaly and had an RV-PA conduit. The patients were followed for transfusion exposure and RV-PA re-intervention. Time to re-intervention in those exposed versus non-exposed was analyzed using Cox regression.
Results
There were 590 patients (58% males; median age at first RV-PA conduit was within the 1st year of life) who met the inclusion criteria. Patients who received a blood transfusion at the time of the initial conduit had near double the risk of a re-intervention compared to those who did not (hazard ratio of 1.913; 95% confidence interval, 1.05–3.49; P=0.0345).
Conclusion
In this population-based analysis, prior blood transfusion after the year 2000 was associated with a higher risk of an RV-PA conduit re-intervention. These data support the hypothesis that a blood transfusion mediated immune response may adversely impact conduit longevity.
MATERNAL DIABETES AND CARDIOVASCULAR MALFORMATIONS IN THE NEWBORN: A POPULATION-BASED CASE-CONTROL STUDY
Author links open overlay panelPankajMadanMattBuasJeffrey R.JohnsonCrystalBonnichsenStephen M.Schwartz
Mayo Clinic, Rochester, MN, USA
University of Washington, Seattle, WA, USA
Background
Although maternal pre-gestational diabetes mellitus (PGDM) has been shown to be associated with infant cardiac malformations, the association of gestational diabetes mellitus(GDM) with cardiac malformations has been inconsistent. In addition, few studies have examined the relationship between maternal diabetes and specific types of infant cardiac malformations. The objective of this study was to assess the associations between maternal PGDM and GDM with the birth prevalence of specific subtypes of infant cardiac malformations.
Methods
A population-based case-control study was conducted using birth certificate data linked with maternal and infant hospital discharge data for delivery hospitalizations in Washington State from 1987 to 2009. 11,043 cases of cardiovascular malformations were frequency-matched by year of birth with 55,598 randomly selected controls. Stratified analyses were conducted to account for effect modification and confounding.
Results
The association of various forms of cardiovascular malformations with PGDM and GDM are shown in Table below.
| PGDM | GDM | |||
| Malformation type | Odds Ratio | 95% Cl | Odds Ratio | 95% Cl |
| All | 5.0 | 4.3–5.8 | 1.6 | 1.4–1.7 |
| Early | 6.3 | 4.1–9.6 | 1.2 | 0.8–1.7 |
| Laterality, looping | 5.4 | 2.4–12.4 | 1.2 | 0.6–2.3 |
| Outflow tract | 7.2 | 4.4–11.8 | 1.1 | 0.7–1.8 |
| Atrioventricular septal defects | 2.9 | 0.4–21.0 | 2.0 | 0.8–5.2 |
| Obstructive/shunting | 5.4 | 4.6–6.4 | 1.6 | 1.4–1.8 |
| L-sided obstructive | 8.7 | 5.8–13.2 | 2.2 | 1.6–3.0 |
| R-sided obstructive | 6.3 | 4.5–8.8 | 1.5 | 1.2–1.9 |
| L-to-R shunting | 4.9 | 4.0–6.0 | 1.6 | 1.4–1.8 |
| Ventricular septal defects | 3.7 | 2.8–4.9 | 1.3 | 1.1–1.5 |
Conclusions
Defects of primary cardiogenesis or early malformations (such as laterality and looping defects and outflow abnormalities) are associated with PGDM but not with GDM. Although both right and left sided obstructive lesions are associated with PGDM and GDM, the association for GDM is relatively weaker.