PERINATAL OUTCOMES AFTER FETAL DIAGNOSIS OF EBSTEIN ANOMALY OR TRICUSPID VALVE DYSPLASIA IN THE CURRENT ERA: A MULTI-CENTER STUDY
Boston Children’s Hospital, Boston, MA, USA
Background
Ebstein anomaly and tricuspid valve dysplasia (EA/TVD) are rare congenital tricuspid valve malformations associated with high perinatal mortality. The literature to date consists of small, single center case series often spanning several decades. We performed a multi-center study to assess perinatal outcomes after fetal diagnosis of EA/TVD in the current era.
Methods
Twenty-three centers contributed to this retrospective study, which included fetuses diagnosed with EA/TVD from January 1, 2005 to September 1, 2011. Fetuses with complex associated lesions, such as congenitally corrected transposition or left heart obstruction, were excluded. Among live-born patients, the primary outcome was survival to neonatal hospital discharge.
Results
We included 272 fetuses with EA/TVD diagnosed at a median gestational age (GA) of 25 weeks (interquartile range: 21-30). Nearly one-third developed hydrops, 15 (6%) had documented arrhythmias in utero, and 61 (22%) were known to have extracardiac anomalies and/or a genetic diagnosis. There were 17 elective terminations (6%), 48 fetal demises (18%) at a median GA of 30 weeks (26-33), and 12 fetuses (4%) lost to follow-up. Of the 195 live-born patients (72% of the initial cohort), 65 (33%) died prior to discharge. Eighteen (9%) patients died within 1 day of life, and among those surviving >1 day, the median age at death was 11 days (6-24). Neonatal non-survivors had lower GA and weight at birth than survivors (35.6 vs. 37.5 weeks; 2.4 vs. 3.0 kg; both p<0.001). Hydrops, intubation in the delivery room, inotropic support, and ECMO were associated with mortality (p<0.001), while neonatal interventional catheterization and cardiac surgery were not (p=0.9).
Conclusion
In this large, contemporary cohort of fetuses with EA/TVD, there was a higher proportion of live-born patients compared to prior series. However, neonatal mortality remained significant and was associated with prematurity, lower birth weight, and the need for more intensive medical therapy. Anatomic and physiologic characteristics as assessed by fetal echocardiography will likely help further delineate predictors of poor outcome in this population.
A POTENTIAL STRATEGY FOR STIMULATING MYOCARDIAL REGENERATION IN INFANTS
Author links open overlay panelBrian DavidPolizzottiBalakrishnanGanapathyStuartWalshSangitaChoudhuryDavidBennettBernhardKuhn
Boston Children’s Hospital, Boston, MA, USA
Harvard Medical School, Boston, MA, USA
Background
Infants with congenital heart diseases (CHD) frequently lack sufficient myocardium and show scar formation. Therapies aimed at regenerating myocardium would change the way CHD is treated. We have shown that administration of recombinant neuregulin-1 (rNRG1) can stimulate heart muscle regeneration in adult mice following myocardial infarction. We hypothesized that the efficacy of rNRG1 therapy may be higher in the neonatal population and may provide a strategy to regenerate myocardium in infants with CHD.
Methods
We developed a myocardial injury model (cryoinjury) in neonatal mice that recapitulates scar formation seen in infants with CHD and used it to evaluate the effectiveness of stimulating cardiomyocyte proliferation with rNRG1. We also evaluated the ability of rNRG1 to stimulate cardiomyocyte proliferation in cultured myocardium from infants with CHD.
Results
(1) Administration of rNRG1 from four to 34 days after cryoinjury in neonatal mice resulted in a 2-fold increase in cardiomyocyte cell cycle activity at 10 days post injury (dpi), transiently reduced scar formation, and transiently improved myocardial structure and function. In contrast, administration of rNRG1 from birth to 30 days of life significantly improved the ejection fraction that was sustained up to 30 days after the cessation of rNRG1 administration. (2) rNRG1 induced cardiomyocyte proliferation in organotypic cultures of myocardium from infants with Tetralogy of Fallot (ToF). rNRG1-stimulated cardiomyocyte cell cycle activity decreased with infant age, with no proliferation occurring in patients older than 6 months.
Conclusions
These results indicate a potential strategy for stimulating myocardial repair in human infants based on early administration of rNRG1 to stimulate cardiomyocyte proliferation.
COMPARISON OF LYMPHATIC ABNORMALITIES IN PATIENTS WITH PROTEIN LOSING ENTEROPATHY AND PLASTIC BRONCHITIS
Author links open overlay panelYoavDoriMarcKellerAndrewGlatzMatthewGillespieDavidGoldbergMatthewHarrisMarkFogelKevinWhiteheadJonathanRomeJackRychikMaximItkin
The Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Background
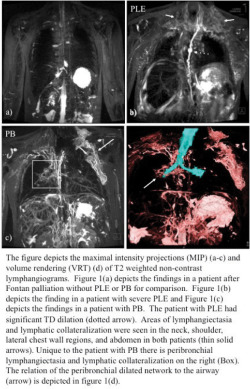
Lymphatic abnormalities are thought to play a key role in two complications of Fontan palliation: protein losing enteropathy (PLE) and plastic bronchitis (PB). However, to date, these abnormalities have been poorly characterized.
Methods
We reviewed imaging data for the presence of thoracic duct (TD) dilation, lymphangiectasia, lymphatic collateralization, and tissue edema from patients with PLE or PB who underwent T2 weighted MR lymphatic mapping in our institution over the past year.
Results
There were 12 Fontan patients in this study including 6 patients with PLE and 6 with PB. All the patients in this study had lymphangiectasia (100%), lymphatic collateralization (100%), and tissue edema (100%). All patients with PB (100%) had significant peribronchial lymphatic collateralization and dilation not present in any of the PLE patients (0%). Relative to the patients with PB the patients with PLE had more significant TD dilation with a larger TD maximal diameter (median 6.05 mm (range 3.5-7.2 mm) versus 2.42 mm (range 2-3.2 mm)) (p<0.01). These findings are not seen in Fontan patients without PLE or PB.
Conclusions
Lymphatic abnormalities are common in patients with PLE and PB. PLE patients have a characteristic TD dilation not seen in patients with PB. Peribronchial dilated lymphatic networks are seen in all patients with PB, which are not present in any of the patients with PLE. Our findings shed new light on the lymphatic system in these patients and warrant additional investigation.
PREDICTIVE VALUE OF BIOMARKERS FOR HEPATIC FIBROSIS IN THE ADULT FONTAN PATIENT
Author links open overlay panelFredWuMichaelEaringJamilAboulhosnMichaelSinghRobertOdzeChinweikeUkomaduMelanie E.JohncillaKimberleeGauvreauAnne MarieValenteMichaelLandzberg
Alliance for Adult Research in Congenital Cardiology (AARCC) Investigators, Boston Children’s Hospital, Boston, MA, USA
Background
Hepatic fibrosis is highly prevalent among adults with single ventricles and Fontan physiology. Few data exist to guide screening for liver disease in this population. Biomarkers, such as FibroSURE and hyaluronic acid (HA), are validated tests for hepatic fibrosis in viral hepatitis, alcoholic liver disease and non-alcoholic fatty liver disease. We sought to explore whether these tests can identify individuals with Fontan circulation who have advanced hepatic fibrosis or cirrhosis.
Methods
Subjects from the Alliance for Adult Research in Congenital Cardiology (AARCC) Fontan Liver Health study were enrolled who had liver biopsy and FibroSURE or HA testing within 6 months of biopsy. All biopsies were reviewed independently by two pathologists, and correlations between these biomarkers and hepatic fibrosis or cirrhosis were sought.
Results
Twenty-seven subjects were enrolled from three adult congenital heart disease centers. Median age was 26.8y (range 17.4 to 59.8). Median time since Fontan surgery was 20.4y (12.0 to 31.3). All subjects had an atriopulmonary connection (56%) or lateral tunnel Fontan (44%). None had known hepatitis C infection. FibroSURE score (>0.21) was elevated in 91% of subjects and was suggestive of cirrhosis (>0.74) in 13%; a similar distribution was seen in previous studies of Fontan patients. HA suggested cirrhosis (>46 ng/mL) in 18% of subjects. On histopathology, 42% of subjects had severe portal fibrosis with cirrhotic nodules; sinusoidal fibrosis involving >2/3 of sinusoids was seen in 63%. FibroSURE score and HA did not correlate with degree of portal or sinusoidal fibrosis and did not predict cirrhosis. FibroSURE, but not HA, correlated strongly with MELD-XI score (rs=0.6, p=0.006); neither correlated with peak VO2.
Conclusions
Abnormal biomarkers for hepatic fibrosis, and hepatic fibrosis or cirrhosis on biopsy are common in adults with Fontan circulation. FibroSURE and HA do not accurately predict degree of histopathologic hepatic fibrosis in these patients. FibroSURE correlates with MELD-XI score, a known predictor for adverse outcomes in Fontan patients. Further studies are needed to guide surveillance of liver disease in this population.
MAGNETIC RESONANCE ELASTOGRAPHY: A NOVEL TECHNIQUE FOR DETECTION OF HEPATIC CIRRHOSIS AND HEPATOCELLULAR CARCINOMA AFTER THE FONTAN OPERATION
Author links open overlay panelJosephPoteruchaJonathanJohnsonCrystalBonnichsenSabrinaPhillipsPatrickKamathPhillipYoungSudhakarVenkateshCaroleWarnesFrankCetta
Mayo Clinic, Rochester, MN, USA
Background
Hepatic dysfunction after the Fontan operation may have an indolent subclinical course. Magnetic resonance elastography (MRE) is a novel screening tool for noninvasive detection of hepatic fibrosis and cirrhosis. Our study aim was to evaluate feasibility of performing MRE to screen patients (pts) for hepatic cirrhosis after Fontan.
Methods
23 pts with prior Fontan operation (male = 11, mean age 30 ± 13 years [median = 26]) were evaluated. Liver MRE was performed with standard methodology using a mechanical driver in conjunction with cardiac MRI adding only 5 minutes to the entire study. Liver stiffness was calculated on automatically generated stiffness maps. Mean liver stiffness in kilopascals (kPa) was correlated with time elapsed since initial Fontan operation, and MR findings suggesting cirrhosis and hepatocellular carcinoma were recorded. Values > 5 kPa were considered indicative of cirrhosis.
Results
All pts had elevated liver stiffness, mean = 5.3 ± 1.2 kPa (4.8 – 5.9). Overall mean duration between Fontan and MRE was 21 ± 5.5 years (median = 23). Duration was longer with atrio-pulmonary (AP) (24 ± 2.6 years, median = 25) than lateral tunnel and extracardiac Fontan (18 ± 4.6, (median = 16) (p = 0.01). Pts with AP type had increased liver stiffness compared to pts with lateral tunnel or extracardiac type (5.9 ± 1.5 versus 4.6 ± 0.8 kPa; p = 0.006). The degree of liver stiffness was associated with time since operation (r = 0.45, p = 0.04). Anatomic imaging revealed cirrhosis (13), advanced fibrosis (3), and enhancing nodules (6). Two subjects (age 26 and 22 years old [5.9 kPa and 8.3 kPa]) with enhancing nodules had biopsy proven hepatocellular carcinoma.
Conclusion
MRE-derived liver stiffness is increased to values consistent with cirrhosis at a mean of 21 ± 5.5 years (median = 23) after Fontan operation. There was a strong positive correlation between patient age and degree of liver stiffness and cirrhosis. AP type Fontan may indicate a higher risk of cirrhosis, though this is more likely due to longer duration since surgery. MRE may be useful to identify pts at risk of cirrhosis and complications after Fontan operation and can be accomplished as an efficient and cost effective adjunct to cardiac MRI.
EFFECTS OF BOSENTAN ON PEAK OXYGEN CONSUMPTION, HEMODYNAMICS AND FUNCTIONAL CLASS IN FONTAN PATIENTS: A RANDOMIZED, PLACEBO CONTROLLED, DOUBLE BLIND STUDY
Author links open overlay panelAnders HedeboeHebertUlla R.MikkelsenUlfThilenLarsIdornAnnette S.JensenEditNagyKatarinaHanseusKeld E.SorensenLarsSondergaard
Copenhagen University Hospital, Rigshospitalet, Copenhagen, Denmark
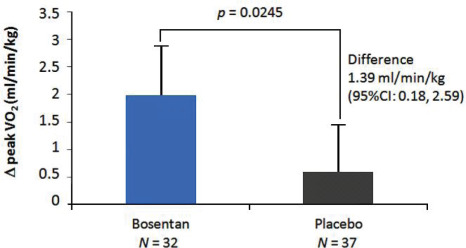
Background
The Fontan procedure has greatly improved survival for children with univentricular heart. However, complications such as reduced exercise capacity are seen more frequently as these patients get older. Several factors have been suggested responsible for the exercise intolerance e.g. a mild elevation in pulmonary vascular resistance. The aim of this study was to examine the safety and effect of the pulmonary vasodilator Bosentan on exercise capacity in clinically stable Fontan patients.
Methods
Seventy-five patients ≥12 years were randomized 1:1 to oral Bosentan or placebo for 14 weeks. Patients and investigators were blinded to randomization. At baseline and after treatment, the patients underwent exercise test and functional classification.
Results
Sixty nine patients (92 %) completed the study. The primary endpoint peak oxygen consumption increased in the Bosentan group compared to placebo (1.99 vs. 0.60 ml/kg/min, p=0.02). The improvement was supported by higher peak pulmonary blood flow(0.86 vs. 0.29 l/min, p=0.03) and longer exercise duration (28.2 vs. 4.8 seconds, p=0.04). Nine patients improved one functional class in the Bosentan group vs. none in the placebo group, p=0.0085. No serious adverse effects were seen and no patients had liver enzyme levels at or above three times the upper reference limit.
POST-OPERATIVE TRICUSPID REGURGITATION IN ADULT CONGENITAL HEART SURGERY IS ASSOCIATED WITH ADVERSE OUTCOMES
Author links open overlay panelMatthew J.LewisJonathanGinnsSiqinYeMarlonRosenbaum
Columbia University Medical Center, New York, NY, USA
Background
While tricuspid regurgitation (TR) is common in adults with congenital heart disease, there is no data to guide management when surgery is performed in conjunction with other indications. We sought to assess the determinants of mortality, repeat intervention, and post-operative (post-op) TR in this population.
Methods
We performed a retrospective cohort study of all adult patients with ≥moderate TR who underwent congenital heart surgery for non-TR indications between 1/1991 and 12/2012. Patients with a single ventricle, Ebstein’s anomaly, or congenitally corrected transposition of the great vessels were excluded. Groups were defined as: a) Tricuspid valve (TV) replacement, b) TV repair, and c) no TV intervention. Degree of post-op TR was determined at all available time points up to 3 years after surgery. Current status was determined using the social security death index. The primary outcome of interest was a composite of death, transplant, or re-operation of the TV.
Results
Of the 1194 adult patients with congenital heart disease who underwent surgery at our institution, 94 (8%) met inclusion criteria. Prior to surgery, 48 (51%) had moderate TR, 20 (21%) had moderate-severe TR, and 26 (28%) had severe TR. 59 (63%) patients underwent TV repair, 7 (7%) underwent TV replacement and 28 (30%) did not have a TV intervention. 17 patients (12%) reached the primary endpoint and 34 (36%) patients had ≥moderate post-op TR. Using a Cox-proportional hazard model, ≥moderate post-op TR was associated with a 7-fold increase in the rate of death, transplant or re-operation (p=0.013). Type of TV intervention was not significantly associated with the primary end-point (p=0.12). By logistic regression, patients who did not have a TV intervention were two-times more likely to have ≥moderate TR post-op (p=0.04).
Conclusion
≥Moderate TR following congenital heart surgery is associated with a significant increase in the odds of death, transplant or repeat surgical intervention. Patients with ≥moderate pre-op TR who did not have TV intervention had a greater degree of post-op TR. These results suggest that patients with ≥moderate TR may benefit from tricuspid intervention at the time of surgery.
CURRENT RESULTS OF THE MELODY REGISTRY: AN INTERNATIONAL MULTICENTER REGISTRY OF TRANSCATHETER PULMONARY VALVE IMPLANTATION
Author links open overlay panelJohannesNordmeyerPeterEwertMarcGewilligMarioCarminatiAnselmUebingLeeBensonDietmarSchranzIngoDaehnertMansourAljufanOliverKretschmarFelixBergerOn Behalf of the MELODY Registry Investigators
German Heart Institute Berlin, Berlin, Germany
Background
To assess the acute and One-Year clinical outcomes of transcatheter pulmonary valveimplantation (TPVI) in a multicenter registry (MELODY Registry).
Methods
Between 12/2006 and 09/2013, 1,003 patients (mean age 21.5±11.4 years) underwent TPVI in 40 cardiac centers. Indications for treatment were predominant stenosis (54%), predominant regurgitation (21%), or combined stenosis and regurgitation (25%). We retrospectively analyzed procedural details, clinical and echocardiographic outcome parameters. The primary outcome was freedom from death / reoperation / reintervention at One-Year (all-cause and TPVI-related); for this analysis, 694 patients were included who reached One-Year follow-up. Secondary outcomes included procedural complication rates, rates of endocarditis and stent fractures at One-Year, as well as echocardiographic parameters of TPV device performance (peak right ventricular outflow tract (RVOT) velocity and percentage of patients with significant pulmonary regurgitation (PR) of grade greater than 2).
Results
The invasively measured right ventricular systolic pressure fell from 62±18 mmHg to 43±12 mmHg (p<0.0001) and so did the percentage of patients with significant PR of grade greater than 2 (pre: 49% to immediate post-intervention: 1%, p<0.0001). Procedural complications occurred in 2.7% (major) and 11.9% (minor) of TPVI procedures, respectively. The One-Year freedom from the combined endpoint was 92.5% for all-cause events and 94.2% for TPVI-related events. At One-Year, the rate of endocarditis was 2.7% and the rate of stent fractures was 11%. There was sustained hemodynamic performance of the TPVI device at One-Year when compared to immediate post-intervention (peak RVOT velocity: 2.5±0.7 versus 2.6±0.6 m/s; PR of grade greater than 2: 1% versus 2%).
Conclusion
The multicenter MELODY Registry represents the largest patient series after TPVI to date with a follow-up of One-Year and offers the great potential for longer clinical observations of this patient population. The analysis of the current data confirms the safety and effectiveness of TPVI in clinical practice utilizing the Melody valve.
RIGHT VENTRICULAR RESTRICTIVE PHYSIOLOGY IS ASSOCIATED WITH EXERCISE PERFORMANCE AND PULMONARY INSUFFICIENCY: A CROSS SECTIONAL STUDY OF ECHOCARDIOGRAM, CARDIAC MAGNETIC RESONANCE AND EXERCISE PERFORMANCE IN REPAIRED TETRALOGY OF FALLOT
Author links open overlay panelLauraMercer-RosaMarkFogelStephenParidonJackRychikWeiYangElizabethGoldmuntz
The Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Background
Antegrade diastolic flow (ADF) in the pulmonary artery with atrial systole is thought to reflect restrictive right ventricular physiology in repaired tetralogy of Fallot (TOF). ADF is believed to have an inverse association with pulmonary insufficiency and to improved exercise performance. Alternatively, restrictive physiology may impede ventricular filling, resulting in worse exercise performance. To test these competing possibilities, we studied whether ADF was associated with pulmonary insufficiency, RV volumes and exercise performance.
Methods
138 repaired TOF patients (mean age 12.5 ±3.1 years, range 8-18.9) recruited to a cross sectional study underwent an echocardiogram, cardiac magnetic resonance (CMR) and exercise stress test. ADF was detected on echocardiogram by spectral Doppler of the main pulmonary artery. On CMR, ADF and pulmonary artery regurgitant fraction were measured by flow phase velocity mapping. Cases were divided into ADF-positive (ADFpos) and ADF-negative (ADFneg) groups. Exercise testing was performed on cycle ergometry with expired gas.
Results
CMR detected ADF more often than echocardiograms [96 (70%) versus 76 (55%) cases, respectively]. Aerobic capacity measured by peak oxygen consumption was decreased for the study group overall (76±18% of predicted). The ADFpos group had slightly superior diastolic function with E/E’ ratio 5.3± 2.1 vs. 7.2± 3.1 (p=0.0001), more pulmonary insufficiency and dilated right ventricles (regurgitant fraction 39±13% vs. 20±18 %, p<0.0001; 129 ±33cc/m2 vs. 95 ±26 cc/m2, p <0.0001, respectively) and better aerobic and physical working capacity (79 ±17 % of predicted oxygen consumption vs. 72± 18%, p=0.02 and 89± 22% vs. 77 ±21 % of predicted work, p=0.01, respectively). Finally, 67% of the ADFpos attained a maximal effort on exercise testing compared to 33% of the ADFneg, p<0.0001. Results trended in the same direction when analysis was restricted to those who achieved a maximal effort.
Conclusions
ADF is associated with more pulmonary insufficiency and superior exercise performance in this cohort. The clinical significance of ADF and its relationship to RV restrictive physiology remains to be defined.
RISK FACTORS FOR SUDDEN DEATH IN CHILDREN WITH CARDIAC ALLOGRAFT VASCULOPATHY
Author links open overlay panelBorah J.HongKristenSexsonAamirJeewaAntonioCabreraJackPriceJeffreyHeinleWilliamDreyerSusanDenfield
Baylor College of Medicine, Houston, TX, USA
Background
Cardiac allograft vasculopathy (CAV) is a frequent cause of late mortality in pediatric heart transplant patients. Many do not survive to retransplantation, and a subset die suddenly. This study evaluates factors associated with sudden death (SD) in pediatric patients with CAV.
Methods
This is a single center retrospective review of all pediatric patients transplanted from 1984 to 2012 who died or were retransplanted due to CAV. The CAV diagnosis was made by coronary angiography, explant pathology, or autopsy. Demographics, episodes of rejection, cardiac catheterization and echocardiographic data, time to CAV and death, and cause of death were compared in SD patients to those dying of heart failure.
Results
Of the 54 patients with CAV, 40 died or underwent retransplantation (RT), and 14 are alive. Three patients were excluded for noncardiac or unknown causes of death. Of the 37 patients who met inclusion criteria, 9 patients (24%) died suddenly. The other 28 patients died of heart failure (12/28 patients) or were retransplanted (16/28 patients). The SD and the heart failure death/RT groups did not differ in age at transplant, episodes of cellular or antibody mediated rejection, or time to CAV or death. Systolic function was better in the SD group with a median ejection fraction of 62% (range 50-70%) versus 50% (range 24-75%) in the heart failure death/RT group (p<0.05). Hemodynamics also differed, with a median right ventricular end diastolic pressure of 8 mmHg (range 3-16 mmHg) in the SD group versus 14 mmHg (range 4-24 mmHg) in the heart failure death/RT group (p<0.02), and a median pulmonary capillary wedge pressure of 9 mmHg (range 4-16 mmHg) in the SD group versus 13.5 mmHg (range 7-27 mmHg) in the heart failure death/RT group (p<0.04). B-type natriuretic peptide (BNP) levels before death or retransplantation were lower in the SD group with a median of 260 pg/ml (range 81-953 pg/ml) versus a median of 1081 pg/ml (range 207-5258 pg/ml) in the heart failure death/RT group (p<0.02).
Conclusions
Sudden death occurred in 24% of CAV associated patient or organ deaths. The SD patients were more likely to have normal hemodynamics and a lower BNP. Normal hemodynamics are not reassuring in the setting of CAV.
INCIDENCE AND CHARACTERISTICS OF ARRHYTHMIAS IN PEDIATRIC PATIENTS WITH MYOCARDITIS: A MULTICENTER STUDY
Author links open overlay panelLeonardoLibermanBrettAndersonEric S.SilverRakeshSinghMarc E.Richmond
Morgan Stanley Children’s Hospital of New York-Presbyterian, Columbia University Medical Center, New York, NY, USA
Background
Myocarditis in children is a cause of significant morbidity and mortality. Multiple prognostic factors have been identified to predict the outcome of these patients (pts). We tested the hypothesis that pediatric pts with tachyarrhythmias during hospitalization for acute myocarditis have worse outcome.
Methods
We performed a retrospective cohort study, using the Pediatric Health Information System (PHIS); an administrative database based on ICD-9 codes from 43 tertiary care hospitals. Data were obtained for all children, ≤ 18 y/o, discharged between 1/1/2004 and 3/31/2013, with a diagnosis of myocarditis. A clinical significant tachyarrhythmia (TACH) was defined as a subject with ventricular (VT) or supraventricular tachycardia (SVT), atrial flutter (AF) or fibrillation (Afib) in which an antiarrhythmic medication was used or a cardioversion was coded. Primary analysis was performed with univariate and multivariate logistic regression modeling of the composite primary outcome of cardiac arrest, mechanical circulatory support or death. A p value of <0.05 was considered statistically significant.
Results
There were 2148 pts identified. Mean age: 8.3 ± 6.9 years. Males: 1305 (61%). There were 411 (19%) pts with the composite outcome [236 pts (11%) had a cardiac arrest, 281 (13%) required mechanical circulatory support and 182 (8.5%) died]. The median hospital length of stay was 8 days (IQR: 3 – 17). There were 1575 pts (73%) admitted to the ICU. Pts that had TACH had longer hospital stay (p<0.001), ICU stay (p<0.001) and higher hospital cost(p<0.001) than pts without TACH. VT was the most common TACH (239 pts, 11%), followed by AF (34 pts, 1.6%), Afib (22 pts, 1 %) and SVT (19 pts, 0.9%). Pts with TACH were more likely to experience the composite outcome than pts without it (53% vs. 15%, p<0.001). TACH was associated with the composite outcome when controlling for age, sex, use of inotropic support, steroids, IVIG, congenital heart disease and the presence of an identified virus (OR: 5.4, 95% CI: 3.9 – 7.4, p<0.001).
Conclusions
The presence of TACH in pediatric pts admitted with myocarditis is associated with longer hospitalization, higher cost and is an independent predictor of poor outcome.
IN-HOSPITAL MORBIDITY AND MORTALITY OF SUPRAVENTRICULAR TACHYCARDIA AND COMPLETE HEART BLOCK AMONG INFANTS WITH STRUCTURALLY NORMAL HEARTS
Author links open overlay panelChristinaMiyakeShirazMaskatiaJeffreyKimShaineMorris
Texas Children’s Hospital, Houston, TX, USA
Background
Supraventricular tachycardia (SVT) and complete heart block (CHB), in the absence of congenital heart disease (CHD), are thought to be rarely associated with adverse outcomes in the first year of life, although data is limited. We investigated inpatient morbidity and mortality in a large cohort of infants with SVT and CHB.
Methods
The Texas Inpatient Public Use Data File, which contains administrative data on nearly 100% Texas hospital admissions, was queried from 1999-2012. Inclusion criteria were age less than 365 days and a diagnosis of SVT or CHB using designated ICD9 codes. Infants with CHD or atrial flutter were excluded. Patient characteristics and adverse outcomes were collected.
Results
Among 5,538,002 total infant admissions, complete heart block was present in 60 and SVT in 452. Of the 452 SVT admissions, treatment in the intensive care unit (ICU) was required in 115 (25%) and electric cardioversion in 17 (4%). Cardiogenic shock was diagnosed in 13 patients (3%), cardiac arrest in 3 (1%), and 3 required extracorporeal membrane oxygenatorsupport. Pre-term infants accounted for 19% of admissions. Among these 84 infants, there were 10 with brain hemorrhages (12%) and 1 with necrotizing enterocolitis (NEC) (1%). Among the 368 term infants, there were 5 with acute renal failure (1%), 1 ischemic stroke(0.3%), 6 brain hemorrhage (2%), 2 seizures (0.5%), and 4 NEC (1%). A total of 5 infants (1%), 3 of whom were term, died during their hospitalization. Of 60 CHB admissions, ICU admission was required in 23/60 (38%). Cardiogenic shock was diagnosed in 1 (2%) and cardiac arrest in 1 (2%). Pre-term infants accounted for 13% of admissions. Among these 8 pre-term infants, 2 were diagnosed with NEC. Morbidities among the 52 term infants included 2 with acute renal failure (3%) and 2 with seizures (3%). Pacemakers were implanted in 28 of 60 admissions (47%). There were 5 in-hospital deaths (8%), 3 of whom were term infants.
Conclusion
Morbidity and mortality among infants with structurally normal hearts and SVT or CHB remain low but may be higher than expected, even among term infants.
PEDIATRIC ECHOCARDIOGRAPHY BY WORK RELATIVE VALUE UNITS: IS STUDY COMPLEXITY ADEQUATELY CAPTURED?
Author links open overlay panelSowmyaBalasubramanianAlainaKippsSheaGluhmTheresaTacy
Elif Seda Selamet Tierney, Stanford University, School of Medicine, Stanford, CA, USA
Lucile Packard Children’s Hospital, Stanford, CA, USA
Introduction
Adoption of resource-based relative value units (RVU) for physician reimbursement is the standard method for determining professional payment. RVUs are intended to determine compensation primarily on the “work” involved in performing various procedures. Present RVU assignment for pediatric echocardiography is based exclusively on the current procedural terminology (CPT) codes, which do not incorporate complexity of diagnosis, time spent for image acquisition or interpretation of echocardiograms. In this study we examined whether CPT-based RVU assignment accurately reflect physician work component while performing and interpreting pediatric echocardiograms.
Methods
We prospectively assigned cardiac complexity (CC) score as well as the time for interpretation of 125 echocardiograms over a period of 3 months. We then extracted a random sample of echocardiograms performed during 6 consecutive months. Each study was designated a CC score and the extrapolated median interpretation time (MIT) based on the prospective data. Assigned work RVUs based on CPT codes were collected. Comparisons were made between the CC score versus time for interpretation, work RVUs, and total scan time.
Results
A total of 567 echocardiograms were analyzed. The CC categories and extrapolated MIT included (1) focused effusion / function evaluation (n = 136, MIT = 10 min); (2) normal anatomy / focused preterm infant studies (n = 117, MIT = 15 min); (3) acquired heart disease(n = 52, MIT 17.5 min); (4) congenital heart disease excluding single ventricles (n = 201, MIT = 25 min); (5) single ventricles including heterotaxy syndrome (n = 44, MIT = 20 min); (6) hearts with mechanical support (n = 17, MIT = 17 min). There were significant differences in the total scan time and time for study interpretation across CC groups (p < 0.0001). There was no statistical difference in the RVUs assigned to the CC categories.
Conclusions
Total scan time and time for interpretation of pediatric echocardiograms increases with complexity of acquired and congenital heart conditions. However, the current CPT-based RVU assignment of pediatric echocardiograms does not adequately capture disease complexity and physician work.
RIGHT VENTRICULAR DEFORMATION AT 14 MONTHS IS NOT IMPACTED BY INITIAL NORWOOD SHUNT TYPE: THE SINGLE VENTRICLE RECONSTRUCTION TRIAL
Author links open overlay panelGarickHillPeterFrommeltJessicaGorentzDavidSaudek
Medical College of Wisconsin, Milwaukee, WI, USA
Background
We compared echo-derived right ventricular (RV) strain (e) and strain rate (SR) indices after stage II palliation at 14 months in children with single RV anomalies enrolled in the Single Ventricle Reconstruction trial randomized to a modified Blalock-Taussig shunt (MBTS) vs. right-ventricle-pulmonary-artery shunt (RVPAS) at Norwood palliation.
Methods
Global and regional RV systolic longitudinal and circumferential e and SR, ejection fraction, and short axis % fractional area change were derived by subendocardial speckle tracking from protocol echocardiograms performed at 14.3±1.2 months. Student’s t-test or Wilcoxon rank sum test was used to compare groups.
Results
The cohort included 275 subjects (129 MBTS and 146 RVPAS). Longitudinal measures could be obtained in 214 (78%) subjects and circumferential measures in 182 (66%) subjects. Global longitudinal and circumferential e and SR did not differ between shunt groups (table) and no regional e differences were seen except the posterior septum(p=0.04). RV ejection fraction and % fractional area change did not differ between groups.
Conclusions
Longitudinal and circumferential RV myocardial deformation at 14 months, after stage II surgery, are unaffected by the type of initial shunt placed. Though RVPAS subjects required a ventriculotomy, no deleterious effect was appreciated on global or regional anterior RV wall e or SR. These data provide a basis for longer-term RV deformation assessment in survivors after Norwood palliation.
Comparison of MBTS and RVPAS groups
| MBTS | RVPAS | p value | MBTS | RVPAS | p value | ||
| Global longitudinal e | −12.2 (±3.3) | −12.6 (±3.9) | 0.50 | Global circumferential ɛ | −13.2 (±4.3) | −12.4 (±4.3) | 0.18 |
| Global longitudinal SR | −1.0 (±0.3) | −1.0 (±0.3) | 0.78 | Global circumferential SR | −1.0 (±0.4) | −1.0 (±0.4) | 0.32 |
| Ejection fraction | 46.7 (±9.1) | 45.2 (±10.9) | 0.26 | Fractional area change | 32.9 (±9.2) | 31.8 (±9.2) | 0.42 |
| Longitudinal e septal basal | −8.9 (±5.7) | −9.5 (±5.6) | 0.33 | Circumferential e anterior | −9.8 (±5.0) | −9.2 (±5.5) | 0.25 |
| Longitudinal e septal medial | −12.0 (±6.1) | −12.8 (±6.5) | 0.28 | Circumferential e anterior medial | −12.7 (±7.0) | −12.2 (±5.7) | 0.66 |
| Longitudinal e lateral medial | −12.3 (±3.7) | −12.5 (±4.8) | 0.75 | Circumferential e anterior lateral | −14.3 (±5.7) | −14.2 (±6.3) | 0.70 |
| Longitudinal e lateral basal | −17.0 (±5.5) | −16.2 (±6.4) | 0.18 | Circumferential e septal medial | −12.9 (±6.7) | −12.3 (±6.8) | 0.54 |
| Circumferential e septal posterior | −13.4 (±7.7) | −10.8 (±5.9) | 0.04 | ||||
| Circumferential e septal lateral | −16.1 (±6.9) | −15.3 (±7.5) | 0.56 |
LONG-TERM OUTCOMES AND RISK FACTORS FOR AORTIC VALVE DYSFUNCTION AFTER DISCRETE SUBVALVAR AORTIC STENOSIS RESECTION IN CHILDREN
Author links open overlay panelSarahPickardAlonGevaKimberleeGauvreauPedrodel NidoTalGeva
Boston Children’s Hospital, Boston, MA, USA
Background
While surgical resection of discrete subvalvar aortic stenosis (DSS) effectively relieves left ventricular outflow obstruction in most patients, only scant data are available on long-term outcomes. This study aimed to characterize rates of adverse outcomes after DSS resection and to identify risk factors for aortic valve (AoV) dysfunction requiring repair or replacement.
Methods
All patients who underwent DSS resection between 1984 and 2008 at our institution with at least 36 months’ follow-up were included. Patients with AV canal, hypoplastic left heart syndrome, hypertrophic cardiomyopathy, and conotruncal anomalies were excluded. Demographic, surgical, and echocardiographic data were reviewed. Outcomes included reoperation for recurrent DSS, complications (death, transplant, endocarditis, or complete heart block requiring pacemaker) and surgery for aortic regurgitation (AR).
Results
The median age at DSS resection for 155 patients was 5.2 y (range [0.1-35.0]) with a median follow-up of 10.9 y (range [3.0, 27.2]). Survival at 1, 5, and 10 years was 100%, 99.2%, and 98.3%, respectively. 32 patients (20.6%) underwent reoperation for recurrent DSS at a median of 6.3 y (range [0.9, 15.3]). By Kaplan-Meier analysis, freedom from reoperation plateaued 9 y after primary resection. Other adverse outcomes included cardiac transplantation in 2, endocarditis in 3, and pacemaker for complete AV block in 6 patients. AoV repair or replacement for predominant AR occurred in 13 patients after primary DSS resection (8.4%). These patients were significantly more likely to have associated valvar aortic stenosis (AS) (92.3% v. 18.3%, p<0.01) and to have undergone AS intervention than those who did not require AoV repair or replacement (84.6% v. 6.7%, p<0.01).
Conclusion
Long-term survival after DSS resection is good with 10-year survival of 98.3%. Risk of reoperation for recurrent DSS plateaus 9 y after initial resection. Late AoV dysfunction occurs in 8.4% of patients, predominantly due to associated AS and its treatment.
IMMUNOLOGIC AGING IN ADULTS WITH CONGENITAL HEART DISEASE: DOES INFANT STERNOTOMY MATTER?
Author links open overlay panelRobert W.ElderRoshan P.GerogeNancyMcCabeFredRodriguezWendyBookWilliamMahleAllan D.Kirk
Yale University School of Medicine, New Haven, CT, USA
Emory University School of Medicine, Atlanta, GA, USA
Background
Thymectomy is preformed routinely in infants during cardiothoracic surgery to enable repair of congenital heart disease (CHD). Prior work has shown that children post-sternotomy have decreased T-lymphocyte levels, without proven compromise in immune function. Long-term assessment of immune function of adults with congenital heart disease (ACHD) with infant cardiac repair is not known. We hypothesized that ACHD patients would show more pronounced changes in T-lymphocyte repertoire and markers for immune senescence.
Methods
ACHD patients >18 yrs were recruited who had sternotomy to repair CHD as infants (<1 yr) as well as age-matched ACHD patients without prior sternotomy. Institutional practice was to perform thymectomy concurrently with infant sternotomy. Exclusion criteria included known or suspected DiGeorge syndrome, pregnancy, recent infection, or NYHA class III-IV. Blood was analyzed using flow cytometry for known markers of lymphocyte maturation, exhaustion and senescence. Group differences were analyzed using Mann-Whitney-U and Fisher’s exact tests.
Results
18 ACHD patients ages 21-40 yrs participated: 10 cases and 8 controls. Mean age at sternotomy for cases was 85.5 days (SD 103.7). Diagnoses were not matched, but CHD complexity was similar in both groups and ranged from simple to complex. Cases and controls were matched for age (28.9 vs. 29.1 yrs; p=0.83), gender (p=0.15), and race (p=0.62). Mean percentage of cytotoxic CD8 lymphocytes was lower in cases compared to controls (26.8 vs. 33.9%; p=0.016). Naïve, undifferentiated CD8 T-cells were also lower in cases than controls (31.0 vs. 53.6%; p=0.027). CD8 cells expressing PD1, a marker of immune exhaustion, tended to be higher in sternotomy cases vs. controls (25.6 vs. 19%; p=0.083). Mean percentage of CD4 cells was higher in cases vs. controls (65.6 vs. 59.6%; p=0.027); there were no differences in CD4 T-cell subtype or markers of senescence.
Conclusion
ACHD patients who undergo sternotomy as infants exhibit differences in T lymphocytecomposition compared to ACHD controls, suggesting accelerated immunologic aging. Further investigation is warranted to understand these differences and any clinical effects.
NEUROCOGNITIVE EVALUATION OF ADULTS WITH CONGENITAL HEART DISEASE: THE NICHE STUDY
Author links open overlay panelWayne J.FranklinLedaKloudasAnitaSarafMelissaKarlstenDhavalParekhDavid D.Schwartz
Baylor College of Medicine, Houston, TX, USA
Texas Children’s Hospital, Houston, TX, USA
Background
Patients with congenital heart disease (CHD) are prone to injury of the developing central nervous system, leading to a higher incidence of neurocognitive and behavioral deficits. This multifactorial brain injury may be antenatal in origin, adversely affected by cardiac surgery with cardiopulmonary bypass, and exacerbated by ongoing cyanosis. Although CHD patients have been shown to have poor medical compliance, lower scholastic aptitude, and difficulty with employment, there are limited data on neurocognitive deficits outcomes in adults with CHD.
Methods
46 English-speaking study subjects with CHD (mean age = 30.0 y, range18-49 y) who had undergone cardiac surgery before age 5 y were recruited from an oupatient clinic setting. CHD severity was classified as moderate or severe, according to the 32nd Bethesda Conference guidelines. Exclusion criteria included a known diagnosis of stroke, comorbid genetic syndrome, severe psychiatric or neurological conditions, or history of substance abuse. A computerized battery of standardized neurocognitive tests (CNS-Vital Signs; CNS-VS) and validated behavioral rating scales were administered to each patient. Patients completed the testing in clinic under direct supervision.
Results
21 subjects had moderate CHD (mean age=25.3+6.2 y), 25 had severe CHD (mean age=33.7+7.7y). The severe group did worse on all measures of the CNS-VS, with significant differences in complex attention, cognitive flexibility, and overall executive functioning (all p-values < 0.01). The severe CHD group was more than twice as likely to have moderate impairment with scores below the 10th percentile on the CNS-VS (Odds Ratio 6.4, 95% CI, 1.3-30.8; p<0.05)
Conclusions
Subjects with severe CHD did significantly worse on measures of attention and executive functioning, which is suggestive of involvement of frontal white matter. Although intuitive, severe CHD is often associated with more complex surgical repairs and prolonged cyanosis. Our data would suggest that these risk factors are detrimental to long-term neurocognitive outcomes.
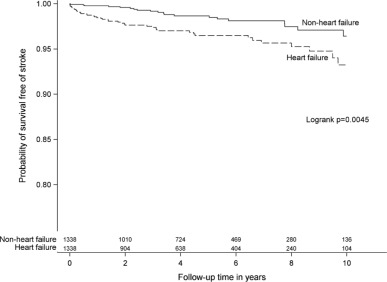
INCIDENCE AND PREDICTORS OF STROKE IN ADULTS WITH CONGENITAL HEART DISEASE: THE IMPACT OF HEART FAILURE
Author links open overlay panelJonasLanzJamesBrophyJudithTherrienMohammedKaouacheArianeMarelli
McGill University Health Centre, Montreal, Canada
McGill University, Montreal, Canada
Background
Stroke is an important cause of morbidity in the general population. There is a lack of data for adults with congenital heart disease (ACHD).
Methods
This was a retrospective cohort study of 28,465 ACHD Quebec patients aged 18 to 64 years between 1998 and 2010 based on aggregated province-wide administrative data.
Results
The cumulative risk of stroke estimated over the course of adulthood was 9.9% (95%-CI: 8.5-11.2%) in men and 7.7% (95%-CI: 6.6-8.8%) in women. Standardized rates compared to the general population of Quebec ranged from 174-383 per 100,000 person-years (py) for age-groups 20-64 compared to 15-111 per 100,000 py for the same age strata. Heart failure (OR 4.73 (95%-CI: 2.73-8.17) for age-group 18-44; OR 1.64 (95%-CI: 1.25-2.03) for age-group 45-64) emerged as the strongest predictors for stroke from a combination of stepwise model selection and Bayesian model averaging. In a propensity score matched sub cohort (Figure) the absolute risk of stroke over a ten-year follow-up was 6.8% (95%-CI 4.4-10.3%) for patients with a first diagnosis of heart failure compared to 3.1% (95%-CI: 2.0-4.9%) in non-heart failure patients (stratified log-rank test: p=0.0045).
Conclusion
One in ten men and one in thirteen women with ACHD suffered a stroke from ages 18-64. This was 12 times more common than non-ACHD adults in the general population less than 55 years of age. Heart failure was the strongest predictor of stroke in ACHD patients.
LONG-TERM SURVIVAL AND NEED FOR REOPERATION AFTER SURGICAL REPAIR OF COMPLETE ATRIOVENTRICULAR SEPTAL DEFECT: 40 YEAR FOLLOW-UP AT A SINGLE INSTITUTION
Author links open overlay panelSalilGindeJannaLamGarickHillJamesTweddellMichaelEaring
Medical College of Wisconsin, Milwaukee, WI, USA
Background
Decreased perioperative mortality over the past several decades, has produced a growing population of adults with repaired complete atrioventricular septal defect (CAVSD). However, early reports suggest a risk for reoperation at short and mid-term follow-up to address left atrioventricular valve (LAVV) regurgitation and subaortic obstruction. Whether the need for reoperation persists in the long-term after CAVSD repair is unknown. The present study reviewed the long-term survival, need for reoperation, and risk factors after CAVSD repair.
Methods
Between 1974 and 2000, 220 patients underwent surgical repair for CAVSD at our institution. A total of 184 patients survived to hospital discharge and had available follow-up data at a median post-operative duration of 16 years (2 months to 40 years).
Results
Associated diagnoses for the 220 CAVSD patients include Down syndrome in 171 (78%) and tetralogy of Fallot (TOF) in 22 (10%). Overall perioperative mortality was 10%, with a significant decrease to 3% in the late surgical era 1991 to 2000 (p<0.001). For the 184 hospital survivors, the long-term survival was 96%, 92%, and 77% at 10, 20, and 30 years, respectively. Risk factors for late mortality include early surgical era (p=0.004) and requiring a reoperation after initial repair (p=0.005). A total of 39 patients (21%) required at least 1 reoperation. The estimated freedom from reoperation was 88% at 10 years, 83% at 20 years, and 78% at 30 years. Risk factors for reoperation include early surgical era (p=0.007), non-Down syndrome (p=0.04), and TOF (<0.0001). Indications for reoperation included LAVV regurgitation in 17 (9.1%) patients at a median follow-up of 2 years (1 month to 19.7 years), and subaortic obstruction in 9 (4.8%) patients at a median follow-up of 9.4 years (2 years to 13.5 years).
Conclusions
Long-term survival following repair of CAVSD remains good, however, survivors are at risk for reoperation. The majority of reoperations appear to occur within the first two decades following initial repair. Early surgical era and associated diagnoses influence long-term survival and need for reoperation after CAVSD repair.
STATIN USE AND ANEURYSM RISK IN PATIENTS WITH BICUSPID AORTIC VALVE DISEASE
Author links open overlay panelAlexander PerryTaylorPatrickMcCarthyAdin-CristianAndreiZhi (Carrie)LiEdwinMcGeeS. ChrisMalaisrieColleenClennonJyothyPuthumana
Northwestern University, Chicago, IL, USA
Background
More than 50% of patients with bicuspid aortic valve (BAV) develop aortic dilatation, placing them at an 8-12 fold increased risk of aortic dissection compared to the general population and thereby warranting prophylactic aortic surgery. Previous studies have indicated that statin therapy might be associated with limited ascending aortic dilatation and aneurysmformation in BAV patients. We seek to determine the association between preoperative statin use and aortic dilatation among BAV patients referred for surgery.
Methods
We included all patients with BAV who underwent aortic valve +/− aortic surgery between April 2004 to December 31 2012 at our center. Use of statins and antihypertensivemedications, and history of aortic stenosis or insufficiency was captured in our registry. In BAV patients undergoing aortic valve replacement, current ACC/AHA guidelines state that aneurysm repair is indicated if the ascending aorta exceeds 4.5 cm. Based on the aortic diameter (AD) defined as the maximum aortic dimension on either echo, CT or MRI, patients were divided into two groups: AD < 4.5 cm or ≥ 4.5 cm. The association between preoperative statin use and aortic dilatation was assessed using logistic regression modeling with stepwise variable selection.
Results
Our study included 565 patients, of whom 326 (58%) had AD < 4.5 cm (mean age 59 14 years, 70% male, 43% on statins), while 239 (42%) had AD ≥ 4.5 cm (mean age 54 13 years, 84% male, 26% on statins) at the time of surgery. After adjusting for preoperative body surface area, beta blocker use, diuretic use and aortic stenosis, patients with AD ≥ 4.5 cm had 0.51 times lower odds (95% CI 0.34 – 0.75) of being on preoperative statinscompared to those with AD < 4.5 cm (p=0.001).
Conclusions
In BAV patients who are referred for surgery, preoperative statin use is associated with a lower odds of ascending aortic dilatation. While further studies are needed to clarify the role of statins in BAV disease, our findings are intriguing and suggest that statins may play a protective role by limiting aortic dilatation in patients with BAV.
RATE OF SUCCESSFUL TRANSFER FROM PEDIATRIC TO ADULT CONGENITAL HEART DISEASE CARE: WHERE ARE WE NOW?
Author links open overlay panelAdrienne H.KovacsErwinOechslinKristaGruenwaldNathanIngJeanineHarrison
University Health Network, Toronto, Canada
Background
The transfer from pediatric to adult congenital heart disease (CHD) care is a period that is known to be associated with lapses in medical care. The previously-documented rate of successful transfer between pediatric and adult CHD programs was approximately 50%. We investigated the rate of successful transfer between our local pediatric and adult CHD programs and compared two 2-year periods (2004-2005 vs. 2009-2010) to determine whether there was any change following the 2008 establishment of a local working group tasked with improving the transition and transfer of young patients with CHD from pediatric to adult care.
Methods
In this retrospective study, the following were patient inclusion criteria: (a) documented CHD, (b) direct transfer from pediatric to adult CHD program, (c) transfer documents received in 2004-2005 or 2009-2010, (d) age < 20 years at the time of transfer, and (e) expected to have been seen in the adult clinic by September 2013. We categorized patients as having a timely transfer (seen within the recommended time frame at the adult clinic), delayed transfer (seen at the adult clinic, but later than the recommended time frame), or failed transfer (never been seen at the adult clinic).
Results
Between 2004-2005, 271 patients met study inclusion criteria (61% male; median age = 17 years); the number of patients increased by 29% to 349 in the 2009-2010 time period (56% male; median age = 17 years). In 2004-2005, 81% of patients had a timely transfer, 11% had a delayed transfer, and 9% had a failed transfer; in 2009-2010, of 320 patients who were not yet due or overdue for their first clinic appointment, 86% of patients had a timely transfer, 9% had a delayed transfer, and 5% had a failed transfer (p = 0.12).
Conclusions
The current rate of successful transfer between our pediatric and adult CHD programs is over 90%. Despite a one-third increase in the number of transferring patients, there was a trend toward an increase in the proportion of timely transfers and a decrease in the proportion of failed transfers. We encourage other centers to consider establishing transition working groups to maintain high rates of transfer despite increasing numbers of patients.
FETAL ECHOCARDIOGRAPHY PREDICTS CLINICAL PRESENTATION AND OUTCOME IN TETRALOGY OF FALLOT WITH ABSENT PULMONARY VALVE: A MULTICENTER STUDY
Children’s National Medical Center, Washington, DC, USA
Background
Tetralogy of Fallot with absent pulmonary valve (TOF/APV) is associated with high rates of perinatal morbidity/mortality. This study aimed to identify fetal characteristics in TOF/APV associated with clinical presentation/outcome.
Methods
Fetuses with TOF/APV from 2002-2012 were retrospectively identified at 17 centers. Clinical data/fetal echocardiograms were obtained. The last study prior to birth was analyzed by a blinded observer and findings compared to outcomes.
Results
Seventy-eight fetuses were identified of which 10 (12.8%) were terminated. Twenty-six of the 68 remaining (38.2%) died (mean f/u 3.4 years), 5 in utero. Fifty-two survived until surgical repair, 17 during initial hospital admission (mean age 2.2 weeks) and 35 electively repaired later (mean age 4.2 months). Fetuses who died in utero were more likely to have hydrops. All fetuses who died in utero had mediastinal shift and moderate/severe right ventricular(RV) dilation. Those who died or were unstable enough to require neonatal repair were more likely to have mediastinal shift, ventricular enlargement, and cardiac dysfunction. Pulmonary artery (PA) and valve size was similar among groups, but the left PA was slightly larger in those who died or had neonatal repair.
Conclusion
Mediastinal shift, ventricular dilation, and decreased function are associated with worse clinical course/outcome in fetuses with TOF/APV. Identifying predictors of poor outcome is important for counseling and improved perinatal care.
Fetal Echocardiographic Characteristics Associated with Morbidity and Mortality in TOF/APV (n=68)
| Fetal Demise (n=5) vs. Live Birth (n=63) | Overall Mortality (Fetal and Postnatal, n=26) vs. Survival (n=42) | Neonatal Complete Repair or Death Prior to Repair (n=51) vs. Late Elective Repair (n=17) | ||||
| Hydrops | 40% vs. 3% | p=0.03 | 8% vs. 5% | p=0.6 | 10% vs. 3% | p=0.3 |
| Mediastinal shift | 100% vs. 44% | p=0.02 | 65% vs. 38% | p=0.03 | 64% vs. 34% | p=0.02 |
| Abnormal cardiac axis (<30 or >75 degrees) | 75% vs. 38% | p=0.3 | 52% vs. 33% | p=0.1 | 56% vs. 26% | p=0.01 |
| Moderate-severe RV dilation | 100% vs. 43% | p=0.02 | 73% vs. 31% | p=0.001 | 67% vs. 29% | p=0.002 |
| Left ventricular (LV) dilation | 0% vs. 13% | p=1 | 23% vs. 5% | p=0.05 | 21% vs. 3 % | p=0.03 |
| Cardiothoracic area ratio | 0.35 vs. 0.34 | p=0.8 | 0.37 vs. 0.33 | p=0.01 | 0.36 vs. 0.33 | p=0.06 |
| RV dysfunction | 60% vs. 19% | p=0.03 | 46% vs. 7% | p<0.001 | 42% vs. 3% | p<0.001 |
| LV dysfunction | 40% vs. 11% | p=0.1 | 27% vs. 5% | p=0.02 | 27% vs. 0% | p<0.001 |
| Pulmonary valve diameter (cm) | 0.57 vs. 0.53 | p=0.6 | 0.62 vs. 0.53 | p=0.06 | 0.59 vs. 0.54 | p=0.3 |
| Main PA diameter (cm) | 1.11 vs. 1.18 | p=0.7 | 1.25 vs. 1.13 | p=0.2 | 1.25 vs. 1.1 | p=0.09 |
| Right PA diameter (cm) | 1.02 vs. 1.08 | p=0.8 | 1.07 vs. 1.08 | p=0.9 | 1.18 vs. 0.99 | p=0.06 |
| Left PA diameter (cm) | 1.18 vs. 1.03 | p=0.5 | 1.17 vs. 0.95 | p=0.03 | 1.16 vs. 0.93 | p=0.02 |
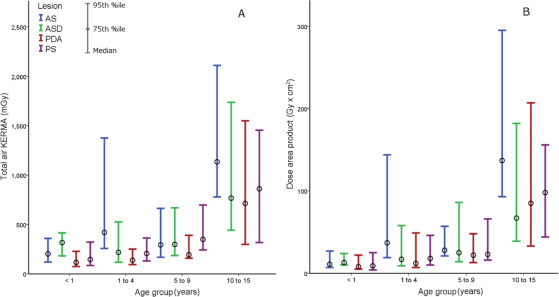
RADIATION DOSE BENCHMARKS DURING CARDIAC CATHETERIZATION FOR CONGENITAL HEART DISEASE IN THE UNITED STATES
Author links open overlay panelSunil J.GhelaniAndrewGlatzSthuthiDavidRyanLeahyRusselHirschLaurieArmsbySaraTruccoRalfHolzerLisaBergersen
Boston Children’s Hospital, Boston, MA, USA
Background
There is a paucity of published literature with regard to radiation doses during catheterizationfor congenital heart disease(CHD). Children and adolescents are at a higher risk of long term adverse effects of radiation. Obtaining benchmark radiation data is essential for assessing impact of quality improvement initiatives for radiation safety.
Methods
Data were obtained retrospectively from seven laboratories participating in Congenital Cardiac Catheterization Project on Outcomes(C3PO) collaborative. Total air KERMA, dose area product, and total fluoroscopy time were obtained for the following procedures: 1) patent ductus arteriosus(PDA) closure, 2) atrial septal defect closure, 3) pulmonary valvuloplasty, 4) aortic valvuloplasty, 5) treatment of coarctation of aorta and, 6) transcatheter pulmonary valve(TPV) placement.
Results
Median, 75th percentile, and 95th percentile values for the above radiation parameters were calculated for 2713 cases identified between January 2009 and July 2013. Radiation exposure was lowest in PDA closure and highest in TPV placement. Total fluoroscopy time was a poor marker of radiation exposure and did not correlate well with total air KERMA and dose area product.
Conclusions
This study presents first, multicenter, age stratified radiation doses for six common interventional procedures for CHD in the US. These values will serve as baseline for measuring the effectiveness of future quality improvement activities by the C3PO collaborative.
THE PEDIATRIC HEART NETWORK FONTAN FOLLOW-UP STUDY: SURVIVAL DATA AND PREDICTORS OF FUNCTIONAL OUTCOME 7 YEARS LATER
Author links open overlay panelAndrew M.AtzVictorZakLynnMahonyKarenUzarkPeterShraderDianeGallagherStephenParidonRichardWilliamsRogerBreitbartStevenColanJonathanKaltmanReneeMargossianSaraPasqualiKerstinAllenWymanLaiRosalindKorsinBradleyMarinoNicoleMirarchiBrianMcCrindle
Medical University of South Carolina, Charleston, SC, USA
Background
Multicenter longitudinal outcome data for Fontan patients surviving into adulthood are lacking.
Methods
Current vital and cardiac transplant status data were assessed 6.8±0.4 years after the Fontan Cross-Sectional Study (Fontan 1) in all 546 subjects. Anatomic, clinical and surgical data were collected along with current clinical state, socioeconomic status and access to health care.
Results
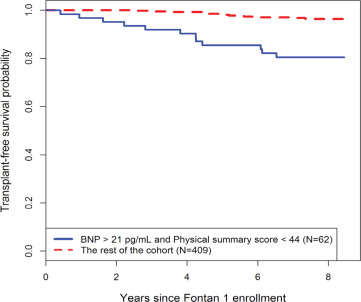
Thirty subjects (5%) died or underwent transplantation since Fontan 1. Subjects with both an higher brain natriuretic peptide (BNP; >21 pg/mL) and a low Child Health Questionnaire (CHQ) physical summary score (<44) measured at Fontan 1 were significantly more likely to die or undergo transplant than the remainder of the cohort (see Figure), with a hazard ratioof 6.2 (2.9-13.5). Among 516 survivors with a Fontan circulation, 427 (83%) enrolled in this follow up study at 18.4 ± 3.4 years of age. Although mean scores on functional health status questionnaires were lower than those in the general population, individual scores were within the normal range in 78% and 88% of subjects for the CHQ Physical and Psychosocial Summary score, and 97% and 91% for the SF-36 Physical and Mental Aggregate Score, respectively.
Conclusions
We found 95% interim transplant-free survival for Fontan patients over an average of 7 years of follow up. Continued longitudinal investigation into adulthood is necessary to better understand the determinants of long-term outcomes and to improve functional health status.
NATIONAL VARIATION IN PRENATAL DIAGNOSIS OF CONGENITAL HEART DISEASE BY STATE AND LESION TYPE: AN ANALYSIS OF THE SOCIETY OF THORACIC SURGEONS CONGENITAL HEART SURGERY (STS-CHS) DATABASE
Author links open overlay panelMichael D.QuartermainSaraPasqualiKevinHillDavidGoldbergJamesHuhtaJeffreyJacobsMarshallJacobsSung HeeKimRossUngerleider
Wake Forest University School of Medicine, Winston-Salem, NC, USA
Background
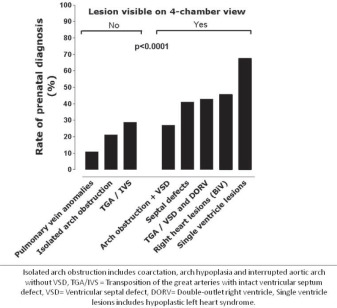
Prenatal diagnosis allows for improved peri-operative outcomes of fetuses with certain forms of congenital heart disease (CHD). Variability in prenatal diagnosis has been demonstrated in other countries, leading to efforts to improve access to care and fetal imaging protocols, but has not been examined across the US. We evaluated national variation in prenatal diagnosis across geographic region and lesion type in neonates with CHD undergoing heart surgery.
Methods
Neonates (≤30d) undergoing heart surgery in the STS-CHS Database (2006-12) were included. Centers with >15% missing prenatal diagnosis data were excluded. Rates of prenatal diagnosis were compared across geographic location of residence and lesion type using the Chi-square test.
Results
Overall, 18,631 neonates from 44 states operated on at 91 US centers were included. Prenatal diagnosis occurred in 42% and increased every year from 33% (2006) to 49% (2012). There was significant geographic variation in rates of prenatal diagnosis (range 23%-61% across states, p < 0.001). Significant variability by lesion type was also observed (figure); with higher rates for lesions identifiable on 4-chamber view versus those requiring outflow tract visualization (39% versus 20%, p < 0.0001).
Conclusions
Rates of prenatal CHD diagnosis in the US remain low, with significant variability between states and across lesion type. Further studies are needed to better define reasons for this variation and the potential impact on patient outcomes.
Background
In prior single institution studies using historical controls, daily home monitoring of oxygen saturation and weight have been reported to improve interstage outcomes for single ventricle heart disease. We aimed to determine the associations of various home monitoring strategies with interstage outcomes using a multicenter cohort with contemporary controls.
Methods
We performed a retrospective cohort study using data from the National Pediatric CardiologyQuality Improvement Collaborative from 2008 to 2012. We compared interstage mortality, unscheduled readmissions, and change in weight-for-age Z-score (ΔWAZ) for various home monitoring strategies of oxygen saturation or weight, adjusting for sex, syndrome, tricuspid regurgitation, arch obstruction, and shunt type.
Results
Of the 575 eligible enrollees at 40 centers, interstage mortality was 7.3%, and 46% had ≥1 unscheduled readmission. We did not find any associations of home oxygen and/or weight monitoring with mortality or readmission. There was no difference in adjusted least squares means ΔWAZ for daily (0.37 ± 0.15) vs. weekly weight monitoring (0.38 ± 0.20, p=0.99), but daily was superior to no home weight monitoring (-0.12 ± 0.20, p<0.01).
Conclusion
Home weight monitoring may be associated with improved interstage weight gain, but factors beyond home monitoring strategies likely explain improvements in other outcomes over time. Efforts to identify and share best practices at high-performing centers are warranted.
Association of Home Monitoring Frequency with Interstage Outcomes for Single Ventricle Heart Disease
| Daily (referent) n (%) | Weekly n (%) | Adjusted OR (95% CI) | P- Value | None n (%) | Adjusted OR (95% CI) | P-Value | |
| Oxygen Saturation Monitoring | N = 461 | N = 66 | N = 48 | ||||
| Interstage Mortality | 35 (7.6%) | 4 (6.1%) | 1.13 (0.35-3.6) | 0.84 | 3 (6.3%) | 0.79 (0.18-3.57) | 0.76 |
| Interstage Mortality or Transplant | 39 (8.5%) | 4 (6.1%) | 1.00 (0.32-3.13) | 0.99 | 6 (12.5%) | 2.00 (0.70-5.70) | 0.20 |
| ≥1 Unscheduled Readmission (any cause) | 217 (47.1%) | 26 (39.4%) | 0.86 (0.48-1.52) | 0.59 | 24 (50.0%) | 0.98 (0.49-1.96) | 0.95 |
| ≥1 Unscheduled Readmission for Cyanosis | 52 (11.3%) | 7 (10.6%) | 0.94 (0.37-2.40) | 0.89 | 7 (14.6%) | 1.01 (0.34-3.04) | 0.98 |
| Weight Monitoring | N = 410 | N= 65 | N = 78 | ||||
| Interstage Mortality | 32 (7.8%) | 4 (6.2%) | 1.09 (0.34-3.53) | 0.89 | 5 (6.4%) | 0.73 (0.21-2.60) | 0.63 |
| Interstage Mortality or Transplant | 36 (8.8%) | 4 (6.2%) | 0.95 (0.30-3.03) | 0.93 | 8 (10.3%) | 1.40 (0.53-3.67) | 0.49 |
| ≥1 Unscheduled Readmission (any cause) | 192 (46.8%) | 25 (38.5%) | 0.84 (0.47-1.52) | 0.57 | 39 (50.0%) | 1.00 (0.57-1.79) | 0.99 |
| ≥1 Unscheduled Readmission for Poor Weight Gain | 25 (6.1%) | 4 (6.2%) | 1.26 (0.38-4.15) | 0.70 | 2 (2.6%) | 0.29 (0.04-2.28) | 0.24 |
| Change in weight-for-age Z-score ≤0 (in those with weights recorded and who underwent stage II palliation) | 126 (34.2%) N = 368 | 21 (34.4%) N =61 | 1.07 (0.56-2.04) | 0.85 | 35 (50.0%) N = 70 | 1.83 (0.98-3.40) | 0.06 |
MAIN PULMONARY ARTERY AREA LIMITS EXERCISE CAPACITY IN PATIENTS LONG-TERM AFTER ARTERIAL SWITCH OPERATION FOR TRANSPOSITION OF THE GREAT ARTERIES (TGA)
Author links open overlay panelMieke MPDriessenVivan JMBaggenGertjanSieswerdaTimLeinerTimTakkenSebastiaan WHvan WijkNicolaas JGJansenPaulSchoofFolkertMeijboomHansBreur
University Medical Center Utrecht, Utrecht, The Netherlands
Wilhelmina Children’s Hospital, Utrecht, The Netherlands
Background
Right ventricular (RV) outflow tract obstruction (RVOTO) is the most frequent residual lesion in pts the after arterial switch operation (ASO) for TGA. This study compares outflow tract area, distensibility and pulmonary blood flow (PBF) distribution of ASO pts to healthy controls and correlates these measurements to right ventricular (RV) function and exercise capacity.
Methods
Participants underwent cardiac magnetic resonance imaging including angiography and flow measurements and cardio-pulmonary exercise testing. RV volumes and function, pulmonary blood flow (PBF) distribution, smallest cross-sectional area of the main (MPA), left (LPA) and right pulmonary artery (RPA), LPA and RPA distensibility (relative area change) and percentage of predicted peak oxygen uptake (VO2max/kg%) were measured. ASO pts were compared to healthy controls.
Results
Fifty pts were included (median follow-up 21.2 [12.1-32.8] yrs). Reintervention for RVOTOwas performed in 9/50 (18%) of patients. ASO are compared to controls in table 1. MPA area was the only factor significantly correlated with RV stroke volume (r2=0.168, p<0.01) and VO2max/kg% (r2=0.194, p<0.01) in multivariate analysis.
Conclusion
In our cohort MPA, LPA and RPA areas were smaller compared to healthy controls. Only MPA area independently correlated to stroke volume and VO2max/kg%, likely because distensibility and PBF distribution were comparable to controls. This should be considered when selecting pts for reintervention.
ASO patients vs healthy controls #median [range] and Mann-Whitney; other mean (SD) and T-test
| ASO (n=48) | controls (n=21) | P-value | |
| Age# | 21.3 [12.2-35.3] | 26.4 [21.0-35.2] | <0.001 |
| RVEDV (ml/m2) | 101.5 (13.2) | 109.2 (18.0) | 0.049 |
| RVESV (ml/m2) | 50.3 (8.5) | 55.2 (10.8) | 0.051 |
| RVEF (%) | 50.4 (5.2) | 49.7 (3.8) | 0.575 |
| RVmass (gr/m2) | 30.7 (5.4) | 22.2 (3.8 | <0.001 |
| MPA area (mm2)# | 184.6 [57.6-345.6] | 270.2 [197.2-537.5] | <0.001 |
| LPA area (mm2)# | 58.9 [15.4-253.6] | 156.5 [117.5-261.6] | <0.001 |
| RPA area (mm2) | 110.0 (53.2) | 151.2 (32.8) | <0.001 |
| LPA area change (%) | 29.8 (8.9) | 28.2 (6.8) | 0.402 |
| RPA area change (%) | 32.2 (9.1) | 33.5 (4.5) | 0.418 |
| LPA : RPA (%) | 46.2 : 53.8 (10.8) | 44.9 : 55.1 (4.7) | 0.593 |
| smallest branch flow (%) | 42.1 (8.2) | 43.9 (3.2) | 0.320 |
HEMODYNAMIC CAUSES FOR EXERCISE INTOLERANCE IN FONTAN PATIENTS
Author links open overlay panelAnders HedeboeHebertAnnette S.JensenUlla R.MikkelsenLarsIdornKeld E.SorensenUlfThilenKatarinaHanseusLarsSondergaard
Copenhagen University Hospital, Rigshospitalet, Copenhagen, Denmark
Background
Exercise intolerance is frequent among Fontan patients and may be an important determinant for quality of life. This study investigated the hemodynamic causes of impaired exercise capacity in Fontan patients with particular focus on the influence of heart rate (HR) and stroke volumes.
Methods
In 38 Fontan patients, peak oxygen consumption (VO2), HR and non-invasive measures of cardiac output (CO) and stroke volume index (SVI) were recorded during incremental load exercise test and compared with 19 age and gender matched controls.
Results
The Fontan patients had a lower VO2, CO and HR at peak exercise than controls, all p<0.0001. Furthermore, SVI dropped 14% (from 44.2±10.6 to 37.6±7.3 ml/m2) in Fontan patients from the peak plateau to maximal exercise vs. 5% (from 57.2±8.4 to 54.4±7.8 ml/m2) in controls, p<0.0001.
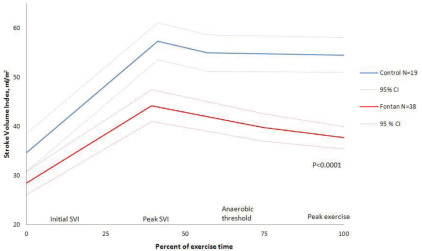
The low SVI and HR explained 67% and 20% of the difference in peak VO2 between Fontan patients and controls respectively.
Conclusions
Low SVI at maximal exercise was the most important hemodynamic factor limiting exercise capacity in Fontan patients, whereas chronotropic impairment had a smaller impact. The low HR and SVI at maximal exercise accounted for the difference in peak VO2 between Fontan patients and controls in this study. Further studies are needed in order to identify the causes of the decreasing SVI during exercise in Fontan patients.
PREOPERATIVE RIGHT VENTRICULAR VOLUMES DETERMINE RIGHT VENTRICULAR NORMALIZATION AND EVENTS LATE AFTER PULMONARY VALVE REPLACEMENT IN PATIENTS WITH TETRALOGY OF FALLOT
Author links open overlay panelJoukeBokmaMichielWinterThomasOosterhofHubertVliegenBarbaraMulderBertoBouma
Academic Medical Center, Amsterdam, The Netherlands, Leiden
University Medical Center, Leiden, The Netherlands
Background
In patients with Tetralogy of Fallot (TOF) longstanding pulmonary regurgitation leads to right ventricular (RV) dilation and dysfunction, and concomitant adverse clinical events. Previous studies revealed that normalization of RV volumes after pulmonary valve replacement (PVR) occurred in those patients with preoperative RV end-systolic volume (ESV) < 80 mL/m2 or RV end-diastolic volume (EDV) < 160 mL/m2. The aim of this study is to determine the relationship of preoperative RV volumes with long-term functional and clinical outcome.
Methods
In this retrospective, multicenter study all TOF patients who underwent successful surgical PVR and in whom cardiovascular magnetic resonance before, early after and late after PVR was available were included. RV normalization was defined as RV ejection fraction >48% and RV EDV < 108 mL/m2. In addition, we determined adverse clinical events after PVR.
Results
A total of 50 TOF patients (64% male) who underwent PVR between 1995 and 2006 at a mean age of 29 (± 9) years were included. Cardiovascular magnetic resonance was performed before (0.6 ± 0.5 years), early after (1.0 ± 0.9 years) and late after (8.1 ± 2.8 years) PVR. RV EDV improved (173 ± 38 to 114 ± 27 mL/m2, P=<0.001) early after PVR and remained stable at late follow-up (113 ± 27 mL/m2, P=NS). RV ejection fraction was unchanged early after PVR (42 ± 9 to 44 ± 8%, P=0.11) and remained stable at late follow-up (45 ± 9%, P=0.18). 12 patients (24%) had RV normalization late after PVR. There was a statistically significant relation between preoperative RV ESV < 80 mL/m2 or RV EDV < 160 mL/m2 and late RV normalization (P=<0.001 and P=<0.001). Six patients (12%) had an adverse clinical event (1 death, 1 sustained VT, 2 heart failure, 2 redo-PVR) after PVR. No events occurred when preoperative RV ESV was < 80 mL/m2 or RV EDV was < 160 mL/m2 (P=0.02).
Conclusions
In patients with TOF, PVR results in a sustained hemodynamic improvement. Preoperative RV ESV < 80 mL/m2 and/or RV EDV < 160 mL/m2 are associated with late RV normalization and less adverse clinical events.
BIVENTRICULAR STRAIN AND DYSSYNCHRONY IN REPAIRED TETRALOGY OF FALLOT: RELATIONSHIP TO DEATH AND SUSTAINED VENTRICULAR TACHYCARDIA MEASURED BY CARDIAC MAGNETIC RESONANCE
Author links open overlay panelThomasMoonNadineChoueiterTalGevaAnne MarieValenteDavidHarrild
Boston Children’s Hospital, Boston, MA, USA
Background
Short- and medium-term survival in tetralogy of Fallot (TOF) has greatly improved; however the risk of death increases significantly after the third post-operative decade. The purpose of our study was to investigate if ventricular strain and dyssynchrony measured by cardiac magnetic resonance (CMR) feature tracking in adults with repaired TOF is associated with death and sustained ventricular tachycardia (VT).
Methods
TOF patients with -death or VT (case, n=16) were compared to age-matched TOF controls (with no adverse outcome, n=32). For each patient, mid-ventricular short-axis and 4-chamber cine steady-state free precession images were analyzed using CMR feature tracking software. Left (LV) and right ventricular (RV) global circumferential and longitudinal strain and indices of dyssynchrony were compared between groups.
Results
Table 1 compares strain values. In a multivariable model including strain and dyssynchrony parameters, impaired RV and LV longitudinal strain were strongly associated with the adverse outcome (p=0.003 and 0.04, respectively); the ROC area under the curve for this model was 0.93, was not significantly different than a model including all variables. No differences in ventricular dyssynchrony were identified.
Table 1
| TOF Case | p Value | TOF Control | |
| Global LV Strain (%) | |||
| Circumferential | 17.5 (7.0–28.9) | 0.003 | 22.6 (9.2–30.0) |
| Longitudinal | 12.7 (8.3–20.0) | <0.001 | 17.7 (9.8–27.4) |
| Global RV Strain (%) | |||
| Circumferential | 9.9 (5.5–21.3) | 0.001 | 16.2 (8.4–25.5) |
| Longitudinal | 11.0 (4.6–21.0) | <0.001 | 18.0 (11.0–23.1) |
| Values shown as median (range). |
Conclusions
In this cohort, all of the strain parameters were significantly impaired in the adverse outcome group, compared to TOF controls. In a multivariable model, both LV and RV longitudinal strain were strongly associated with death and VT.
HYPERTROPHIC CARDIOMYOPATHY CENTER: CONTEMPORARY MULTIDISCIPLINARY GUIDELINE-BASED EXPERIENCE
Author links open overlay panelAnushreeAgarwalRayanYousefzaiChiChoKambizShetabiM. FuadJanMichelleBushBijoyKhandheriaTimothyPaterickPaulWernerTanvirBajwaSuhailAllaqabandA. JamilTajikAurora CardiovascSvcs
Aurora Sinai/St. Luke’s Med Ctrs, Univ Wisconsin Sch Med and Public Health, Milwaukee, WI, USA
Background
Real-life clinical experience of hypertrophic cardiomyopathy (HCM) in community hospitals is lacking. We aim to report our contemporary experience of a newly established HCM center where patients (pts) are referred for comprehensive evaluation.
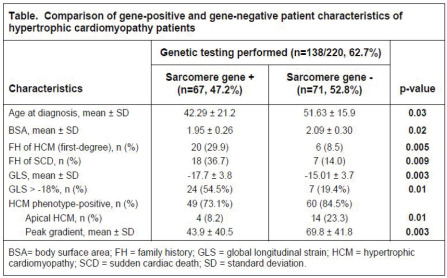
Methods/Results
From 7/2010 to 9/2013, 228 pts were referred. 187 (82%) were phenotype positive (P+) for HCM, with 5% involving apex. Mean maximal left ventricular thickness was 2.2 ± 1.4 cm, with >2.5 cm thickness seen in 20%. Of 41 phenotype-negative pts, 44% were sarcomere gene positive (G+), 37% were gene negative (G-), and 20% were HCM phenocopies (2 Danon, 3 Fabry, 2 amyloid and 1 hypertension). Obstructive HCM was present in 70%. P+ characteristics included: mean age 49 ± 19 years, males 54%, whites 74%, hypertension62%, sleep apnea 62%, NYHA III/IV symptoms 23% and >grade 1 diastolic dysfunction65%. Mean global longitudinal strain was −15.9 ± 4. At least 1 sudden death risk factor was present in 72%, and 23% received implantable defibrillator. 43% had magnetic resonance imaging; 58% of those had delayed enhancement. Management included beta blockers in 81%, calcium channel blockers in 40%, angiotensin blockers in 27% and disopyramide in 38%. Septal reduction included ablation in 26% and myectomy in 13%. Genetic testing was performed in 63%. Significant differences among G+ vs. G- are shown in the table.
Conclusion
We present the largest, most contemporary, single-center community hospital HCM experience conforming to the latest guidelines.
PREVALENCE OF PULMONARY ARTERIAL HYPERTENSION IN ADULT CONGENITAL HEART DISEASE
Author links open overlay panelAnnelieke CMJvan RielMarkSchuuringIrene D.van HessenAeilkoZwindermanLucCozijnsenStan C.L.A.ReichertJanHoorntjeLodewijkWagenaarM.C.PostArieVan DijkElkeHoendermisBarbaraMulderBertoBouma
Academic Medical Center, Amsterdam, The Netherlands
Background
The aging congenital heart disease (CHD) population is prone to develop a variety of sequelae, including pulmonary arterial hypertension (PAH). Previous prevalence reports have a high degree of variability, with an overrepresentation of tertiary centers. We aimed to report robust prevalence estimates of PAH in adult CHD patients.
Methods and Results
We performed a cross-sectional analysis to determine prevalence of PAH in adults with CHD using the population-based Dutch Congenital Corvitia (CONCOR) registry. Of 12 624 adults with CHD alive in 2011, 5 487 (44%) had an initial diagnosis of systemic-to-pulmonary shuntand were thereby at risk for developing PAH. From these patients, a random sample of 1 814 subjects was obtained, mean age 40±15 years, and 135 PAH cases were observed. Total PAH prevalence in patients born with a systemic-to-pulmonary shunt was 7.4%. A remarkable high number of patients had PAH after corrective cardiac surgery, with a prevalence of 5.7%. PAH prevalence increases with age, from 2.5% under 30 years until 35% in the oldest patients of the study cohort. In the entire CHD population the PAH prevalence was 3.2%. Based on an overall prevalence of CHD in the adult population of 3000 per million, we can assume a prevalence of PAH-CHD of 100 per million inhabitants.
Conclusion
Prevalence of PAH in CHD patients is 3.2%, and 100 per million in the general adult population. Especially in patients after corrective cardiac surgery and the elderly, physicians should be aware of PAH-CHD, to provide optimal therapeutical and clinical care.
ASSOCIATION BETWEEN FUNCTIONAL OUTCOME AND VENTRICULAR MECHANICS IN EISENMENGER SYNDROME: A SPECKLE TRACKING STUDY
Author links open overlay panelKrong-OnPinyoluksanaBenjaminEidemHector RVillarragaHeidiConnollyGarvanKaneNaserAmmash
Mayo Clinic, Rochester, MN, USA
Background
The association between ventricle function and functional class (FC) in Eisenmenger Syndrome (ES) is not well described. Speckle tracking echocardiography (STE) is suggested to be sensitive and more accurate for analyzing ventricular function. We sought to compare RV and left ventricular (LV) systolic strain and SR in patients with different FC.
Methods
We retrospectively evaluated 34 ES patients [aged 43 ±12 years; 62% women; 6 atrial septal defect, 7 atrioventricular septal defect (AVSD), 16 ventricular septal defect, 4 patent ductus arteriosus (PDA), 1 truncus arteriosus and 1 combined AVSD and PDA]. FC was based on New York Heart Association classification. 44% were FC 3-4. Velocity vector imaging was used to measure myocardial strain and SR for both free walls. Wilcoxon’s rank sum test and logistic regression were performed.
Results
RV lateral wall longitudinal strain (LS) and SR were significantly reduced in FC 3-4 compared to FC 1-2 (p = 0.01, 0.04 respectively) but not with LV. Worsening RV LS and SR were associated with higher FC (table). Excluding AVSD, RV LS was reduced in pre-tricuspid shunts (n=6) than post-tricuspid shunts (n=21) (p = 0.02), whereas LV LS was not. There was an association between RV LS and SR vs LV LS and SR (β = 0.36, 0.38 respectively) after adjusted for medications and FC but not for age and gender.
Conclusions
The study shows an association between RV and LV function assessed by STE which may reflect ventricular interdependence but only RV function is associated with FC.
Association between functional class and right ventricular lateral wall longitudinal strain and strain rate
| OR per 1 SD | p-value | 95% confident interval | |
| Association between FC and RV lateral wall longitudinal strain | |||
| Without adjustment | 6.3 | <0.01 | 5.1 to 8.1 |
| Adjusted for age and gender | 6.4 | <0.01 | 5.2 to 8.4 |
| Adjusted for medications | 6.2 | 0.01 | 5.1 to 8.0 |
| Adjusted for pre vs post-tricuspid shunts | 6.5 | 0.03 | 5.0 to 9.2 |
| Association between FC and RV lateral wall longitudinal strain rate | |||
| Without adjustment | 8.5 | 0.03 | 0.57 to 270.0 |
| Adjusted for age and gender | 8.5 | 0.03 | 0.56 to 275.4 |
| Adjusted for medications | 7.1 | 0.04 | 0.47 to 215.8 |
| Adjusted for pre vs post-tricuspid shunts | 2.9 | 0.17 | 0.14 to 105.3 |
Abbreviations: OR odd ratio; SD standard deviation (4.6% and 0.3 s-1 for right ventricular lateral wall longitudinal strain and strain rate); FC functional class; RV right ventricular
EFFECTS OF BETA BLOCKERS ON MYOCARDIAL MECHANICS IN HYPERTROPHIC CARDIOMYOPATHY
Author links open overlay panelChiaraPisanelloHongchangLuoIraklisPoziosLarsSorensenHsinYuehLiangFilippoCreaM. RoselleAbrahamTheodoreAbraham
Johns Hopkins University, Baltimore, MD, USA
Background
Beta-blockers (BB) are the primary medical therapy in obstructive and nonobstructive hypertrophic cardiomyopathy (HCM). However, the effects of BB therapy on cardiac mechanics are unknown. In particular, it is unclear if decreasing gradients have salutary effects on myocardial mechanics or if BB universally reduce cardiac contractility.
Methods
49 HCM patients underwent conventional and strain echocardiography (SE) prior to and after initiation or augmentation of BB.
Results
Mean age was 52±14 years (men 48%); 12 obstructive, 37 non/labile obstructive. Maximum wall thickness was 2.0±0.5 cm, mean ejection fraction 68±3%, mean E/e’ 17±7, resting gradient 25±37 mmHg (70±37 mmHg obstructive, 10±6 mmHg non/labile); mean duration of beta blocker therapy was 14±13 months (19 patients had de novo BB, 30 patients had increases in BB dosage). Mean increment in BB dose was 45±57 mmHg; the mean BB dose at follow-up for the whole group was 104±93 mg. Pre and post BB mean longitudinal strain (LS) 17±4% vs. 17±4%, p=0.5 and mean longitudinal systolic strain rate (SSR) 1.0±0.2 vs. 1.0±0.2 s-1 were not statistically different while mean longitudinal early diastolic strain rate (SRE) decreased from 1.25±0.3 to 1.0±0.2, p<0.01. Post BB rest gradient correlated significantly with BB dose (r=0.35, p<0.01). In the subgroup of obstructive HCM patients with significant decrements in gradients (108±67 to 56±40 mmHg) the SRE demonstrated a non-significant increase from 1.34±0.3 to 1.50±0.2 s-1. There were no statistically significant differences in pre vs. post BB mechanics in those patients with de-novo vs. increases in BB dose.
Conclusion
BB therapy does not appreciably impact systolic mechanics in HCM. Early diastolic mechanics are worsened after BB therapy as evidenced by significantly lower SRE. Obstructive HCM patients who have significant decrements in outflow gradients show a non significant improvement in early relaxation mechanics. Our data suggest that BB have an overall salutary effect on myocardial mechanics particularly in obstructive HCM patients with large reductions in outflow gradients.
THE EFFECT OF WELL-CONTROLLED MATERNAL DIABETES ON FETAL HEART FUNCTION: A TISSUE DOPPLER STUDY
Author links open overlay panelAshishSainiSerdarUralLindaPauliks
Penn State Hershey Medical College, Hershey, PA, USA
Background
Previous studies on fetal heart function in infants of diabetic mothers have shown altered diastolic myocardial velocities on tissue Doppler imaging (TDI) and an abnormal myocardial performance index (MPI) in affected fetuses even without hypertrophy. It is unclear whether better maternal glycemic control may prevent these fetal changes. This study therefore compared color TDI velocities and MPI in fetuses of mothers with well-controlled diabetesand normal controls.
Methods
The study included 42 fetuses as 21 matched pairs of infants of diabetic mothers (DM) and controls. Color TDI cine loops of apical 4-chamber views were acquired as digital echocardiographic raw data. During off-line analysis, systolic (S’) and diastolic (E’, A’) velocities and fetal MPI were measured at the tricuspid, septal and lateral mitral ring as average of 3 beats.
Results
Fetal pairs were matched for maternal and gestational age (32.0±5.4 vs. 31.7± 5.4 weeks; NS). Among DM mothers, 14 were on insulin while 10/21 had gestational DM only. Fetal TDI velocities correlated with gestational age. All fetuses had similar S’, E’ and A’ wave velocities (Table). Moreover, fetal MPI was also comparable: RV MPI in controls was 0.32±0.07 vs. 0.31±0.07 in DM (NS) and LV MPI was 0.34±0.07 vs. 0.33±0.07 in DM (NS).
Conclusions
In this study, well-controlled maternal diabetes did not affect fetal MPI or color TDI myocardial velocities. These findings suggest that optimal maternal glycemic control may prevent injury to the fetal heart.
COMPARISON OF FOUR-DIMENSIONAL ECHOCARDIOGRAPHY AND TWO-DIMENSIONAL ECHOCARDIOGRAPHY IN ASSESSMENT OF FETAL CARDIAC FUNCTION: AN IN VIVO STUDY
Author links open overlay panelDavid J.SahnMeihuaZhuErikoShimadaColeStreiffSumitoKimuraMuhammadAshraf
Oregon Health & Science University, Portland, OR, USA
Background
This in vivo study was designed to compare the accuracy of stroke volume (SV) and left ventricular mass (LVM) determinations of fetal sized hearts by using four-dimensional echocardiography (4DE) and two-dimensional echocardiography (2DE) against sonomicrometry data and displacement values.
Methods
Eight open-chest rabbits were studied under baseline conditions, a 2ml/kg saline bolus, a 4ml/kg saline bolus, an inferior vena cava ligation, and an ascending aorta ligation. Sonomicrometry crystals were sutured at apex, left ventricular outflow tract, septum and posterior wall to determine SV. 4DE data was recorded using a Philips® iU-22 system and analyzed in QLab™ GI-3DQ program. 2DE images were recorded by GE Vivid E9 system and analyzed in EchoPAC.
Results
4DE-derived SV (r = 0.78) and LVM (r = 0.99) demonstrated superior linear correlations than 2DE derived SV (r = 0.703) and LVM (r = 0.88) when compared with sonomicrometry SV and displacement LVM under all conditions. Bland-Altman analyses showed slight bias on SV determination for 4DE (SV: +0.93 ml; LVM: −0.0076g), but higher overestimations for 2DE (SV: +1.56 ml, LVM: + 0.45 g).
Conclusions
4D echocardiography is feasible for determining stroke volume and ventricular mass in fetal heart under different conditions, it is more accurate that 2D echocardiography.
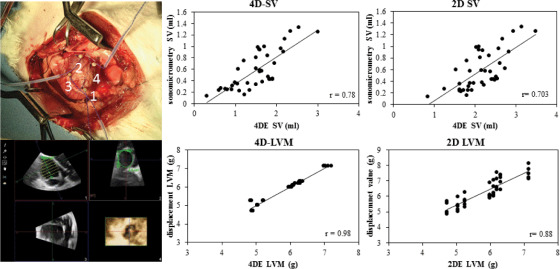
NEUTROPHIL/LYMPHOCYTE RATIO AND ASSOCIATION WITH ARCH INTERVENTION IN PATIENTS WITH HYPOPLASTIC LEFT HEART SYNDROME UNDERGOING HYBRID PROCEDURE
Author links open overlay panelElizabethMitchellJohnCheathamJamesSiskLisaNicholsonRalfHolzerMarkGalantowiczCliffordCua
Nationwide Children’s Hospital, Columbus, OH, USA
Background
Hybrid procedure is an alternative initial palliation for patients with hypoplastic left heart syndrome (HLHS). One major complication associated with this procedure is stenosis in the aortic arch isthmus possibly due to inflammation from the PDA stent. In adult studies, neutrophil/lymphocyte (N/L) ratio has been used as a marker for increased inflammation and has been associated with increased risk for coronary artery stent stenosis. Goal of this study was to determine if there were differences in N/L ratio between patients with HLHS undergoing the hybrid procedure that required an arch intervention versus those that did not require an intervention.
Methods
Retrospective chart review was performed on all patients with HLHS undergoing the hybrid procedure between 7/2002 to 1/2013. Complete blood counts as well as differentials were recorded at four time periods: one day pre-hybrid palliation, one day post-hybrid palliation, one week post-hybrid palliation, and 3 weeks post-hybrid palliation. Two-tailed T-tests were used to examine mean differences in all variables between patients requiring arch intervention (AI-Group) compared to those who did not require arch intervention (NAI-Group).
Results
One hundred six patients were evaluated (AI-Group = 38, NAI-Group = 68). AI-Group generally had a higher N/L ratio vs. NAI-group and this was significant immediately one day post-hybrid palliation: AI-Group vs. NAI-Group, pre-hybrid (2.95 + 2.62 vs. 2.44 + 1.71), one day post-hybrid (5.95 + 4.16 vs. 4.34 + 3.87*), one week post-hybrid (2.72 + 3.01 vs. 2.28 + 2.12), and 3 weeks post-hybrid (1.85 + 1.24 vs. 1.45 + 1.16), respectively. In addition, lymphocyte percentage was significantly lower in the AI-Group vs. NAI-Group three weeks post-hybrid palliation (33.00 + 11.30% vs. 40.65 + 16.82%).
Conclusion
Patients that required an arch intervention after hybrid palliation had a higher N/L ratio immediately after the procedure. This may signify an increased inflammatory reaction that places these patients at risk for stenosis. Future studies are needed to determine if N/L ratio is a robust marker to risk stratify patients undergoing the hybrid procedure for arch complications.
TIMING AND MODE OF DELIVERY IN PRENATALLY DIAGNOSED CRITICAL CONGENITAL HEART DISEASE: AN ANALYSIS OF PRACTICES WITHIN THE UNIVERSITY OF CALIFORNIA FETAL CONSORTIUM
Author links open overlay panelShabnamPeyvandiTina A.NguyenTracyAntonNina M.BoeLailaRhee-MorrisMarkSklanskyMaryamTarsaAnitaMoon-Grady
University of California San Francisco, San Francisco, CA, USA
Background
Prenatal diagnosis of congenital heart disease (CHD) is associated with decreased operative morbidity and mortality. However, prenatal diagnosis of CHD has also been associated with lower birth weights and lower gestational age at birth, which may influence long-term survival and neurodevelopmental outcomes. We sought to describe delivery practices in five University of California medical centers that perform prenatal diagnosis of CHD requiring neonatal intervention, and to correlate delivery practices with pre- and post- surgical outcomes.
Methods
The University of California Fetal Consortium (UCfC) campuses were surveyed on data regarding deliveries and outcomes for prenatally diagnosed neonates (</= 28 days) undergoing cardiac surgery between January 2011-2013. Data collected included gestational age (GA) at diagnosis of CHD, planned and actual delivery mode, planned and actual delivery GA, birth weight and postnatal data.
Results
A total of 178 patients were prenatally diagnosed with critical CHD. Of those, 130 were ductal-dependent and 20 required an additional immediate intervention after birth for extreme instability after separation from placental circulation. Mean birth weight for the entire cohort was 2.85 +/− 0.65 kg. Planned GA at delivery was a mean of 38.9 +/− 1.1 weeks and actual GA at delivery was 37.6 +/− 2.2 weeks. Mean GA at birth for infants alive at 30 days was 37.8 +/− 2.1 weeks and 36.5 +/− 2.6 weeks for those not alive at 30 days. Although the planned mode of delivery was induction of labor or natural in 70% of mothers and cesarean section in 30%, the majority of mothers delivered via cesarean (52%).
Conclusion
Current practices demonstrate that fetuses with critical CHD are delivered at a slightly earlier GA than planned and are delivered via cesarean more often than not. Cesarean delivery rates are higher as compared to the general population in California (33%). In addition, the mean gestational age at delivery for infants alive at 30 days was slightly later than for those not alive at 30 days. Further studies to assess the impact of current delivery practices on long-term outcomes are warranted to establish optimal delivery guidelines for fetuses with CHD.
TWIN REVERSED ARTERIAL PERFUSION CAUSES DECREASED FETAL CEREBRAL VASCULAR IMPEDANCE
Author links open overlay panelShabnamPeyvandiMichaelBrookVickieFeldsteinShinjiroHiroseLarryRandAnitaMoon-Grady
University of California San Francisco, San Francisco, CA, USA
Background
Twin reversed arterial perfusion (TRAP) sequence affects 1% of monochorionic (MC) pregnancies. Abnormal vascular connections between the pump and acardiac twin lead to high output heart failure in the pump twin causing hydrops or demise in up to 50% of pregnancies. Fetal intervention (radiofrequency ablation of blood supply to the acardiac fetus) has increased survival of pump twins to as high as 90%. The effects of a high output cardiac state in the pump twin (and effect of fetal intervention) on cerebral flow and vasculature are unknown. We hypothesize that abnormal cerebral vascular impedance, assessed by the pulsatility index (PI), is present in the pump twin and fetal intervention acutely alters cerebral impedance.
Methods
Fetal echocardiograms (ECHO) performed between January 2010- June 2013 for pregnancies with a diagnosis of TRAP (cases, n= 18) or uncomplicated MC twins (controls, n= 36/18 pairs) were retrospectively analyzed. We compared middle cerebral artery (MCA) PI of the pump twin against normal MC twins. In TRAP pregnancies, combined cardiac output (CCO) was calculated for the pump twin. Mean and 95% confidence intervals were calculated for all parameters. Two-sample t-test was used to compare cases and controls.
Results
The mean gestational age at ECHO was 20 weeks with no difference between groups (p= 0.73). CCO in the pump twins was mildly elevated for gestational age (199.7 +/− 127.2 mL/min). MCA PI was significantly lower in the TRAP pump twin compared to controls (1.55, 95% CI 1.47-1.64 vs. 1.74, 95% CI 1.65-1.82, p = 0.004). Post-intervention ECHO (within 24 hours of intervention) was available in six TRAP cases. MCA PI increased after intervention from 1.56 (95% CI 1.36-1.75) to 1.82 (95% CI 1.5-2.2).
Conclusion
TRAP pump twins in a high output state have decreased cerebral vascular impedance compared to normal MC twins, suggestive of a brain-sparing effect. MCA PI increased acutely in the pump twin after fetal intervention. These findings suggest a fetal cerebral autoregulatory response to a high cardiac output state that begins to normalize after fetal intervention. Long-term implications for neurodevelopmental outcomes in these patients deserves further study.
HIGH PREVALENCE OF RESPIRATORY CILIARY DYSFUNCTION ASSOCIATED WITH TRANSPOSITION OF THE GREAT ARTERIES
Author links open overlay panelMalihaZahidYouLiXinTianRichardFrancisNikolaiKenaOmarKhalifaWilliamDevineDong M.LeeCyrusYauKristenLemkeLindaLeatherburyKimimasaTobitaCecilia W.Lo
University of Pittsburgh, Pittsburgh, PA, USA
Background
Heterotaxy patients have randomized left-right patterning and exhibit a high incidence of airway ciliary dysfunction similar to that of primary ciliary dyskinesia (PCD), a reflection of the common requirement for motile cilia in left-right patterning and airway clearance. Transposition of the great arteries (TGA), a congenital heart defect that may be considered a laterality defect, is characterized by aorta transposed anteriorly and inserted into the right ventricle on the body’s left (L-TGA) or right (D-TGA). In this study, we investigated whether TGA patients may have PCD-like airway ciliary dysfunction and exhibit increased respiratory symptoms.
Methods and Results
We recruited 64 patients, 45 D-TGA and 19 L-TGA, and assessed ciliary function by measuring nasal nitric oxide (nNO), typically low with PCD, and obtained nasal scrapes for ciliary motion (CM) analysis by videomicroscopy. We found 35% (16/46) of the TGA patients had low nNO, and 59% (34 /58) had abnormal CM, with 25% (11/44) exhibiting both abnormal CM and low nNO. Respiratory symptoms were increased with abnormal CM, but not low nNO. Sequencing analysis showed TGA patients with CM defects had significantly more novel/rare coding variants in PCD genes, similar to PCD patients and heterotaxy(HTX) patients with CM defects. D vs. L-TGA patients were indistinguishable with respect to all these parameters.
Conclusions
We found high prevalence of CM defects in conjunction with increase respiratory symptoms and the enrichment of PCD gene sequence variants. These findings suggest TGA and HTX patients might share a common etiology involving motile cilia defects.
EXPERIMENTAL CONSTRICTION OF FETAL DUCTUS ARTERIOSUS, OXIDATIVE STRESS, AND POLYPHENOL EXCRETION AFTER MATERNAL POLYPHENOL-RICH DIET IN LATE PREGNANCY
Author links open overlay panelPauloZielinskyGuilhermeBubolsLuiz H.NicolosoAntonioPiccoliJrIzabeleVianAngelaMoroMarieleCharoNatliaBruckerRachelBulcoSabrinaNascimentoGabrielaGethelMarceloAlieviMelissaMarkoskiSolangeGarcia
Fetal Cardiology Unit, Institute of Cardiology, Porto Alegre, Brazil
Toxycology Department, University of Rio Grande do Sul, Porto Alegre, Brazil
Background
Maternal consumption of polyphenol-rich foods interferes with fetal ductus arteriosus flow in humans and its restriction reverses ductal constriction. We aimed to assess experimentally the interrelations of ductal dynamics, oxidative damage and polyphenol excretion after a high polyphenol intake in pregnant sheep.
Methods
Six pregnant sheep > 120 days of gestational age were fed for 2 weeks with a standardized amount of polyphenol-rich foods (basal intake 3100 mg/day). Fetal ductal systolic and diastolic flow velocities and PI obtained by Doppler echocardiography, lipid peroxidationrepresented by plasma TBARS, and urinary excretion of total polyphenols were assessed, before and 14 days after dietary intervention. Multiple comparison tests were used.
Results
A significant increase of ductal systolic and diastolic velocities (SV; DV) and a decrease in PI was shown after 14 days of intervention, when compared to the basal state (SV: 1.34 ± 0.01 vs. 0.75 ± 0.05 m/s, p < 0.001, DV: 0.28 ± 0.02 vs.0.18 ± 0.01 m/s, p<0.001; PI:,2.04 ± 0.11 vs. 2.54 ± 0.07m/s, p< 0.001), indicating fetal ductal constriction. Urinary total polyphenolexcretion increased significantly after intervention (687.47 ± 106.47 vs. 316.79 ± 30.31 mg GAE/g creatinine, p < 0.001). A decrease in lipid peroxidation was shown, determined by TBARS (15.50±0.20 mM), and by non-proteic reduced thiols after treatment. Oxidative stress was associated with ductal constriction, through proteic damage with SV (r =0.629, p=0.028), DV (r =0.905, p=0.0001), and PI (r=−0.772, p=0.003). Ductal SV was correlated with catalase (r=0.672, p= 0.033) and PI inversely with glutathione peroxidase (r=0.629, p=0.05). Ductal SV and DVs correlated to nitric oxide (r=0.853, p=0.0004 and r=0.705, p=0.010, respectively), and ductal PI (r=0.599, p=0.039). Antiinflammatory and antioxidantmechanisms (nitric oxide with glutathione peroxidase, and nitric oxide with catalase) were correlated (r=0.755, p=0.004 and r=0.812, p=0.001, respectively).
Conclusions
High maternal polyphenol consumption induced fetal ductal constriction in ewes with alteration in oxidative stress, because of its antioxidant and antiinflammatory actions.
DIASTOLIC FUNCTION IN FETUSES UNDERGOING FETAL AORTIC VALVULOPLASTY
Author links open overlay panelKevin G.FriedmanLindsayFreudDavidSchidlowMariaEscobarWayneTworetzky
Boston Children’s Hospital, Boston, MA, USA
Background
Fetal aortic valvuloplasty (FAV) has shown promise in averting progression of mid-gestation aortic stenosis (AS) to hypoplastic left heart syndrome (HLHS). Patients with biventricular circulation after FAV often have diastolic dysfunction (DD).
Methods
We compared fetal echo parameters of DD, including atrioventricular valve inflow and tissue Doppler, from pre-FAV studies on 21 consecutive fetuses to gestational age-matched controls (n=42). We collected pre- and post-FAV variables (1-3 days post procedure) and evaluated for acute change and for variables associated with postnatal biventricular (n=10) vs. univentricular circulation (n=8).
Results
Median gestational age (24 weeks, range 18-29 weeks), estimated fetal weight and fetal heart rate were similar between FAV and controls. Systolic function was severely depressed in all pre-FAV patients and normal in all controls. Pre-FAV patients were more likely to have mitral inflow E and A fusion (80% vs. 10 %, p<0.001), higher E velocity (0.49 vs. 0.27 m/s, p<0.001) and shorter mitral inflow time (108 vs. 168 ms, p=0.001). Pre-FAV patients had lower left ventricle (LV) lateral annulus E’ (2.2 vs. 3.9 cm/s, p=0.001), septal E’ (2.4 vs. 3.2 cm/s, p=0.003), and higher E/E’ (19.1 vs. 7.8, p< 0.001) than controls. They also abnormal right ventricular (RV) mechanics with higher tricuspid E velocity (0.40 vs. 0.30 m/s, p<0.001), shorter tricuspid inflow time (146 vs. 168 ms, p=0.03) and higher likelihood of E and A fusion (50% vs. 3%, p<0.001). Post-FAV, fewer patients had fused mitral inflow E and A than pre-FAV (45 vs. 80%, p=0.05) and septal E’ improved (2.8 vs. 2.3 cm/s, p=0.03). On post-FAV fetal echo, LV E’ (4.0 vs. 2.6 cm/s, p=0.05) and RV E’ (6.2 vs. 3.8 cm/s, p=0.06) were higher in those who achieved postnatal biventricular circulation compared to HLHS group. There were no differences in DD parameters on pre-FAV echo between patients with HLHS and biventricular circulation.
Conclusions
Fetuses with mid-gestation AS have evidence of marked DD. Indices of DD may be helpful in determining likelihood of postnatal biventricular circulation after FAV. Additional data is needed to determine if DD improves after FAV.
MANAGEMENT AND OUTCOMES OF COMPLEX, MULTIPLE VENTRICULAR SEPTAL DEFECTS IN CHILDREN
Author links open overlay panelBenjamin W.KozyakRekhaGadiparthiLuis G.QuinonezJamesLockDoffMcElhinneyDavidBrownSitaramEmani
Boston Children’s Hospital, Boston, MA, USA
Harvard Medical School, Boston, MA, USA
Background
Management of multiple ventricular septal defects (mVSD) remains a challenge. While most VSDs can be closed surgically via the tricuspid valve, those in the apical trabecular septumare more complicated and may require several procedures. Approaches have included apical ventriculotomy and transcatheter device placement; the optimal strategy remains unclear.
Methods
Retrospective analysis of 187 patients (age 2d-27y) with mVSD who underwent surgical and/or catheter-based closure 2000-2012.
Results
Types of VSD: multiple muscular (123 patients), apical muscular (90), membranous (60), conoventricular (47), AV canal defect (CAVC, 9). mVSD were isolated in 47% of patients and associated in 53% with: coarctation (17%), transposition of the great arteries (17%), tetralogy of Fallot (7%), double-outlet right ventricle (DORV, 6%), CAVC (7%), and mitral stenosis (5%). Primary surgical closure was performed in 133 patients (71%), and was definitive in 113 (60%). Ventricular incisions (46) were infundibular in 20, apical RV in 23, LV in 3. VSD management required ≥2 procedures in 68 patients (36%) and ≥3 in 30 (16%). These included pulmonary artery banding (PAB) in 41 and device implant in 40 (multiple devices in 15). Multiple procedures were more frequent in patients with apical VSD (p=0.05) or DORV (p<0.01). Devices were more often used in those with >mild LV dysfunction (p=0.02). In 17/46 patients with residual VSD referred to cath, subsequent surgery was not needed. Three patients were palliated to a single ventricle circulation. Residual VSD shunt at follow-up (mean 43 mos) was ≤mild in 88% of patients. RV pressure (RVp) was ≤mildly elevated in 75%. Global RV/LV dysfunction was ≤mild in 94%. There were 14 deaths. Patients with multiple muscular VSD tended toward higher RVp (p=0.08) and those with apical VSD or CAVC toward larger residual shunt.
Conclusion
Primary surgical closure is successful in the majority of patients with mVSD. Apical right ventriculotomy appears to be well tolerated. Patients with apical defects, DORV or CAVC benefit from collaboration between surgeons and cardiologists with expertise in device closure, which may mitigate the need for multiple bypass operations.
LOWER EXTREMITY ARTERIAL FUNCTION IN CHILDREN AT RISK FOR ARTERIAL INJURY AFTER CARDIAC CATHETERIZATION
Author links open overlay panelAndrew C.GlatzSamirShahKatherineBatesAnnMcCarthyKaitlynDanielsDaweiXieXueWangYoavDoriMatthewGillespieEmileMohlerJonathanRome
Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, USA
Background
Arterial injury is a known complication after pediatric cardiac catheterization, particularly for infants <6 months. Longer-term sequelae of arterial cath in these patients have not been studied. We sought to characterize lower extremity arterial function in children at-risk for arterial injury after cath.
Methods
A cross-sectional assessment of lower extremity arterial function was performed in a cohort of children >1 year after arterial cath (performed at age <6 mos), including parental claudication questionnaire, exam, anthropometry, and vascular Doppler ultrasound (US).
Results
119 children were studied at median follow-up of 4 (range: 1.2 – 6.8) years after first arterial cath, at 4.3 ± 1.7 years of age and 16.2 ± 4.2 kg. Symptoms suggestive of claudication were reported in 27%. For the overall cohort, the cathed leg more frequently had a weaker pulse (≥2 grades of pulse amplitude asymmetry, 7.6% v. 1.7%, p=0.03). There were no differences in blood pressure indices or anthropometric measures between legs. The cathed leg had significantly lower peak systolic velocity (PSV) in the superficial femoral artery (SFA) (p=0.002), lower pulsatility (p=0.007) and resistive (p=0.02) indices in the common femoral artery (CFA) and higher prevalence of pulse waveform abnormality (34% v. 20%, p=0.006). For the 33 subjects with known post-cath thrombus, the cathed leg had a weaker pulse (9.1% v. 0%, p=0.0006), smaller thigh and calf circumferences (p=0.05), lower PSV (p=0.002), lower pulsatility and resistive indices in the SFA (p=0.04), and more prevalent CFA pulse waveform abnormalities (p=0.008). 9 patients (7.6% of cohort) had ≥2 cm limb length discrepancy. In 8/9, the shorter leg was previously cathed.
Conclusion
In children at-risk for post-cath arterial injury, clinical abnormalities in the cathed leg were infrequent, although femoral artery flow disturbances were seen by US. In a subset with known post-cath thrombus, however, there were significant clinical differences in the cathed leg, including limb length discrepancy. This suggests that, while sub-clinical injury may not occur, patients with post-cath thrombus may be at increased risk for longer-term sequelae.
LEFT VENTRICULAR DYSFUNCTION FOLLOWING NEONATAL PULMONARY VALVE BALLOON DILATION FOR PULMONARY ATRESIA OR CRITICAL PULMONARY STENOSIS
Author links open overlay panelChristinaRonaiRahulRathodAudreyMarshallKimberleeGauvreauStevenColanDavidBrown
Boston Children’s Hospital, Boston, MA, USA
Background
Pulmonary valve (PV) balloon dilation (BD) is the primary therapy for infants born with critical pulmonary stenosis or membranous pulmonary atresia with intact ventricular septum(PAIVS). We have observed left ventricular (LV) dysfunction in patients following BD, and sought to determine its incidence, clinical course and associated risk factors.
Methods
Clinical, echocardiographic and catheterization data for all patients who underwent neonatal (<2 weeks age) PV BD for critical pulmonary stenosis or PAIVS between January 2000 and September 2013 were retrospectively analyzed (n=127). Post-procedure LV dysfunction was defined as an ejection fraction (EF) <54%.
Results
Median age at PV BD was 1 day. Most (71%) patients had critical PS. Median PV diameter pre-BD was 6.0mm with PV z-scores −4.1 to 0.9, median LV EF pre BD was 58%. Post-BD LV dysfunction developed in 44 pts (35%); 14 patients had LV EF ≤40%. Median time course to normalization of LV EF was 10 days (range 3-72 days) in those with serial echo follow-up. Acute procedural complications, all right ventricular outflow tract perforations, occurred in 7 patients (5.5%), all were managed medically. In univariate analysis, diagnosis type (critical pulmonary stenosis or PAIVS), right ventricle to LV pressure ratio pre-BD, acute procedural complication and post BD inotropic support were not associated with post BD LV dysfunction. In multivariable analysis, the only statistically significant predictors of post-procedure LV dysfunction were lower PV z-score (median −2.1 vs. −1.6, p 0.005) and larger tricuspid valve lateral dimension z-score (median 1.0 vs. 0.1, p 0.01), with a trend towards lower pre-dilation right ventricular pressure in those with post LV dysfunction (94 vs. 105 mmHg, p 0.09).
Conclusion
LV dysfunction post neonatal PV BD develops in a significant number of patients (35%) and can be severe, but appears to resolve in short term. The risk for developing LV dysfunction post PV BD is highest in patients with smaller PV z-scores and larger tricuspid valve z-scores. While further study is necessary, this may be related to increased potential for ventricular-ventricular interaction in those with larger right ventricles.
PREVALENCE OF DEFICIENT RETRO-AORTIC RIM AND ITS EFFECT ON OUTCOME IN DEVICE CLOSURE OF ATRIAL SEPTAL DEFECTS
Author links open overlay panelMichael L.O’ByrneAndrewGlatzSherzanaSunderjiAswathiMathewDavidGoldbergYoavDoriJonathanRomeMatthewGillespie
The Children’s Hospital of Philadelphia Division of Pediatric Cardiology, Philadelphia, PA, USA
Background
Deficient retro-aortic rim has been identified as a potential risk factor for aortic erosion, following device closure of atrial septal defects (ASD). However, the prevalence of deficient retro-aortic has not been well defined. The purpose of this study was to report the prevalence of retro-aortic rim in children and adults undergoing device closure of ASD and to determine whether deficient retro-aortic rim was a risk factor for technical failure or adverse outcome.
Methods
A single-center retrospective cohort study of 445 consecutive subjects of median age 5.9 years (range: 0.8-80 years) undergoing cardiac catheterization for possible device occlusionof ASD between 1/1/1999 and 4/1/2012 was performed. Risk factors for early and mid-term major adverse events were assessed using univariate and multivariate logistic regression.
Results
Of subjects with reviewable echocardiograms, 60% had deficient retro-aortic rim. No attempt was made at device closure in 3.6% of subjects. Of the remaining 429 subjects, 96% underwent successful device occlusion. Major early adverse events occurred in 1.2% (95% CI: 0.4-2.7%) of cases, all either device embolization or malposition. Deficient retro-aortic rim was not a risk factor for composite outcome of technical failure or early major adverse event on multivariate analysis. No deaths, late re-interventions, or aortic erosion events occurred over 2395 total person-years of follow-up (median 5.8 years). Deficient retro-aortic rim was associated with increased risk of device impingement on the aorta, but no association was seen between device impingement or deficient retro-aortic rim and the development of new/progressive aortic insufficiency.
Conclusion
Deficient retro-aortic rim is highly prevalent, but was not associated with increased risk of adverse outcomes. Its contribution to the risk of aortic erosion could not be addressed by this study.
REDUCTION OF ADVERSE VENTRICULAR INTERACTION AFTER TRANSCATHETER PULMONARY VALVE REPLACEMENT IN PATIENTS WITH RIGHT VENTRICULAR OUTFLOW TRACT OBSTRUCTION
Author links open overlay panelFatimaLunzeBabarHasanKimberleeGauvreauDavidBrownStevenColanDoffMcElhinney
Boston Children’s Hospital, Boston, MA, USA
Background
Transcatheter pulmonary valve replacement (TPVR) for postoperative right ventricular outflow tract obstruction (RVOTO) improves biventricular function and exercise capacity over the short term, but the longer term effects on adverse ventricular interaction are unknown.
Methods
This study investigated changes in ventricular interaction and remodeling in 24 patients (17 tetralogy of Fallot) who underwent TPVR for predominant RVOTO (median age 18 yrs). Patients were evaluated with conventional and speckle tracking strain echocardiography and cardiopulmonary exercise, testing before TPVR, early post-TPVR (median 6 mo), and at mid-term follow-up (FU; median 2.5 yrs). Strain data were compared to healthy age- and heart rate-matched controls.
Results
The maximum RVOT gradient decreased from baseline to early post-TPVR (59±24 to 25±9 mmHg, P<0.001), as did RV end-diastolic and end-systolic areas (P=0.017 and P=0.014, respectively). End-diastolic and end-systolic LV eccentricity (leftward shift of the interventricular septum) improved early after TPVR (1.37±0.18 to 1.26±0.20, 1.33±0.23 to 1.17±0.19, respectively; both P=0.001), and end-diastolic septal shift improved further at mid-term FU (to 1.12±0.13, P=0.017). LV longitudinal, circumferential, and radial strains were below normal at baseline (-22±1% vs. −17±3%, −29±3% vs. −24±4%, −37±5% vs. −27±8%, respectively; all P<0.001) and gradually recovered by mid-term (all P≤0.004). RV longitudinal strain was impaired at baseline (-15±3%), but improved early post-TPVR (to −17±3%, P<0.001) and further at mid-term FU (to −21±3%, P<0.001), although it remained lower than in controls (-29±2%, P<0.001). Peak oxygen uptake improved early post-TPVR (from 69±16% of predicted to 80±16%, P=0.006), and further at mid-term FU (to 82±13%, P=0.018 vs. early).
Conclusions
There was adverse ventricular interaction due to leftward septal shift associated with biventricular dysfunction at baseline. Relieving RVOTO with TPVR led to progressive improvement in biventricular function and reduced septal shift at early and mid-term FU. In patients with RVOTO, positive functional remodeling continues beyond the acute effects of TPVR.
CUMULATIVE MEDICAL RADIATION EXPOSURE THROUGHOUT STAGED PALLIATION OF SINGLE VENTRICLE CONGENITAL HEART DISEASE
Author links open overlay panelTacy E.DowningAliciaMcDonnellXiaoweiZhuYoavDoriMatthewGillespieJonathanRomeAndrewGlatz
The Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Background
Patients with single ventricle heart disease undergoing staged palliation are exposed to ionizing radiation from multiple medical sources. As long-term survival improves, the potential consequences of such exposure become increasingly relevant. We sought to quantify typical radiation burden in this population and identify risk factors for increased exposure.
Methods
We retrospectively reviewed all single ventricle patients born 1/1/2009 or later who underwent Fontan completion by 5/31/2012 and had cardiac care exclusively at our institution. All studies utilizing ionizing radiation and occurring from birth through Fontan hospital discharge were compiled. Exposures were converted to effective dose (mSv) to permit comparison across modalities.
Results
38 patients were followed for a median of 33 months. 50% underwent a Norwood procedure, 71% had a systemic right ventricle and 18% had heterotaxy syndrome. A median of 59 (range 26-180) radiation events occurred during the study period, with a median cumulative effective dose of 25.7 (4.7-113.8) mSv. On average, cardiac catheterization accounted for 4% (2-11%) of patient radiation encounters, but comprised 78% (20-98%) of cumulative radiation exposure. In a multivariate model, factors associated with increased total radiation exposure included pulmonary artery (PA) stenosis requiring intervention (p =0.005) and systemic right ventricle (p = 0.02). Risk factors for increased exposure from catheterizationincluded heterotaxy (p = 0.007), re-coarctation (p = 0.003) and PA stenosis (p = 0.02). The highest burden of non-cath radiation for the overall cohort was derived from x-rays, but nuclear medicine contributed significantly in 13 patients who required gastric emptying studies.
Conclusions
At our institution, many single ventricle patients are exposed to substantial radiation through the palliative surgical stages, the majority of which derives from cardiac catheterization. PA stenosis was identified as a risk factor for increased total and catheterization-based exposure. As long-term survival improves, awareness of this scale of radiation exposure at a vulnerable period is imperative.
STROKE IN PEDIATRIC CARDIAC SURGICAL PATIENTS ON EXTRACORPOREAL MEMBRANE OXYGENATION: AN ANALYSIS OF THE EXTRACORPOREAL LIFE SUPPORT ORGANIZATION DATABASE
Author links open overlay panelDavidWerhoSaraPasqualiSunkyungYuJanetDonohueGailAnnichRaviThiagarajanJenniferHirschMichaelGaies
University of Michigan, Ann Arbor, MI, USA
Boston Children’s Hospital, Boston, MA, USA
Background
Stroke is a common complication of extracorporeal membrane oxygenation (ECMO), and pediatric cardiac surgical patients on ECMO, particularly neonates or those with complex repairs, may be at higher risk. However, the epidemiology and predictors of stroke in these patients are not well-characterized.
Methods
We performed an analysis of the Extracorporeal Life Support Organization (ELSO) Registry from 2002-2013 under ELSO data sponsorship, including initial ECMO runs for all patients ≤18 years-old. Cardiac patients were identified using diagnostic and procedure codes and surgical patients were identified using ELSO procedure codes. Procedures were mapped to STAT (Society of Thoracic Surgeons-European Association of Cardiothoracic Surgery) morbidity categories to define complexity. The primary outcome was any stroke (neurologic hemorrhage or infarction). Risk factors for stroke in surgical patients were analyzed using multivariate logistic regression.
Results
The cohort included 4,797 cardiac patients, 74% (3,563) with cardiac surgery. Of the surgical cohort, 54% were neonates, 81% had cyanotic disease and 57% were in high STAT categories (4-5). Overall, 12% had a stroke on ECMO with similar rates in surgical and non-surgical patients (p=0.5). Patients with stroke had higher in-hospital mortality compared to those without (53% vs. 25%, p<0.0001). Multivariable analysis of the surgical cohort found independent associations with stroke for neonates (adjusted odds ratio [AOR] 1.7, 95% confidence interval [CI] 1.3-2.3), lower weight-for-age z-score (AOR 1.2 for each one-point decrease, CI 1.1-1.3), and longer ECMO duration (upper quartile [≥168 hours] AOR 1.4, CI 1.1-1.8). Cyanotic disease, STAT category and bypass time were not associated with stroke in this model.
Conclusion
In this multicenter analysis, we found that pediatric cardiac surgical patients on ECMO have a high rate of stroke comparable to non-surgical patients, and that stroke doubles the likelihood of in-hospital mortality. We did not identify modifiable risk factors in this cohort. Future study is necessary to determine if anticoagulation or other practices can be modified to reduce stroke incidence.
THE EFFECT OF VARIOUS RADIATION SHIELDS ON OPERATOR EXPOSURE DURING CONGENITAL CARDIAC CATHETERIZATION
Author links open overlay panelSarosh P.BatlivalaDenniseMagillMarc A.FeliceVirginiaJonesYoavDoriMatthewGillespieJonathanRomeAndrewGlatz
The Children’s Hospital of Philadelphia, Philadelphia, PA, USA
The University of Pennsylvania, Philadelphia, PA, USA
Background
Cardiac catheterization personnel are exposed to occupational radiation and its attendant health risks. Little data exist regarding the efficacy of radiation-protective equipment used in congenital catheterization laboratories (CLs).
Methods
We retrospectively reviewed data collected prospectively for a continuing quality improvement initiative in which primary CL operators wore a radiation dosimeter, external to the lead apron, during procedures on patients >20 kg. A leaded undertable skirt was used in all cases. Three additional radiation-protective devices were used at operator discretion and in any combination: a top extension to the undertable skirt, a ceiling-mounted shield, and a radiation-attenuating bismuth disposable drape placed over the patient’s legs. All devices are designed for operator position at the groin. Case details, operator position, fluoroscopytime, patient air KERMA (aK, mGy), and dose-area product (DAP, μGy-m2) were recorded.
Results
Data from 136 catheterizations were studied. The median operator dose (OpD) was 12 μSv (range 0-930), and was indexed to patient aK and DAP to correct for patient factors and case times. Indexed OpD decreased significantly with each additional shield used (14.8 v. 6.6 v. 5.3 v. 1.3 μSv*1000/μGy-m2 and 12.4 v. 4.6 v. 3.9 v. 1.4 μSv*100/mGy with 1, 2, 3, and 4 shields, respectively, p<0.001). This trend was not significant in the 45 cases with the operator at head-of-bed. Combinations of shielding which included the ceiling mount had the lowest indexed OpD. The patient drape did not further reduce OpD when all 3 other shields were in use (1.3 v. 2.2 μSv*1000/μGy-m2, p=0.5; and 1.4 v. 1.7 μSv*100/mGy, p=0.4) and was associated with higher patient exposure indexed to patient weight and fluoroscopy time (4.5 v. 3.1 μGy-m2/kg-min, p=0.009; and 0.51 v. 0.38 mGy/kg-min, p=0.01).
Conclusions
Utilizing x-ray attenuating barriers in addition to a leaded table skirt can significantly decrease operator-absorbed radiation. A ceiling mounted shield may provide the greatest benefit. Routine use of radiation-attenuating patient drapes may not be warranted given minimal benefit to the operator and potential increase in patient dose.
ACUTE, EARLY AND INTERMEDIATE EFFECTS OF A NOVEL 8 MM DIAMETER DOUBLE OPPOSED HELICAL BIODEGRADABLE STENT IN PORCINE ARTERIES
Author links open overlay panelCarrie EvansHerbertSurendranath VeeramReddyTreWelchJianWangJamesRichardsonJosephForbessAlanNugent
University of Texas Southwestern, Dallas, TX, USA
Background
Double opposed helical (DH) biodegradable stents (BDS) enable manufacturing to diameters applicable to congenital heart disease. The primary objective is to evaluate delivery and deployment of 6 and 8mm diameter DH BDS in a porcine animal model. Secondary objectives are to evaluate patency, thrombosis, and inflammation at 1-week, 1 and 9-months.
Methods
6 and 8mm diameter DH BDS were manufactured with poly-L-lactic acid fiber and delivered in the external iliac artery (EIA) and distal descending aorta (DAO) of Sinclair minipigs. Patency and thrombosis was assessed at 1-week, 1 and 9-months with angiography and intravascular ultrasound. Histopathology was performed at each time interval.
Results
14 stents were placed in 9 animals: 8mm (8) and 6mm (1) were delivered in the DAO and 6mm (5) in the EIA. The 8mm diameter stent required a 9Fr delivery sheath. 8mm stents were frequently too small for this model with embolization of 4/9 stents requiring recapturing and redilation. All stents remained patent with no thrombosis. There was mild neointimal proliferation (NIP) at 1 week and 1 month and moderate NIP at 9-months follow-up. Neoendothelialization was complete at 1 month.
Conclusions
DH BDS designed to 8mm diameter have been manufactured and implanted. A sustained, significant inflammatory response with moderate NIP was seen at 9 months. Further improvements in fiber properties, investigation of anti-inflammatory drug coatings and miniaturization for ease of delivery are needed.
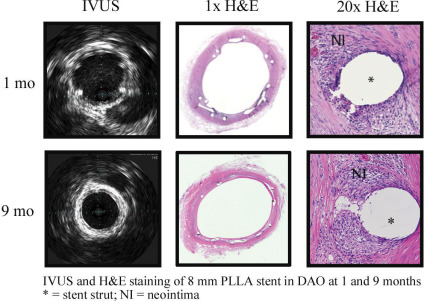
CLINICAL AND GENETIC FEATURES OF PULMONARY VEIN STENOSIS
Author links open overlay panelMing HuiChenChristopherDebbautKerryMcEnaneyAmyRobertsKimberleeGauvreauKaraWesternChristinaIrelandChristopherBairdKathyJenkins
Boston Children’s Hospital, Boston, MA, USA
Background
Pulmonary vein stenosis (PVS) is a rare and frequently lethal disease. PVS has been reported concomitantly with congenital heart disease (CHD), as well as chronic lung disease (CLD). In this single-center study we examined the association of PVS with CHD and CLD, along with genetic abnormalities seen with PVS.
Methods
An existing registry of all PVS patients seen at Boston Children’s Hospital (BCH) was reviewed, and all patients evaluated between 8/15/2006 to 12/1/2012 were included in this study (n=88). PVS was defined as intraluminal pulmonary venous obstruction in ≥2 vessels with mean pressure gradients >4mm Hg. Thirty-three patients (37.5%) were consented to clinical genetic evaluation and karyotyping.
Results
Eighty-eight patients with PVS (58% male, median age of PVS diagnosis: 5 months, range 0.2-49.6 months) formed our cohort. Twenty-nine patients (33%) were born at < 36 weeks gestation (median: 30 weeks, range: 25-36 weeks). Seventy-five patients (85.2%) had concomitant CHD, of which 17 (19.3%) also had CLD. Six patients (6.8%) were diagnosed with isolated PVS without concomitant CHD or CLD. Fifty-two patients (59.1%) were diagnosed with multiple CHD lesions. Post-natal CHD diagnoses included atrial septal defect(45.5%), anomalous pulmonary venous return (39.8%), patent ductus arteriosus (31.8%), and hypoplastic left heart syndrome (13.6%). Thirty-eight patients (43.1%) were diagnosed with pulmonary hypertension. Karyotyping and clinical genetic evaluation were available in 33 patients (37.5%). Of those, chromosomal abnormalities or specific genetic diagnoses were present in 23 patients (69.7%), while 10 (30.3%) had normal results. Among patients with genetic abnormalities, 6 (26.1%) were diagnosed with trisomy 21, 2 (8.7%) with Smith-Lemli-Opitz syndrome, and 6 (26.1%) with multiple chromosomal abnormalities. No karyotypic abnormalities were highly recurrent.
Conclusion
In patients with PVS, complex CHD was common. Gross chromosomal abnormalities were surprisingly prevalent, but there was significant genetic heterogeneity. Future prospective genetic evaluation in PVS is likely to be informative.
THREE-DIMENSIONAL ECHOCARDIOGRAPHIC PREDICTORS OF SUCCESSFUL BALLOON DILATION FOR CONGENITAL VALVAR AORTIC STENOSIS
Author links open overlay panelRamakrishnanSivasubramanianAnitaSaxenaNaveenKhannaSaurabhGuptaRajnishJunejaShyamKothari
All India Institute of Medical Sciences, New Delhi, India
Background
Aortic valve Balloon Dilatation (AVBD) is the procedure of choice in children and adolescents with congenital aortic valve stenosis. Predictors for the success or failure of AVBD have not been well defined. We evaluated the 3 D (Three-dimensional) echocardiographic predictors of successful AVBD.
Methods
We studied 27 patients with a diagnosis of severe congenital aortic stenosis, aged 6 months – 21 years, who underwent AVBD at our institute. Routine 2D and 3D transthoracic echocardiography was done before AVBD. Morphological details of the aortic valve as seen on 3 D echocardiography were recorded including mobility, thickness, area of the cusps and calcification, if any. We calculated a leaflet score by addition of grades of calcium, mobility, and thickness. All patients underwent AVBD as per institutional protocol. A repeat echo including 3D echocardiography was performed within 24 hours of AVBD. Successful AVBD was defined as more than 50% reduction in peak gradient with final gradient < 40 mmHg in the absence of any complication including more than mild AR.
Results
AVBD could be performed in all 27 patients. Aortic valve orifice area increased from 0.67 ± 0.22 cm2 to 1.56 ± 0.36 cm2 with a fall in peak gradients from 97.2 ± 41.0 mmHg to 38.0 ± 18.3 mm of Hg. A total of 7 patients had unsuccessful procedure as defined by pre-specified criteria described above. Valves with restricted mobility and increased thickness had statistically significant chances of a failed procedure. Mean leaflet score in patients who had a successful AVBD was 3.80 ± 1.24 as compared to a mean leaflet score of 5.57 ± 0.78 in patients who had an unsuccessful AVBD (p = 0.002).
Conclusions
Good enface images of the aortic valves are possible with trans-thoracic 3D echocardiography and it complements 2D echocardiographic findings. Aortic leaflet score derived from morphological features like mobility, thickness, and calcium of the aortic cusps by 3 D echocardiography may be helpful in predicting the outcomes of AVBD. These findings need to be evaluated in larger studies.
IMPLANT AND CLINICAL CHARACTERISTICS FOR PRIMARY VERSUS SECONDARY PREVENTION ICD INDICATIONS FOR PEDIATRIC AND CONGENITAL HEART PATIENTS IN THE NCDR®
Author links open overlay panelChristopher PhillipsJordanVicki A.FreedenbergJepthaCurtisYongfeiWangMaryeGlevaCharles I.Berul
Children’s National Medical Center, Washington, DC, USA
Yale School of Medicine, New Haven, CT, USA
Background
The ICD Registry® began collecting pediatric and congenital heart disease (CHD) specific data with version 2.1 in April 2010. There is limited data on who are these patients and their indications for ICD.
Methods
ICD procedures between April 2010 – December 2012 in the ICD Registry for all patients with CHD or < 21 years were included. Variables included implant indications, demographic, diagnostic and clinical history. Univariate associations with F-test in ANOVA for continuous variables and c2 test for categorical variables were used.
Results
There were 4,614 ICD procedures in 4,527 patients in the study cohort, of which 3,076 patients had CHD and 1,576 patients were < 21 years. The mean age was 40.0 + 24.6 years (range 0-92 years). CHD patients underwent 3,139 ICD procedures. Implant indications were 1 prevention in 2,819 (61%) and 2 prevention in 1,630 (35%). Among CHD patients, tetralogy of Fallot (TOF, 379/751=51%) and common ventricle (13/25=52%) had highest rates of 2 prevention. Among pediatric non-CHD group, primary electrical disorders (296/516=57%), CPVT (18/23=78%), and idiopathic VT/VF (80/120=67%) had highest rates of 2 prevention. 1 prevention patients had higher NHYA scores than 2 prevention patients. Pediatric cardiologists performed only 153 cases (9.6%) in patients <21 years and 187 cases (4.1%) in the total study cohort.
Conclusions
This is the largest pooled analysis of ICD implantation characteristics in CHD or pediatrics. Rates of 1 prevention implantation exceeded 2 prevention for the total cohort and specifically among pediatric patients. 2 prevention represented a majority for TOF, common ventricle, CPVT, and idiopathic VT/VF patients. Pediatric cardiologists accounted for implanting < 5% of all CHD and pediatric ICD patients in ICD Registry. Greater participation by pediatric electrophysiologists in the ICD Registry is desirable to accurately measure quality and outcomes of care in pediatric and CHD patients receiving ICD therapy.
MID-TERM RESULTS FOLLOWING CARDIAC RESYNCHRONIZATION THERAPY FOR PATIENTS WITH COMPLEX CONGENITAL HEART DISEASE
Author links open overlay panelMohamad KhaledAl-AhdabDavidRobersonIraShettyAnneFreterVivianCuiJanisDennisFrankZimmerman
Advocate Children’s Hospital, Oak Lawn, IL, USA
Background
Cardiac resynchronization therapy (CRT) is a valuable adjunct to treatment of refractory congestive heart failure in adults with wide QRS. Favorable short term outcomes have been reported in patients with complex congenital heart disease (CHD). However, there is limited data on mid-term follow up of those who have undergone CRT.
Methods
Retrospective review of consecutive cases of CRT in pts with complex CHD at a single center. Functional status (NYHA) and echocardiographic findings (ejection fraction, 3D ventricular synchrony parameters) were compared at baseline, acutely after CRT (within 6 months) and at last follow-up.
Results
The study included 17 consecutive pts with CHD who underwent CRT (ages 3-68 yrs, mean 23.5yrs). Diagnosis was single ventricle (5), systemic RV (6), and systemic LV (6). 12 pts (70.5%) had ventricular pacing prior to CRT upgrade. Age at time of CRT was 1-61 yrs (mean 21 yrs) and follow-up after CRT was 1-7.5 yrs (mean 4.7 yrs). Overall acute response to CRT occurred in 10 pts (59%). 5 had improved echo findings and 5 had both improved functional status and echo findings. At mid-term follow-up, 14/17 pt’s status remained unchanged (stable) but 3/17 pts had deterioration of function. 2/3 pts [1: Double inlet LV/AV block, 2: Double outlet RV/unbalanced AV canal/Pulmonary arterial (PA) band] had initial significant positive response to CRT with late deterioration at 2-3 yrs. 1/3 pts (L-Transposition of the great arteries/ PA band) had no change with CRT and had progressive deterioration of cardiac function.
Conclusions
This is the first study to report the mid-term outcomes of CRT in pts with CHD. Overall, a positive response to CRT was seen in 59% with the majority having stable functional status and echocardiographic findings at mean 4.7 yrs follow-up. Importantly, 20% of pts (2/10) who had an initial positive response to CRT later developed further decline in function over time. Long-term predictors of mortality and morbidity for those patients who respond positively to CRT remain poorly investigated and further studies are needed to select good long-term responders.
DIRECT VENTRICULAR CONTRACTILITY EVALUATION ASSURES RESPONSE FOR RESYNCHRONIZATION PACING AMONG CONGENITAL HEART PATIENTS WITH REFRACTORY HEART FAILURE
Author links open overlay panelPeterKarpawichHarinderSinghYamunaSanil
The Children’s Hospital of Michigan/Wayne State, Detroit, MI, USA
Background
Cardiac resynchronization pacing (CRT) can be an effective mode of therapy in patients (pts) with advanced heart failure (HF). But there are no selection criteria applicable to pts with congenital heart defects (CHD). QRS duration varies with age, dyssynchrony can exist with a narrow QRS, CHD pts often have pacemakers (PM), and accurate ejection fractionestimation is difficult in some CHD anatomies. The aim of this study was to evaluate utilization of direct hemodynamics as selection criteria for CRT among CHD pts and their outcomes.
Methods
This was a review of CHD pts with medically refractory HF, who were considered for orthoptic heart transplant (OHT) listing from 1999-2013. Pts underwent cardiac cathterization comparing intrinsic versus temporary CRT paced rhythm hemodynamics to determine efficacy of CRT. Comparative QRS duration, ventricular pressures and contractility indices (dP/dt; dP/dt/p), were obtained. Pts showing acute CRT paced dP/dt improvement >15% from baseline underwent permanent CRT in lieu of OHT listing.
Results
A total of 15 CHD pts, 4-28y (mean 19), with refractory heart failure (NYHA class 3-4) met benefit criteria and underwent CRT. CHD included repaired septal defects, d-TGA/Mustard, Tetralogy of Fallot, congenital AV block, and single ventricle. Most (60%) had surgical AV block with preexisting PM. Temporary CRT acutely improved dP/dt (mean 571 vs. 807mm Hg-sec (p=0.007). QRS duration and pressures did not show any significant change with CRT. After permanent CRT, all pts improved clinically (NYHA class 1-2) and were removed from transplant consideration. On clinical follow-up from 4-144mos (mean 41), 4 were re-listed and received OHT, 2 died of non-HF causes, and 9 showed clinical stability (repeat dP/dt mean 842mmHg).
Conclusions
CHD pts with refractory HF pose a dilemma for management. OHT is not always a viable option. CRT implant has morbidites. Preselecting CHD patients, with medically refractory heart failure, by determining paced ventricular contractility effects prior to permanent CRT implant, helps to assure a favorble response to improve pt lifestyle and/or act as a bridge to eventual OHT.
SPORTS FOR YOUNG PATIENTS WITH IMPLANTABLE CARDIOVERTER-DEFIBRILLATORS: REFINING THE RISK
Author links open overlay panelElizabethSaarelThomasPilcherDavidGamboaSusanEtheridge
University of Utah, Salt Lake City, UT, USA
Background
Despite data suggesting positive outcomes from sports and recent data about safety, current guidelines restrict those with implantable cardioverter-defibrillators (ICDs). Nonetheless many pediatric and young adult congenital heart (CHD) patients choose to participate regardless of expert recommendations. We examined the safety of sports participation for young patients with ICDs who choose to play.
Methods
Athletes with an ICD >/= 10 yr were enrolled in a prospective registry at a single pediatricand CHD center. Inclusion criteria were regular participation in competitive or dangerous sports greater than 1A. Pre-specified outcomes included death, injury, shocks or change in ICD system function. Data collected were type and level of sport participation, ICD generator and lead performance indices, number of appropriate (AS) and inappropriate shocks (IS), device or shock related complications, injury, and death or cardiac transplant.
Results
There were 21 athletes enrolled, 10 (48%) with CHD, 6 (28%) with inherited arrhythmiasyndromes, and 5 (24%) with cardiomyopathy. Mean age at enrollment was 16 years (range 10-40) and mean weight was 63 kg (range 21-104). Mean follow up was 5 years (range 2-6). Most common sports were basketball and baseball. Other sports were soccer, football, skiing, snowboarding, tennis, weight lifting, track, rock climbing, competition dance and rock climbing. There were 5 athletes on high school varsity, 2 on junior varsity, and 2 on organized college teams. During follow-up 7 (33%) received AS, 2 occurred during sports. One (5%) received IS for SVT during sports and in the setting of medication non-compliance. There were no ICD generator malfunctions. There were 2 lead fractures unrelated to sports (10%), both Fidelis models, without IS or life threatening events. There was one non-cardiac death unrelated to sports and one cardiac transplant. Athletes cited quality of life, mental and physical health benefits as reasons for participation.
Conclusion
Complications and shocks in our young athletes with ICDs were low. Patients are choosing to participate and sports can be safe. Future prospective studies and guideline revision should be considered.
OUTCOMES OF BIVENTRICULAR PACING IN PATIENTS WITH TRANSPOSITION OF THE GREAT ARTERIES
Author links open overlay panelAbbie ChristineHagemanJamilAboulhosnLeighReardonPamelaMinerLindaHouserKevinShannonJeremyMooreJeannetteLin
University of California Los Angeles, Los Angeles, CA, USA
Background
As a late outcome of transposition of the great arteries (TGA), systemic right ventricular dysfunction can lead to deterioration of clinical status. Biventricular pacing (BVP) has been suggested as a treatment to reverse ventricular dysfunction in TGA patients, however there is scant data to support this.
Methods
We analyzed 14 TGA patients (11 males, 3 females) who underwent biventricular pacemaker implantation (2 surgically, 12 transvenously) from 2004 to 2013 at an average age of 36.5±6.6 years. We compared New York Heart Association (NYHA) functional class at baseline, acutely (≤1year) and long-term (3-5years) by subgroup. The subgroups included 6 NYHA class ≤II, 8 NYHA Class ≥III, 11 levo-TGA (L-TGA), and 3 dextro-TGA (D-TGA) patients.
Results
NYHA class improved significantly for all subgroups within one year, except for the NYHA class ≤II group. Patients NYHA Class ≥III had significant improvement in NYHA class long-term. Of the 8 patients NYHA Class ≥III, 4 had improvement to NYHA class I, 2 to class II and 2 with no improvement. One patient died and two patients had heart transplants 5-6 years after BVP, all three patients had D-TGA.
Conclusion
NYHA class significantly improved within one year in all subgroups and long-term in patients NYHA Class ≥III. BVP can improve the quality of life and activity limitation in patients with TGA. Prospective evaluation with a larger sample size should be considered to verify these findings.
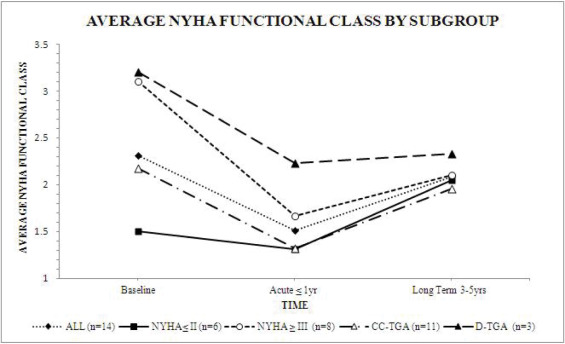
SALT WITH LOW-DOSE FUROSEMIDE DECREASES PLASMA ALDOSTERONE LEVEL IN ACUTE DECOMPENSATED HEART FAILURE
Author links open overlay panelYoshitakaOkuharaShinichiHirotaniToshihiroIwasakuAkiyoEguchiDaisukeMorisawaTomotakaAndoHisashiSawadaKouichiNishimuraYoshiroNaitoTohruMasuyama
Cardiovascular Division, Department of Internal Medicine, Hyogo College of Medicine, Nishinomiya, Japan
Background
Recent reports have provided findings that severe salt restriction may be harmful in acute decompensated heart failure (ADHF). We have reported that salt supplementation enhances diuretic effects in ADHF, which could avoid administration of high doses of diuretics. The aim of this study is to investigate effects of salt supplementation and low-dose furosemide on changes of neurohumoral factors and urinary volume in treatment of ADHF.
Methods
Forty four patients were randomly administered either continuous intravenous infusion of 500 mL of 1.7% NaCl supplemented with 40 mg/day of furosemide (salt infusion group) or continuous intravenous infusion of 500 mL of 5% glucose supplemented with furosemide 40 mg/day (glucose infusion group). Venous blood samples were collected to measure plasma electrolytes, plasma renin activity, plasma aldosterone, plasma norepinephrine, plasma anti-diuretic hormone and NT-proBNP at baseline and 24 hours after initiation of the treatment. The total 24 hours urinary volume was measured and urinalysis was performed.
Results
Urinary volume was greater in the salt infusion group than in the glucose infusion group [salt infusion: 2701 ± 920mL; glucose infusion: 1777 ± 797mL, p<0.001]. Creatinine clearance rate was significantly greater in the salt infusion group than in the glucose infusion group [salt infusion: 63.5 ± 52.6mL/min/1.73m2; glucose infusion: 39.0 ± 26.3mL/min/1.73m2; p=0.048]. We assessed respective variation of neurohumoral factors (Δ = 24 hours after initiation of the treatment – baseline). Only Δplasma aldosterone was greater in the salt infusion group than in the glucose infusion group [salt infusion: −36.9 ± 42.0pg/mL; glucose infusion: −14.0 ± 32.4pg/mL, p=0.05]. Although urinary volume was greater in the salt infusion group than in the glucose infusion group, ΔSerum K level, urine K/Na ratio and TTKG did not differ significantly in both groups.
Conclusion
These results suggest that favorable diuresis in salt and low-dose furosemide combination therapy is mediated by inhibition of plasma aldosterone. This may ultimately results in improvement of prognosis of heart failure.
DIURETICS WITHIN 24 HOURS OF DISCHARGE
Author links open overlay panelJosephIngrassiaEvanMarinoPoojitaShivamurthyWilliamPeruckiRichardSoucier
St. Francis Hospital and Medical Center, Hartford, CT, USA
University of Connecticut Health Center, Farmington, CT, USA
Background
Intravenous loop diuretics (IVLD) are the most commonly used medication for hospitalized congestive heart failure (CHF) patients; however, many questions remain regarding their best use. Our objective was to determine if there was any difference in the 30 day readmission rates between patients admitted with CHF that received IVLD within 24 hours of discharge and those who were transitioned to stable oral dosing (SOD) at least 24 hours prior to discharge.
Methods
We performed a retrospective chart review on all patients admitted to our CHF unit from 9/1/2009 to 1/13/2013 using our existing Get With the Guidelines® database and our electronic medical record to determine the timing of the patient’s last IVLD dose.
Results
The mean age, sex, and ejection fraction was evenly distributed between groups. Patients with renal dysfunction were more likely to be on SOD for at least 24 hours prior to discharge and mean length of stay was shorter in the group that did not receive this transition. There was no difference in readmission rates when comparing patients on SOD for at least 24 hours (Group 1) vs. those that were transitioned to oral diuretics on the day of discharge (Group 2).
Conclusions
We did not find any difference in the 30 day readmission rate between those receiving IVLD within 24 hours of discharge and those on SOD. Further study is needed to identify which populations can safely be discharged with late transition to oral diuretics and whether different post discharge strategies will impact outcomes
| Group 1 n = 1575 | Group 2 n = 604 | p | |
| Age | 74.4 | 73.4 | 0.17 |
| Male Gender | 820 (52%) | 308 (51%) | 0.67 |
| LVEF<40% | 682 (43%) | 262 (43%) | 0.95 |
| Mean Ejection Fraction (%)mg/dL) | 40.8 | 40.4 | 0.73 |
| Ischemic CHF | 852 (54%) | 324 (54%) | 0.85 |
| Chronic Kidney Disease (Baseline Serum Creatinine ≥2 mg/dL) | 197 (13%) | 34 (6%) | 0.00002 |
| Mortality Risk Score at Discharge (%) | 3.76 | 3.41 | 0.07 |
| Length of Stay (days) | 8.86 | 6.92 | 0.00009 |
| 30d readmission rate | 357 (23%) | 120 (20%) | 0.16 |
IMPACTS OF ANTI-DIURETIC HORMONE BY SALT SUPPLEMENTATION IN ACUTE DECOMPENSATED HEART FAILURE
Author links open overlay panelYoshitakaOkuharaShinichiHirotaniToshihiroIwasakuDaisukeMorisawaAkiyoEguchiTomotakaAndoMakikoOboshiHisashiSawadaYoshiroNaitoTohruMasuyama
Cardiovascular Division, Department of Internal Medicine, Hyogo College of Medicine, Nishinomiya, Japan
Background
Recent reports have provided findings that severe salt restriction may be harmful in acute decompensated heart failure (ADHF). We have reported that salt supplementation enhances diuretic effects in ADHF. Salt administration generally increases a plasma anti-diuretichormone (ADH) level. It induces fluid retention. The aim of this study is to study the relation of urinary volume and ADH by salt supplementation in treatment of ADHF.
Methods
Forty four patients with ADHF were randomly administered either continuous intravenous infusion of 500 mL of 1.7% NaCl supplemented with 40 mg/day of furosemide (salt infusion group) or continuous intravenous infusion of 500 mL of 5% glucose supplemented with furosemide 40 mg/day (glucose infusion group). We investigated about plasma ADH at baseline and 24 h after initiation of the treatment. Urinalysis was performed by 24-h urinary collection.
Results
Urinary volume was greater in the salt infusion group than in the glucose infusion group [2701 ± 920mL vs. 1777 ± 797mL, p<0.001]. Although plasma ADH level did not differ significantly in both groups, the salt infusion group shows a clear positive correlation between change of ADH level and free water clearance [r=0.68, p=0.001]. Urinary volume was positively correlated with osmotic clearance by salt supplementation [r=0.75, p<0.001].
Conclusion
These results suggest that salt supplementation induces favorable diuresis independent of ADH in ADHF.
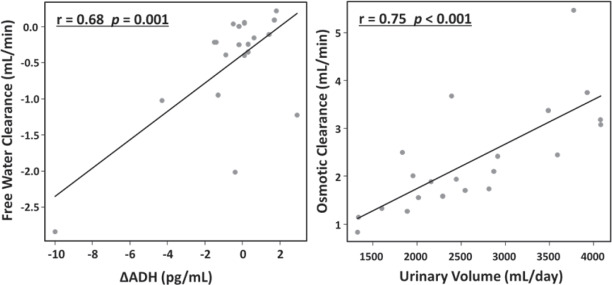
LOW-DOSE TOLVAPTAN AS FUROSEMIDE ALTERNATIVE PRESERVES RENAL FUNCTION AND RENIN-ANGIOTENSIN SYSTEM DURING INTENSIVE TREATMENT IN PATIENTS WITH CONGESTIVE HEART FAILURE
Author links open overlay panelKentaroJujoAhsungKimIsseiIshidaYukiSuzukiKatsumiSaito
Nishiarai Heart Center Hospital, Tokyo, Japan
Background
Although loop diuretics are broadly used for congestive heart failure (HF), there frequently appear serious adverse effects such as worsening of renal function and activations of the sympathetic and renin-angiotensin system via arterial underfilling. On the other hand, the effects of sodium channel independent diuretic Tolvaptan on those complications in acute phase of HF patients are still unclear.
Methods and Results
Forty consecutive patients hospitalized due to worsening of congestive HF were randomly assigned to receive either daily 40 mg of intravenous furosemide or 7.5 mg of oral Tolvaptan, in addition to intravenous 0.025g of carperitide and 200 mg of canrenoate potassium. Renal functions and neurohumoral factors were evaluated for 5 days after the admission. As results, patient characteristics were similar between Furosemide (n=21) and Tolvaptan group (n=19). Total of 5-day urine volume or fluid balance was not significantly different (10169 vs. 9807 mL, −4627 vs. −3549 mL, respectively), and similar degrees of improvement in BNP were achieved in both groups (-155±485 vs. −284±535 pg/mL). However, the value of serum creatinine (Cr) significantly deteriorated in Furosemide group (25±58 vs. −5.4±16%, p=0.033), and preservation of renal function occurred more frequently in Tolvaptan group (9.5 vs. 44%, p=0.018). Consequently, increase of Cr to earn 1000 mL of urine was 3-fold higher in Furosemide group (0.046±0.070 vs. 0.016±0.030 mg/dL/1000mL, p=0.086). On the contrary, increase in the ratio of BUN/Cr was significantly higher in Furosemide group (2.7±8.1 vs. −5.7±14, p=0.023), suggesting arterial underfilling via forced dehydration. In terms of neurohumoral factors, although decreases of catecholamines were not significantly different (adrenaline: 49±95 vs. 55±82, noradrenaline: 41±60 vs. 74±19, dopamine: 3.6±257 vs. 55±71%), the value of plasma renin activity was enhanced only in Furosemide group (200±365 vs. 16±92%, p=0.040).
Conclusion
Low-dose Tolvaptan preserved renal function and renin-angiotensin system during intensive treatment in patients with congestive HF. This novel therapy may release HF patients from adverse effects with furosemide.
UDENAFIL IMPROVES EXERCISE CAPACITY AND LEFT VENTRICULAR REMODELING IN PATIENTS WITH SYSTOLIC HEART FAILURE
Author links open overlay panelKyung-HeeKimHyung-KwanKimJinsikParkYong-JinKimDae WonSohn
Sejong General Hospital, Bucheon, South Korea
Seoul National University Hospital, Seoul, South Korea
Background
Over the last few years, the use of phosphodiesterase type 5 (PDE5) inhibitors has been expanded to management of various cardiovascular disorders. We investigated the ability of udenafil, a newly developed long-acting PDE5 inhibitor, to improve functional capacity and hemodynamic status in a cohort of systolic heart failure (SHF) patients.
Methods and Results
Stable, chronic SHF patients were randomly assigned to placebo (20 patients) or udenafil at a dose of 50 mg twice per day (21 patients) for the first 4 weeks followed by 100 mg twice daily for the next 8 weeks. Patients underwent cardiopulmonary exercise testing before and after treatment. The change in peak VO2 from baseline, the primary end point, was greater in the udenafil group (3.47±1.07 mL x kg(-1) x min(-1)) than in the placebo group (-0.36±0.56 mL x kg(-1) x min(-1); P=0.01). Udenafil treatment also was associated with left ventricular(LV) remodeling. LV volume was smaller in the udenafil group compared with the placebo group (baseline LV end-systolic volume, 148ml for udenafil versus 145ml for placebo group; P= NS.; 3month later LV end-systolic volume, 110ml for udenal versus 132ml for placebo, respectively; P< 0.05). LV ejection fraction was greater in the udenafil group than in the placebo group (36% for udenafil versus 31% for placebo, P< 0.05) without mean arterial pressure, heart rate, or systemic vascular resistance. Udenafil treatment also was associated with improvement in 6-minute walk distance (33 m versus placebo; P=0.04) and Minnesota Living With Heart Failure score (-10 versus placebo; P=0.01). Subjects in the udenafil group experienced fewer hospitalizations for HF and a higher incidence of than those in the placebo group without incurring excess serious adverse events.
Conclusions
Phosphodiesterase 5 inhibition with udenafil improves exercise capacity and quality of life in patients with chronic SHF.
PREDICTORS OF 1-MONTH AND 1-YEAR READMISSION FOR WORSENING OF HEART FAILURE IN AMBULATORY PATIENTS
Author links open overlay panelJesusÁlvarez-GarciaAndreuFerreroTeresaPuigRafaelVazquezJuanDelgadoDomingo PascualFigalLuisAlonso-PulponJose Ramon GonzalezJuanateyMiguelRiveraFernandoWornerAlfredo BardajiRuizJuanCinca
Hospital de Sant Pau, Barcelona, Spain
Background
Prevention of hospital readmissions is a main objective in the management of heart failure (HF). Most stratification models are based on data extracted from inpatients, but information based on ambulatory patients is scanty. The aim of this study was to develop a score predicting 1-month and 1-year risk of readmission for worsening of HF.
Methods
A cohort of 2,507 ambulatory HF patients was prospectively followed for a median of 27 months. Clinical, Echo, ECG, and biochemical parameters were used in a multivariable Cox model analysis to develop a risk score for readmissions for worsening of HF. Score was externally validated using the MUSIC cohort study (992 patients).
Results
Predictors of 1-month readmission were: a) elevated NT-proBNP, b) left HF signs, and c) estimated glomerular filtration rate26 mm/m2, d) heart rate>70 beats/minute, e) left HF signs, and f) estimated glomerular filtration rate<60 ml/min/m2. C statistics index for the two models were 0.68 and 0.69. Kaplan-Meier curves distinguished a low-risk (<1% event rate) and a high-risk group (>5% event rate) for 1-month HF readmission risk, and a low-risk (6% event rate), intermediate-risk (17% event rate) and a high-risk group (29% event rate) for 1-year HF readmission risk. The C statistics index remained consistent after the external validation (<5% lost of discrimination).
Conclusions
Early and late readmission for worsening of HF can be predicted using variables that are routinely collected in outpatient management of chronic HF.
CHARACTERISTICS, TREATMENTS, AND OUTCOMES OF HOSPITALIZED HEART FAILURE PATIENTS STRATIFIED BY ETIOLOGIES OF NON-ISCHEMIC CARDIOMYOPATHY
Author links open overlay panelSupriyaShoreMariaGrau-SepulvedaDeepakBhattPaulHeidenreichZubinEapenAdrianHernandezClydeYancyGreggFonarow
University of Colorado, Aurora, CO, USA
University of California Los Angeles, Los Angeles, CA, USA
Background
Whether characteristics, treatment and short-term outcomes of hospitalized heart failure (HF) patients differ by specific etiology of non-ischemic cardiomyopathy (NICM) has not been studied.
Methods
From a cohort of 219,953 patients hospitalized with HF at 319 US hospitals participating in Get With The Guidelines-HF between January 2005 and April 2013, we analyzed data on 58,058 NICM. Characteristics, treatment and outcomes were assessed by NICM etiology.
Results
Hypertensive heart disease (n=28,141; 48.5%) and idiopathic etiology (n=17,808; 30.7%) accounted for the vast majority of patients with NICM. Postpartum, viral, chemotherapy, substance abuse, familial and other etiologies were far less frequent. Baseline characteristics differed significantly by etiology, though were similar for hypertensive and idiopathic patients (Table). Quality of care provided to eligible patients was highest for postpartum and lowest for idiopathic but, was not significant after risk-adjustment. Furthermore, after risk-adjustment mortality was similar by etiology except for hypertensive etiology which was associated with lower in-hospital mortality (OR 0.83, 95% CI 0.71-0.97).
Conclusions
Characteristics of hospitalized HF patients with NICM vary substantially by etiology. Nonetheless, risk-adjusted quality of care provided did not differ by etiology and risk-adjusted in-hospital mortality was similar except for hypertensive etiology being associated with lower mortality risk.
HOSPITAL FOLLOW-UP FOR HEART FAILURE IN AN INTEGRATED HEALTHCARE DELIVERY SYSTEM
Author links open overlay panelAli R.RahimiElizabethNeeleySherryBowenCarlaLetoBinweiSong
Kaiser Permanente Georgia, Atlanta, GA, USA
The Southeast Permanente Medical Group, Atlanta, GA, USA
Background
Timely outpatient follow-up after heart failure (HF) hospitalization has been identified as an essential element in coordinated care delivery. Due to this and efforts to reduce readmission rates, hospitals and physician practice groups have developed performance improvement (PI) initiatives around post-discharge follow-up. We sought to determine the improvement in follow-up after HF hospitalization when such an initiative was promoted in an integrated healthcare delivery system, Kaiser Permanente (KP) of Georgia.
Methods
A KP HF discharge planner was used at core contracted hospitals, staffed by KP physicians, case managers and clinical pharmacists. An outpatient KP team, including case managers and a clinical pharmacist, monitored the daily inpatient census and assisted in hospital follow-up, patient education, and medication reconciliation. For this analysis, administrative claims data was used to identify HF discharges between September 2009 to August 2010 (pre-initiative, n = 221) and September 2012 to August 2013 (post-initiative, n = 273). Patient demographic data were obtained thru electronic medical records. CarePOINT, an internal disease registry system was used to identify the patient’s medical history. Hospital follow-up, within 7 days and 14 days, was determined by examining days between a HF discharge date and the date in which an office visit to primary care, cardiology, or nephrology was scheduled or completed.
Results
In comparing the two time periods, pre- and post- HF PI initiative, there was a significant increase in the within 7 day (47.5% vs. 78.4%; p < 0.001) and 14 day (70.2% vs. 94.3%; p < 0.001) scheduled follow-up appointment rate. Similarly, there was a significant increase in the within 7 day (33.5% vs. 60.8%; p < 0.001) and 14 day (51.4% vs. 80.6%; p <0.001) completed follow-up appointment rate.
Conclusion
Following implementation of a coordinated HF PI initiative, there was significant improvement in the scheduled and completed outpatient HF follow-up rate within 7 and 14 days. The comparative effectiveness of such performance improvement initiatives across different models of healthcare delivery are unknown and is an area for further research.
IMPACT OF A MULTI-DISCIPLINARY HEART FAILURE POST-DISCHARGE MANAGEMENT CLINIC ON MEDICATION ADHERENCE
Author links open overlay panelLingyunLuCynthiaJackeviciusNoellede LeonAlbertaWarnerDonaldChangFrenyMody
VA Greater Los Angeles HealthCare System, Los Angeles, CA, USA
Western University of Health Sciences, Pomona, CA, USA
Background
Specialized clinics have been associated with improved medication adherence to evidence-based heart failure (HF) therapies. We evaluated a structured multi-disciplinary HF clinic focused specifically on those recently discharged after a HF hospitalization. In addition to reducing readmissions, one of the clinic’s goals was to improve medication adherence, which is critical to obtaining benefit from prescribed guideline therapies.
Methods
In this retrospective cohort study, patients discharged with a primary HF diagnosis who attended the HF post-discharge clinic in 2010-12 were compared with historical controls from 2009. Within an average of 6 clinic visits, patients were seen by a physician assistant, a clinical pharmacist and a nurse educator, with care overseen by an attending cardiologist. The main outcome was adherence to evidence-based HF therapies within 90 days of discharge, assessed by proportion of days covered (PDC-90), which was defined as the ratio of total days’ supply of medication divided by total days prescribed, within 90 days of discharge and proportion of patients with PDC-90≥0.80.
Results
Among 277 patients (144 clinic/133 control), 11 patients were excluded due to lack of medication record. There was no difference between groups in HF medication prescribing within 90 days post-discharge, except for angiotensin-receptor blockers (11.2% vs 21.5%, p=0.01). Both univariate and multivariate analysis showed the clinic improved medication adherence, with the most significant increase in adherence to ACE inhibitors (PDC-90: 0.84 vs 0.93, p=0.008; PDC-90≥0.80: 69% vs 86.5%, p=0.005;) and aldosterone antagonists (AA, PDC-90: 0.72 vs 0.94, p=0.0002; PDC-90≥0.80: 45.8% vs 84.6%, p=0.001). Adherence to beta-blockers (BB) trended towards the clinic group (PDC-90: 0.85 vs 0.92, p=0.02; PDC-90≥0.80: 72.8% vs 83.1%, p=0.06).
Conclusions
The multidisciplinary HF post-discharge clinic was associated with a significant increase in 90-day adherence to ACE inhibitors and AA, with a trend towards increased adherence to BB. Improved medication adherence is critical to obtaining benefit of reduced readmission and mortality from evidence-based HF therapy.
ATRIAL FIBRILLATION AS AN INDEPENDENT PREDICTOR OF HEART FAILURE READMISSIONS: ANALYSIS OF “GET-WITH-THE-GUIDELINES” HEART FAILURE
Author links open overlay panelNayan K.DesaiMaryannPowellJadSkafKrystalHunterJohnAndriulliMatthewOrtmanLawrenceGessmanAndreaRusso
Cooper University Hospital, Camden, NJ, USA
Background
Atrial fibrillation (AF) and heart failure (HF) frequently coexist in hospitalized patients (pts). The impact of AF on re-hospitalization for HF is not well studied. We investigated the potential impact of AF and 30-day readmissions in pts admitted with HF.
Methods
We studied 3,758 pts admitted with HF at our institution from 2007 to 2012 using data collected in the AHA Get-With-the-Guidelines registry. Patients who were re-admitted within 30 days for all causes were compared to those who were not re-admitted. Multivariate logistic regression analysis was utilized.
Results
780/3758 (21%) pts were readmitted within 30 days. Characteristics of pts who were readmitted were compared to those who were not readmitted (Table). The presence of AF, diabetes, devices, noncompliance, ischemic heart disease at admission were independent predictors for 30-day readmission. Pts with AF had a 1.39 times greater odds of readmission than those without AF.
Conclusion
The presence of AF particularly pre-existing AF on admission, in HF pts is an independent predictor of 30-day readmission. Whether primary arrhythmia therapy aimed at rate control or restoration and maintenance of sinus rhythm would reduce HF readmissions warrants additional investigation.
Characteristics of pts who were readmitted were compared to those who were not readmitted
| Readmission (n= 780) | No readmission (n=2978) | p value | |
| Age (yrs) | 68.8 | 67.7 | 0.058 |
| Male | 430 (55%) | 1678 (56%) | 0.56 |
| Race | |||
| -Caucasians | 486 (62%) | 2018 (67%) | |
| -Africo-Americans | 286 (37%) | 930 (31%) | |
| -Others | 8 (1%) | 31 (1%) | 0.014 |
| Payment source – Medicare | 515 (66%) | 1798 (60%) | 0.003 |
| Diabetes | 480 (62%) | 1234 (41%) | <0.001 |
| Chronic Dialysis | 60 (8%) | 121 (4%) | <0.001 |
| AF on index admission | 432 (55%) | 1118 (37%) | <0.001 |
| -Pre-existing AF | 395 (51%) | 998 (34%) | <0.001 |
| -New onset AF | 37 (5%) | 119 (4%) | 0.35 |
| Reason for index admission | |||
| -Noncompliance(Medication/Diet) | 535 (68%) | 1689 (55%) | <0.001 |
| -Arrhythmias | 515 (66%) | 1333 (44%) | <0.001 |
| -Weight gain | 512 (65%) | 1316 (44%) | <0.001 |
| -Uncontrolled Hypertension | 342 (44%) | 957 (32%) | <0.001 |
| Mean Heart rate on admission (bpm) | 116 | 112 | 0.01 |
| Devices (CRT±ICD) | 280 (36%) | 504 (17%) | <0.001 |
| EF > 40% | 325 (42%) | 1212 (41%) | 0.80 |
| Non-ischemic Heart disease | 380 (49%) | 1515 (51%) | 0.83 |
| Ischemic heart disease | 529 (69%) | 1448 (51%) | <0.001 |
| In-patient Death | 80 (10%) | 123 (4%) | <0.001 |
USE OF ACOUSTIC CARDIOGRAPHY TO GUIDE OUTPATIENT THERAPY OF PATIENTS WITH ACUTE HEART FAILURE SYNDROME
Author links open overlay panelShih-HsienSungWen-ChungYuHao-MinChengYu-PingChangChen-HuanChen
Taipei Veterans General Hospital, Taipei, Taiwan, ROC
Background
The electromechanical activation time normalized by cardiac cycle length (%EMAT) measured with an automated acoustic cardiography is useful in the prediction of post-discharge cardiovascular outcomes in patients with acute heart failure syndrome (AHFS). The aim of this study was to evaluate whether the %EMAT guided post-discharge management improves outcomes in patients with AHFS when compared with conventional therapy.
Methods
This prospective single-blind study randomized 194 AHFS subjects (aged 75.4±14.7 years, LVEF 37.5±16.9%, and NTproBNP 14168.5±21019.8) before discharge to the %EMAT-guided group (n = 102) with the goal to reduce %EMAT to <15%, and the symptom-guided group (n = 92) without the knowledge of %EMAT. The primary endpoints were re-hospitalization for HF and CV mortality during 1-year follow-up.
Results
The two groups were well-matched. Through a mean follow-up period of 173±142 days, a significant reduction in the primary endpoints was seen in the %EMAT-guided group compared with the symptom-guided group (27 events vs. 39 events, P = 0.02). Kaplan-Meier curves showed significant differences in time to first event, favoring the %EMAT-guided group in the total study population (P = 0.03, Fig A), as well as in the pre-specified subgroup of patients with a pre-discharge %EMAT of >15% (n =79, P=0.04, Fig B).
Conclusions
In patients with AHFS, %EMAT-guided management was superior to the conventional therapy with significantly improved clinical outcomes. (NCT01298232).
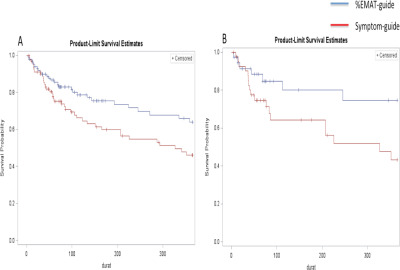
INFERIOR VENA CAVA MEASUREMENT BY FOCUSED CARDIAC ULTRASOUND IN ACUTE DECOMPENSATED HEART FAILURE PREVENTS HOSPITAL READMISSIONS
Author links open overlay panelLuke J.LaffinAmitPatelNarayanSahaJulianBarbatJames K.HallMatthewCainKishanParikhJayShahKirkSpencer
University of Chicago, Chicago, IL, USA
Background
Previous work demonstrates that patients discharged from the hospital after admission for acute decompensated heart failure (ADHF) are more likely to be readmitted if they leave with an inferior vena cava (IVC) that is plethoric. We propose that IVC diameter and collapsibility, as measured by Focused Cardiac Ultrasound, can help guide inpatient management of ADHF and prevent hospital readmission.
Methods
Patients presenting with ADHF to a single tertiary academic medical center between February and October 2013 were enrolled. Exclusion criteria included the need for hemodialysis or admission to an intensive care unit. IVC diameter and collapsibility were measured upon admission, the following 4 days, and the day of discharge. Measurements were performed by housestaff trained in ultrasound IVC measurement who were blinded to all clinical data. Clinicians on 1 of the 4 cardiology services (intervention group) were provided IVC data, to integrate into their clinical care plan. Patients were contacted by telephone to determine if hospital readmission or emergency department visits occurred in the 30 days following discharge.
Results
61 patients were enrolled. The 30-day hospital readmission rate was decreased in the intervention group (4% vs 30%, p=0.03.) The combined rate of emergency room visits and hospital readmission was also decreased (8% vs 43%, p=0.01.) Both intervention and control groups had the same average length of stay (5 days). The intervention group demonstrated a trend toward a greater percentage of body weight lost (10% vs. 4%, p=0.07) and no deterioration in renal function during the hospitalization. Control group patients seen in the emergency department, or readmitted, had a smaller absolute change in IVC size during their admission (-0.21 vs −0.56 cm, p=0.04,) when compared to controls who were not readmitted or seen in emergency department.
Conclusions
The use of IVC diameter and collapsibility, as measured by Focused Cardiac Ultrasound, is associated with decreased readmission rates in patients with ADHF. Use of bedside assessment of the IVC with a focused cardiac ultrasound exam is an effective tool to guide management and prevent hospital readmissions.
PROGNOSTIC IMPLICATION OF LEFT VENTRICULAR FUNCTION AMONG PATIENTS WITH ACUTE KIDNEY INJURY AND ACUTE DECOMPENSATED HEART FAILURE
Author links open overlay panelSabryOmarElsayedAbo-SalemSian YikLimJasonWischmeyerSharmaPrabhakar
Texas Tech University Health Science Center, Lubbock, TX, USA
Background
Acute kidney injury (AKI) is a common complication among patients with acute heart failure(AHF) (30%) and is associated with increased in-hospital mortality and readmission. Limited data are available about the impact of left ventricular systolic function on the prognosis of these patients.
Methods
Medical records of patients who were admitted with AHF and AKI between 2008 and 2010 were reviewed. The patients were divided into two groups: AHF with reduced ejection fraction (HFrEF; left ventricular ejection fraction (LVEF) ≤ 45%), and AHF with preserved ejection fraction (HFpEF; LVEF > 45%). AKI was defined as a rise of serum creatinine > 0.3 mg/dL above the baseline.
Results
We studied 244 patients with AHF and AKI (121 male and 123 female) with a mean age of 64.12 ± 16.4. The in-hospital mortality, 30-days readmission and requirement for dialysis were significantly higher in the HFrEF compared to HFpEF (Table 1). In the multivariate logistic regression model, the only independent predictors of mortality were the use of beta blockers (Odds ratio: 0.27, 95% confidence interval(CI): 0.88 to 0.84, P = 0.02) and angiotensin converting enzyme (ACE) inhibitors (Odds ratio: 0.272, 95% CI: 0.07 to 0.96, P = 0.04).
| HfrEF | HfpEF | P value | |
| Total number | 135 | 109 | |
| Baseline characteristics | |||
| Age | 60.94 ± 17.7 | 68.02 ± 13.7 | 0.0001 |
| LV ejection fraction % (median) | 25 | 59 | 0.0001 |
| Estimated GFR mg/dL (mean) | 57.51 ± 21.7 | 56.18 ± 24.8 | 0.658 |
| DM (%) | 65.92 | 77.98 | 0.054 |
| HTN (%) | 57.78 | 84.40 | 0.001 |
| B-blockers (%) | 55.6 | 63 | 0.027 |
| ACEI (%) | 48 | 64 | 0.046 |
| Outcome | |||
| In-hospital mortality (%) | 11.1 | 4 | 0.023 |
| Days in hospital (median) | 9.4 | 7.8 | 0.016 |
| Readmission within 3 months (%) | 66.4 | 44.1 | 0.0001 |
| Dialysis requirement (%) | 8.9 | 2.8 | 0.04 |
Conclusions
Among cases with AKI and AHF, the mortality, readmission rates and requirement of dialysis were significantly higher in those with HFrEF than HFpEF. The use of beta blockers and ACE inhibitors were independent predictors of reduced mortality in both groups.
BLOOD-PRESSURE REDUCTION IS ASSOCIATED WITH WORSENING IN RENAL FUNCTION BUT DOES NOT PREVENT SUCCESSFUL DECONGESTION IN PATIENTS TREATED FOR ACUTE DECOMPENSATED HEART FAILURE
Author links open overlay panelAlexanderKulaOlgaLaurSusanChengMeredithBriscoBrianMcCauleyStevenCocaJeffreyTestani
Yale University School of Medicine, New Haven, CT, USA
Background
Recent data have demonstrated that substantial reductions in blood pressure are common during the treatment of acute decompensated heart failure (ADHF) and are associated with worsening renal function (WRF). However, since the kidney serves as the primary conduit by which fluid and sodium is removed, it is possible that the reduction in blood pressure secondary to factors such as routine titration of vasodilators and neurohormonal antagonistsduring the treatment of ADHF could limit successful decongestion. Our aim was to investigate whether a decline in systolic blood pressure (SBP), and the associated deterioration in renal function, might limit successful diuresis.
Methods
We analyzed consecutive admissions with a primary discharge diagnosis of HF at a single center (n=657) and determined the change in SBP from the admission to discharge. WRF was defined as a ≥20% reduction in estimated glomerular filtration rate (eGFR).
Results
Overall 77.5% of the population had a discharge SBP lower than the admission value. Reduction in SBP and deterioration in eGFR were significantly correlated (r=0.27, p<0.0001), and in patients with a relative reduction in SBP above the median (9.9% relative reduction in SBP), WRF was significantly more common (OR= 1.9, p=0.004). Despite the negative association with renal function, SBP reduction was not associated with a lower total fluid output (p=0.293), average daily fluid output (p=0.306), or longer length of stay (p=0.249). There was no correlation between change in blood pressure and net fluid loss (r=0.01, p=0.77) or % change in eGFR and fluid loss (r=0.03, p=0.39). The similar diuresis achieved between groups was not at the expense of higher doses of loop diuretics (p=0.77), use of loop diuretic infusions (p=0.86), or the use of adjuvant thiazide diuretics (p=0.73). Furthermore, the rate of hemoconcentration was not different between patients with a SBP reduction above or below the median (p=0.238). Even amongst those who developed WRF in the context of a SBP reduction, fluid output was similar (p=0.174).
Conclusion
Despite apparent negative effects on renal function, a reduction in blood pressure did not appear to limit successful decongestion.
SARCOPENIA IS ASSOCIATED WITH THE SEVERITY OF HEART FAILURE IN PATIENTS WITH ACUTE DECOMPENSATED HEART FAILURE
Author links open overlay panelEiichiAkiyamaMasaakiKonishiYasushiMatsuzawaMitsuakiEndoHiroyukiSuzukiNaokiNakayamaNobuhikoMaejimaNoriakiIwahashiKengoTsukaharaYoshioTaharaKiyoshiHibiToshiakiEbinaSatoshiUmemuraKazuoKimura
Yokohama City University Medical Center, Yokohama, Japan
Background
Heart failure (HF) is a clinical syndrome associated with diverse metabolic disturbances. Recent studies suggest that failing heart trough secretion of soluble myostatin may induce skeletal muscle wasting in HF patients and skeletal muscle plays an important role in pathogenesis of exercise intolerance in patients with chronic HF. The prevalence of sarcopenia is reported as 5-13% in general 60-70year-olds and as about 20% in patients with chronic HF, however, the prevalence and clinical significance of sarcopenia in patients with acute decompensated HF (ADHF) remain unclear. We investigated the association between sarcopenia and ADHF.
Methods
We assessed lean body mass by dual energy X-ray absorptiometry in 52 patients with ADHF(age 71±10, left ventricular ejection fraction (LVEF) 38±16%, B-type natriuretic peptide(BNP) levels on admission 540 [275-1161] pg/ml). Sarcopenia was defined as the appendicular skeletal muscle mass index (appendicular skeletal muscle mass/height2) 2 standard deviations below the mean of young healthy Japanese subjects (<6.87 kg/m2 in male, <5.46 kg/m2 in female).
Results
Appendicular skeletal muscle mass index significantly correlated with age, (r=−0.27, P=0.04), male sex (r=0.43, P=0.002), body mass index (r=0.50, P<0.001), heart rate (r=−0.31, P=0.02), and BNP levels (r=−0.27, P=0.04). The prevalence of sarcopenia was 54%. ADHF patients with sarcopenia had more severe HF symptoms (New York Heart Association class- 2.8±0.6 versus 2.5±0.5, p=0.03), higher BNP levels (656 [372-1326] versus 353 [234-813], p=0.009), and higher rate of clinical scenario 2-3 (43% versus 13%, p=0.02) than those without sarcopenia. Multivariate logistic regression analysis demonstrated that sarcopenia (odds ratio (OR): 5.5, 95%-confidence interval (CI): 1.1-28.6, P=0.04), LVEF (OR: 0.95, 95%-CI: 0.90-0.99, P=0.03), and hemoglobin level (OR: 0.66, 95%-CI: 0.44-0.99, P=0.04) independently correlated with higher BNP levels (>400pg/ml) in ADHF patients.
Conclusions
Sarcopenia is frequently observed in ADHF patients and is associated with severity of HF in ADHF, irrespective of LV systolic function and other clinical profile.
LEFT VENTRICULAR ASSIST DEVICE THERAPY IN PATIENTS WITH ADULT CONGENITAL HEART DISEASE
Author links open overlay panelMelissaLyleRichardDalyAvishayGrupperSarahSchettleJohnStulakLyleJoyceSoonParkSudhirKushwaha
Mayo Clinic, Rochester, MN, USA
Background
As a result of advancements in surgical repair and treatment, there are an increasing number of patients with congenital heart disease surviving into adulthood. Continuous flow left ventricular assist devices (LVAD) have been infrequently used in those patients that develop end stage heart failure, and thus there is limited clinical experience with the use of LVAD support in congenital heart disease patients.
Methods
We performed a retrospective chart review of all adult patients who received LVAD support from May 2008 until August 2013 at Mayo Clinic Rochester. The records were analyzed for relevant clinical data before and after LVAD implantation.
Results
4 adult male patients with end-stage congenital heart disease underwent LVAD implantation. The average age at implant was 46 (31,60). 3 patients underwent at least one prior heart surgery during childhood. All 4 patients required either inotropic or intra-aortic balloon pumpsupport prior to LVAD surgery. Patient 1 underwent LVAD implant as BTT for congenitally corrected transposition of the great vessels, and remains alive 9 months post LVAD implantation without any major post-operative complication. Patient 2 underwent LVAD implant as BTT for dilated cardiomyopathy in the setting of dextrocardia, and expired 7 days post-implantation due to cardiac tamponade. Patient 3 underwent LVAD transplant as DT for tricuspid atresia, but expired 9 days post-implantation due to hypoxia and bleeding, after requiring ECMO and dialysis support. Patient 4 underwent LVAD implant as DT for ventricular septal defect with double outlet right ventricle, with major post-operative complications including dialysis for acute renal failure. He is alive and functional 3 years and five months post-implantation.
Conclusion
LVAD therapy in adult patients with complex congenital heart disease may be challenging, and the outcome is difficult to predict due to the unique anatomic and physiologic abnormalities. As more patients with congenital heart disease survive into adulthood and develop heart failure, LVAD therapy may be appropriate therapy, with better patient selection based on defined protocols to improve morbidity and mortality.
SURVIVAL IN ADULTS UNDERGOING PRIMARY HEART TRANSPLANT AFTER FONTAN PALLIATION
Author links open overlay panelLeigh C.ReardonEugeneDePasqualeDanielCruzHillelLaksBrianReemtsenReshmaBiniwaleGwendolynDerkAbbieHagemanMarioDengJamilAboulhosn
UCLA, Los Angeles, CA, USA
Background
Survival in pediatric and adult patients with failing Fontan physiology undergoing orthotropic heart transplantation (OHT) has been reported to be 77% at one year and 70% at five years (Lamour 2009). There is a paucity of data on the outcomes of adult failing Fontan patients who undergo OHT. We reviewed the results of adult failing Fontan patients undergoing OHT at UCLA Medical Center over the past decade.
Demographics
Thirteen patients were identified of 744 OHT recipients. The ages ranged from 19-44 years with an average age of 30.4 years. Five patients were male. The age at the time of the Fontan palliation ranged from 3 to 22 (mean 10.1 years). Eight patients had a classic RA-PA Fontan, three patients had undergone previous Fontan conversion from RA-PA to lateral tunnel. Two patients had heterotaxy syndrome and one patient underwent concomitant OHT and liver transplant.
Results
Thirteen patients were transplanted between 2002 and 2013; two of which were transplanted in 2013. Survival at 90 days (n=13) and one year (n=11) was 100%, survival at three years (n= 6) was 83%, and survival at five years (n=5) was 80%. The single mortality occurred at 33 months after OHT from coronary artery vasculopathy.
Conclusions
In this single center cohort, adult patients with failing Fontan physiology undergoing OHT have similar short, intermediate, and long-term survival compared to non-congenital adult patients at our center. These encouraging results in a contemporary cohort of adults are in contrast to prior published reports of poor outcomes following OHT in failing Fontan patients.
REDUCED HEPATIC VENOUS FLOW IS A MARKER OF ADVERSE OUTCOMES IN PATIENTS WITH FONTAN CIRCULATION
Author links open overlay panelMakotoMoriMaanJokhadarKayokoShiodaAnuragSahuRobertElderCamdenHebsonNancyMcCabeBrianKogonWendyBook
Emory University School of Medicine, Division of Cardiology, Atlanta, GA, USA
Background
Liver injury and portal hypertension are significant complications of the Fontan circulation and are thought to result from chronic venous hypertension. The flow characteristics of the involved veins, specifically the hepatic vein (HV), are unknown in this population, and their association with clinical outcomes has not been studied. We hypothesize that decreased HV flow is associated with adverse clinical outcomes.
Methods
A retrospective review of 58 adult post-Fontan patients referred for an echocardiographicevaluation from 2001 to 2013 was performed. The Doppler echocardiographic data was used to estimate the HV flow. The relationship between HV flow per cardiac cycle (HV cross-sectional area multiplied by the average velocity time integral per cardiac cycle) and outcome measures, which were features of portal hypertension (VAS score ≥2, 1 point each for Varices, Ascites, or Splenomegaly) or a major adverse event (death or heart transplant) were examined using multivariable logistic regression.
Results
58 post-Fontan patients (79.3% systemic left ventricle, mean age 29.3 ± 8.2 years, mean interval from Fontan 22.4 ± 4.8 years) were included in analysis. The mean hepatic venous flow per cardiac cycle was 12.1 ± 10.9ml, mean HV diameter was 1.2 ± 0.4cm, and the mean anterograde-retrograde HV flow ratio was 2.9 ± 2.3. Features of portal hypertension(VAS score ≥ 2) were present in 14 (24.1%), and there were 16 (27.6%) major adverse events: death (n = 11) and transplant (n = 8). After adjusting for time since Fontan operation and age, a significant relationship was found between HV flow per cardiac cycle and both major adverse events and features of portal hypertension: the estimated odds ratio for VAS score ≥ 2 comparing 25th percentile to 50th percentile of HV flow was 2.29 [95% CI 1.06-4.93, p=0.034], and that for death and need for transplant was 2.16 [95% CI 1.00-4.64, p=0.049].
Conclusions
Hepatic venous flow is a novel echocardiographic marker associated with major clinical adverse outcomes in Fontan patients. Future prospective studies are needed to establish the reproducibility and predictability of this novel marker.
LEFT VENTRICULAR DYSFUNCTION HAS AN ADDITIONAL NEGATIVE IMPACT ON CARDIAC OUTCOMES IN ADULTS WITH EBSTEIN’S ANOMALY
Author links open overlay panelYumiShiinaSonyaBabu-NarayanKoichiroNiwaRiikkaRydmanWeiLiTheodorKaronisVasilisPapaioannouOktayTutarelAleksanderKempnyGerhard-PaulDillerPhilipKilnerHidekiUemuraMichaelGatzoulis
Royal Brompton Hospital, London, United Kingdom
St. Luke’s International Hospital, Tokyo, Japan
Background
Non-invasive predictiors of cardiac events in Ebstein’s anomaly are not established.
Methods
105 adults [aged 39.4±15.8 (18-83) years] with unrepaired Ebstein’s anomaly underwent protocolised cardiovascular magnetic resonance (CMR) and echocardiography between January 2004 and December 2011. Cardiac events including death, sustained tachyarrhythmia, congestive cardiac failure, and cardiac transplantation were recorded and patients were censored when they underwent surgical repair.
Results
At latest follow-up (median 3.71 years), 100/105 were in sinus rhythm, 5/105 (0.5%) in persistent atrial fibrillation (AF), 26/105 (24.8%) patients had presented with new episodes of atrial tachyarrhythmia (AT) and 2/105 (1.9%) had sustained ventricular tachycardia (VT). On multivariate Cox proportional hazard analysis, maximum functional RA indexed volume [hazard ratio (HR) 1.01, 95% confidence interval (CI) 1.003-1.02, p=0.005] was an independent risk factor. A composite score including 1 point for each independent predictor (maximum RA indexed volume >100 ml/m2, TR%RF >35%, indexed RVEDV>150ml/m2), was found highly predictive of AT (logrank P=0.002). At latest follow-up, 9/105 patients (8.6%) had fatal cardiac events (cardiac failure, VT, sudden cardiac death). On univariate Cox proportional hazard analysis, oxygen desaturation during exercise, peak VO2 of the predicted value, stroke volume, Maximum functional RA indexed volume, atrialised RV indexed volume, RVEF, LVEF, LV longitudinal global strain (p<0.047) were important predictors of fatal cardiac event. As for left-sided cardiac predictor of cardiac event, 11.5% in LV global strain was a cut off value (sensitivity 77.8%, specificity 82.1%, AUC 0.79 [95%CI 1.003-1.02, p=0.006, log rank P=0.02]).
Conclusions
Predictors of fatal cardiac events are multifactorial and LV dysfunction as well as right sided volume overload is also one of the important predictors even in a representative right-sided cardiac disease, Ebstein’s anomaly.
DON’T HOLD YOUR BREATH: IS SLEEP APNEA MORE COMMON IN ADULTS WITH CONGENITAL HEART DISEASE?
Author links open overlay panelArwaSaidiPetarBreitingerDiegoMoguillanskyConnieNixonBrandonKueblerJamesFudgeFredrickFrickerKarenStout
University of Florida, Gainesville, FL, USA
University of Washington, Seattle, WA, USA
Background
The prevalence of sleep apnea (SA) is 5 to 10% in the general population. SA is associated with increased cardiac morbidity that can worsen the functional status of adult congenital heart disease (ACHD) patients. We hypothesized that ACHD patients have a higher prevalence of SA than the general population.
Methods
We prospectively invited patients aged > 18 years attending an ACHD clinic to participate in this study. We administered the Epworth Sleepiness Scale (ESS), a validated, reproducible measure to screen patients. Total scores ≥ 11 are highly suggestive of SA. Patient demographics, comorbidities and cardiac history were obtained from medical chart review.
Results
126 patients have participated in the study and completed ESS surveys of whom 18 patients (14%) had been previously diagnosed with SA and 28 others (22%) had an elevated ESS Score. Statistical analysis was performed.
| Patients with SA by diagnosis or ESS ≥ 11 (n = 46) | Patients without SA (n =80) | ||
| Male | 27 | 33 | NS |
| Female | 19 | 47 | NS |
| Mean age (years) | 37.5 | 33.9 | NS |
| Mean BMI | 29.8 | 25.5 | P=0.005 |
| Mean oxygen saturation- | 97 % | 96% | NS |
| Defect of moderate or great complexity | 42 | 74 | NS |
| Number of previous surgeries | 1.6 (0–4) | 1.8 (0–5) | NS |
| Co morbidities | 37 (80%) | 60 (75%) | NS |
Conclusions
Sleep apnea was observed in a third of ACHD patients and the prevalence is higher than in the general population. It is reasonable to consider including ESS screening as part of an ACHD evaluation given that:
(a)
Sleep apnea is associated with other cardiac morbidities associated with decreased functional status in ACHD patients, and
(b)
Availability of treatment options.
Further, the finding that participants with higher BMIs appear to represent a particularly vulnerable sub-group of patients suggests yet another reason to promote healthy weights in this patient population.
RIGHT VENTRICULAR MECHANICS IN ADOLESCENTS AND YOUNG ADULTS LATE AFTER REPAIR OF COARCTATION OF THE AORTA
Author links open overlay panelWing Yi VivianLiYiu-faiCheung
University of Hong Kong, Hong Kong, Hong Kong
Background
Alteration of right ventricular (RV) function has been found in patients with pressure-loaded left ventricles due to systemic hypertension and aortic stenosis. We tested the hypothesis that RV mechanics may be altered in adolescents and adults with repaired coarctation of the aorta (CoA) and related to left ventricular (LV) mass.
Methods
Twenty-eight (15 males) patients with CoA, aged 23.7±6.5 years, at 20.6±5.4 years after surgical repair and 28 (14 males) aged matched healthy controls were studied. Patients with significant residual CoA were excluded. M-mode, tissue Doppler imaging, and speckle tracking echocardiography were performed to assess LV mass and shortening fraction, anterior RV wall thickness, and RV myocardial tissue velocities and deformation.
Results
Systolic (p=0.14) and diastolic (p=0.32) blood pressure was similar between patients and controls. Compared with controls, patients had significantly greater LV shortening fraction(p=0.028), indexed LV mass (p=0.016), and indexed RV anterior wall thickness (p=0.012). With regard to RV mechanics, patients had significantly lower tricuspid annular systolic (p<0.001) and early diastolic (p<0.001) velocities, global RV systolic longitudinal strain (p=0.03), systolic strain rate (p=0.012), and early (p=0.021) and late (p=0.012) diastolic strain rates than controls. Patients with an associated ventricular septal defect (n=6) requiring closure compared to those without had even lower tricuspid annular systolic (p=0.01) and early diastolic (p=0.041) velocities. For the whole cohort, LV mass correlated negatively with RV systolic strain rate (r=−0.27, p=0.045) and tricuspid annular early diastolic velocity (r=−0.40, p=0.002), while RV anterior wall thickness correlated negatively with tricuspid annular systolic (r=−0.42, p=0.002) and late diastolic (r=−0.40, p=0.003) velocities, and positively with e/a ratio (r=0.31, p=0.024).
Conclusion
RV systolic and diastolic mechanics are impaired in patients late after repair of CoA, which are related to increased LV mass and RV thickness, even in the absence of residual CoA and systemic hypertension.
CLINICAL UTILITY OF THE LEVEL OF PLASMA BRAIN NATRIURETIC PEPTIDE IN TETRALOGY OF FALLOT PATIENTS LONG-TERM AFTER INITIAL INTRACARDIAC REPAIR: CONSIDERATION FOR PULMONARY VALVE REPLACEMENT
Author links open overlay panelAtsushiKitagawaTakashiHondaSumitoKimuraKagamiMiyaji
Department of Cardiovascular Surgery, Kitasato University School of Medicine, Masahiro Ishii
Department of Pediatrics, Kitasato University School of Medicine, Mimami, Sagamihara, Kanagawa, Japan
Background
The outcome of tetralogy of Fallot (TOF) patients after intracardiac surgery has improved over the years. We are now faced with an increasing number of patients who present with pulmonary insufficiency (PI) or right ventricular (RV) dysfunction, and these patients always have a risk for sudden death. However the indication of pulmonary valve replacement (PVR) is still uncertain. The purpose of this study was to evaluate the brain natriuretic peptide(BNP) level of patients with long after repair of TOF and to address the optimal surgical indication and timing of PVR.
Methods
We examined 33 patients (21 males, 12 females) older than 10 years of age who underwent TOF repair at Kitasato University Hospital.
Results
The median age at the initial repair was 1.1 (range 0.3 – 2.8) years. The median interval that had passed since the original corrective surgery was 12.2 (range 9.3 – 17.9) years. 27 patients had moderate-severe pulmonary valve regurgitation (PR) in echocardiography and 6 patients had trivial-mild PR. Patients who had moderate-severe PR had significantly higher brain natriuretic peptide (BNP) levels than patients who had trivial-mild PR (mean 37.5 ± 33.1 vs. 17.3 ± 6.6 pg/ml, p = 0.013). 7 patients underwent PVR and BNP levels were significantly decreased after PVR (mean 71.3 ± 46.1 to 26.1 ± 13.2 pg/ml, p = 0.021). All 7 patients who underwent PVR were also improved QRS duration (mean 167 ± 16 to 152 ± 12 msec, p = 0.042) and RV end-diastolic volume index (mean 126 ± 19 to 107 ± 15 ml/m2, p = 0.043), and New York Heart Association functional class.
Conclusions
The severity of PR may have a relationship with the BNP level long term after repair of TOF. The BNP level may contribute to defining the indication and timing of PVR for TOF long term after the initial repair.
SYSTOLIC TO DIASTOLIC DURATION RATIO AND EXERCISE STRESS RESPONSE IN 150 CHILDREN WITH AND WITHOUT HEART DISEASE: A TISSUE DOPPLER STRESS ECHOCARDIOGRAM STUDY
Author links open overlay panelLinda B.PauliksMattDeanStephenCyranDavid G.Currie
Penn State Hershey Medical College, Hershey, PA, USA
Background
In pediatric heart failure, systolic to diastolic duration ratio (SD ratio) may be an age-independent marker of disease. SD ratios are increased in cardiomyopathy and hypoplastic left heart syndrome. We analyzed SD ratio and exercise performance in children with and without heart disease.
Methods
In this study, 56 children with structural heart disease and 94 age-matched controls (Table) underwent clinically indicated Bruce treadmill maximum exercise stress echocardiograms. All reached ≥85% of maximum predicted heart rate (HR). Baseline and peak SD ratios were calculated from color tissue Doppler velocity traces, defining systolic duration as time from onset of QRS complex on ECG to end of isovolumic relaxation wave.
Results
SD ratio increased significantly with exercise stress in diseased hearts but not in controls (Table). Baseline SD ratio weakly correlated with exercise time for all patients (R −0.22; p<0.01) but not for controls alone. There was a strong correlation of HR and baseline SD ratio (R 0.78; p<0.001) but not for HR and peak SD ratio. Groups were otherwise comparable (Table).
Conclusions
In this study, the presence of structural heart disease altered the normal exercise response of the systolic to diastolic duration ratio in children (despite normal baseline SD ratios and exercise times). Only diseased hearts showed an increase of the SD ratio with stress: In controls SD ratios were maintained. This marker appears to be highly sensitive for subclinical cardiac dysfunction.
Effect of Exercise Stress on the Systolic to Diastolic Duration Ratio in 150 Children
| Parameter | Diseased (n=56) | Controls (n=94) | P value |
| Age (years) | 13.0 ± 3.5 | 13.2 ± 3.2 | NS |
| Height (cm) | 152.5 ± 20.5 | 155.4 ± 17.8 | NS |
| HR pre (bpm) | 90.6 ± 16.8 | 88.9 ± 15.1 | NS |
| HR post (bpm) | 194.4 ± 8.7 | 196.8 ± 9.5 | NS |
| HR post (% predicted) | 93.3 ± 4.7 | 94.5 ± 5.1 | NS |
| Exercise time (min) | 12.8 ± 2.7 | 12.7 ± 2.4 | NS |
| Peak MET | 14.9 ± 3.3 | 14.7 ± 2.9 | NS |
| SD ratio pre stress | 0.86 ± 0.22 | 0.86 ± 0.22 | NS |
| SD ratio post stress | 0.94 ± 0.24 | 0.85 ± 0.17 | P<0.01 |
RELATIONSHIP BETWEEN TOTAL CAVOPULMONARY CONNECTION GEOMETRY AND EXERCISE HEMODYNAMICS
Author links open overlay panelElaineTangReza H.KhiabaniKevinWhiteheadMariaRestrepoJamesBethelMarkFogelAjitYoganathan
Georgia Institute of Technology & Emory University, Atlanta, GA, USA
Children_s Hospital of Philadelphia, Philadelphia, PA, USA
Background
Patient-specific total cavopulmonary connections (TCPC) have complex geometries, which can impact the hemodynamics in the single ventricle circulations. Previous studies have shown that the TCPC energy dissipation under exercise conditions is negatively correlated to patient exercise tolerance. In this study, correlations between TCPC geometric features and patient exercise hemodynamic performance were investigated to identify possible predictors of poor exercise tolerance.
Methods
29 patients (age=19±6years) with TCPC anatomies were reconstructed from cardiac magnetic resonance (CMR) images. Geometric parameters analyzed included: vessel diameter, angles between connecting vessels, and caval offset (distance between the superior vena cava and the Fontan pathway (FP)), which are normalized by the square root of body surface area. Vessel flow rates were obtained from phase contrast CMR images acquired immediately following lower leg exercise in the supine position using a CMR-compatible cycle ergometer. Computational fluid dynamics simulations were carried out using time-averaged exercise flow boundary conditions to quantify power loss (PL). Linear regressions between the exercise normalized TCPC PL and its geometric features were investigated. Considering a statistical power >0.8, only correlations with r>0.4690 or r<-0.4690 are presented here (a<0.05, two-tailed).
Results
An inverse correlation between normalized PL at exercise and normalized minimum FP diameter was observed (r=−0.6370). Normalized exercise PL was also inversely correlated with normalized minimum pulmonary artery diameter (r=−0.4963). There was no significant difference between the correlations in intra-atrial (N=21) and extracardiac (N=8) TCPCs.
Conclusion
The results suggest that exercise tolerance in Fontan patients may be related to vessel narrowing at the FP. The dependence of normalized exercise PL on minimum FP diameters suggests it may be important to dilate such narrowing, and long-term follow-up can be recommended for these patients.
STRAIN TO EVALUATE VENTRICULAR FUNCTION IN FONTAN PATIENTS UNDERGOING EXERCISE CARDIAC MAGNETIC RESONANCE IMAGING
Author links open overlay panelShafkatAnwarRaviDoddaspmayajulaMarcKellerMatthewHarrisAjitYoganathanMarkFogelKevinWhitehead
The Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Introduction
Feature tracking strain (FTS) is a new technique to assess cardiac function from cardiac magnetic resonance (CMR) images. We compared FTS with conventional function parameters in single ventricle undergoing exercise CMR.
Methods
28 Fontan subjects underwent a resting and exercise CMR. Segmented balanced steady state free precession (SSFP) images were acquired at rest. Cartesian real time (RT) cine images were acquired at rest and exercise, targeting the HR at anaerobic threshold on a recent exercise stress test (EST). Ventricular volumes, cardiac output and feature tracking strain analysis was performed (TomTec 2D CPA, v. 1.0) on the “4-chamber” and short-axis views at basal, mid & apical levels.
Results
At rest there was moderate correlation between global circumferential strain (GCS) and stroke volume (SV), Pearson r = 0.48 (p = 0.009) and cardiac index (CI), r = 0.39 (p = 0.04), Figure 1 left panel. There was also good correlation between resting GCS and exercise SV, r = 0.56 (p = 0.002). At exercise there was good correlation between GCS, SV and cardiac output indexed to body surface area (SV/BSA, CI), r = 0.45 (p = 0.015) and r = 0.56, p = 0.002) respectively, Figure 1 right panel. There was no relationship between GCS and ejection fraction, end-diastolic volume or end-systolic volume.
Conclusion
In Fontan patients there is moderate correlation between strain and measures of ventricular output (SV and CI) at rest and exercise, but not directly to ventricular size or ejection.
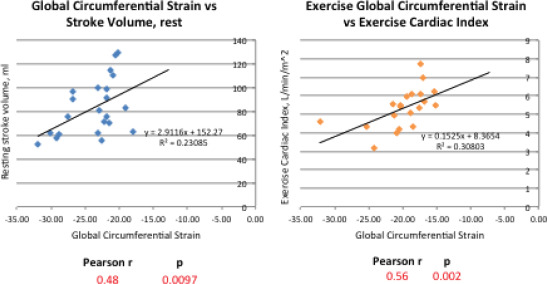
SPORTS PARTICIPATION AND QUALITY OF LIFE IN ADOLESCENTS AND YOUNG ADULTS WITH CONGENITAL HEART DISEASE (SQUAD STUDY)
Author links open overlay panelPeter N.DeanCatherine W.GillespieElizabethGreeneGailPearsonAdelaide S.RobbCharlesBerulJonathanKaltman
Children’s National Health System, Washington, DC, USA
Background
Adolescents and young adults with congenital heart disease (CHD) are often restricted from physical activity and sports participation. Our goal was to determine the amount of physical activity, type of sports participation, reasons for sports restrictions and quality of life (QoL) in a cohort of patients with CHD.
Methods
Individuals with CHD aged 13-30 years were recruited at outpatient visits or by mailings to participate in this cross-sectional study. Patients completed a questionnaire addressing physical activity, sports participation, sports restrictions and QoL (PedsQLTM). We interrogated the medical record for diagnosis, interventions, comorbid medical conditions, body mass index (BMI) and exercise stress test results (when available). Data were analyzed using Chi-square tests and multivariable linear regression.
Results
Of the 180 patients enrolled (mean age 19±5 years; 53% female), 32% have mild CHD, 40% have moderate CHD and 28% have severe CHD. In the cohort, 52% participate in competitive sports, 24% recreational sports and 24% no sports. Patients with moderate or severe CHD are less likely to participate in competitive sports than patients with mild CHD (p = 0.01). Of the patients with severe CHD, 29% participate in competitive sports that would be restricted by published guidelines (36th Bethesda Conference). After controlling for age, sex, CHD severity and presence of comorbidities, participation in competitive sports and increased frequency of physical activity are independently associated with a higher QoL (p=0.03 and p=0.007, respectively). In an identical model, participation in competitive sports and frequency of physical activity are associated with higher maximum predicted VO2 (n = 38; p = 0.003 and 0.03) and lower BMI (p = 0.006 and 0.02). Patients who report any type of restrictions (37% of patients) have marginally lower QoL (p = 0.08). Of the patient reported restrictions, 56% are due to physician recommendations, 24% to fear, 11% to pain and 9% to parent.
Conclusion
In a cohort of young CHD patients, participation in competitive sports and increased frequency of physical activity are associated with higher QoL, higher maximum predicted VO2 and lower BMI.
IMPLANTABLE CARDIOVERTER DEFIBRILLATOR OUTCOMES IN PEDIATRIC AND CONGENITAL HEART DISEASE: IT’S COMPLICATED
Author links open overlay panelBrynnDechertDavid J.BradleyGerald A.SerwerMacdonaldDickIIMartin J.LaPage
University of Michigan Mott Children’s Hospital, Ann Arbor, MI, USA
Background
ICDs are intended to prevent sudden cardiac death. They also impose a risk of increased morbidity. We describe the outcomes of ICDs in a pediatric and congenital heart disease(CHD) population from a single center.
Methods
Retrospective cohort study of all patients (pts) with an ICD followed at the University of Michigan Congenital Heart Center from 2005 – 2013. The primary outcome was ICD system revision for any reason excluding generator change for battery depletion. Post-revision devices were considered new for survival analysis purposes.
Results
There were 131 pts including 64 with abnormal heart structure (CHD or dilated cardiomyopathy), 24 with hypertrophic cardiomyopathy and 43 with a primary rhythm disorder. Mean age 20±13yrs at initial implant. All 190 ICD systems for these pts were analyzed. Total follow-up was 850 pt*yrs; median 4.9yrs / pt. Thirty pts (23%) received at least 1 appropriate device therapy. Inappropriate shocks were delivered in 39 pts (30%). There were 60 ICD system revisions in 41 (31%) pts, a rate of 70 revisions/1000pt*yrs. Indications for revision: 33 lead malfunction/fracture, 8 shock failure, 5 malpositioned leads, 3 infections, 2 lead perforations, and 6 others. Revisions included 25 lead extractions with replacements, 21 lead additions, 5 lead repositions, 4 full system revisions, and 5 other procedures. Kaplan-Meier (K-M) median time to appropriate shock was > 15.1yrs and median time to system revision 9.3 years (logrank p=0.41). K-M time to system revision was significantly shorter from 2005-2008 compared to pre-2005 (logrank p=0.001), but not different compared to 2009-2011 (logrank p=0.2).
Conclusions
This population of pediatric and CHD pts required ICD system revision at a similar rate to receiving appropriate therapy. Revision rates were higher from 2005-2008 compared to prior years. More recent systems have not shown a significant improvement in complication rate over short term follow-up.
NON-TRANSVENOUS LEAD IMPLANTATION IN PEDIATRIC AND CONGENITAL HEART DISEASE PATIENTS: EARLY ANALYSIS FROM THE NCDR®
Author links open overlay panelVicki A.FreedenbergChristopher PhillipsJordanJepthaCurtisYongfeiWangMaryeGlevaCharles I.Berul
Children’s National Medical Center, Washington, D.C., DC, USA
Yale School of Medicine, New Haven, CT, USA
Background
Implantable cardioverter-defibrillator (ICD) therapy in children and congenital heart disease(CHD) patients is challenging due to small patient size, complex venous and/or intracardiacanatomy. We sought to determine if patients with CHD or under age 21 had higher rates of non-transvenous lead implantation.
Methods
ICD procedures in patients with CHD or < 21 years of age in the ICD Registry between April 2010 – Dec. 2012 were included. Patients with transvenous (TV) and non-TV lead implants were compared for demographics, type of CHD, and implant indication. Non-TV included subcutaneous, epicardial, and pericardial coil placement, without a TV ICD lead. Univariate associations for continuous variables were assessed using F-test in ANOVA, categorical variables with X2 test.
Results
There were 4,614 ICD procedures for 4,527 patients in the cohort, in which 1576 were pediatric and 3076 had CHD. Overall, 97% of leads were TV (N=4477), and 3% non-TV (N=137). Mean age was lower in the non-TV (35.9±23 yr) than TV cohort (40.1±25, p=.05). Height was lower in non-TV (167.1±19cm) vs. TV group (170.4±13, p<.01). There were higher rates of non-TV lead implants among patients with transposition of great vessels(TGV) (16.1% vs. 7.9%, p<.01), and common ventricle (3.6% vs. 0.4%, p<.01). Among the pediatric cohort, the non-TV had lower age (10.3±8 vs. 12.6±8 yr, p=.04), height (163.7±26 vs. 169.1±16 cm, p=.03) and weight (67.2±25 vs. 76.5±27 kg, p=.02). There was no significant difference in TV or non-TV routes between this cohort and all other implants in the registry over same period (TV leads: N=406,010, 97.5%; non-TV: 10,558, 2.5%, p=.09).
Conclusion
ICD Registry data show that non-TV leads were implanted in younger and smaller patients. Higher rates of non-TV implants occurred in patients with TGV and common ventricle. These pediatric and CHD patients are not adequately served by current technology and TV approach to ICD lead implantation.
THROMBOEMBOLIC COMPLICATIONS AFTER FONTAN OPERATION WITH ATRIAL FLUTTER
Author links open overlay panelJiuann-Huey I.LinTimothyCordes
Riley Hospital for Children, Indianapolis, IN, USA
Background
Atrial arrhythmia remains one of the major complications after Fontan procedure. This study explores the incidence of thromboembolic complications in Fontan patients with atrial flutteracutely after electric cardioversion.
Methods and Results: We performed a retrospective chart review of 49 patients with a history of Fontan operation treated with electric cardioversion for atrial flutter at Riley Children’s hospital between 1990 and 2013. Thirty-one (63.3%) patients originally had a history of a classic Fontan procedure. Thirteen of 49 patients had a lateral caval tunnel, 3 of 49 patients underwent a right atrium to RVOT modification, and two had an extra-cardiac Fontan. The 49 patients experienced 179 episodes of atrial flutter requiring electric conversion. Right atrial clots occurred in 30 patients (61.2%). Twenty-three of 30 patients had an atriopulmonary Fontan (76.7%), 4 patients had a lateral caval tunnel had clots in the Fontan conduit and all three patients with right atrium to RVOT connections presented with right atrial mural thrombi. 164 transthoracic echocardiogram (TTE) and 22 transesophageal echocardiogram (TEE) were performed prior to cardioversion with intracardiac thrombi were detected in 57 TTEs and 10 TTEs. All of these 49 patients received anti-coagulations. Electric cardioversion was performed either clear of intracardiac thrombi or after at least 2 weeks of anticoagulation administration with evidences of thrombi becoming organized. Five of 49 (10.2%) patients had documented stroke, although none were associated with electric cardioversion. Despite of the aggressive medical and surgical management of Fontan patients with atrial flutter, 21 patients (42.9%) remained in intermittent or persistent atrial flutter, 28 patients have remained in normal sinus rhythm.
Conclusion
Thromboembolism is a frequent phenomenon in Fontan patients with atrial flutter. However, none of the cardioembolic strokes were associated with cardioversion in our series. The risk of cardioembolic stroke with atrial flutter in a Fontan patient on anticoagulation therapy is low, even with a 61.2% incidence of organized thrombus in the venous circulation.
QRS DURATION CHANGES IN PATIENTS WITH SINGLE VENTRICLE PHYSIOLOGY: BIRTH TO 10 YEARS
Author links open overlay panelSairahKhanHollyNadorlikNaomiKerteszLisaNicholsonPamela S.RoCliffordCua
Nationwide Children’s Hospital, Columbus, OH, USA
Background
QRS prolongation may be a predictor of mortality in certain forms of congenital heart disease. Minimal data exist describing changes in QRS duration in patients with single ventricles (SV). Goal was to describe changes in QRS duration in patients with SV and to determine if differences existed between single right ventricle (sRV) versus single left ventricle (sLV) patients.
Methods
Chart review was performed on patients with SV physiology. Patients were divided into sRV and sLV groups. QRS durations were measured monthly for the first six months, at one year, and then yearly until 10 years. T-tests were used for analysis.
Results
One hundred sixty patients were evaluated (95 sRV, 65 sLV). Greatest change in QRS duration for the entire cohort occurred in the first 6 months of life versus 6 months to 10 years of age (1.81 ms/month vs. 0.20 ms/month) (Figure 1). sRV QRS durations were significantly longer than sLV QRS durations at 1 year (78.9 + 1.5 ms vs. 73.2 + 1.8 ms), 2 year (81.7 + 1.7 ms vs. 73.4 + 1.8 ms), 4 year (84.2 + 1.5 ms vs. 77.9 + 2.5 ms), 6 year (90.8 + 2.0 ms vs. 83.4 + 2.3 ms), 7 year (90.8 + 3.0 ms vs. 81.2 + 2.9 ms), and 8 year (96.7 + 2.7ms vs. 84.8 + 2.7 ms) time points.
Conclusion
Greatest change in QRS duration in SV patients occurred in the first six months of life when these patients’ ventricles are volume loaded. Differences in QRS duration between sRV and sLV patients occurred early in life. Further studies are needed to determine if minimizing volume load early in life decreases the rate of change in QRS duration.
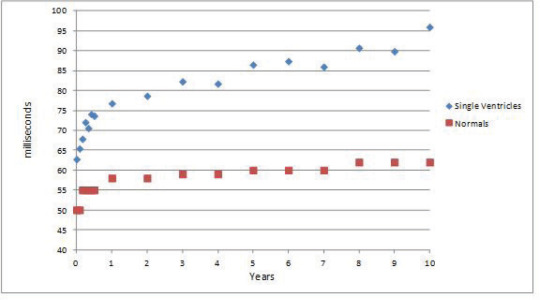
CARDIAC SURGERY OUTCOMES IN HETEROTAXY SYNDROME: 25 YEARS EXPERIENCE FROM A MULTICENTER CONSORTIUM
Author links open overlay panelShanthiSivanandamParvinDorostkarLazarosKochilas
University of Minnesota, Minneapolis, MN, USA
Background
Heterotaxy syndromes of asplenia and polysplenia encompass a wide spectrum of complex cardiovascular abnormalities associated with left-right asymmetry. The combination of structural and electrical cardiac abnormalities along with extracardiac co-morbidity makes cardiac surgery in heterotaxy syndrome challenging and associated with high morbidity and mortality. We report the mortality after cardiac surgery in patients with heterotaxy from the Pediatric Cardiac Care Consortium (PCCC).
Methods
We identified 1,169 patients with a diagnosis of heterotaxy that underwent cardiac operation in a PCCC center between 1982 and 2005.
Results
753 (64.4%) had asplenia and 416 (35.6%) polysplenia. Detailed results are presented in the following table.
| A. Initial Procedure | ||||
| Asplenia | Polysplenia | |||
| n | Mortality | n | Mortality | |
| Aorto-Pulmonary shunt | 375 | 17% | 114 | 13.20% |
| Pulmonary band | 25 | 28% | 21 | 38.10% |
| Glenn shunt | 44 | 9.10% | 18 | 0.00% |
| Fontan | 8 | 37.50% | 11 | 27.30% |
| Total anomalous pulmonary venous return repair | 157 | 47% | 17 | 23.50% |
| Pacemaker | 8 | 25% | 30 | 46.7% |
| Miscellaneous* | 136 | 13.4% | 205 | 24.50% |
| Total | 753 | 27.8% | 416 | 30.5% |
| B. Subsequent Procedures | ||||
| Asplenia | Polysplenia | |||
| n | Mortality | n | Mortality | |
| Aorto-Pulmonary shunt | 110 | 10.90% | 34 | 0% |
| Glenn shunt | 257 | 5.80% | 92 | 5.40% |
| Fontan | 274 | 15.30% | 97 | 9.30% |
| Total anomalous pulmonary venous return repair | 45 | 24.40% | ||
| Miscellaneous* | 233 | 6.9% | 116 | 6.9% |
| Total | 919 | 11.6% | 339 | 6.3% |
| C. Accumulative outcomes after 1st and subsequent procedures | |||
| Asplenia | Polysplenia | All Heterotaxy | |
| n (total patients) | 753 | 416 | 1,169 |
| n1 (survivors 1st procedure) | 543 (72.1%) | 289 (69.5%) | 832 (71.2%) |
| n2 (survivors subsequent procedure) | 480 (63.7%) | 272 (70.4%) | 752 (66.3%) |
| Univentricular palliation (% of n1) | 232 | 89 | 321 |
| Cardiac transplantation | 20 (2.7%) | 13 (3.1%) | 33 (2.8%) |
| Pacemaker/AICD | 65 (8.7%) | 89 (21.4%) | 154 (13.2%) |
| Overall mortality | 267 (35.8%) | 114 (27.4%) | 381 (32.6%) |
*
Miscellaneous procedures include: atrioventricular valve repair, closure of atrial or ventricular septal defects, augmentation of the aorta and others.
Conclusion
Our results illustrate a high overall surgical mortality (32.6%) in patients with heterotaxy syndrome (35.9% in asplenia and 27.4% in polysplenia). Univentricular palliation occurs frequently in asplenia (48.3%) than polysplenia (32.7%) survivors (p<0.01). Pacemaker implantation occur in 1% of the asplenia and 7% in polysplenia (p<0.0001) with significant mortality (25% and 46.7% respectively).
ANNULUS-SPARING TETRALOGY OF FALLOT REPAIR IN THE MODERN ERA: LOW COST AND EARLY EVIDENCE OF POTENTIAL BENEFITS TO RV GEOMETRY
Author links open overlay panelEdwardHickeyEricPham-HungMichaelGrittiChristopherCaldaroneAndrewRedingtonGlenVan Arsdell
The Hospital for Sick Children, Toronto, Canada
Background
Annulus-sparing (AS) repair of tetralogy of Fallot (TOF) carries a potential cost of increased reoperation for re-stenosis and unproven benefits on RV geometry.
Methods
Primary TOF repairs (N=458) between 2000 and 2012 were studied. Prior palliation was rare (invariably RVOT stent; N=16).
Results
Repair was mean age 180 days: AS in 297 (65%), trans-annular patch (TAP) in 137 (30%) and conduit in 24 (5%). Intra-op revisions (for residual stenosis) were required in 135 (29%). In the AS group, if reoperation was required for RVOT re-stenosis, the strategy “failed” (14/297, 5%). Failed strategies were linked to smaller pre-op PV (5.6 v 7.5 mm, P=.01), RVEDD (0.9 v 1.2 cm, P=.04) and TV dimensions (1.2 v 1.4 cm, P=.04). Failed strategies were significantly related to smaller RVOT (mean 9 vs 10.5 mm, P=.01) and higher RVSP (mean 56 vs 45 mmHg, P=.002) measured intra-op after repair (figure). Repeated measures analysis of 2,103 RVEDD and 2,009 QRS measurements demonstrated accelerated RV dilatation in TAP versus non-TAP P<.0001, figure), but no differences in QRS. Only 4 deaths have occurred (survival 99%). Surgical re-intervention to a TAP was occasionally required (5/137, 4%) and this rate was not different to the AS group (P=.83).
Conclusions
The cost of pursuing an AS approach seem negligible. PV enlargement to >10 mm and RVSP <50 should equate to low risk of restenosis. Faster RV dilatation after TAP seen herein supports AS strategy. Whether the AS strategy will translate into reduced PVR rate is not known.
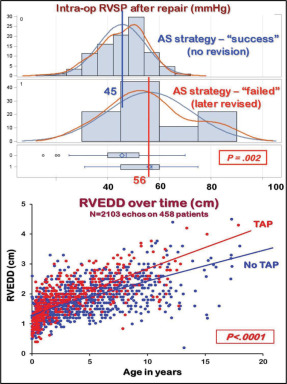
RESOURCE UTILIZATION AND OUTCOME FOLLOWING THE GLENN AND FONTAN OPERATION: A MULTI-INSTITUTIONAL STUDY
Author links open overlay panelKevinHinkleJacobWilkesShajiMenon
University of Utah, Salt Lake City, UT, USA
Background
Compared to the Glenn, the Fontan operation is thought to be associated with longer hospitalization and resource utilization. There is a lack of large, multi-institutional and contemporary data on resource utilization and outcomes following the Glenn and Fontan operation. The objective of this study was to evaluate resource utilization and outcomes associated with the Fontan operation in a large multi-institutional cohort.
Methods
Retrospective review of all patients who underwent a Glenn and survived to the subsequent Fontan operation (1/2004-6/2011) using the Pediatric Health Information Systems Database (44 US children’s hospitals). Generalized linear regression analyses were performed to evaluate factors associated with resource utilization and mortality.
Results
Of 2190 patients included in the study, 55% were males. The mean age at Glenn and Fontan were 5.2 months and 2.8 years respectively. The mean duration between Glenn and Fontan operation was 2.7 years. The mean length of hospitalization at the Glenn and Fontan operations were 13.5 days and 13.1 days respectively. Post-operative mortality following the Fontan was 1% (n=21). Atrioventricular valuloplasty was performed in 9% of patients during the Glenn and Fontan each. Following the Fontan, 7% had heart block, 13% had tachycardia, 3% developed stroke, 1% underwent dialysis, and 2% had diaphragm paralysis before hospital discharge. The median cost in 2012 Dollars for the Glenn and Fontan operations were $46,976 and $55,868 dollars respectively.
Conclusions
Pediatric Health Information Systems Database provides a large and comprehensive dataset to evaluate outcomes and resource utilization following Glenn and Fontan. The duration of hospitalization following a Fontan operation is similar to post Glenn hospitalization. However, the cost of hospitalization post Fontan was higher when compared to the Glenn hospitalization.
CHRONIC MITRAL REGURGITATION: WHEN SHOULD WE INTERVENE IN ASYMPTOMATIC CHILDREN?
Author links open overlay panelJoyceJohnsonAaronEckhauserHsin-YiWengL. LuAnnMinichLloydTani
University of Utah, Salt Lake City, UT, USA
Background
Surgery is currently recommended for asymptomatic adults with chronic severe mitral regurgitation (MR) associated with systolic dysfunction, pulmonary hypertension, atrial fibrillation, or high likelihood of successful repair. Surgical indications in asymptomatic children with chronic MR are not well defined. We sought to determine predictors of postoperative left ventricular (LV) dysfunction in children with chronic MR.
Methods
Retrospective chart review of children who underwent mitral valve surgery for chronic MR in the absence of symptoms (2000-12). Exclusion criteria: acute MR, cardiomyopathy, or other cardiac defects known to affect LV size. Clinical and echo data were obtained. LV dysfunction was defined as ejection fraction (EF) ≤55% or shortening fraction (SF) ≤28% at latest follow-up. Associations between preoperative factors and late postoperative LV dysfunction were determined using univariate logistic regression.
Results
Surgery was performed in 25 asymptomatic children (40% male), including 17 repairs and 8 replacements. Preoperatively, 2 (8%) had pulmonary hypertension and 3 (12%) had atrial arrhythmias. The preoperative median LV end systolic z-score (LVESZ) was 5.3 (IQR 2.9-6.9), EF was 65% (IQR 61-69.5%), and SF was 34% (IQR 31-41%). The median age at surgery was 8.6 (IQR 4.7-12.7) years with no perioperative deaths and a median follow-up of 5 (IQR 2.4-8.6) years. Late LV dysfunction (n=9, 36%) was associated with a lower preoperative SF (OR 0.6, 95% CI 0.4-0.9, p<0.001) and a higher LVESZ (OR 1.7, 95% CI 1.03-2.7, p<0.01). The combination of LVESZ ≥5 and SF ≤33% had a sensitivity of 89%, specificity of 88%, positive predictive value of 80%, and negative predictive value of 93% for late LV dysfunction. In patients with a preoperative SF ≥34%, only 1/13 had late LV dysfunction (negative predictive value 92%). Residual MR was ≤grade 2 in 22 (88%) and none were symptomatic at latest follow-up.
Conclusions
To prevent late postoperative LV dysfunction in asymptomatic children with chronic MR, surgery should be considered before LVESZ ≥5 and SF ≤33%. In asymptomatic patients with SF ≥34%, observation with serial echocardiographic measurements may be appropriate.
PREDICTING OUTCOME FOLLOWING INFANT CARDIAC SURGERY
Author links open overlay panelKurtSchumacherDanielEhrmannSunkyungYuJanetDonohueRobertGajarskiJohnCharpie
University of Michigan Congenital Heart Center, Ann Arbor, MI, USA
Background
Many patient and procedural characteristics have been investigated for their impact on outcomes after infant heart surgery, but risk-stratification models incorporating early post-operative biophysical markers are lacking. This study aimed to identify independent risk factors for poor outcome and to build a risk stratification model.
Methods
This prospective, observational study in a pediatric cardiac ICU analyzed pre- and post-operative data in infants (< 12 months) undergoing cardiac surgery to determine which factors were associated with a composite “poor” outcome of death, emergent need for extracorporeal life support, and dialysis. Independent risk factors were used to build a simple risk score based on adjusted odds ratio (AOR).
Results
In 283 infants enrolled, factors significantly associated with poor outcome in univariate analyses were as follows: gender, age, size, STS-EACTS category, single ventricle, heartrate, arterial pressure, central venous pressure, vasoactive inotrope score, serum lactate, and arterial blood gas values including pH, bicarbonate and base excess. Multivariable logistic regression identified the following independent risk factors for poor outcome and points were assigned: male gender (AOR 4.4; 95% confidence interval (CI) 1.1, 17.4; 1 point), minimum pH ≤ 7.19 (AOR 6.7; CI 1.6, 27.4; 1 point), base excess ≤ −5.1 (AOR 9.9; CI 2.1, 47.7; 2 points) and lactate ≥ 5.6 (AOR 23.8; CI 2.8, 201; 3 points). The model had near perfect discrimination (C-statistic = .97) between high and low risk patients and was well calibrated (goodness of fit c = 2.72, p = .44). Using the scoring system, the incidence of poor outcome increased linearly from 0% in patients with a risk score of 0 points (70.6% of the cohort) to 16.7% in patients with a risk score of 4-5 points (11.2% of the cohort) to 45.8% in patients with a risk score of 7 points (4.5% of the cohort).
Conclusions
Independent risk factors for poor outcome after infant heart surgery were identified and used to construct a simple risk score that accurately identified high and low risk patients based on early post-operative clinical variables. Once externally validated, this risk score may be helpful to guide therapy.
PREDICTORS OF EARLY POSTOPERATIVE COMPLICATIONS AFTER ARTERIAL SWITCH OPERATION OF NEWBORNS WITH TRANSPOSITION OF THE GREAT ARTERIES
Author links open overlay panelPetruLiubaLoveAhlstrm
Pediatric Heart Center, Lund, Sweden
Background
Lund is one of the two tertiary referral centers for pediatric cardiac surgery in Sweden, with nearly 350 surgical procedures every year. We performed a retrospective analysis of newborns and infants with transposition of the great arteries (TGA) operated with arterial switch (ASO) during the past 10 years.
Methods
a single-institution retrospective analysis of nearly 100 newborns and infants with transposition of the great arteries (TGA) operated with arterial switch during the past 10 years. Postoperative morbidity and mortality during the the first month was recorded. Patients with TGA/double outlet right ventricle were excluded from the analysis.
Results
103 patients with TGA (median for birth weight, gestational week, and age at surgery: 3.5 kg, 39 weeks, and 4 days) were included. There was only 1 death. Surgery beyond 5 days of age (n=46) was associated with prolonged mechanical ventilation (p<0.05) but with comparable overall postoperative ward duration. Prematurity (<36 weeks of gestation) was significant predictor for delayed sternum closure (p=0.01) and prolonged postoperative mechanical extubation (p<0.0001). Preoperative minor cerebral insult (documented on MRI, n=5) was found in 11 % of patients who underwent balloon atrial septostomy (BAS) prior to ASO but not in the non-BAS group, and had no impact on the overall postoperative stay duration.
Conclusion
At our institution, ASO of full term babies with TGA can be performed safely even beyond the first week of life.
INTRAOPERATIVE ECHOCARDIOGRAPHIC PREDICTORS OF EARLY REOPERATION FOR RECURRENT REGURGITATION AFTER CONGENITAL AORTIC VALVE REPAIR
Author links open overlay panelKenan W.D.SternMatthewWhitePedrodel NidoTalGeva
Boston Children’s Hospital, Boston, MA, USA
Background
Post-cardiopulmonary bypass transesophageal echocardiography (post-CPB TEE) is routinely performed to evaluate the adequacy of congenital aortic valve repair. Post-CPB TEE risk factors for early valve dysfunction requiring reoperation have not been reported.
Methods
We analyzed post-CPB TEEs in patients with congenital aortic valve disease undergoing valve repair for predominant regurgitation (AR). Cases underwent reoperation for recurrent AR within 2 years whereas controls were free from reoperation for >2 years. Measurements of aortic dimensions, leaflet prolapse, and asymmetry were obtained.
Results
Cases (n=22; median time to reoperation 0.3 years) and controls (n=28; median freedom from reoperation at least 4.2 years) were similar with respect to demographics, aortic dimensions, and degree of preoperative AR. Cases had higher indexed LV diastolic volume by MRI (median 155 vs. 128 ml/m2, p=0.01) and lower peak aortic stenosis Doppler gradient (median 24 vs. 43 mm Hg, p=0.02). Cases underwent more valve-sparing aortic root and/or ascending aorta replacements (27% vs. 0%), and fewer subaortic resections (0% vs. 21%, p=0.004 for both). Post-CPB TEE risk factors for early reoperation on univariate logistic regression analysis included prolapse of the anterior leaflet (odds ratio (OR) for every 1mm of prolapse below the annular plane 1.3, 95% confidence interval (CI) 1.01-1.69, p=0.046), shorter distance from the leaflet coaptation tip to the annulus (OR for 1 mm decrease 1.39, 95% CI 1.07-1.82, p=0.012), and increased percent difference (%diff) between longest and shortest commissural lengths in a short-axis view (OR for 10% increase 1.76, 95% CI 1.15- 2.68, p=0.009). A forward-selection model building procedure identified %diff in commissural lengths as the strongest predictor of early reoperation (area under the receiver operator curve = 0.72). The sensitivity and specificity of a %diff of 50% were 0.45 and 0.92 whereas a %diff of 25% had a sensitivity of 0.8 and specificity of 0.42.
Conclusion
Leaflet asymmetry, measured as increased %diff in commissural lengths on post-CPB TEE, is associated with early reoperation for recurrent AR after congenital valve repair.
ATRIAL AND VENTRICULAR MECHANICS IN PATIENTS AFTER FONTAN-TYPE PROCEDURES: ATRIOPULMONARY CONNECTION VERSUS EXTRACARDIAC CONDUIT
Author links open overlay panelShujuanLiSophiaWongYiu-FaiCheung
Division of PaediatricCardiology, Department of Paediatrics and Adolescent Medicine, QueenMaryHospital, HongKong, People’s Republic of China
Department of Paediatric Cardiology, the First Affiliated Hospital of Sun Yat-sen University, Guangzhou, People’s Republic of China
Background
Differences in systemic venous flow dynamics and energy losses exist in various Fontan-type procedures, which may affect atrial and ventricular filling. Fontan conversion has been advocated in patients with failing atriopulmonary connection (APC). We tested the hypothesis that atrial and ventricular mechanics differ between two types of Fontan procedures, APC and extracardiac conduit (EC), which have distinctly different systemic venous haemodynamics.
Methods
Twenty-eight Fontan patients (13 APC, 15 EC) aged 19.8±6.5 years were studied. Atrial and systemic ventricular myocardial deformation was determined using speckle-tracking echocardiography, while ventricular volumes and systolic dyssynchrony index were assessed by three-dimensional echocardiography. The results were compared with those in 26 controls.
Results
Compared with controls, patients had significantly lower global ventricular systolic strain in all three dimensions, reduced systolic and early diastolic strain rates (SRs) in more than one dimension, lower ejection fraction, and worse ventricular dyssynchrony. For atrialdeformation, patients had lower global and positive strain and conduit and reservoir SRs, and delayed electromechanical coupling. Among patients, those with APC had significantly lower ventricular longitudinal strain and early diastolic SR, worse ventricular dyssynchrony, and reduced atrial positive and negative strain and conduit and active contractile SRs. Atrial global strain (r=0.60, p =0.001) and conduit SR (r=0.49, p=0.008) correlated positively with systemic ventricular early diastolic SR.
Conclusions
Atrial and ventricular mechanics are impaired in patients after Fontan-type operation, which is worse with APC than EC. Our findings provide a mechanical basis for Fontan conversion in patients with failing APC.
EXPLORING THE RELATIONSHIP BETWEEN HEMOCONCENTRATION AND OUTCOME IN PATIENTS UNDERGOING NORWOOD OPERATION
Author links open overlay panelStephanie L.SiehrHuZhongkaiJinBoLing XuefengBruceAndrewShin
Stanford University, Palo Alto, CA, USA
Background
The practice to raise hematocrit in cyanotic patients following palliative congenital heart surgery is controversial. The purpose of this study is to understand the relationship between hemoconcentration and clinical outcome for patients with Hypoplastic Left Heart Syndrome(HLHS) following the Norwood operation.
Methods
Infants with HLHS (or HLHS variants) admitted to our medical center from September 2009 to December 2012 undergoing Stage 1/Norwood operation were identified. Charts were abstracted for baseline demographic and clinical information, including first recorded post-operative hematocrit and subsequent mean, median and nadir hematocrits during the first 72 hours post-operatively. The primary outcomes were in-hospital mortality and length of hospitalization.
Results
Thirty-two patients were included in the analysis. Hemoconcentration (Hct > 50%) was associated with longer CVICU stay [51.0 (±38.6) vs 21.4 (±16.2) days, p=0.002] and total hospital length of stay [65.0 (±46.5) vs 36.1 (±20.0) days, p=0.034]. Patients did not differ by operative factors (cardiopulmonary bypass time, cross clamp time), severity of illness (vasoactive infusion score, lactate, saturation, P/F ratio) or mortality. In a multivariate analysis, hemoconcentration remained independently associated with length of hospitalization after controlling for amount of red blood cell transfusion [OR 78 (95% CI 3.84-1590), p=0.036].
Conclusions
Hemoconcentration in the first 3 days following Norwood operation is independently associated with longer length of hospitalization even after controlling for blood cell transfusion practices. Our study suggests that hemoconcentration may be used as an early marker of disease severity complicating the concept of an ‘optimal hematocrit’ for post-operative cyanotic patients.
MAJOR ADVERSE CARDIAC EVENTS IN CHILDREN WITH WILLIAMS BEUREN SYNDROME UNDERGOING SURGERY: AN ANALYSIS OF THE SOCIETY OF THORACIC SURGEONS CONGENITAL HEART SURGERY DATABASE
Author links open overlay panelChristoph P.HornikRobertJaquissJeffreyJacobsMarshallJacobsSaraPasqualiAmeliaWallaceKevinHill
Duke University, Durham, NC, USA
Background
Children with Williams Beuren Syndrome (WBS) undergoing cardiac surgery are at risk for major adverse cardiac events (MACE) but the frequency of and risk factors for such events have not been well described. We sought to better define frequency and risk of MACE in WBS using the STS-CHS Database.
Methods
We examined patient characteristics and in-hospital outcomes for cardiac operations in WBS patients (2000-2012) using the STS-CHS Database. The cohort was divided into 4 procedural groups: isolated supravalvar aortic stenosis, complex left ventricular outflow tract(LVOT), isolated right ventricular outflow tract (RVOT) and combined LVOT + RVOT surgeries. We used univariate logistic regression to evaluate the association between preoperative factors and a composite outcome of in-hospital death, cardiac arrest or postoperative mechanical circulatory support.
Results
Of 447 index operations (87 centers), median (IQR) age and weight at surgery were 2.4 years (0.6, 7.4) and 10.6 kg (6.5, 21.5). Overall mortality was 4.5%. The composite outcome occurred in 9.2% but with significant procedural variability (p<0.001) [Table1]. Odds of the composite outcome were lower with increasing weight (OR=0.97; 95% CI 0.93, 0.99) and age (OR=0.99; 95% CI 0.98, 0.99) at surgery, but higher in the presence of any preoperative risk factor (OR=2.1; 95% CI 1.1, 4.0).
Conclusion
Major adverse cardiac events are common in WBS following left sided cardiac surgery but less frequent after isolated RVOT surgery.
ACUTE KIDNEY INJURY FOLLOWING SURGERY FOR CONGENITAL HEART DISEASE: ROLE OF URINE BIOMARKERS, RENAL PERFUSION PRESSURE, AND SOMATIC OXYGEN SATURATION
Author links open overlay panelDavid A.HehirJohn P.ScottKevinRegnerMatthewBuelowAmanda J.ShillingfordPippaSimpsonYumeiCaoAaron T.DallBrianaHornMichaelMitchellJamesTweddellNancy S.GhanayemGeorgeHoffman
Medical College of Wisconsin, Milwaukee, WI, USA
Background
Acute kidney injury (AKI) is common following cardiopulmonary bypass (CPB), and may result in increased morbidity and mortality. Definitions of AKI that rely solely on serum creatinine are inaccurate markers of early renal injury. We investigated the role of urine biomarkers and indices of renal perfusion in the detection of AKI.
Methods
Prospective observational study of 120 children undergoing surgery with CPB. AKI defined as creatinine increase >50% or >0.3 mg/dL from pre-operative baseline within 48 hours of CPB. Urine NGAL, IL18 and KIM1 measured pre-op and at 6 post-op time points over 72 hours. Vital signs, fluid balance, renal perfusion pressure (RPP=mean arterial pressure-central venous pressure), arterial-somatic oxygen saturation difference (DaRSO2) and vasoactive inotrope score (VIS) were measured.
Results
Median age was 9 months (1 week – 17 years), 47 (39%) had single ventricle heart disease, and 25 (20%) were RACHS 4-6. 54/120 (45%) had AKI. Subjects with AKI had longer CPB (p=.025), lower urine output in the first 24 hours (p=.025), and lower baseline creatinine (p=.005). At ICU arrival, subjects with AKI had higher VIS (p=.008), higher heart rate (p=.01) and lower RPP (p=.03). AKI resulted in longer chest tube drainage, time of intubation and length of stay. Although biomarker levels were higher in AKI, they discriminated poorly by receiver operating characteristic, with an area under the curve for NGAL = .6, KIM1 = .61 and IL18 = .625. Multivariable logistic regression found lower urine output (OR 1.06 {1.03, 1.1}; p<.001), higher chest tube drainage (OR 1.04 {1.01, 1.07}; p=.01), and a higher VIS (OR 1.08 {1.002, 1.2}; p=.04) to be associated with AKI. Classification tree analysis using urine output, NGAL, KIM1, central venous pressure, and mean arterial pressure resulted in a model with a sensitivity of 92% and specificity of 68% for AKI.
Conclusions
AKI was common in this cohort, and associated with increased length of stay and morbidity. Current creatinine-based definitions of AKI in children may be improved by incorporation of urine biomarkers, urine output, and indices of renal perfusion. These results provide targets for goal-directed therapy to prevent and treat AKI.
MAGNESIUM LOWERS THE INCIDENCE OF POSTOPERATIVE JUNCTIONAL ECTOPIC TACHYCARDIA IN CONGENITAL HEART SURGICAL PATIENTS: IS THERE A RELATIONSHIP TO SURGICAL PROCEDURE COMPLEXITY?
Author links open overlay panelDingchaoHeNathanielSznycer-TaubYaoChengRobertMcCarterRichardJonasHanumanthaiahSridharJeffreyMoak
Children’s National Medical Center, Washington, DC, USA
Background
The occurrence of postoperative junctional ectopic tachycardia (PO JET) is more frequent in certain types of congenital heart surgery (CHS). Magnesium decreases the incidence of PO JET. We tested the hypothesis that magnesium is more effective with more complex surgery.
Methods
1088 CHS, performed from 2005 to 2010, were reviewed. 750 cases (non-magnesium group) did not receive magnesium and 338 cases (magnesium group) received magnesium (25 mg/kg) after aortic cross clamp was released. All procedures were classified according to Aristotle Score from 1 to 4. Pearson chi-square test and logistic model analyses were used to evaluate the effect of magnesium on PO JET in the two groups and in different Aristotle levels of complexity.
Results
Overall there was a significant difference in PO JET occurrences between the two groups regardless of the Aristotle score, 15.33% (115/750) in non-magnesium group vs. 7.10% (24/338) in magnesium group, P<0.001. Reduction of PO JET was significantly greater with increasing Aristotle level of complexity (PO JET in Aristotle Level 1 – non-magnesium vs. magnesium group: 1.82% vs. 10.00%; Level II: 9.73% vs. 6.32%; Level III: 27.91% vs. 13.89%; Level IV: 14.89% vs. 0%; odds ratio = 0.49, 95% CI = (0.29, 0.85), P = 0.01). Aortic cross clamp time increased with higher level of Aristotle complexity (level I: 29.4 ± 13.8 min, level II: 31.7 ± 22.6, level III: 44.3 ± 18.1, level IV: 66.6 ± 26.9). We also confirmed our previous finding that JET occurred more commonly with dopamine and milrinone infusions in both groups (odds ratio = 1.81, 95% CI = (1.10, 2.96), P = 0.018 for dopamine; odds ratio = 2.85, 95% CI = (1.84, 4.41) P <0.001 for milrinone).
Conclusions
Intra-operative usage of magnesium reduced the occurrence of PO JET in patients undergoing CHS, and was more effective in CHS with higher level of Aristotle complexity. We speculate that magnesium may lessen the effects of ischemia and retraction in more complicated CHS with longer cross-clamp times. Despite the intra-operative usage of magnesium, postoperative administration of dopamine and milrinone continued to increase the risk to develop JET.
CREATION OF A SURGICAL FONTAN ANIMAL MODEL AND THE USE OF A VENTRICULAR ASSIST DEVICE TO RESTORE CARDIAC OUTPUT
Author links open overlay panelGwendolyn R.DerkHillelLaksReshmaBiniwaleSanjeetPatelKimDeLaCruzEinatMazorRyanWilliamsJohnValdovinosDanielLeviJamilAboulhosn
Ahmanson/UCLA Adult Congenital Heart Disease Center, Los Angeles, CA, USA
UCLA, Los Angeles, CA, USA
Background
Current ventricular assist devices are not designed for use in patients with failing Fontans. This study evaluated the efficacy of the Jarvik 2000 ventricular assist device (VAD) as a pulmonary pump to power a Fontan circuit in a large animal model.
Methods
Without the use of cardiopulmonary bypass, Fontan circulations were surgically created in 4 pigs (50kg) using synthetic grafts from the inferior and superior vena cavas to the main pulmonary artery. The VAD was then implanted within the common Fontan graft to provide a pulmonary pump. Chamber pressures and epicardial Doppler images were taken during each phase of the experiment. Heart rate, femoral artery blood pressure, oxygen saturation, and aortic flow rate were continuously recorded. The outflow cannula of the VAD was then banded by 50% and 75% to mimic increased afterload.
Results
The Fontan and VAD implantation were successfully performed in all 4 animals. Arterial pressure and aortic flow decreased dramatically with institution of the Fontan but were restored to baseline upon activation of the VAD. The pressure within the systemic venous circulation rose precipitously with institution of the Fontan circulation and improved appropriately with VAD activation. (Figure 1) Adequate perfusion was maintained during increased afterload.
Conclusion
An axial flow VAD can restore normal hemodynamics and cardiac output when used as a pulmonary pump in a Fontan circulation. A VAD can rescue a failing Fontan as a bridge to transplant or recovery.
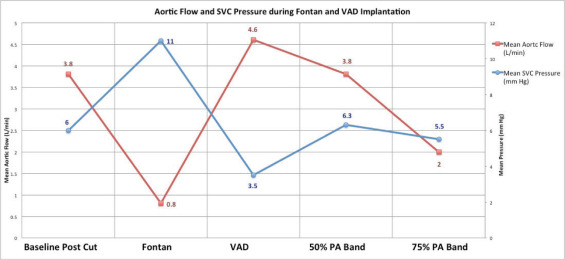
SYSTEMIC RAPAMYCIN TO PREVENT IN-STENT STENOSIS IN PERIPHERAL PULMONARY ARTERIAL DISEASE: EARLY CLINICAL EXPERIENCE
Author links open overlay panelAnnaHallbergsonJamesLockAudreyMarshall
Boston Children’s Hospital, Boston, MA, USA
Background
Patients with peripheral pulmonary stenosis (PPS) are at risk of right ventricular (RV) failure, arrhythmias, and sudden death as a result of extreme pressure load imposed by diffuse anatomic obstruction of the pulmonary vasculature. PPS can be managed surgically and by transcatheter angioplasty and stent placement which acutely can relieve obstructions, but they often recur. Approximately 1/3 of PPS patients with arteriopathies and/or Tetralogy of Fallot (TOF) develop in-stent stenosis (ISS) with subsequent stent obstruction. Supported by literature showing that local or systemic rapamycin reduces ISS in adult coronary arteriesand a dosing and safety profile established in the pediatric transplant population, we have used oral rapamycin to reduce recurrence of pulmonary artery (PA) obstructions due to ISS.
Methods
We have treated 8 patients (1.5-16 years) with severe PPS due to Williams or Alagille syndrome and/or TOF. All patients had ISS and either RV hypertension, pulmonary blood flow maldistribution, and/or segmental pulmonary hypertension. Monthly labs were monitored and follow-up catheterization was performed when clinically indicated, typically within 6 months.
Results
All 8 treated patients achieved targeted systemic levels of rapamycin (6-10 ng/mL). Two patients experienced possibly drug-related adverse events (diarrhea and a gastrointestinal bleed related to an indwelling feeding tube). Five patients treated with short-term (1-3 mo) rapamycin have shown at least mild angiographic ISS improvement. The child with the longest (27 mo) follow-up has severe Williams arteriopathy. She has experienced marked reduction in ISS which correlated temporally with initiation of rapamycin, her baseline RV pressure has decreased from 150% to 60 % of systemic, and her RV function has normalized. Prior to rapamycin therapy she developed recurrent fatigue and tachypnea and required catheterizations every 3-4 mo due to ISS, while she is now asymptomatic at 1 year after catheterization.
Conclusions
This initial clinical experience suggests that systemic rapamycin may provide a novel and safe medical approach to reduce ISS following PA stent placement.
PHARMACOKINETICS AND PHARMACODYNAMICS OF TOLVAPTAN IN CHILDREN WITH CONGENITAL HEART DISEASE AND WATER RETENTION RESISTANT TO CONVENTIONAL DIURETICS
Author links open overlay panelMikikoShimizuTakeshiMiyamotoHirokiMoriTetsukoIshiiToshioNakanishi
Tokyo Women’s Medical University, Tokyo, Japan, Japan
Background
Tolvaptan has been used to adjust hyponatremia, and to increase urination in adult heart failure. However, little is known about its safety and efficacy in small children. No pharmacokinetics data is available in children with congenital heart disease (CHD). Purpose of this study was to clarify the pharmacokinetics and pharmacodynamics of tolvaptan in children with CHD.
Methods
Single arm and single dose prospective study was carried out. Patients younger than 10 years old, and who had water retention, which was difficult to control with conventional diuretic therapies were recruited. Pharmacokinetic data was obtained every 2 hours for 12 hours and at 24hours of tolvaptan administration (0.15mg/kg), and pharmacodynamics data including urine output, urine and serum sodium concentration (Na) and osmolality were obtained during the first week of tolvaptan administration.
Results
There were 7 patients who completed the study. The mean age and body weight was 29.6 month (0-146month) and 9.7 kg (2.4-29.8kg). Three of 7 patients had single ventriclephysiology. The maximum plasma concentration of tolvaptan was 41.1±33.7ng/ml, time to reach the maximum plasma concentration was 3.1± 2.3hours, and terminal phase elimination half life was 3.5±1.5 hours. Urine output was increased from 4.5ml/kg/h to 7.1 ±1.5ml/kg/h at 4 hours (p=0.04, paired t-test), and urine osmolality was reduced from 331±150 mOsm to 197±40 mOsm (paired t-test, p=0.03) at 4 hours. Serum Na was unchanged, but urine Na tended to be reduced from 72±54 to 34±25 mEq/L at 4-8 hours after tolvaptan administration. (p=0.06, paired t-test) There was no creatinine, AST and ALT changes during the study period.
Conclusions
Pharmacokinetic data was obtained in patients with CHD for the first time. Tolvaptan was safe and effective to prevent Na excretion, and to increase urination in small children with CHD.
EFFECTS OF SYSTOLIC LOAD AND IGF1 ON COLLAGEN CONTENT OF NEONATAL LAMB MYOCARDIUM
Author links open overlay panelNaineshGandhiSamanthaLoueyGeorgeGiraudSonnetJonker
Oregon Health and Science University, Portland, OR, USA
Background
Congenital heart defects can impose a variety of maladaptive changes in heart development, of which one is an alteration in the amount of extracellular collagen deposited. Children with aortic coarctation have been found to have high procollagen levels, which may lead to adverse changes in ventricular composition, stiffness, and performance throughout life. Insulin like growth factor 1 (IGF1) has been shown to reduce myocardial collagen deposition. In this study, we hypothesized that administration of IGF1 in the early neonatal period would reduce collagen deposition, while elevated systolic arterial pressure would increase it, compared to control lambs.
Methods
3 groups of lambs were surgically instrumented at 7 days after birth with indwelling arterial and venous catheters, and an aortic occluder just below the ligamentum arteriosum. After a 4 day recovery period, pressures were measured daily from 11-18 days of age. The 3 groups were: 1) Control, 2) Load, in which the aortic occluder was progressively inflated, and 3) IGF1, in which the IGF1 analog LR3 was given ∼0.6mg IV twice a day. At the end of the experimental period, the hearts were arrested in diastole and fixed with buffered formaldehyde. Sections of myocardium were stained with Masson’s Trichrome. Microscopic morphometric analysis using a point counting technique was done to determine myocyte and collagen quantities.
Results
Aortic pressure increased progressively in the Load group, and was 35mmHg greater than in Control and IGF1 groups on the final day. Heart weight to body weight ratio (g/kg) was greater in Load (8.9±1.1) and IGF1 (7.1±0.9) groups compared to Control (6.4±0.5). Histological analysis showed no significant differences in collagen and connective tissue content between Load (12.4±3.7%), IGF (11.9±4.8%) and Control (10.8±3.8%) groups. No differences were appreciated in myocyte percent area between groups.
Conclusions
Contrary to our hypothesis, neither increased systolic arterial load nor IGF1 treatment in the early neonatal sheep altered cardiac collagen content compared to controls. We speculate that the greater heart weight was due to cardiac myocyte enlargement in the Load and IGF1 groups.
QUANTITATIVE EVALUATION OF VENTRICULAR WORKLOAD IN INFANTS WITH VENTRICULAR SEPTAL DEFECT: ENERGY LOSS ESTIMATION USING ECHOCARDIOGRAPHY VECTOR FLOW MAPPING
Author links open overlay panelTakashiHondaKeiichiItataniAtsushiKitagawaKagamiMiyajiMasahiroIshii
Kitasato University School of Medicine, Kanagawa, Japan
Background
In infants with ventricular septal defect (VSD), volume overload based on the left-right shunt has been considered to influence the ventricular workload; however, the extent of the workload has never been evaluated quantitatively. Echocardiography Vector Flow Mapping (VFM) enabled calculation of energy loss (EL), which is considered to be caused by inefficient flow. In the present study, we examined the relationship between ventricular EL and cardiac function parameters, and revealed the impact of volume overload on the ventricle.
Methods
We measured energy loss in the left ventricle using echocardiography VFM in 14 infants with VSD (Figure). We also performed catheterization measuring pulmonary to systemic blood flow ratio (Qp/Qs), pulmonary vascular resistance (Rp), systemic vascular resistance (Rs), pulmonary arterial pressure (PAP), systolic arterial pressure (SAP), and brain natriuretic peptide (BNP).
Results
The peak value of EL in the diastolic phase (ELD) significantly correlated with Qp/Qs, Rp/Rs and PAP/SAP (r = 0.706, 0.712 and 0.846, respectively). ELD also has strong correlation with BNP (r= 0.848). The ELD-BNP curve had an inflection point at 0.6mW/m, which corresponded to Qp/Qs 1.7.
Conclusions
ELD was considered to be a sensitive parameter which reflects ventricular workload. The ELD-BNP curve indicated the possibility that Qp/Qs 1.7 is the turning point at which ventricular overload drastically increases in infants with VSD.
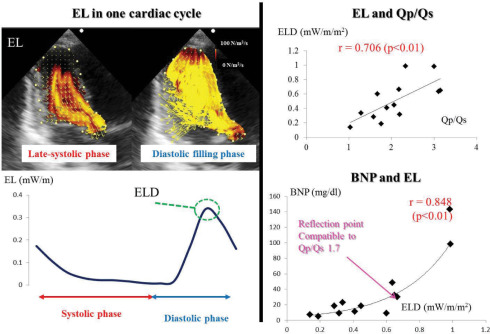
TISSUE DOPPLER IMAGING MEASURES CORRELATE POORLY WITH LEFT VENTRICULAR FILLING PRESSURES IN PEDIATRIC CARDIOMYOPATHY
Author links open overlay panelDavidEzonShirazMaskatiaWilliamDreyerAamirJeewaSusanDenfield
Baylor College of Medicine, Texas Children’s Hospital, Houston, TX, USA
Background
Tissue Doppler Imaging (TDI) measures have been shown in adults to correlate with left ventricular filling pressures (LVFP) and outcome, but data in children are less clear. This study assesses the degree with which the mitral valve (MV) lateral and septal E/E’ correlate to LVFP in pediatric patients with cardiomyopathy (CM).
Methods
We performed a retrospective review of patients ≤18 years old with dilated, hypertrophic, restrictive, or left ventricular non-compaction (LVNC) CM, who from 2003 to 2013 underwent cardiac catheterization within 3 months of an echocardiogram without interval clinical changes. Patients with hemodynamically significant comorbidities were excluded. LVFP was determined by the left ventricular end-diastolic, left atrial, or pulmonary capillary wedge pressure. MV inflow velocities and TDI lateral and medial velocities were measured by echocardiogram. Spearman correlation coefficients were calculated. A subgroup analysiswas performed for patients with either hypertrophic or restrictive CM.
Results
Thirty-eight patients met the inclusion criteria; median age 8.6 years (0.5-18). Dilated CM accounted for 24%, hypertrophic CM for 10%, restrictive CM for 29%, LVNC for 13%, and a mixed phenotype for 24%. LVFP was abnormal (≥10mmHg) in 92%. The median LVFP was 19mmHg (1-37). The median MV lateral E/E’ was 8 (2.4-18.5, n=36), while the median MV septal E/E’ was 11 (0.6-41, n=35). The median MV E/A ratio was 1.8 (0.7-6.3, n=29). Only 17% of patients had an abnormal MV E/A ratio. LVFP did not correlate with MV lateral E/E’ (r=0.05, p=0.76) or septal E/E’ (r=0.19, p=0.26), but did show a weak correlation to the MV E/A ratio (r=0.59, p=0.01). The subgroup analysis of hypertrophic and restrictive CM did not demonstrate improved correlations.
Conclusion
Non-invasive estimates of diastolic function, including TDI, were poor surrogates for LVFP in children with cardiomyopathy. While MV E/A ratio did show a weak correlation with LVFP, the majority of the MV E/A measurements were normal despite abnormal LVFP, likely representing pseudo-normalization. Larger studies are needed to confirm these findings.
OPTICAL COHERENCE TOMOGRAPHY (OCT) IN THE YOUTH FOLLOWING KAWASAKI DISEASE: A SINGLE INSTITUTION SERIES
Author links open overlay panelNagib S.DahdahAnneFournierMohamedBakloulJean-BernardSellyRoseChami
CHU Sainte-Justine, Montreal, Canada
Background
Coronary artery aneurysms (CAA) are serious complications of Kawasaki disease (KD). Current evidenced based therapy is limited to anticoagulation for cases with large CAA. Otherwise therapeutic choices remain unsupported.
Methods
To better understand luminal and coronary wall modifications following KD, we performed intracoronary imaging using OCT in patients with CAA.
Results
Cases were 11 KD patients scheduled for routine angiography follow-up between March and September 2013. KD diagnosis was at 3.8±3.1 yo, with current investigation 8.4±5.5 years later at 12.2±6.4 yo; median weight 32Kg (17-125). Giant CAA was present in 10/11 cases, and former isolated myocardial dysfunction (immune carditis) in 1/11. Besides the size of the giant CAA, outstanding findings were intimal hyperplasia in all CAA cases versus normal intima in the myocarditis patient. Intimal hyperplasia was prominent at the sites of regressed CAA or adjacent to persistent CAA (380±170um, v.s. 76±11um in normal segments). The media was not identifiable in 4/10 CAA, often replaced by a layer of patchy or circumferential fibrosis and calcification. Intimal hyperplasia was also a striking feature in segments with apparent normal taper and size on selective angiography, segments which were previously documented to be aneurismal. In one case, a vasospasm occurred at the site of a former CAA where intimal hyperplasia was subsequently recorded. Bridging myocardium was recorded in the only case free of CAA, an incidental finding. In two cases with previously implanted stents, the neo-intima was easily identified, measuring 50-90um. Interestingly, we were able a post-mortem OCT on the heart of a patient who succumbed very early following the diagnosis of KD. Prominent intimal hyerplasia was diffusely present, with preserved media. Microscopic pathology correlation was possible in this case, including the identification of the lamina elastica interna and externa.
Conclusions
This 1st pediatric OCT series offers new insight on structural CAA changes following KD. Despite size regression and normal angio appearance, the intima/media layers may be dramatically affected, including scarring and calcification.
NOVEL APPLICATION OF VIRTUAL 3D MODELS DERIVED FROM CARDIAC CT AND MRI TO ASSESS CANDIDACY FOR TWO VENTRICLE REPAIR IN PATIENTS WITH COMPLEX CONOTRUNCAL DEFECTS
Author links open overlay panelKanwal M.FarooqiSantoshUppuShubhikaSrivastavaIraParnessKhanhNguyenJamesNielsen
Mount Sinai Medical Center, New York, NY, USA
Background
Complex ventriculo-arterial relationships in patients with conotruncal defects often render it difficult to plan baffling of one outflow tract without resulting in obstruction of the other. We hypothesized that constructing a 3D virtual model would allow more informed preoperative planning.
Methods
Virtual 3D models were generated from either cardiac CT or MRI using Mimics, 3- Matic and Meshlab software. Patients were chosen for their complexity of intracardiac anatomy and need for better delineation of potential baffle pathways with avoidance of outflow tract obstruction.
Results
Three models, from CT and MRI’s, were generated from patients with complex double outlet right ventricle (DORV) anatomy. The path from each ventricle to a respective outflow tract was visualized clearly in all patients, as were structures such as conal septum, which may contribute to outflow tract obstruction. Atrioventricular (AV) valve attachments were not well delineated. A sample coronal intracardiac view of a patient with DORV {S, L, A} subpulmonary ventricular septal defect in dextrocardia is shown in Figure1.
Conclusion
Construction of virtual 3D models in patients with complex conotruncal defects allows for more precise preoperative planning. Correlation with echocardiography is needed to delineate AV valve attachments.

ASSOCIATED EXTRACARDIAC MALFORMATIONS IN THE CONGENITAL HEART DISEASE POPULATION: CURRENT ESTIMATES AND TEMPORAL VARIATION IN PREVALENCE
Author links open overlay panelAlexEgbeSantoshUppuSimonLeeHoDeborahShubhikaSrivastava
Mount Sinai Medical Center, New York, NY, USA
Background
Previous studies established association between congenital heart disease (CHD) and certain extracardiac congenital malformations (ECM). We hypothesized that prenatal diagnosis and termination of pregnancy for fetal anomalies (TOPFA) altered prevalence of ECM rendering previous estimates obsolete.
Methods
We reviewed the Nationwide Inpatient Sample (NIS) database from 1998-2008 and compared prevalence of ECM among live births with CHD diagnosis (case) and live births without CHD diagnosis (control). We then selected 56 ECM and 17 CHD diagnoses for sub-analysis. Longitudinal analysis was performed to determine temporal variation of ECM prevalence in the CHD population.
Results
Our cohort consisted of 97,154 and 12,078,482 subjects in the case and control groups respectively. In the CHD population, prevalence of non-syndromic congenital malformation (NSCM), genetic syndrome (GS), and overall extracardiac congenital malformation (ECM) were 11.4%, 2.2%, and 13.6% respectively. In the control group, prevalence of NSCM, GS, and ECM were 6.7%, 0.3%, and 7.0% respectively. NSCM (OR: 1.8 CI: 1.7-1.8), GS (OR 2.5 CI 2.4-2.6) and overall ECM (OR: 2.0 CI: 2.0-2.1) were strongly associated with CHD. Prevalence of GS and multiple CM decreased significantly over the study period.
Conclusion
This is the largest and most comprehensive population-based study showing strong association between CHD and ECM. Decreased prevalence of associated GS and multiple CM may be due to effect of TOPFA.
TABLE 1
| ECD | AV dx | PV dx | TOF | TRUNCUS | AAA | ALL CHD | |
| Cleft Lip/Palate | NS | NS | NS | 1.5 (1.1–1.8) | 1.4 (1.1–2.1) | 1.8 (1.6–2.2) | 2.9 (2.7–3.1) |
| Laryngotracheal | 3.4 (3.1–3.9) | NS | NS | 1.4 (1.1–1.9) | NS | NS | 1.8 (1.6–2.2) |
| TEF/Esophageal | 2.9 (2.1–4.2) | NS | 1.8 (1.5–2.1) | NS | NS | NS | 1.6 (1.1–2.3) |
| Spina Bifida/NTD | NS | 0.7 (0.6–0.9) | NS | NS | NS | NS | 0.7 (0.3–0.9) |
| Renal Dysplasia | 1.8 (1.2–2.7) | NS | NS | 1.5 (1.2–1.8) | NS | NS | 1.7 (1.4–2.0) |
| Genital Anomaly | 2.4 (2.1–2.7) | 1.4 (1.1–1.7) | 1.9 (1.1–2.4) | NS | NS | NS | 1.4 (1.1–1.7) |
| Hirschsprung dx | NS | NS | NS | NS | NS | NS | 0.8 (0.7–0.9) |
| Heterotaxy | 2.8 (2.5–3.2) | NS | 1.7 (1.3–2.1) | 1.8 (1.2–2.7) | NS | NS | 3.6 (3.3–3.9) |
| Limb anomaly | 0.7 (0.4–0.9) | NS | NS | NS | NS | NS | 0.8 (0.7–0.9) |
| NS-CM | 2.8 (2.1–4.0) | NS | 1.9 (1.3–2.4) | 1.7 (1.2–2.5) | NS | NS | 1.8 (1.7–1.8) |
| Down | 6.8 (5.5–7.2) | NS | 1.7 (1.3–2.1) | 3.8 (3.2–4.7) | 1.4 (1.1–1.7) | NS | 3.9 (3.7–4.1) |
| Patau | 2.4 (2.0–2.8) | NS | NS | 1.7 (1.1–2.6) | NS | NS | 2.4 (2.1–2.7) |
| Edward | NS | NS | NS | NS | NS | 1.5 (1.2–2.9) | 2.8 (1.6–3.8) |
| DGS/VCF | NS | 4.3 (3.5–5.1) | NS | 3.1 (2.4–3.8) | 6.1 (3.9–8.4) | NS | 4.6 (4.1–5.2) |
| Turner | NS | 2.4 (1.9–2.8) | NS | NS | NS | 3.6 (3.2–3.9) | 1.7 (1.1–2.4) |
| ALL GS | 5.4 (4.7–6.1) | NS | 1.7 (2.1–2.7) | 2.4 (2.1–2.7) | 1.6 (1.2–2.0) | 1.9 (1.6–2.5) | 2.5 (2.4–2.6) |
ECM: Extracardiac congenital malformation; GS: Genetic syndrome NS-CM: Non-syndromic congenital malformation; MCM: Multiple congenital malformations; ECD: Endocardial cushion defect; AV dx: Aortic valve disease: PV dx: Pulmonary valve disease; Dx: disease; AAA: Aortic arch anomaly; DGS: DiGeorge syndrome; NS: Not statistically significant
DOES GENOTYPE PREDICT AGE OF ONSET OF CARDIOMYOPATHY IN PATIENTS WITH DUCHENNE MUSCULAR DYSTROPHY?
Author links open overlay panelCharlotteVan DornMichaelPuchalskiHsin-YiWengRussellButterfieldStevenBleylRichardWilliams
University of Utah, Salt Lake City, UT, USA
Background
Up to 90% of patients with Duchenne muscular dystrophy (DMD) develop cardiomyopathy(CM) during the second decade of life. Mutations in the hinge 3 portion of the dystrophin gene (exons 50-52) may be cardioprotective. We assessed the relationship between dystrophin mutation and age of onset of CM in a cohort of DMD patients.
Methods
DMD patients who had left ventricular function assessed by echo as well as genotyping between 2004-2013 were categorized into four genotypic groups: (1) exon 2-9 deletions, (2) exon 45-49 deletions, (3) exon 50-52 deletions, and (4) exon 10-44, exon 53-79 deletions. Hinge 3 (exon 50-52) and non-hinge 3 mutations were also compared. Age at onset of CM was defined as first echo with an ejection fraction of <55% and/or shortening fraction <28%. Statistical analysis was performed using Chi-square and nonparametric Kruskal-Wallis test for cross group age comparisons.
Results
Of 103 subjects with DMD, 40 had CM. Subjects without CM were younger than those with CM (10.8 ± 4.1 vs. 14.0 ± 3.1 yrs, p<0.0001). There was no difference in the age at onset of CM among the 4 genotype subgroups (p=0.97, Table). Mean age at onset of CM with hinge 3 deletions was 14.3 ± 2.9 yrs and 13.8 ± 3.3 yrs for all non-hinge 3 mutations (p=0.65).
Conclusion
In contrast to previous studies, we found hinge 3 mutations in DMD were not associated with later onset of CM. Further study of interactions between modifier genes and dystrophin mutations may provide insight into the timing of CM.
Age at Onset of Cardiomyopathy by Mutation
| Mutation | n | Mean age, years (+/− SD) | |
| Exon 2–9 deletions | 10 | 13.7 +/− 4.8 | |
| Exon 45–49 deletions | 4 | 14.3 +/− 1.0 | |
| Exon 50–52 deletions (hinge 3) | 12 | 14.3 +/− 3.3 | |
| Exon 10–44, 53–79 deletions | 14 | 13.8 +/− 2.5 | |
| p=0.97 |
HOSPITAL CHARGES FOR PEDIATRIC HEART FAILURE RELATED HOSPITALIZATIONS ADMISSIONS IN THE UNITED STATES FROM 2000 TO 2009
Author links open overlay panelDeipanjanNandiKimberlyLinMatthewO’ConnorOkanElciJeffreyKimJamieDeckerJackPriceFarhanZafarDavidMoralesSusanDenfieldWilliamDreyerJohnJefferiesJosephRossano
Cardiac Center, The Children_s Hospital of Philadelphia, Philadelphia, PA, USA
Background
Treatment of heart failure is resource intensive. However, little is known about the costs of pediatric heart failure related hospitalizations (HFRH) or how costs have changed over time. Using charges as a proxy for cost, we tested the hypothesis that pediatric HFRH costs would increase over time.
Methods
A retrospective analysis of the 2000, 2003, 2006, and 2009 Healthcare Cost and Utilization Project Kids’ Inpatient Database was performed on pediatric HFRH. This nationwide database is the largest all-payer administrative database of pediatric admissions in the US. Charges were adjusted for inflation.
Results
There were 6,478 pediatric heart failure admissions in 2000 and 9,560 in 2009. Median HFRH charges rose from $35,079 (interquartile range [IQR], $11,697-$91,357) in 2000 to $72,087 (IQR, $23,512-$179,742) in 2009 (p<0.0001). The greatest charges were incurred in patients on extracorporeal membrane oxygenation ($442,134 [IQR, $259,704-$684,806] vs $53,998 [IQR, $17,437-$136,400]) or a ventricular assist device ($462,647 [IQR, $212,083-$776,572] vs $55,151 [IQR, $17,688-$141,421]). Comorbidities, including sepsis($207,511 [IQR, $80,429-$436,263] vs $48,995 [IQR, $16,138-$121,013]), renal failure ($180,624 [IQR, $59,064-$416,706] vs $52,812 [IQR, $16,889-$132,310), stroke ($198,260 [IQR, $81,563-$438,410] vs $54,974 [IQR, $17,639-$141,111]) and respiratory failure($146,200 [IQR, $57,838-$324,518] vs $48,797 [IQR, $15,847-$123,090]), were also associated with greater charges (all p<0.0001). Comorbidities and the use of mechanical support increased over time. However, after adjusting for these factors, demographics, and length of stay, later calendar year remained significantly associated with greater charges (p<0.0001).
Conclusions
From 2000 to 2009 there has been an almost two-fold increase in pediatric HFRH charges, after adjusting for inflation. Although major comorbidities and use of mechanical support account for some of this increase, later calendar year remained independently associated with greater charges. This study highlights the need to develop cost-effective therapies in this population.
INFECTIVE ENDOCARDITIS PROPHYLAXIS – CURRENT PRACTICE AMONGST PEDIATRIC CARDIOLOGISTS: ARE WE FOLLOWING 2007 GUIDELINES?
Author links open overlay panelNishant C.ShahNeilPatelRonakNaik
Penn State Hershey Children’s Hospital, Hershey, PA, USA
University of Tennassee Health Science Center, Le Bonheur Children’s Hospital, Memphis, TN, USA
Background
The indications for antibiotics prophylaxis for prevention of Infective endocarditis (IE) have been revised in 2007. A web-based, anonymous survey was conducted in 2013 to evaluate the current practice for IE prophylaxis amongst the pediatric cardiologists.
Results
Total 302 responses were received. The lesions, for which significant level of non-agreement for IE prophylaxis exist, are shown in table 1. Most cardiologists indicated no prophylaxis in cases of clinically silent PDA (97%), small muscular ventricular septal defect (VSD) (95%) and bicuspid aortic valve without valvulopathy (94%). Despite current guidelines, IE prophylaxis is not recommended in “Post Glenn/hemiFontan procedure” and “VSD repair with residual shunt” by 35% and 32% respectively. 57% do not follow 2007 IE guidelines exclusively for various reasons including conservative approach (20%), patient/family’s unwillingness (13%) and lack of clarity in 2007 guidelines (12%). Only 33% discuss the importance of dental hygiene with patients who are at risk of IE regularly.
Table 1
| Clinical scenario | IE prophylaxis recommended (%) | IE prophylaxis not recommended (%) |
| Rheumatic heart disease (more than mild degree of valvular lesion) | 53 | 47 |
| Fontan palliation without fenestration | 55 | 45 |
| Ross procedure | 45 | 55 |
| Intravenous pacemaker lead in right ventricle and small VSD | 44 | 56 |
| > mild degree of valvular lesion in single ventricle | 62 | 38 |
| Residual Aortic valve lesion post repair | 38 | 62 |
| Pulmonary valve replacement surgery in TOF | 62 | 38 |
| Cardiac transplant recipient without valvulopathy | 34 | 66 |
| Residual Mitral valve lesion post repair | 34 | 66 |
Conclusion
Substantial amount of heterogeneity persists amongst pediatric cardiologists in recommending IE prophylaxis for certain cardiac lesions even after six years post new guidelines. More than half participants don’t follow 2007 guidelines exclusively in their practice. Proper dental hygiene counseling in high risk patients for IE needs to be optimized in current practice.
AORTIC SURGERY IS ONE OF THE RISK FACTORS FOR ENHANCEMENT OF PRESSURE WAVE REFLECTION IN ADULT PATIENTS WITH CONGENITAL HEART DISEASE
Author links open overlay panelTomoakiMurakamiShojiFukuokaKazuhiroShiragaYukoSaitoKojiHigashiShigeruTatenoYasutakaKawasoeHiromichiNakajimaHiroyukiAotsukaKoichiroNiwa
Chiba Children’s Hospital, Chiba, Japan
Chiba Cardiovascular Center, Ichihara, Japan
Background
Enhancement of aortic pressure wave reflection accompanying aortic aging is one of the risk factors for cardiovascular diseases. After reconstruction of aortic arch in patients with aortic coarctation, the enhancement of aortic pressure wave reflection was reported. Based on advance of surgical procedure and medical therapy, most patients with congenital heart disease can be expected to survive into adulthood today. It means the patients are faced with problems associated with cardiovascular diseases. Therefore, we examined the risk factors for the enhancement of aortic pressure wave reflection in adult patients with congenital heart disease.
Methods
We non-invasively evaluated radial pressure augmentation index (rAI) by using HEM-9000AI (Omron Healthcare Co., Ltd., Kyoto, Japan) in 99 adult patients with congenital heart diseases (36.1 ± 14.6 years, male/female 63/36) and examined the relationship between rAI and patients’ demographic information, basic disorders, and the risk factors for hypertension. We especially analyzed the relationship between rAI and history of aortic surgeries, which were classified into two categories. One is direct aortic surgery (20 patients), and the other is systemic-to-pulmonary shunt (23 patients).
Results
The rAI was 77.1 ± 19.1%, and the significant determinants of the value were the history of systemic-pulmonary shunt (t=4.194, p<0.0001), age (t=4.091, p<0.0001), height (t=−3.580, P=0.0010) and the history of direct aortic surgery (t=2.253, p=0.027) by multiple regression analysis. The rAI was elevated in 44 patients (>1SD compared to age and gender matched control). The determinants of the elevated rAI were the history of systemic-pulmonary shunt (Odd ratio (95% CI)=21.319 (5.467-83.142), p<0.0001) and direct aortic surgery (Odd ratio (95% CI)=4.183 (1.376-12.721), p=0.012).
Conclusions
In adult patients with congenital heart disease, the history of aortic surgery is one of the risk factors for the enhancement of aortic pressure wave reflection. It is important to prevent cardiovascular diseases from early life.
PREDICTORS OF EMERGENCY DEPARTMENT VISITS AMONG ADULT CONGENITAL HEART DISEASE PATIENTS: A POPULATION-BASED ANALYSIS
Author links open overlay panelVanessaNanciJudithTherrienMohammedKaouacheDarrenMylotteArianeMarelli
McGill University Health Center, Montreal, Canada
Background
We have previously shown that adult congenital heart disease (ACHD) patients are growing in number and have high hospitalization rates. We sought to examine trends and predictors of cardiac-related emergency department (ED) visits in this population.
Methods
Using the Quebec Congenital Heart Disease (CHD) database, we examined annual ED visit rates among ACHD patients, aged 18 to 65 years old and alive, assessed yearly between January 1st 1998 and December 31st 2010. We performed a retrospective case control study (20:1 matched on age and calendar time) at the time of first ED visit, analyzing predictors within 3 years prior to the ED visit. Subgroup analyses were performed by age. Logistic regression was used to measure the strength of predictors of ED visit.
Results
The annual rate of ED visit among our ACHD patient population fluctuated between 5 to 8%. The strongest predictors of ED visits included: arrhythmia OR 2.59 (95% CI: 2.45- 2.74); heart failure OR 2.27 (95% CI: 2.12-2.43) and cardiac surgery OR 2.07 (95% CI: 1.79-2.39). Other predictors of ED visits were male sex OR 1.34 (95% CI: 1.27-1.40), pulmonary hypertension OR 1.54 (95% CI: 1.27-1.86) and severe CHD OR 1.71 (95% CI: 1.56-1.86), the latter most significant in patients 18-30 years of age.
Conclusions
Despite universal health insurance in Quebec, ACHD patients have high rates of ED utilization, the strongest predictors of which include heart failure and arrhythmia. Our findings should inform the planning of sub-specialty cardiology services aimed at reducing ED visits in this population.
THE ASSOCIATION BETWEEN SELF-REPORTED DEPRESSION AND ANXIETY SYMPTOMS WITH ALCOHOL AND TOBACCO USE IN ADULT PATIENTS WITH CONGENITAL HEART DISEASE
Author links open overlay panelMunziba TasnimKhanNancyKleinPaulaGoldbergGeorgeRuizAnithaJohn
Children’s National Medical Center, Washington, DC, USA
Background
Adult congenital heart disease (ACHD) patients (pts) have high rates of untreated depression and anxiety disorders. We evaluated the association of self-reported depression and anxiety symptoms and alcohol/tobacco use.
Methods
From 2009 to 2013, 219 ACHD pts (46% Male) completed clinical questionnaires including data regarding depression, anxiety, and substance use. Data were collected by retrospective review.
Results
Mean age was 31 + 10 years. Disease severity was: mild (20%), moderate (48%), and severe (32%). 21% of pts reported often being depressed and 33% were nervous or anxious. 14% of pts were on antidepressant/antianxiety (AD/AA) medications (meds). There was no association between age, gender or severity of disease and depression or anxiety symptoms. 61% of pts reported alcohol intake. Alcohol use was classified (Dietary Guidelines of America) as none (39%), 1-6 drinks/week (wk), (52%), or >7 drinks/wk, (9%). Pts who drank alcohol were 3x as likely to be depressed when compared to no alcohol (OR 2.89; 95% CI 1.29 to 6.51). Comparing depressed versus non-depressed pts, more pts with depression consumed > 7 drinks/wk (12% vs 7%) and 1-6 drinks/wk (67% vs 49%) than those with no alcohol intake (21% vs 44%), p = 0.03. There was no association between alcohol use and anxiety symptoms, but pts with depression symptoms were 19x more likely to report anxiety symptoms (OR 18.98 95% CI 7.12 to 50.58). There was a significant association between smoking and depression (p=0.0046). Pts who smoked were 5x more likely to report depression symptoms than nonsmokers (OR 5.17; 95% CI 1.49 to 17.87). Of pts on AD/AA meds, 57% reported no depression symptoms. Of pts who drank alcohol and reported feeling depressed, fewer pts (17%) were on AD/AA meds than pts who didn’t consume alcohol (56%). In pts reporting depression symptoms, the percentage of pts on AD/AA meds decreased with increased alcohol consumption (56% for none vs 22% for 1-6 drinks/wk and 17% for >7 drinks/wk).
Conclusion
Alcohol and tobacco use by ACHD pts are associated with increased self-reported depressive symptoms. Use of alcohol and tobacco may be a means of self-medicating for untreated depression, but further investigation is needed.
THE ADULT WITH CONGENITAL HEART DISEASE IN A CORONARY CARE UNIT: CLINICAL CHARACTERISTICS AND OUTCOME
Author links open overlay panelÁlvaroContrerasHectorGonzalez-PachecoAlexandraArias-MendozaCarlosMartinezJoseBriseñoAmadaAlvarezFrancisco AzarManzurJulioSandoval
National Institute of Cardiology Ignacio Chavez, Mexico, Mexico
Background
The increasing prevalence, complex diagnosis and management of the adult patient with congenital heart disease (ACHD), has become a new challenge in the modern practice of cardiology. Nowadays, there are more adults than pediatric patients with congenital heart disease in developed countries. According, there is a growing need of information about the clinical characteristics of this population, frequently seen in an acute coronary setting.
Objective
To analyze the demographic, clinical characteristic and the in-hospital evolution of ACHD patients admitted to the coronary care unit of our institution
Methods
Retrospective analysis of the characteristics of patients admitted to the coronary care unitwith the diagnosis ACHD between 2005 and 2012.
Results
We studied 195 patients with diagnosis of ACHD. There was a male: female ratio of 1:1.2 and the mean age was 35.9±15.9 years. Most of patient had moderate ACHD. 33% of these patients were diagnosed for the first time in the emergency room, and only 36% of the patients had been previously diagnosed and had a corrective or palliative procedure for treatment. The most frequent cause of hospitalization was heart failure (31.9%) and infection was the main trigger for heart failure (50%). Infectious endocarditis was the most frequent infectious disease and septic shock (17.9%) was the main cause of death.
Conclusion
The congenital heart disease of the adult is a complex disease with a wide spectrum of clinical presentations. In this population infections endocarditis should be always looked for as the potential cause of heart failure on admission
RARE COMPLICATION OF A RARE CORONARY ANOMALY
Author links open overlay panelRushitKanakiaTejasPatelMarcFeldman
University of Texas Health Science Center San Antonio, San Antonio, TX, USA
Background
Anomalous Left Coronary Artery from Pulmonary Artery (ALCAPA) is a rare congenital cardiac disease. Diagnosis at presentation in adults is uncommon as 90% of patients die within the first year of life without treatment. We report a unique case of newly diagnosed ALCAPA and an iatrogenic complication occurring during the diagnostic workup in an adult patient.
History
A 32-year-old Hispanic woman presented to the ER for chest pain lasting for 30 minutes that was similar to prior episodes precipitated by emotional stress. Physical exam was remarkable for morbid obesity and a BP of 150/90 mm of Hg. EKG demonstrated non-specific ST-T wave changes and Troponin I was elevated with a peak of 5.6.
Management
Right coronary angiography was performed which was concerning for ALCAPA. An attempt was made to engage the left main from pulmonary artery, which resulted in dissection of ALCAPA. Definitive surgery was deferred at the time with planned observation. Cardiac CTperformed 3 months later demonstrated ALCAPA without any evidence of residual dissection and patient subsequently underwent successful re-implantation of left main from pulmonary artery to aorta.
Discussion
The estimated incidence of ALCAPA is approximately 1 in 300,000 live births. We present an unusual case and an uncommon complication of ALCAPA dissection, which to our knowledge has not been previously reported. The above case demonstrates that cardiac CT may be a preferred non-invasive way of diagnosing ALCAPA.
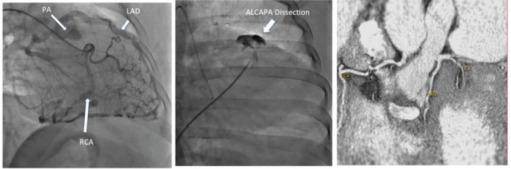
NATIONAL ADMISSIONS OF ADULTS WITH SINGLE VENTRICLE CONGENITAL HEART DISEASE: DIFFERENCES IN PEDIATRIC AND GENERAL HOSPITALS
Author links open overlay panelRonnie T.CollinsRickiFramPratikDoshiJennifer I.OnukwubeJames M.Robbins
University of Arkansas for Medical Sciences, Little Rock, AR, USA
Background
Most patients with single ventricle congenital heart disease (SV) are now expected to survive to adulthood. Medical comorbidities are common in SV.
Methods
We used nationally representative data from 1998 to 2011 Nationwide Inpatient Sample database to identify patients ≥ 18 years of age admitted to the hospital with International Classification of Diseases-9th Revision codes for a diagnosis of either hypoplastic left heart syndrome (HLHS), tricuspid atresia (TA) or common ventricle (CV). National estimates of hospitalizations at pediatric (PH) and general hospitals (GH) were calculated. Length of stay (LOS), total hospital charges and associated comorbid medical conditions were determined for each anatomic diagnosis.
Results
There were 10,237 admissions of adults with SV from 1998 to 2011. Admissions of adults with SV increased 19% from 684 in 1998 to 814 in 2011. During the study period, adult SV admissions increased 71% in GH and decreased 86% in PH. Age was greater in GH (34.1±0.5 vs 25.5±0.8)(p<0.0001). Gender distribution and LOS were similar between GH and PH. Hospital charges were higher in PH ($95,194±15,898 vs $68,416±5,389)(p=0.0491). Mortality was higher in GH (4% vs 2%)(p=0.0192). Differences in selected hospital diagnoses are shown in Table 1.
Conclusions
Admissions of adults with SV are more common in GH and are increasing. Hospitalization costs are higher in PH, but mortality is lower. Comorbid medical conditions impact hospital outcomes between PH and GH in adults with SV.
Differences in Selected Hospital Diagnoses in SV Adult Admissions to General and Pediatric Hospitals
| Diagnosis | Pediatric Hospital | General Hospital | p-value |
| (n=1,946) | (n=8,291) | ||
| Cardiovascular | 1,824 (94%) | 7,439 (90%) | 0.0145 |
| Atrial flutter | 589 (30%) | 1,878 (23%) | 0.0076 |
| Congestive heart failure | 427 (22%) | 2,715 (33%) | <0.0001 |
| Other arrhythmias | 728 (37%) | 3,630 (44%) | 0.845 |
| Coronary artery disease | 9 (0.5%) | 462 (5.6%) | <0.0001 |
| Pulmonary hypertension | 109 (5.6%) | 932 (11.2%) | 0.0796 |
| Protein-losing enteropathy | 155 (8.0%) | 365 (4.4%) | 0.0326 |
| Liver cirrhosis | 49 (2.5%) | 491 (5.9%) | 0.0047 |
OVERVIEW OF PATIENT PREFERENCE AND PERCEPTION OF CARE PROVIDED BY ADVANCED NURSE PRACTITIONERS AND ADULT CONGENITAL PHYSICIANS IN AN OUTPATIENT ADULT CONGENITAL CLINIC
Author links open overlay panelStephen C.CookVanessaKowalskiJenneHickeyReneeSchnugGeniseGreenMorganHindesTimothyMaulAliZaidi
Heart Institute, Children’s Hospital of Pittsburgh of UPMC, Pittsburgh, PA, USA
The Heart Center, Nationwide Children’s Hospital, Columbus, OH, USA
Background
Nurse practitioners (NPs) have an established role for delivering competent, cost-effective care to patients in a primary care setting. Little research has been conducted on patient preference or satisfaction in non-primary venues. We sought to compare patient satisfactionof NPs vs. physicians (MDs) in an outpatient adult congenital heart disease (CHD) clinic.
Methods
A prospective study was conducted in two outpatient adult CHD clinics to assess patient satisfaction between NPs and MDs through standardized surveys. Demographic data included CHD diagnosis, age, and NYHA functional class. All patients completed a Short-Form-12 (SF-12) to assess health status.
Results
Of the 231 patients recruited (48.5% men; median age 30 yrs (24-40), severe CHD complexity 31.5%) and seen by NP (n=99) or MD (n=132) demonstrated a statistically significant (p<0.001) moderate (rho=−0.346) inverse correlation between the SF-12 Physical Health T-score and NYHA classification. MD-managed practices had higher perceived: Receipt of Desired Information about Condition (17%), Overall Experience (14%), Quality of Experience (9%), Confidence (Trust) in Provider (9%), and Courtesy of Provider (9%). Areas without difference between NP/MD-managed practices were: Friendliness, Ability to Discuss Private Thoughts with Provider, Receipt of Safe Medical Care, Ability to Ask Questions, Feeling Rushed by Provider, Patient Comprehension of Answers, and Receipt of Information on Care of Condition. Overall, patients reported satisfaction with a NP providing care (97%), the NP able to effectively deal with illness/CHD (93%), and increased chance (95%) of patients willing to see a NP at a future visit. Only 73% had a good understanding of NP training and how a NP differed from a nurse with a stronger perception of how an NP differed from a MD (84%).
Conclusion
Patient satisfaction was high regardless of whether care was provided by physicians or nurse practitioners. However, patients appear to make distinctions in what they believe the type of care each practitioner is best at providing. Patient education regarding competence of the different health care providers may continue to improve patient satisfaction.
CONGENITAL HEART DISEASE, THE POSTGRADUATE YEARS: WHAT HAPPENS TO OUR PATIENTS AFTER THEY LEAVE PEDIATRIC CARDIOLOGY PRACTICE?
Author links open overlay panelAmandaCai
St. Christopher’s Hospital for Children, Philadelphia, PA, USA
Background
Congenital heart disease (CHD) is the most common birth defect, found in up to 75/1,000 live births.4 Currently, 90% of patients born with congenital heart defects will survive into adulthood, and the prevalence for adult congenital heart disease (ACHD) worldwide is estimated to be 13 million7 with over 1 million in the US alone.9 In the year 2000, the number of adult patients with CHD surpassed that of children.6 As the ACHD population continues to grow, an examination of the physician workforce equipped to take care of these patients and the current status of ACHD medical practice is imperative.
Methods
A Medline search, review of references cited, as well as perusal of the Centers for Disease Control and International Society for Adult Congenital Heart Disease websites were performed.
Results
The 32nd Bethesda Conference on “Care of the Adult with Congenital Heart Disease” reported that 55% of the adult population with CHD has at least “moderate” disease necessitating follow up at a specialized regional ACHD center.10 Yet, available data suggests less than half of all patients with CHD (47%) are successfully transitioned to adult care8 and a large range, 14-76%, of ACHD patients are lost to follow up after leaving pediatric cardiology practice.1,2,5,8,11-13 Challenges facing transition of care and follow up are numerous and complex. Nascency of the ACHD field is marked by lack of specialized cardiologists and regional ACHD centers. Of the 128 accredited cardiology training programs in the US, only 11 currently offer ACHD fellowship training opportunities.3 As of 2011, only 74 adult and pediatric cardiologists and approximately two dozen large regional centers in the US were identified as concentrating their practices in ACHD.14 With the recent Accreditation Council for Graduate Medical Education (ACGME) acceptance of the ACHD Training Program application in 2013, an increase in training opportunities and future board certification are expected.
Conclusions
The number of adults with congenital heart disease is growing and there is currently an inadequate workforce available to meet the evolving healthcare needs of this population.