COST COMPARISON OF TRANS-CATHETER AND OPERATIVE PULMONARY VALVE REPLACEMENT
Author links open overlay panelMichael L.O’ByrneMatthewGillespieYoavDoriJonathanRomeAndrewGlatz
The Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Background:
Clinical outcomes for trans-catheter (TC-PVR) and operative (S-PVR) replacement of the pulmonary valve are excellent. The economic cost of each method has only been compared in small series, which have not accounted for confounding variables or differences in practice between centers.
Methods:
A retrospective cohort study of children and adults undergoing PVR with age >8 years from 1/1/2011 to 12/31/2013 at 35 centers contributing data to the Pediatric Health Information Systems database was performed to measure differences in inflation-adjusted cost (derived by ratio of cost to charges from charge data) of S-PVR and TC-PVR. A propensity scoreweight-adjusted multivariable regression model was used to account for measured confounders. Secondary outcomes included in-hospital mortality, hospital length of stay, and department level charges.
Results:
A total of 2,109 pulmonary valve replacement procedures were performed in 2,097 subjects over the study period (14% trans-catheter and 86% operative). In-hospital mortality was not significantly different between S-PVR and TC-PVR (0.8% vs. 0%, p=0.24). Length of stay was shorter following TC-PVR (median: 1 day, IQR: 1-1) than following S-PVR (median: 4 days, IQR: 3-5.5 days, p<0.0001). The cost of S-PVR and TC-PVR was not significantly different (2013US$50,030 vs. 2013US$51,297; p=0.89). In a multivariate propensity-scoreadjusted model, there still was no significant difference in cost between S-PVR and TC-PVR (p=0.51). History of malignancy was associated with increased cost of pulmonary valve replacement (p=0.004), but other patient level factors including genetic syndrome, age, and cardiac diagnosis did not significantly affect cost of pulmonary valve replacement. Clinical and supply charges were greater for TC- PVR (p<0.0001) while lab, pharmacy, and other charges (all p<0.0001) were greater for S-PVR.
Conclusion:
At this time, cost of TC-PVR and S-PVR are not significantly different. Longer length of stay and associated costs of hospitalization drive the cost of S-PVR while the relatively expensive clinical and supply charges drive the cost of TC-PVR.
MULTICENTER VALIDATION OF TECHNICAL PERFORMANCE SCORE AS A QUALITY ASSESSMENT TOOL IN CONGENITAL CARDIAC SURGERY
Author links open overlay panelMeenaNathanHuaLiuStevenColanLazarosKochilasGeethaRaghuveerDavidOvermanEmileBachaO BrienJamesJames StLouisDavidKalfaBrettAndersonMarkoVezmarKimberleeGauvreauKathyJenkinsPedrodel Nido
Boston Children’s Hospital, Boston, MA, USA
University of Minnesota Children’s Hospital, Minneapolis, MN, USA
Background:
Technical Performance Score (TPS), a novel tool for assessing adequacy of repair of congenital cardiac defects based on clinical and echocardiographic data, has been validated and correlates with outcomes in single center studies. This study aims to validate TPS in a multicenter environment.
Methods:
Patients discharged between January 1 and December 31, 2011 from 5 participating centers who underwent Norwood, bidirectional Glenn (BDG), Fontan, arterial switch operation (ASO), arch repair /VSD closure (Arch/VSD), complete atrioventricular canal (CAVSD) repair, tetralogy of Fallot (TOF) repair, ventricular septal defect (VSD) closure and pulmonary valve replacement (PVR), were assigned TPS at each center. Outcomes included postoperative adverse events, length of ventilation and hospital stay, assessed using regression techniques.
Results:
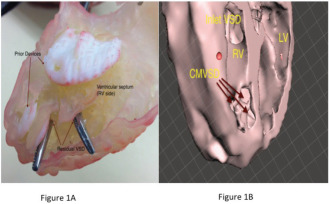
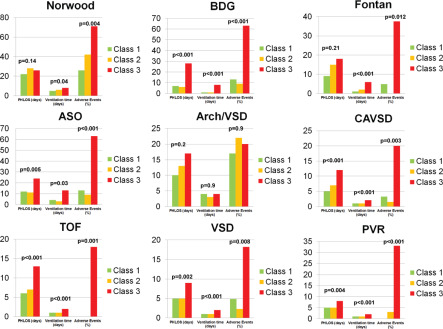
The 925 discharges included: Norwood 85, BDG 75, Fontan 97, ASO 58, Arch/VSD 58, CAVSD 135, TOF 112, VSD 163 and PVR 116. Figure1 shows that Class 3 TPS (major residua or unplanned pre discharge reintervention) had worse outcomes compared to Class 1 TPS (trivial or no residua) for all except Arch/VSD. On multivariable modeling after adjusting for age, prematurity, extracardiac anomalies, center and cardio-pulmonary bypasstime; Class 3 TPS remained associated with adverse outcomes for Norwood, BDG, Fontan, ASO, CAVSD and TOF .
Conclusion:
TPS correlates with early outcomes and may serve as a quality assessment tool in congenital heart surgery.
THE FIRST-EVER PEDIATRIC APPROPRIATE USE CRITERIA IMPLEMENTATION PROJECT: A LARGE MULTICENTER QUALITY INITIATIVE
Author links open overlay panelRituSachdevaWymanLaiJosephAllenOscarBenavidezRobertCampbellBenjaminEidemLaraGoldMichaelKellemanLeoLopezCourtney E.McCrackenKenanSternRoryWeinerElizabethWelchPamelaDouglas
Emory University School of Medicine, Atlanta, GA, USA
Background:
The first pediatric appropriate use criteria (AUC) were recently published for initial outpatient transthoracic echocardiography (TTE). We sought to determine the appropriateness of TTE performed prior to AUC release, identify any gaps and guide AUC education.
Methods:
Data were prospectively collected from patients undergoing initial outpatient TTE in 5 centers. TTE indications [Appropriate (A), May Be Appropriate (M) or Rarely Appropriate (R)] and findings (normal, incidental or abnormal) were recorded.
Results:
Of 1,634 studies ordered by 80 physicians, the most common indications were murmur, N = 481 (29%) and chest pain, N = 248 (15%). Seventy orders (4%) had indications not included in the current document. One fourth of the indications were not used. TTE findings and the top 3 indications for each rating are shown (Table). Innocent murmur, syncope and palpitations accounted for 74% of TTEs rated R. The most common abnormal findings were septal defects (n=83) and pulmonary stenosis (n=26). The Odds Ratio for abnormal findings on A or M vs R TTEs was 2.3 [95% CI (1.3-4.2)].
Conclusion:
Most TTEs ordered in pediatric cardiology clinics were appropriate. AUC ratings successfully stratified the indications based on the yield of abnormal findings, and identified the most common indications rated R. This study lays the framework for addressing current AUC gaps and designing educational interventions to improve initial pediatric TTE utilization in the outpatient setting.
| Rating N (%) | TTE findings N (%) | 3 most common indications (N) | ||
| Normal | Incidental | Abnormal | ||
| Appropriate
1139 (70%) |
922 (81%) | 66 (6%) | 151 (13%) | Murmur (358)
– With signs, symptoms or findings of CV disease (113) – Pathologic (245) Chest pain (212) Systemic disorders (169) |
| May Be Appropriate 208 (13%) | 194 (93%) | 6 (3%) | 8 (4%) | Family history (72)
Palpitations (23) Chest pain (22) |
| Rarely Appropriate 217 (13%) | 197 (90%) | 9(4%) | 11 (6%) | Murmur, innocent (111)
Syncope (28) Palpitation (21) |
| Unclassified
70 (4%) |
61 (87%) | 3 (4%) | 6 (9%) | Click (11)
Hemangiomas (7) Apnea (3) |
| Total 1634 | 1374 (84%) | 84 (5%) | 176 (11%) | |
FACTORS ASSOCIATED WITH PROCEDURAL SUCCESS AND COMPLICATIONS IN PULMONARY ARTERY STENTING: INSIGHTS FROM THE NCDR®
Author links open overlay panelMatthew J.LewisNatalieJayaramKevinKennedyJonathanGinnsMatthewCrystalAlejandroTorresJulieVincentMarlonRosenbaum
Columbia University, New York, NY, USA
Background:
Because risk factors associated with outcomes for pulmonary artery (PA) stenting remain poorly defined, we sought to determine the effect of patient and procedural characteristics on complication rates and procedural success.
Methods:
Demographic, procedural and lesion specific data was collected through the Improving Pediatric and Adult Congenital Treatment (IMPACT) registry. Two definitions of procedural success were pre-specified for patients with biventricular (BV) circulation: 1) 20% reduction in right ventricular pressure (RV) or 50% increase in PA diameter; 2) 25% reduction in RV pressure or 50% decrease in PA gradient or post procedure ratio of in-stent minimum to pre-stent distal diameter >80%. A separate definition of procedural success based on normalization of PA diameter was pre-specified for patients with single ventricle (SV) palliation. Complications were classified as life-threatening based on expert consensus.
Results:
Between 1/2011 and 1/2014, 1183 PA stenting procedures were performed at 59 institutions. 262 (22%) procedures were performed in patients with a SV. Mean age and weight were 9 (+/- 9) years and 29 (+/- 26) kg respectively. The rate of procedural success was 76% for definition 1, 86% for definition 2, and 75% for SV patients. By multivariate analysis, ostial stenosis was significantly associated with procedural success for BV patients by both definitions. No variable was associated with procedural success for SV patients. The overall complication rate was 14% with 9% of patients having a life-threatening complication. By multivariate analysis, weight <4 kg, SV, and emergency status were significantly associated with life-threatening complications. Procedure indication was not associated with procedural success or complication.
Conclusion:
In our analysis of 1183 PA stenting procedures, success was 75% across all definitions and complications were relatively common. BV patients with an ostial stenosis had a higher probability of a successful outcome. Patients who had a SV, weight <4 kg, or emergency procedure had a higher risk of having a life-threatening complication. These findings may help inform patient selection for PA stenting.
LONGITUDINAL ASSESSMENT OF SINGLE VENTRICLE PATIENTS IN THE PEDIATRIC HEART NETWORK FONTAN COHORT
Author links open overlay panelAndrew M.AtzVictorZakLynnMahonyKristinBurnsDavidGoldbergRichardWilliamsRogerBreitbartRosalindKorsinStevenColanBradley S.MarinoReneeMargossianKaitlynDanielsKarenUzarkHeatherHendersonBrianMcCrindle
Pediatric Heart Network Investigators, Medical University of South Carolina, Charleston, SC, USA
Background:
Multicenter longitudinal outcome and functional assessment data for Fontan patients surviving into adulthood are lacking.
Methods:
Current vital and cardiac transplant status data were assessed 9.4±0.4 years after the Fontan Cross-Sectional Study in 546 subjects. Maximal exercise testing, echocardiographyand B-type natriuretic peptide (BNP) analysis were performed prospectively and compared to previously measured values.
Results:
Twenty-five subjects died, 14 were transplanted, 1 had a biventricular conversion and 40 were lost to follow up. Of 466 remaining subjects, 377 (80%) were studied at 21.2± 3.5 years of age. Compared to baseline data, exercise performance and ejection fraction (EF) decreased and BNP increased. (Table) When divided into 2 equal sized subgroups by age and baseline max VO2, the annual rate of decline in % predicted max VO2 was larger in the younger vs. older cohort (mean slope = -1.03 vs. -0.47) and in those with better vs. worse baseline exercise performance (mean slope -1.31 vs. -0.19). EF decreased as a result of greater increase in end systolic volume (mean Z score increase +0.7, P=0.002) than end diastolic volume (mean Z-score increase +0.3, P=0.06).
Conclusion:
We found a substantial decrease in exercise performance with small changes in EF and BNP in this cohort followed over nearly a decade. Younger subjects and those with better initial exercise performance showed a greater rate of decline. Future interventions should focus on preserving exercise capacity.
| Subjects with Two Sets of Data (Mean±SD) | N | Baseline | Follow-up | P |
| Age (years) | 373 | 11.7±3.4 | 21.2±3.5 | |
| % predicted VO2 at anaerobic threshold | 196 | 80±25 | 72±25 | 0.002 |
| % predicted max VO2 (RER> 1.1) | 95 | 69±14 | 61±16 | <0.001 |
| % predicted max work rate (RER> 1.1) | 95 | 69±15 | 56±16 | <0.001 |
| % predicted max O2 pulse | 263 | 91±23 | 79±22 | <0.001 |
| Oxygen saturation, % | 267 | 92±5 | 93±5 | 0.9 |
| Ejection fraction, % | 236 | 58±10 | 55±10 | <0.001 |
| BNP, pg/mL | 340 | 21±25 | 43±135 | 0.002 |
RER = Respiratory Exchange Ratio >1.1 designates maximal effort
INVESTMENT IN INPATIENT FATALITY IN CONGENITAL HEART DISEASE: VARIABILITY BY LESION AND INSTITUTIONAL VOLUME
Author links open overlay panelDavid A.DanfordQuentinKarelsAyshaHussainAparnaKulkarniYunbinXiaoShelbyKutty
University of Nebraska Medical Center & Children’s Hospital and Medical Center, Omaha, NE, USA
Background:
Inpatient (inpt) care of congenital heart disease (CHD) can be complex, lengthy, and expensive. Major investments of time, financial resources, and emotional capital are very discouraging when the outcome is a fatality. We define a measure of that discouragement, the investment in inpt fatality (IIIF) as the resources expended in inpt care which the patient does not survive divided by all inpt care resources expended regardless of survival. Our purpose is to identify variations in IIIF by CHD lesion and by institutional volume.
Methods:
The Pediatric Health Information System (PHIS) database representing 47 children’s hospitals was queried for admissions of 4 CHD lesions (hypoplastic left heart syndrome (HLHS), tetralogy of Fallot (TOF), ventricular septal defect (VSD), and atrial septal defect(ASD)) among patients (pts) <21 years old during 2004-2013. Institutional volume, pt age, inpt deaths, billed charges (BC) and length of stay (LOS) were recorded. IIIF was calculated in 2 ways: (1) based on LOS and (2) based on BC.
Results:
In all, 48159 admissions (11,122 HLHS, 12,891 TOF, 14,220 VSD, 9926 ASD) were identified. There were 1520 inpt deaths (3.2%). Mortality rates were 10.3% HLHS, 2.7% TOF, 0.7% VSD, 0.3% ASD. IIIF (BC) was 21% for HLHS, 10% TOF, 4% VSD, and 3% ASD. IIIF (LOS) was 16% for HLHS, 8% TOF, 4% VSD, and 3% ASD. IIIF (BC) range by institution was 0-41% for HLHS, 0-34% TOF, 0-28% VSD, 0-45% ASD. IIIF (LOS) range by institution was 0-31% for HLHS, 0-27% TOF, 0-15% VSD, 0-26% ASD. There was no significant correlation of IIIF with institutional volume for any lesion.
Conclusion:
IIIF is highest in the most complex CHD, but is surprisingly high in simple lesions such as ASD and VSD, despite very low mortality rates. Remarkably broad variation in IIIF from one institution to another is noted in all lesions, but high IIIF is not a phenomenon peculiar to either low or high volume institutions. It is clear from this investigation that there is room for improvement in IIIF for CHD care in lesions of all complexities, at programs of all volumes. More detailed research will be required to identify specific markers for IIIF which will point to potentially beneficial changes to be made in CHD management.
DIGOXIN USE AT DISCHARGE IS ASSOCIATED WITH REDUCED INTERSTAGE MORTALITY AFTER STAGE I PALLIATION FOR SINGLE VENTRICLE HEART DISEASE
Author links open overlay panelDavid W.BrownColleenMangeotJeffreyAndersonLaura E.PetersonEileenKingStaceyLihnStevenNeishRobertBeekmanCaroleLannon
Boston Children’s Hospital, Boston, MA, USA
Background:
Interstage mortality (IM) remains significant after discharge from Stage I palliation (S1P) for single ventricle heart disease (SVD), with many deaths sudden and unexpected. We sought to determine whether digoxin use is associated with reduced IM utilizing the multicenter database of the National Pediatric Cardiology Quality Improvement Collaborative.
Methods:
From 06/2008-07/2013, 815 infants discharged from 50 surgical sites completed the interstage with Stage II palliation, transplant or IM. Those with arrhythmia during S1P hospitalization were excluded (n=256). Two analyses were performed: 1) a case:controlanalysis for patients discharged on digoxin versus not, matched for surgical site and other established risk factors for IM; 2) logistic regression with mortality as the outcome variable and propensity score included as a covariate. Variables used to develop the propensity score for treatment with digoxin included type of S1P, post-S1P ECMO use, genetic syndrome, discharge feeding route, ventricular function, tricuspid regurgitation, and aortic arch gradient; sites were grouped by number of enrolled infants in the registry per year as a surrogate for patient volume. Multiple imputation was used for missing variables.
Results:
Of 559 patients without history of arrhythmia, 121 were discharged on digoxin, and 60 (50%) matched in case:control analysis for site of care, type of S1P, post-S1P ECMO use, genetic syndrome, discharge feeding route, ventricular function, tricuspid regurgitation, and aortic arch gradient. Fishers’ exact test showed use of digoxin at discharge was associated with lower IM (0 vs. 10.6%, p=0.01). Logistic regression analysis with mortality as the outcome variable and propensity score, site size group and use of digoxin at discharge as predictor variables showed an increased risk of IM in those not discharged on digoxin (OR 2.9, p=0.005).
Conclusion:
Among SVD infants in the NPCQIC database discharged after S1P with no history of arrhythmia, use of digoxin at discharge was associated with reduced IM. Further study is warranted.
SECUNDUM ATRIAL SEPTAL DEFECT IS ASSOCIATED WITH REDUCED SURVIVAL IN ADULT MEN
Author links open overlay panelJoey MikeKuijpersTeunvan der BomAnneliekevan RielFolkertMeijboomArieVan DijkPetronellaPieperHubertVliegenMarcWaskowskyToonOomenCarlaZomerWilfredHeesenLodewijkWagenaarBarbaraMulderJolienRoos-HesselinkBertoBoumaAeilkoZwinderman
Interuniversity Cardiology Institute of the Netherlands, Utrecht, The Netherlands
Academic Medical Center, Amsterdam, The Netherlands
Background:
We investigated whether gender disparity exists in long-term outcome of adult ASD2 patients, as this might call for a gender-specific approach toward these patients.
Methods:
Patients with ASD2 as the primary defect were selected from the Dutch national registry of adult congenital heart disease patients. Using prospective data from this registry, survival stratified by gender was compared to a gender-matched general population. Differences in incidence of adverse events between genders were evaluated using logistic regression, controlling for age.
Results:
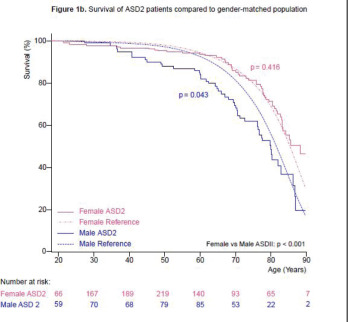
In 2241 adult patients (mean age 44.6 years, 32.3% male), 103 deaths occurred during a cumulative follow-up of 13.889 patient years. Median survival was 79.9 years for men and 88.3 years for women. Compared to a gender-matched general population, survival was lower for male, but equal for female patients (p=0.043 and p=0.416, respectively). Men had a higher risk of conduction disturbances (OR=1.38; 95% CI, 1.00-1.91) supraventricular dysrhythmias (OR=1.33; 1.05-1.67), thromboembolic cerebrovascular events (OR=1.59; 1.15-2.21) and heart failure (OR=1.87; 1.04-3.34), but a lower risk of pulmonary hypertension (OR=0.65; 0.44-0.96).
Conclusion:
In contrast to women, adult men with ASD2 have worse survival than a gender-matched general population. Men also have a greater risk of morbidity during adult life. This gender disparity in prognosis suggests the need for a gender-specific clinical approach toward these patients.
WHOLE EXOME SEQUENCING IN CONGENITAL HEART DISEASE REVEALS VARIANTS IN LEFT-RIGHT PATTERNING GENES PREVIOUSLY ASSOCIATED WITH HETEROTAXY SYNDROME AND PRIMARY CILIARY DYSKINESIA
Author links open overlay panelKeila N.LopezAlexander H.LiNeilHanchardMahshidAzamianSeemaLalaniHeatherDickersonJimLupskiDanielPennyCharlesFraserJamesMartinEricBoerwinkleJohn W.Belmont
Baylor College of Medicine, Houston, TX, USA
University of Texas Health Science Center, Houston, TX, USA
Background:
Heterotaxy syndrome (HTX) is a constellation of defects defined primarily by abnormal lateralization of thoracic and abdominal organs across the left-right axis of the body of either the polyspenia or asplenia type, and often involving complex congenital heart disease(CHD). Based on rare isolated cases, mutations in the same gene and even the same allele of a gene may cause either type of HTX. It is not known how genes associated with HTX are associated with other types of CHD.
Methods:
Potential left right patterning defect cases were identified through a retrospective chart review of pre-surgical echocardiograms. Whole exome sequencing was performed on these samples at the Baylor-Hopkins Center for Mendelian Genomics. We stratified variants/genes into three categories: 1) loss-of-function (LOF) variants in known HTX genes; 2) homozygous or compound heterozygous mutations in genes known to cause primary ciliary dyskinesia (PCD); and 3) LOF variants in novel genes involved in left-right signaling pathways (NOTCH, NODAL and SHH). In category 3 genes, no LOF variants were found in control exome data (n=15,000).
Results:
We ascertained 332 CHD cases with potential left right patterning defects. Of those cases, 32 were found to have candidate pathogenic variants in one of the three categories. For those with HTX, five cases had category 1 and five cases had category 2 variants. Twenty-two non-HTX cases included CHDs with dextrocardia, juxtaposition of the atrial appendages, transposition of the great arteries, double inlet left ventricle, and double outlet right ventricle. Of these, 15 had category 2 variants, four had category 1 variants (previously associated with HTX genes), and three had category 3 variants (involving potential novel gene associations).
Conclusion:
Our results indicate that early disturbances in embryonic left-right patterning may lead to both classic HTX and a wider array of cardiac defects. In our study, only a small fraction of HTX cases bear candidate mutations in previously identified genes. Ongoing analyses include targeted re-sequencing of candidate variants within cases and direct family members to determine mode of inheritance and to validate genotypes.
CHARACTERIZING THE ANGIOGENIC ACTIVITY OF SINGLE VENTRICLE PATIENTS WITH AORTOPULMONARY COLLATERAL VESSELS
Author links open overlay panelNefthiSandeepJoshuaKanterLindaLeatherburyYoh-sukeMukouyama
Children’s National Health System, Washington, DC, USA
National Institutes of Health, Bethesda, MD, USA
Background:
Single ventricle (SV) congenital heart disease patients often form abnormal aortopulmonary collateral (APC) blood vessels via an unclear mechanism. Prior studies separately showed elevated hypoxia-inducible angiogenic factor levels such as vascular endothelial growth factor (VEGF) in SV serum and the ability of SV serum to stimulate endothelial cells to form simple tubules in vitro. However, no study has correlated angiogenic factor levels with in vitro activity and angiography. We examined whether SV patients with APCs have increased angiogenic factors that can stimulate endothelial sprouting in vitro.
Methods:
In single ventricle (n=17) and biventricular acyanotic control patients (n=13), VEGF and other plasma angiogenic factor levels were measured in femoral venous and arterial blood at cardiac catheterization. To assess plasma angiogenic activity, we developed a 3-D in vitroendothelial cell sprouting assay that recapitulates angiogenic sprouting, a possible key step in APC formation.
Results:
Angiogenic activity of SV patients was not significantly greater than controls. While some SV patients had elevated plasma VEGF, average levels were not significantly different from controls. SV plasma also did not stimulate cells to form significantly more sprouts than control plasma. Plasma factor levels and the number of cell sprouts formed correlated poorly with APC severity. However, arterial soluble fms-like tyrosine kinase-1 (sFlt-1), a regulatory VEGF receptor, was significantly elevated in SV patients (550±94 pg/mL) versus controls (238±32 pg/mL) (p < 0.01).
Conclusion:
Our ongoing study is the first to simultaneously correlate angiography with plasma angiogenic factor levels and in vitro angiogenic activity in SV patients with APCs. Surprisingly, preliminary data show that SV patients with APCs have a wide range of factor levels and angiogenic activity that correlates poorly with APC severity suggesting a complex mechanism of angiogenesis. Arterial sFlt-1 is elevated in SV patients and may have a role in APC formation that requires further investigation.
IBUPROFEN PROPHYLAXIS IS ASSOCIATED WITH IMPROVED HOMOGRAFT LONGEVITY IN THE RIGHT VENTRICULAR OUTFLOW TRACT IN CHILDREN
Author links open overlay panelFrances ChenTravelliAndrew S.HaynesPamela M.FaireVaughn A.StarnesRam KumarSubramanyanWinfieldWellsJondavidMenteer
Children’s Hospital Los Angeles, Los Angeles, CA, USA
Background:
Inflammatory response has been implicated in homograft failure in children, and ibuprofen has been postulated to mitigate this effect. We investigated the effect of a 3-month postoperative ibuprofen regimen on durability of homografts in the right ventricular outflow tract (RVOT) in our institution.
Methods:
We began using prophylactic ibuprofen (5 mg/kg/dose 3 times daily for 3 mos) in 2008. We retrospectively reviewed our surgical database for patients 4 yrs prior to and 4 yrs after the introduction of this policy. Patients without follow-up after living to discharge were excluded from analysis. Data was analyzed with Wilcoxon analysis of Kaplan Meier curves, and significance is defined as p<0.05.
Results:
174 patients met inclusion criteria. 103 patients received ibuprofen by intent-to-treat analysis and 71 did not. There were no statistically significant differences between groups’ age, gender, body surface area, conduit type and conduit size. Median follow-up was 19.7 months (interquartile range 11.4 – 46.2 mos) for patients who received ibuprofen, and 57.1 months (interquartile range 13.2 – 92.3 mos) for those who did not (p<0.05). Conduit failure (defined as need for conduit exchange) occurred in 7%, 15%, and 18% at 1, 3, and 5 years postoperatively for patients receiving ibuprofen; compared with 10%, 31%, and 33% at 1, 3, and 5 years for those who did not receive ibuprofen (p=0.03). Grafts placed orthotopically (i.e. Ross procedures) lasted longer than heterotopically placed grafts (e.g. Rastelli or tetralogy of Fallot repairs), with 4% failure rate vs 27% failure rate at 3 years (p=0.009). Aortic homografts had inferior durability (failure rate 32%, 52% at 3 and 5 years) compared with pulmonary homografts (failure rate 19% and 21% at 3 and 5 years) (p=0.005).
Conclusion:
A prophylactic regimen using ibuprofen in the early postoperative period after homograftplacement in the RVOT may prolong conduit survival.
PACEMAKER IMPLANTATION IN PEDIATRIC HEART TRANSPLANT RECIPIENTS IS PREDICTED BY BIATRIAL ANASTOMOSIS AND DONOR AGE BUT DOES NOT AFFECT SURVIVAL
Author links open overlay panelIqbalEl-AssaadSadeerAl-KindiGuilhermeOliveiraBruceWilkoffGerardBoylePeterAziz
Cleveland Clinic Children’s, Cleveland, OH, USA
University Hospitals Case Medical Center, Cleveland, OH, USA
Background:
Bradyarrhythmia is a major complication after heart transplantation and may require pacemaker implantation. Little is known about the incidence and determinants of this complication in the pediatric population. This study sought to investigate the incidence, predictors and outcomes of permanent pacemaker (PPM) implantation in pediatric heart transplant recipients.
Methods:
We queried the United Network for Organ Sharing (UNOS) database for all pediatric (age <21) patients who received heart transplants (1994-2013). Regression models are reported for prediction of PPM implantation. Survival analysis was performed using Kaplan-Meier method.
Results:
6739 mostly Caucasian (59.0%) males (55.9%) with median age 7.0 years were analyzed, of which 91 (1.4%) required post-transplant PPM implantation. PPM use decreased over the study period from 1.7% (1994-2003) to 1.0% (2004-2013), (p=0.014). Compared with the non-PPM group, PPM group recipients were more likely to be older (14.0 vs. 7.0 years, p<0.001), had used antiarrhythmics at listing (34.5% vs. 19.3%, p=0.007), had implantable cardioverter defibrillator at listing (15.3% vs. 8.5%, p=0.032), and had undergone biatrial anastomosis (69.2% vs. 52.7%, p=0.002). In a multivariate model, PPM implantation was predicted by higher donor age (HR 1.026, p=0.029) and biatrial anastomosis (HR 1.857, p=0.022). PPM recipients were at increased risk for post-transplant infection (44.4% vs. 25.3%, p=0.001) and post-transplant dialysis (14.3% vs. 6.7%, p=0.01). Over a mean follow-up of 7.8 years, age-adjusted graft survival did not differ between the two groups (p=0.66).
Conclusion:
Pacemaker implantation in pediatric heart transplant recipients is rare and has decreased over time. PPM use is predicted by biatrial anastomosis and higher donor age and, although associated with higher risk of infections and dialysis, does not adversely impact survival.
ASSOCIATION OF POST-NORWOOD ARRHYTHMIA WITH SUBSEQUENT OUTCOMES IN THE SINGLE VENTRICLE RECONSTRUCTION TRIAL
Author links open overlay panelMatthewOsterShanChenEricGerstenbergerYanivBar-CohenMatthewBrothersNicoleCainStevenColanRichardCzosekJamieDeckerDavidGamboaSalimIdrissJoelKirshMartinLaPageRichardOhyeElizabethRadojewskiMaullyShahEricSilverAnoopSinghJoelTempleJohnTriedmanJonathanKaltman
Children’s Healtchare of Atlanta, Emory University School of Medicine, Atlanta, GA, USA
Background:
Arrhythmias are common following the Norwood procedure for single ventricle congenital heart disease, but their clinical impact is unclear. The purpose of this study was to determine the associations of post-Norwood tachyarrhythmias and heart block with short- and long-term outcomes.
Methods:
We analyzed data from the multicenter Pediatric Heart Network Single VentricleReconstruction trial for infants undergoing a Norwood procedure from 2005-2008. The study variables were any documented tachyarrhythmia (supraventricular tachycardia, junctional ectopic tachycardia, atrial flutter, ventricular tachycardia, or atrial fibrillation) or heart block(2nd or 3rd degree only) requiring medication or treatment during the postoperative stay. The outcomes were postoperative length of stay, total ventilation time, and transplant-free survival (30-day, interstage, and 1-year). Subjects receiving a permanent pacemaker in the postoperative period were excluded (n=5). We performed multivariable linear regression for length of stay and ventilation time and multivariable logistic regression and Cox proportional hazards for survival. Covariates included relevant demographic, operative, institutional, and clinical factors.
Results:
Of 524 subjects, 108 (21%) had at least one documented tachyarrhythmia, and 16 (3.1%) had at least one episode of 2nd or 3rd degree heart block. Compared to subjects without arrhythmia, those with tachyarrhythmia or heart block had longer length of stay (48 days and 57 days vs. 31 days, respectively, both p<0.001) and ventilation time (27 days and 27 days vs. 11 days, both p<0.001), but had no difference in 30-day or 1-year survival. For interstage mortality, there was no association with tachyarrhythmia, but there was an association with heart block (adjusted HR 4.2 [95% CI 1.04-16.91], p=0.044).
Conclusion:
Post-Norwood arrhythmias are associated with increased ventilation time and increased length of hospital stay, and 2nd or 3rd degree heart block are also associated with increased interstage mortality. Further studies are needed to determine strategies that may modify these outcomes.
ULTRASOUND-INDUCED CHANGES IN DEPOLARIZATION OF NEONATAL VENTRICULAR CARDIOMYOCYTES
Author links open overlay panelNatashaMehtaRandall A.LeeYouhanSunnyChrisBawiecStevenKutalekPeter A.LewinAndrewKohut
Drexel University College of Medicine, Philadelphia, PA, USA
School of Biomedical Engineering, Science & Health System, Drexel University, Philadelphia, PA, USA
Background:
Ultrasound interacts with tissue through either thermal or non-thermal physical mechanisms. Radiation force has been shown to stimulate cardiac and neural tissue in vivo. Ultrasound might hold clinical potential as a noninvasive therapeutic tool via specific bioeffects on cardiomyocytes. This study aims to assess the effect of ultrasound on cardiomyocyte depolarization in a tissue culture model.
Methods:
Cardiomyocytes were isolated from neonatal rat ventricular tissue and plated on microelectrode arrays to record action potentials (AP) and analyze depolarization patterns. A custom 2.5 MHz unfocused ultrasound transducer was directed at cardiomyocytes in a tissue culture model. A function generator, with an amplified signal +50 dB, delivered acoustic energy at variable settings of 0.1, 0.3, 0.5 and 1.0 Vpp, pulse durations of 2, 5 and 10 ms, and burst periods of 100, 250 and 300 ms. Multiple trials were conducted at each setting with 30 total trials; consisting of 30s continuous ultrasound exposure with subsequent off interval of 1 minute.
Results:
AP durations, peak amplitudes, including peak maximum and minimum were analyzed pre and post-ultrasound exposure on consecutive days. AP durations in both groups remained consistent averaging 30-50ms. Interestingly, peak maximum and minimum AP amplitudes, which initially ranged from 20-30mV, nearly doubled with ultrasound exposure. This increase in peak amplitude was more prominent after several days of repeated ultrasound exposure. In addition, new small APs were observed before or after large APs post-ultrasound with an increasingly distinct pattern on subsequent days.
Conclusion:
Our trials consistently demonstrated the ability of ultrasound energy to not only perpetuate APs but also induce new depolarizations with successive exposure to ultrasound over consecutive days without compromising AP duration. These manifestations may be the result of ultrasound energy conditioning [Na+] and [Ca+2] ion channels responsible for cardiac depolarization. It can also be theorized that ultrasound energy induces more pacemaker activity by mechanically stimulating cells or by increasing ion currents within the cells.
SURVIVAL AND OUTCOMES OF PATIENTS WITH UNOPERATED SINGLE VENTRICLE: A 30-YEAR CASE SERIES
Author links open overlay panelJosephPoteruchaMikeBierlePaulJulsrudHeidiConnollyNaserAmmashNandanAnavekarCaroleWarnes
Mayo Clinic College of Medicine, Rochester, MN, USA
Background:
Patients (pts) with unoperated single ventricle (SV) physiology rarely survive into adulthood with good functional status and may develop Eisenmenger syndrome (ES). We report survival and outcomes of a 30 year cohort of such pts.
Methods:
Adult pts with unoperated SV were captured from the Mayo Clinic echocardiographicdatabase from 1984 – 2014. Clinical data were obtained by clinic visits, chart review and surveys. Variables between pts with pulmonary stenosis (PS) and ES were compared.
Results:
Characteristics of PS versus ES pts are shown (Table). A total of 24 pts were identified; 22 had left ventricular morphology. The 50 year survival was 75% and 66% pts with PS and ES respectively. There was similar peak age between groups, with the oldest ES pt living into the 8th decade of life. Pulmonary vasodilator therapy was used in 72% of pts with ES. Pts with ES had higher incidence of hemoptysis; only 1 pt with PS had a stroke secondary to atrial fibrillation. Three with PS needed transplant at 40, 42, and 48 years; 1 had right ventricular morphology. Atrial arrhythmias were common (46% in PS; 45% in ES) and 3 pts with ES were able to tolerate epicardial pacing systems.
Conclusion:
Selected pts with unoperated SV with PS and balanced physiology can survive with good functional class to the 7th decade with good medical management. Strikingly, those pts with ES had similar survival, were effectively managed with pulmonary vasodilator therapy, and tolerated epicardial pacing, but had higher rates of stroke and hemoptysis.
| PS
(n = 13) |
Eisenmenger
(n = 11) |
p | |
| Clinical data | |||
| Male | 10 | 4 | NS |
| Single ventricle type | |||
| LV | 12 | 10 | NS |
| RV | 1 | 1 | NS |
| Peak age at last follow-up/death | 55 (30 – 67) | 51 (31 – 77) | NS |
| 50-year survival | 9/12 (75%) | 6/9 (66%) | NS |
| NYHA Class | |||
| I/II | 10 | 6 | NS |
| III/IV | 3 | 5 | NS |
| Pulmonary vasodilators | 0 | 8 | 0.0001 |
| Prostacyclin analogue | 0 | 4 | 0.03 |
| PGE1 inhibitors | 0 | 4 | 0.03 |
| Endothelin antagonist | 0 | 1 | NS |
| Combination therapy | 0 | 2 | NS |
| Complications | 13 | 21 | NS |
| Atrial arrhythmias | 6 | 5 | NS |
| Stroke | 1 | 5 | 0.06 |
| Hemoptysis | 0 | 5 | 0.01 |
| Complete heart block | 3 | 2 | NS |
| Need for epicardial pacing | 3 | 3 | NS |
| Hemodynamic and imaging data | |||
| Hgb (g/dL) | 19 ± 2 | 20 ± 2 | NS |
| SaO2 (%) | 87 ± 4 | 81 ± 7 | NS |
| EF (%) | 57 (35 – 60) | 55 ± 7 (40 – 64) | NS |
| AV regurgitation grade | |||
| Trivial | 9 | 7 | NS |
| Mild | 4 | 3 | NS |
| Moderate | 1 | 0 | NS |
| Severe | 0 | 1 | NS |
PS, pulmonary stenosis; LV, left ventricle; RV, right ventricle; PGE1, prostaglandin E1; Hgb, hemoglobin; EF, ejection fraction; AV, atrioventricular
ACCURACY OF IMAGING MODALITIES IN DETECTION OF BAFFLE LEAKS IN PATIENTS FOLLOWING ATRIAL SWITCH OPERATION
Author links open overlay panelCarolynWilhelmTraceySiskSharonRobleJoanneChisolmJohnCheathamCliffordCua
Nationwide Children’s Hospital, Columbus, OH, USA
Background:
Patients with D-transposition of the great arteries status post atrial switch operation are vulnerable to complications such as baffle leaks. The best imaging modality to detect baffle leaks is unknown. The purpose of this study was to determine the sensitivity and specificityof different imaging modalities in the detection of baffle leaks in this population.
Methods:
A single center retrospective chart review of atrial switch patients was performed. Sensitivity, specificity, negative predictive value and positive predictive value for detecting leaks were calculated for transthoracic echocardiogram (TTE) with and without agitated saline, transesophageal echocardiogram (TEE) with and without agitated saline, and cardiac magnetic resonance imaging. Studies were included if performed within one year of catheterization. Angiography via catheterization was used as the gold standard for detection of baffle leaks.
Results:
Fifty-eight atrial switch patients (54 Mustards : 4 Sennings) at a single pediatric center, undergoing 76 catheterizations, were analyzed. Age at catheterization was 30.1 ± 9.1 years. Thirty-nine catheterizations documented a baffle leak.
| Sensitivity % | Specificity % | Postive predictive value % | Negative predictive value % | |
| TTE
(n = 46) |
40.9 | 91.7 | 81.8 | 62.9 |
| TTE + agitated saline
(n = 10) |
71.4 | 100.0 | 100.0 | 60.0 |
| TEE
(n = 57) |
83.3 | 77.8 | 80.7 | 80.8 |
| TEE + agitated saline
(n = 27) |
100.0 | 92.3 | 93.3 | 100.0 |
| cMRI
(n = 26) |
60.0 | 100.0 | 100.0 | 80.0 |
cMRI = cardiac magnetic resonance imaging, TEE = transesophageal echocardiogram, TTE = transthoracic echocardiogram
Conclusion:
TTE or TEE with agitated saline is superior to cMRI in detecting baffle leaks in atrial switch patients. Agitated saline studies should be performed in this population when looking for baffle leaks.
TIMING OF PULMONARY VALVE REPLACEMENT IN ADULTS AFTER TETRALOGY OF FALLOT REPAIR IS SIGNIFICANTLY IMPACTED BY OBESITY
Author links open overlay panelElizabeth S.MakilAsifPadiyathKatherineBraleySean M.LangRonnie T. CollinsII
University of Arkansas for Medical Sciences, Little Rock, AR, USA
Background:
Tetralogy of Fallot (TOF) is one of the most common congenital heart diseases (CHD). Over 90% of all patients with CHD, including those with TOF, are expected to live to adulthood. Chronic pulmonary insufficiency in TOF leads to right ventricular (RV) dilation and is associated with increased arrhythmias and death. The timing of pulmonary valvereplacement in adults with TOF is largely based on RV size. RV end-diastolic volumeindexed (RVEDVI) to body surface area (BSA) > 150mL/m2 has been suggested as a threshold for pulmonary valve replacement and reversible RV dilation. We hypothesized a weight-based index would underestimate RV volume in obese patients compared to normal weight patients.
Methods:
A single institution retrospective review was performed of all patients with diagnosis of TOF or TOF/pulmonary atresia who underwent cardiac magnetic resonance imaging (MRI) from January 1, 2001 through September 30, 2014. Patients were excluded for age < 18 years or if biometric data were not available. Using each subject’s height as a constant, BSA was calculated by Dubois method at ideal body mass index (BMI), defined as 24 kg/m2, and obese BMI, defined as 30 kg/m2. The calculated BSA values were then used to determine RVEDVI for ideal and obese weights. Comparisons were made using paired t-test. P-value <0.05 was considered significant.
Results:
36 patients (55% male) met inclusion criteria. The mean age of the cohort was 27.7±9.3 years, height was 166.7±11.3 cm and weight was 72.5±19.7 kg. The mean difference in RVEDVI between the ideal weight and obese groups using calculated BSA was 11.5 mL/m2 (p<0.001). The RVEDVI was 10% less in the obese group. 8 patients were actually obese at the time of MRI. In this subgroup, the mean RVEDVI was 25.8 mL/m2 less (129.4 mL/m2 vs 155.2 mL/m2) when using actual BSA from the subjects’ true, obese weight compared to the RVEDVI based on calculated ideal weight (p<0.002). The RVEDI was 20% less for obese weight compared to normal weight.
Conclusion:
Indexing RV volume to a weight-dependent measure significantly underestimates the degree of RV dilation in adults with TOF. This underestimation delays intervention and may contribute to increased morbidity and mortality.
ANOMALOUS ORIGIN OF THE CORONARY ARTERIES: INCIDENCE AND OUTCOMES AMONG PATIENTS UNDERGOING CORONARY CTA
Author links open overlay panelMichaelCheezumBrianGhoshhajraMarcioBittencourtEdwardHultenNegarehMousaviMichaelSteignerFrankRybickiNishantShahThomasMacGillivrayAmiBhattAnne MarieValenteSuhnyAbbaraUdoHoffmannMarceloDi CarliDoreenYehMichaelLandzbergRichardLiberthsonRonBlankstein
Brigham and Women’s Hospital, Boston, MA, USA
Massachusetts General Hospital, Boston, MA, USA
Background:
We aimed to evaluate the incidence of anomalous coronary arteries arising from the opposite sinus (ACAOS) among patients undergoing CTA, and report CTA findings associated with revascularization.
Methods:
We examined 3585 consecutive patients referred for coronary CTA to identify those with ACAOS. Patients were followed for early (<90d) vs late revascularization, CV death and myocardial infarction. CTAs were reviewed for ACAOS proximal narrowing (none/minimal versus “slit-like”) and CAD (none/nonobstructive versus obstructive [≥50%] stenosis
Results:
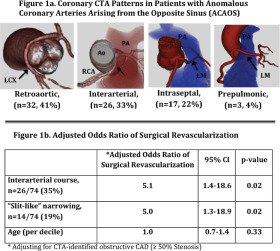
The final cohort included 74 patients (2.1%) with ACAOS; mean age 52±17 yrs. 31 (42%) patients had known ACAOS, while 43 (58%) were discovered on CTA. ACAOS subtypes and incidence are shown in Figure 1a. In 41±23 month follow-up there were 15 early revascularizations (14 surgical/1 PCI), 1 late CABG and 1 CV death. Among patients undergoing surgery, all patients age <45 (n=5) were treated with unroofing/reimplantation, while all patients age ≥45 had CABG (n=10) including 6 patients with obstructive CAD. Adjusted for obstructive CAD, the presence of slit-like narrowing and interarterial course were independently associated with revascularization (Figure 1b).
Conclusion:
Among CTA patients, the incidence of ACAOS was 2.1%. While hard event rates were very low with 1 CV death in 3.4 year follow-up, 16 patients underwent coronary revascularization, attributed to high risk ACAOS with proximal narrowing and/or obstructive CAD.
PREVALENCE AND LONG TERM FOLLOW-UP OF ANOMALOUS CORONARY ARTERIES ORIGINATING FROM OPPOSITE SINUS (ACAOS)
Author links open overlay panelNeginNezaratYantingLuoSirousDarabianRineNakanishiAnasAlaniSuguruMatsumotoJebyAbrahamFernandezFloresMatthewBudoff
LAbioMED, Torrance, CA, USA
Background:
Coronary artery anomalies (CAAs) are the second cause of sudden cardiac death in young individuals, although many older adults with these anomalies have been found incidentally. Anomalous coronary arteries originating from the opposite sinus (ACAOS) is a clinically important type of CAA; however, its management creates some dilemma. Because the incidence and risk of ACAOS during long-term observation have not been well examined, we sought to determine its prevalence and all-cause mortality rate.
Methods:
We evaluated 9,907 patients who underwent electron-beam CT or 64-detector MDCT from August 2000 to June 2014. Patients’ demographic and clinical information was obtained. The number and anatomical characteristics of coronary artery anomalies were determined. Coronary arteries with interarterial, acute angle, slit-like, intramural, and all types of left main ACAOS were defined as high risk. Patients without follow-up were contacted for additional data. Fisher’s Exact Test was applied for the comparison of prevalence between high risk and non-high risk groups.
Results:
Among 83 patients identified with anomalous origin coronary artery, 69 cases (mean age: 54.8±17.2 years; female 33.3%) were ACAOS (0.7% of total population). Only 8 (9.8% of all anomalies) patients were below 30 years old. The most prevalent ACAOS was right coronary artery from opposite sinus with rate of 47 (56.0%). In addition, the prevalence of patients with left circumflex, left main, and left anterior descending ACAOS was 14 (16. 7%), 7(8.3%) and 2(2.4%), respectively. In total, 45 (53.6%) patients with anomalous origin coronary artery, showed high risk patterns. There was no significant demographic difference between the high risk and non-high risk groups. Over the average 5.6 years follow up, we had five all-cause mortalities among anomalous origin coronary artery. Only one patient with slit-like RCA from opposite sinus was in the high risk ACAOS group.
Conclusion:
The prevalence of anomalous coronary artery from opposite sinus is 0.7% in our population. The most prevalent case of ACAOS was a right coronary artery originating from the opposite sinus. In adult patients, the outcome of ACAOS tends to be benign.
STANDARDIZED APPROACH TO PATIENTS WITH ANOMALOUS AORTIC ORIGIN OF A CORONARY ARTERY: RESULTS FROM THE CORONARY ANOMALIES PROGRAM AT TEXAS CHILDREN’S HOSPITAL
Author links open overlay panelSilvanaMolossiCarlosMeryRajeshKrishnamurthyKristenSexsonKathleenCarberryCarmen H.WatrinDanaReavesPrakashMasandDeanMcKenzieCharlesFraser
Baylor College of Medicine, Houston, TX, USA
Texas Children’s Hospital, Houston, TX, USA
Background:
Anomalous aortic origin of a coronary artery (AAOCA) is the second leading cause of sudden cardiac death in young athletes. Management is controversial and longitudinal follow-up data is lacking.
Methods:
Prospective, observational study of patients (pts) seen with AAOCA from 12/2012 to 04/2014. The Coronary Anomalies Program (CAP) was established with defined multidisciplinary team, clinic, imaging (CTA), management algorithm and follow-up. Surgical indication is based on lesions deemed high-risk including anomalous left coronary artery(ALCA), symptoms ascribed to or evidence of myocardial ischemia, intramurality, or abnormal ostium.
Results:
A total of 58 pts were evaluated. From these, 36 (62%) had anomalous right coronary artery(ARCA), 10 (17%) ALCA, 5 (9%) a single coronary, 4 (7%) anomalous circumflex, and 3 (5%) high origin CA. Surgery was indicated in 25 pts (43%), 4 declined (ALCA 1, ARCA 3). Of those operated on, 6 had ALCA (30%) and 14 ARCA. Unroofing was performed in 15 (ALCA 4, ARCA 11), coronary translocation in 2 ARCA, and ostioplasty in 3 (ALCA 2, ARCA 1). Among surgical patients, symptoms included: non-specific chest pain (CP) in 9 (ALCA 3, ARCA 6), CP on exertion in 2 ARCA, syncope on exertion in 2 (ALCA 1, ARCA 1), aborted SCD in 2 ALCA, ECG changes with troponin leak in 1 ARCA, and no symptoms in 7 pts (ALCA 2, ARCA 5). Post-operative complications occurred in 4 pts including absence seizures (likely present pre-operatively), small aortic tear requiring a second run of bypass, post-cardiotomy syndrome, and left lung collapse. Recurrent symptoms of CP occurred in 3 pts, all with negative diagnostic testing. All pts have returned for follow-up. All surgical pts were released to unrestricted exercise activities. None has suffered a recurrent event. During this time period, the CAP has also seen pts with hypoplastic right coronary (2), coronary atresia (1), and myocardial bridge (3).
Conclusion:
Development of a dedicated multidisciplinary team has allowed a consistent approach to the evaluation and management of AAOCA pts. Longitudinal follow-up is imperative to define best treatment strategies, exercise recommendations and possibly risk stratification in this population.
DOES LOCATION OF ADMISSION AFFECT RESOURCE UTILIZATION AND OUTCOME AFTER NEONATAL CARDIAC SURGERY? A MULTI-CENTER STUDY
Author links open overlay panelJoyceJohnsonJacobWilkesShajiMenonLloydTaniHsin-YiWengNelangi M.Pinto
Ann & Robert H. Lurie Children’s Hospital of Chicago, Chicago, IL, USA
University of Utah, Salt Lake City, UT, USA
Background:
Neonatal cardiac surgeries are resource intensive with high costs and significant hospital lengths of stay (LOS). Location of inital admission unit may impact resource use and outcomes. Understanding this relationship may allow modifications to improve efficiency. We compared resource use, costs, and outcomes in neonates undergoing cardiac surgery by location of initial admission unit and sought to determine factors contributing to differences.
Methods:
Data was collected from the Pediatric Health Information Systems database (38 hospitals) on neonates (age < 30 days) undergoing cardiac surgery (2004-13). Hospital costs, LOS, and mortality were adjusted for disease severity (RACHS-1 score), prematurity, genetic syndrome, prostaglandin use, low birth weight, payer, admit year, race and compared by admission unit. Costs were modeled using multivariate gamma regression models with log link and were adjusted by region to 2013 dollars. The impact of complications (including infections, ECMO use, and cardiac arrest) on differences in cost were analyzed.
Results:
There were 20,995 patients admitted (neonatal ICU (NICU) 45%, cardiac ICU (CICU) 37%, pediatric ICU (PICU) 13%, other 5%). Adjusted odds of mortality was 0.59 (95% Confidence Interval (CI) 0.43-0.80, p<0.001) in the CICU compared to the NICU. Median cost was $108,710 (interquartile range (IQR) $67,550-185,890) and median LOS 21 (IQR 13-36) days. After controlling for the above factors, CICU admission was independently associated with lower hospital cost (-$7,372, 95% CI -$5,826, -8,917, p <0.001), and shorter hospital LOS (-3.5 days, 95% CI -3.2,-3.8, p <0.001). While all categories of costs were lower, the biggest differences were in room and other charges. Of factors examined, the presence of infection led to the largest change in costs between the CICU and NICU.
Conclusion:
After controlling for patient and institutional factors, initial admisson of neonates undergoing cardiac surgery to the CICU is associated with lower adjusted mortality, costs, and LOS when compared to the NICU. ICU specialization may result in better outcomes and more efficient resource use.
THE INFLUENCE OF DEFICIENT RETRO-AORTIC RIM ON TECHNICAL SUCCESS AND EARLY ADVERSE EVENTS FOLLOWING DEVICE CLOSURE OF SECUNDUM ATRIAL SEPTAL DEFECTS: AN ANALYSIS OF THE IMPACT® REGISTRY
Author links open overlay panelMichael L.O’ByrneMatthewGillespieYoavDoriKevinKennedyJonathanRomeAndrewGlatz
The Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Mid America Heart Institute, Kansas City, KS, USA
Background:
Concern regarding aortic erosion has focused attention on deficient retro-aortic rim in patients undergoing device closure of atrial septal defects (ASD). However, whether retro-aortic rim size is a risk factor for technical failure and early adverse outcomes has not been delineated.
Methods:
A multi-center retrospective cohort study of children and adults undergoing cardiac catheterization for device occlusion of ASD between 1/2011-4/2014 was performed, using data from the IMPACT® (Improving Pediatric and Adult Congenital Treatment) Registry. Subjects with reported retro-aortic rim were divided between those with rim <5 and >5 mm. The two primary outcomes were technical failure and composite of all major early adverse events. Secondary outcomes were surrogates of technical complexity including total case time, total sheath time, and fluoroscopy time. The effect of deficient retro-aortic rim on risk of technical failure and early adverse outcome was assessed using hierachical logistic regression, adjusting for subject age, height, sex, ASD diameter, balloon sizing technique, and device type.
Results:
1,230 subjects (from 72 centers) in whom retro-aortic rim size was recorded underwent attempted device closure during the study period, of which 43% had deficient retro-aortic rim. Technical failure occurred in 73 subjects (5.9%) and a major early adverse event in 65 subjects (5.3%). In multivariate models, the presence of a deficient retro-aortic rim was not significantly associated with either technical failure (OR: 1.5, 95% CI: 0.92-2.44, p=0.11) or major early adverse event (OR: 0.77, 95% CI: 0.45-1.32, p=0.34). In multivariate models, total case time (p=0.01) and fluoroscopy time (p=0.02) were greater in subjects with deficient retro-aortic rim, but sheath time was not significantly different (p=0.07).
Conclusion:
Deficient retro-aortic rim is highly prevalent in patients presenting for device closure of secundum atrial septal defects. These defects may be technically more challenging to treat, but deficient retro-aortic rim was not associated with risk of technical failure or early adverse outcomes. Effects on longer-term outcomes require further study.
TRENDS IN RIGHT VENTRICULAR DYSFUNCTION AND TRICUSPID REGURGITATION AFTER SINGLE VENTRICLE PALLIATION OF HYPOPLASTIC LEFT HEART SYNDROME AND THEIR DIFFERENTIAL IMPACT ON SURVIVAL
Author links open overlay panelTravis J.WilderEugeneBlackstoneJeevananthamRajeswaranChristopherCaldaronePeter J.GruberBahaaldinAlsoufiRobertJaquissChristo I.TchervenkovJamesJaggersMing-SingSiChristopherMascioChristianPizarroDavidOvermanEdwardHickey
CHSS Data Center, Hospital for Sick Children, Toronto, Canada
Background:
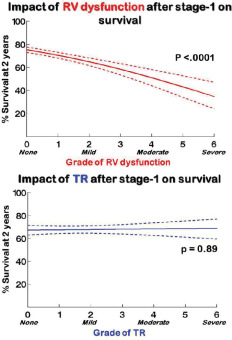
Successful single ventricle (1-V) HLHS repair relies on durability of right ventricular (RV) and tricuspid valve performance. We studied trends in RV dysfunction and tricuspid regurgitation(TR) and their differential impact on survival.
Methods:
5,477 echo reports on 515 neonates with HLHS (2005-2014; 20 institutions) were used to grade RV dysfunction or TR. Nonlinear mixed models characterized time-related risks of ≥moderate RV dysfunction and ≥moderate TR. These, and parametric survival models, were used for regression.
Results:
Prevalence of RV dysfunction was 10% ≤6 months, and ~2 fold higher in those who died. During late follow-up RV function was preserved in >95%. TR also peaked ≤6 months, but persisted ~10% thereafter. Worse RV dysfunction pre-stage-1 strongly predicted continued RV dysfunction after stage-1 (P<.0001), but did not predict TR. Baseline TR did not predict RV dysfunction or TR after stage-1 (P=.43). In risk-adjusted models, worse RV dysfunction immediately after stage-1 strongly predicted persistent dysfunction, persistent TR and death (P<.01, figure). The corollary was not true: worse TR immediately after stage-1 was not a strong predictor of death. 27 children had TV repairs; 22 remain alive and 3 (14%) have ≥moderate TR at last follow-up.
Conclusion:
TR without RV dysfunction can be mitigated. RV dysfunction after 1-V palliation, however, is poorly tolerated – even in absence of TR; early evaluation for transplantation may be appropriate.
ETIOLOGY, NEW TREATMENT, AND SHORT-TERM OUTCOME OF PLASTIC BRONCHITIS IN FONTAN PATIENTS TREATED WITH SELECTIVE LYMPHATIC DUCT EMBOLIZATION
Author links open overlay panelYoavDoriMarcKellerJackRychikMaximItkin
The Children’s Hospital of Philadelphia, Philadelphia, PA, USA
The Hospital of the University of Pennsylvania, Philadelphia, PA, USA
Background:
Plastic bronchitis (PB) is a potentially life-threatening disorder found in patients after total cavopulmonary connection (TCPC). Although lymphatic abnormalities have been postulated to play a role in the disease process, to date, the etiology and pathophysiology of this complication remains incompletely understood. Here we report on the etiology of plastic bronchitis as demonstrated by MR lymphangiography and a new potential treatment option for these patients.
Methods:
This is a retrospective case series of the 7 patients with TCPC and PB in our institution that underwent T2 non-contrast lymphatic mapping, dynamic contrast MR lymphangiography(DCMRL), and selective lymphatic duct embolization (SLDE) procedures.
Results:
All 7 (100%) of the patients were after TCPC. By MR lymphangiography all 7 (100%) patients had dilated peribronchial lymphatic networks supplied by retrograde lymphatic flow from the TD. This was confirmed by conventional lymphangiography. In four of the patients (57%) there was resolution of casting within 1 week of the procedure without recurrence, 2 of the patients had one additional casting episode 1 month post procedure, and 1 patient had an additional cast 2 months post procedure in the setting of a severe viral respiratory illness. All of the 7 patients (100%) are currently cast free. One of the patient developed PB and chylothorax 4 days after the TCPC operation and was headed for TCPC takedown. After SLDE, his effusions and PB resolved and he was discharged home after 2 weeks. Median follow-up in this cohort is 3.8 mo with range 2-14 mo. There were no significant complications from the procedure. The most common complication has been non-specific transient abdominal and chest pain shortly after the procedure.
Conclusion:
The hallmark finding on MRI in patients with PB are the presence of peribronchial dilated lymphatic networks supplied by retrograde lymphatic flow originating from the TD. This leads to continuous spillage of protein into the airway with accretion of material into a bronchial cast. SLDE of these networks is feasible and potentially safe. The procedure can result in resolution of PB symptoms and is a new possible treatment option for these patients.
40 YEARS OF THE FONTAN OPERATION: LONG-TERM OUTCOME OF 1,052 PATIENTS
Author links open overlay panelKavithaPundiJosephDearaniKrishnaPundiJonathanJohnsonZhuoLi
Patrick O’Leary, David Driscoll, Frank Cetta, Mayo Clinic, Rochester, MN, USA
Background:
We sought to examine our institution’s experience over 4 decades with the Fontan operation, and to determine factors associated with morbidity and mortality.
Methods:
Records of all patients who had a Fontan from 1973 – 2012 at Mayo Clinic were reviewed. A follow-up questionnaire was mailed to all patients known to not be deceased at the time of study.
Results:
1052 pts had a Fontan operation (mean age = 9.4 ± 7.5 yrs). 616 pts had an atriopulmonary connection, 262 lateral tunnels, 120 extracardiac conduits, and 54 had other modifications. Fenestration was performed in only 86 pts (8%). Anatomy included Tricuspid Atresia (273), DILV (271), Heterotaxy (135), PA/IVS (55), and HLHS (24). The overall 10, 20, and 30-year survival was 75%, 62%, and 47%, respectively. Factors associated with decreased long-term survival include: preop diuretic use, asplenia, longer bypass time, postop Fontan pressure > 20 mmHg, elevated postop LA pressure, and operation prior to 1990. There was no mortality difference between patients with RV and LV dominant ventricular morphology. Preop and post bypass sinus rhythm was associated with improved long-term survival. Ten-year survival was improved in patients undergoing extracardiac conduit or lateral tunnel Fontan compared to patients who had atriopulmonary connection (p<0.04), though this was influenced by surgical era. Freedom from death or reoperation at 10, 20, and 30 years after the Fontan was 70%, 51%, and 37%, respectively. The most common re-operations were pacemaker insertion/revision in 212 patients (20%), Fontan revision/conversion in 117 patients (11%) and AV-valve repair/replacement in 66 patients (5%). Clinically significant atrial or ventricular arrhythmias occurred in 468 (44%) pts. 95 (9%) pts developed PLE, and 38 (4%) pts had cardiac transplantation.
Conclusion:
As the surgical techniques for the Fontan operation have improved over the last 40 years, there has been improvement in survival. However, the development of PLE and arrhythmias, and the need for reoperation during long-term follow-up pose significant management challenges.
THE RELATIONSHIP BETWEEN ATRIAL FLUTTER AND ATRIAL FIBRILLATION IN ADULTS WITH CONGENITAL HEART DISEASE
Author links open overlay panelElmarMalekDucDoGeorgeLuiDanielMurphyJamilAboulhosnAminAl-AhmadNoelBoyle
UCLA Division of Cardiology, Los Angeles, CA, USA
Stanford School of Medicine Division of Cardiovascular Medicine, Palo Alto, CA, USA
Background:
Atrial arrhythmias are a common cause of morbidity in the adult congenital heart disease(ACHD) population. Atrial flutter (AFL) is most prevalent of these arrhythmias and can be typical cavotricuspid dependent or atypical scar-based intra-atrial reentrant tachycardia. Atrial fibrillation (AF) is also frequently seen in the ACHD population with aging. The aim of this study is to evaluate whether AF in the ACHD population is generally preceded by a diagnosis of AFL, thus suggesting a progression of disease, or if they are independent conditions.
Methods:
A random sample of 628 patients age ≥ 18 years seen at the UCLA and Stanford ACHD clinics from January 2000 to November 2013 was evaluated. Data regarding congenital abnormality and arrhythmic history, including age at onset of AFL and of AF were collected.
Results:
A history of AFL was present in 96 (18.2%) patients, AF in 68 (10.8%), and both AFL and AF in 28 (4.6%) patients. In patients with both, AFL was diagnosed before AF in 14 (50.0%) patients, at the same time of AF in 6 (21.1%) patients, and after AF in 7 (25.0 %) patients. In 5/11 (45%) of Tetralogy of Fallot (TOF), 3/9 (33%) Systemic Right Ventricle (RV), and 3/6 (50%) Single Ventricle patients with AF, this diagnosis was preceded by AFL. In contrast, 0/6(0%) patients with Ebstein’s anomaly, and 0/11(0%) valvular lesion (7/11 of whom had pulmonic stenosis) and AF were diagnosed with AFL prior to AF.
Conclusion:
A diagnosis of AFL often preceded AF in patients with complex lesions (TOF, Systemic RV, Single Ventricle) suggesting that AF may be a progression of a similar pathophysiologicprocess, whereas AF appears independent of AFL in patients with valvular lesions. This suggests that surgical or ablation management of AFL in patients with complex lesions and more extensive surgical histories may prevent progression of AFL to AF.
CONTRACEPTION PRACTICES AND PREGNANCY OUTCOME IN PATIENTS AFTER FONTAN OPERATION
Author links open overlay panelKavithaPundiJonathanJohnsonCrystalBonnichsenSabrinaPhillipsMaryCannobioFrankCetta
Mayo Clinic, Rochester, MN, USA
Background:
The feasibility and safety of pregnancy in the patient with Fontan operation is incompletely understood. The purpose of this single center study was to determine contraception habits and early and late outcomes of pregnancy after Fontan operation.
Methods:
Retrospective review of medical records and patient surveys for women of child bearing age from our Fontan database. Patients with recent contraception and pregnancy data were included in the study.
Results:
Of the 138 women with available contraception data, 44% used no contraception, 12% each used barrier methods, combination hormone therapy and sterilization, 8% Depo-Provera, 7% IUDs, 4% had a partner with a vasectomy and 1% used progestin pills. 6 women had thrombotic complications (only 1 on oral contraceptives). There were no known IUD complications. 35 women had pregnancy data available. Ventricular morphology was RV in 9 (26%), LV in 22 (61%), and common/indeterminate morphology in 4. Before Fontan operation there were 10 pregnancies (8 miscarriages, 2 therapeutic abortions). After Fontan operation there were 70 pregnancies resulting in 35 miscarriages (50%), 28 live births (40%), 6 therapeutic abortions (9%) and 1 ongoing (1%). In the 6 women with hepatic cirrhosis there were 7 pregnancies (5 miscarriages, 1 therapeutic abortion and 1 live birth). There were no viable pregnancies in women with a post-Fontan EF < 40%. Pregnancy outcome did not correlate with immediate postoperative Fontan intracardiac pressures. Atrial arrhythmias occurred in 7 pregnancies (6 women, 3 with arrhythmia prior to pregnancy). There were no maternal deaths during pregnancy. During long term follow up, 1 death and 1 transplant occurred. Mean gestational age of the newborns (n = 18) was 32.6 ± 4.1 weeks; mean birth weight (n = 16) was 1992 ± 756 gm. There was 1 neonatal death due to prematurity and 2 children were born with CHD (1-PDA, 1-VSD).
Conclusion:
In women with Fontan palliation who become pregnant, miscarriages, preterm delivery and low birth weight are common. However, further studies are needed to identify specific variables influencing risk stratification of pregnancy in this patient population.
THROMBOEMBOLISM PROPHYLAXIS IN FONTAN PATIENTS. WHAT SHOULD WE USE? A META-ANALYSIS OF PUBLISHED TRIALS
Author links open overlay panelSaidAlsidawiTarekAlsaiedGruschenVeldtman
Division of Cardiovascular Health and Diseases, University of Cincinnati, Cincinnati, OH, USA
The Heart Institute, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA
Background:
The role of anti-platelets and anticoagulation in patients who underwent the Fontan procedure remains controversial. While most authors agree on the need for prophylaxis to prevent thromboembolic (TE) events, there is still lack of strong evidence to support such approach and the best agent that provide the best protection.
Methods:
We conducted a meta-analysis of published trials that studied the role of using TE prophylaxis in patients who underwent the Fontan procedure. We searched PubMed and the Cochrane Library for trials published in English language. Both randomized trials as well as registries were included. We identified 11 studies with a total number of 2275 patients with an average follow-up time of 7.1 years.
Results:
Our analysis showed clear advantage of using TE prophylaxis (aspirin or warfarin) in preventing TE in patient with fontan compared to no prophylaxis (OR: 0.425. 95% CI: 0.194-0.929. P <0.01 and I²= 37%). There was a significant advantage to aspirin over no TE prophylaxis (OR: 0.363. 95% CI: 0.177-0.744. P<0.01 and I²=0%) as well as to warfarin over no TE prophylaxis (OR: 0.327. 95% CI: 0.168-0.634. P<0.01 and I²=2.5%). There was however no significant difference between warfarin and aspirin in preventing TE (OR: 0.936. 95% CI: 0.609-1.438. P=0.54. I²=0%). When only new type Fontan technique (total cavo-pulmonary connection) was included, there was again no significant advantage to warfarin over aspirin (OR: 0.813. 95% CI: 0.471-1.401. P: 0.34. I²=11%). Furthermore, There was no significant advantage to warfarin over aspirin in preventing early (within 6 months of the operation) (OR: 0.784. 95% CI: 0.310-1.982. P=0.37. I²=8%) and late (>6 months) TE events (OR: 0.776. 95% CI: 0.249-2.42. P=0.3. I²=45%).
Conclusion:
In our meta-analysis, we showed a clear benefit of using TE prophylaxis (with aspirin or warfarin) to prevent TE events in patients after fontan procedure. Our data suggests no significant benefit of warfarin when compared to aspirin in preventing early and late TE events in all type of fontan operations as well as in the newer fontan type techniques. Large randomized controlled trials are needed to confirm these results.
GEOMETRY OF TRICUSPID VALVE INFLOW CORRELATES WITH VENTILATORY EFFICIENCY AND PEAK OXYGEN PULSE IN ADULTS WITH SYSTEMIC RIGHT VENTRICLES AND TRANSPOSITION OF THE GREAT ARTERIES
Author links open overlay panelKeri M.ShaferNinaMannAnne MarieValenteJonathanRhodes
Boston Children’s Hospital, Boston, MA, USA
Background:
Exercise test variables including ventilatory efficiency (VE/VCO2 slope) and peak oxygen uptake (pVO2) correlate with mortality in adults with congenital heart disease. O2 pulse (VO2 divided by heart rate) is used as a surrogate for stroke volume. However, correlation of these exercise values with standard imaging measures is limited in those with Transposition of the Great Arteries (TGA) with systemic right ventricles (SRV).
Methods:
We retrospectively identified 84 TGA patients with SRVs who had cardiopulmonary exercise tests and cardiac magnetic resonance imaging (CMR) (median = 1 day between exams). Standard imaging, demographic and clinical variables were recorded. Geometric assessment of the SRV in diastole was made on CMR by measuring 1) angle of tricuspid valve (TV) inflow relative to the apex 2) sphericity index (short axis/long axis) and 3) a new geometric index was devised [inflow angle * (distance from TV to perpendicular free wall – TV to apex)].
Results:
Mean age was 30.1±7.2 years, 75% had D-loop TGA with atrial switch and 38% were women. Mean SRV ejection fraction was 48±9%, and SRV indexed end diastolic volumewas 117.47±33.8 mL/m2. Peak VO2 was 23.5±7.6 mL/kg/min, Ve/VCO2 slope 29 ±5.6, peak O2 pulse 11±3.2mL. SRV ejection fraction correlated with pVO2 (r=0.32, p=0.002) but did not correlate with VE/VCO2 slope or O2 pulse. Peak O2 pulse correlated with the inflow angle (r=-0.24, p=0.03). The VE/VCO2 slope correlated with both the inflow angle(r=0.35, p=0.001) and geometric index (r=0.27, p=0.01). In multivariate analysis, correlation between O2 pulse and inflow angle remained significant (p=0.03). Multivariate analysis also revealed independent correlations between VE/VCO2 slope and D-loop TGA anatomy (p=0.01), geometric index (p=0.03) and inflow angle (p=0.04). Correlation of sphericity index with exercise variables was not significant.
Conclusion:
Tricuspid valves angled away from the apex are correlated with lower O2 pulse and higher VE/VCO2 slopes representing poorer performance on cardiopulmonary exercise testing. Noninvasive imaging assessment in TGA patients with SRVs is enriched by evaluation of tricuspid valve and ventricular geometries.
HALF A CENTURY’S EXPERIENCE WITH CLASSIC GLENN SHUNT
Author links open overlay panelRiad AbouZahrPaulKirshbomGaryKopfSandeepSainathanMargaret M.SteeleRobertElderMohsenKarimi
Yale University School of Medicine, New Haven, CT, USA
Background:
Five decades after its introduction, the Glenn shunt remains an integral step for patients undergoing single ventricle palliation. Mid-term outcomes of the original experience were previously reported. The aim of this study was to perform a longitudinal follow up of the original cohort of patients who underwent the Glenn shunt.
Methods:
We preformed a retrospective study of the original cohort of patients who underwent Glenn shunt at Yale between 1958-1988. Electronic medical records and chart review up to current era were used to collect comprehensive data. Kaplan-Meier survival curves and statistical analysis were performed.
Results:
91 patients underwent a Glenn shunt at an average age of 6.6 ± 2.5 years, of which 89 were a classic Glenn shunt. Median overall survival was 43 years (95% CI 39.5-46.5) while median survival from the Glenn shunt was 31.4 years (95% CI 23.9-38.9). 46 patients died, 7 in the early post-operative period and 39 late deaths. 26 were lost to follow up. 19 patients remain alive with active clinical follow up, 6 of whom still live with their classic Glenn shunt without conversion to bidirectional Glenn. Following original Glenn, the most common subsequent operative procedures were Fontan (n=35), BT shunt (n=14), biventricular repair (n=8), axillary arteriovenous fistula (n=8), central shunt (n=3), tricuspid valve repair (n=2), and cardiac transplantation (n=2). Overall, 26 patients (31%) developed pulmonary arteriovenous (AV) fistula with 11 patients (42%) requiring coil embolization. There were a total of 28 patients who developed arrhythmias, mostly in the tricuspid atresia group (n=16), with the majority being atrial tachyarrhythmias (48%). 16 patients required permanent pacemaker placement for sinus node dysfunction.
Conclusion:
The Glenn shunt continues to provide an excellent staged palliation in single-ventricle patients and a bridge to two-ventricle repair half a century from its inception. Most patients required subsequent surgical interventions. Arrhythmias and pulmonary AV fistulas were common among single ventricle cohort. Quality of life evaluation of the surviving patients would be an important outcome measure for future investigation.
POST-CARDIOTOMY EXTRACORPORAL MEMBRANE OXYGENATION SUPPORT AFTER HIGH-RISK OPERATIONS IN ADULTS WITH CONGENITAL HEART DISEASE
Author links open overlay panelBenjaminAcheampongJohnStulakJosephDearaniGregorySchearsSudhirKushwahaRichardDalyJonathanJohnson
Mayo Clinic, Rochester, MN, USA
Background:
Cardiac surgery in high-risk patients (pts) with adult congenital heart disease (ACHD) may require mechanical circulatory support (MCS) such as extracorporeal membrane oxygenation (ECMO) or intra-aortic balloon pump (IABP) in the post-operative period.
Methods:
We reviewed records for all ACHD pts who required MCS following cardiotomy from 1/2001-12/2013.
Results:
During the study period, 4,220 operations were performed in ACHD pts at our institution, of whom 25 (0.6%) required postoperative MCS (15 males; median age 41 yrs, range 19-75; median past sternotomies 2 [1-4]). Pre-operatively, mean systemic ventricular EF was 47% (range 10-66%); 68% of pts were in NYHA class IV heart failure. Underlying diagnoses included pulmonary atresia with intact ventricular septum (24%), tetralogy of Fallot (16%), Ebstein anomaly (12%), cc-TGA (12%), and septal defects (12%), with tricuspid atresia, truncus arteriosus and congenital valve abnormalities constituting the remaining diagnoses (24%). The most common operations performed were valvular operations with/without maze (52%), Fontan conversion (20%), coronary bypass grafting with valvular operations (12%), and heart transplant (8%). Indications for MCS were left-sided (systemic) heart failure (32%), right-sided (sub-pulmonary) heart failure (24%), biventricular heart failure (36%), persistent arrhythmia (4%) and hypoxemia (4%). Both ECMO and IABP were used in 68% of pts, while 32% used ECMO only. The mean duration of MCS was 195.8 hrs (range 20-850). Common early morbidities included coagulopathy (60%), renal failure (56%) and arrhythmia (48%). Overall, 48% of pts survived to hospital discharge. All deaths were due to either multi organ failure or the underlying cardiac diagnoses, with one pt dying from overwhelming sepsis. Median available follow up for survivors was 38.5 months (max 106 months). New York Heart Association functional class was I/II in 6/9(67%) late survivors in whom close follow up was available.
Conclusion:
Following complex operations in high-risk ACHD pts, MCS may be required. Despite significant morbidity, nearly half of pts survive to hospital discharge with good functional status at late follow up.
ACUTE IMPACT OF FONTAN OPERATION ON ENTERIC PROTEIN LOSS AND MESENTERIC VASCULAR RESISTANCE
Author links open overlay panelJyoti KandlikarPatelKathleen M.LoomesDavidGoldbergAgbenuEjembiKathrynDoddsJackRychik
The Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Background:
Protein losing enteropathy (PLE) is a challenging complication after Fontan operation (FO). PLE may develop over a wide time course, ranging from days to decades after FO. Sub-clinical enteric protein loss (EPL) in which stool protein levels are elevated but not to the extent to cause hypoalbuminemia and edema may be common after FO and may precede development of clinical PLE. We sought to determine the acute effects of Fontan circulation on EPL and mesenteric vascular resistance.
Methods:
A prospective longitudinal study was performed. EPL was evaluated through stool alpha-1-antitrypsin (A1AT) concentration, and intestinal circulation was characterized by Doppler derived resistance indices of the superior mesenteric artery (SMA). Serum albumin levels were also obtained. Assessments were performed before FO and acutely after FO. Post FO data were collected when the patient met earliest criteria of wellness (>4 days post FO, spontaneously breathing, not receiving inotropic support, and taking enteric feeds).
Results:
We enrolled 31 subjects (27 M, 4 F). In most (n=29), the Fontan type was fenestrated extracardiac. Median age at FO was 3.0 years (IQR 2.5-3.3). Pre FO study was performed 9 days (IQR 2-36) prior to surgery, and post FO study 6 days (IQR 5-8) after surgery. No clinical PLE was observed. Abnormal A1AT (> 54 mg/dl) was present in 2 subjects pre FO and in 2 different subjects post FO. One subject with abnormal A1AT at each time point had unique and significant hemodynamic disturbance (junctional bradycardia or tricuspid stenosis after valvuloplasty). There was no difference in SMA resistance indices pre versus post FO. Albumin (mg/dl) was lower post FO compared to pre FO (3.2[0.5] vs 3.8[0.7], p=.0008) but did not correlate with abnormal A1AT or with SMA resistance indices.
Conclusion:
Imposition of a Fontan circulation does not commonly result in acute development of EPL. However, EPL may occur before or after FO particularly when hemodynamic disturbances are present, which suggests an inherent association with single ventricle defects. Serial stool A1AT evaluation post FO may better delineate the time course of development of EPL or possible progression to PLE in at-risk patients.
CHANGES IN CEREBROVASCULAR RESISTANCE IN RESPONSE TO MATERNAL HYPEROXYGENATION DEPENDS UPON GESTATIONAL AGE IN FETUSES WITH HYPOPLASTIC LEFT HEART SYNDROME
Author links open overlay panelAnitaSzwastMary E.PuttDanielLichtJ. WilliamGaynorJackRychik
Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Background:
Fetuses with Hypoplastic Left Heart Syndrome (HLHS) compensate for diminished cerebral blood flow and oxygen content by lowering cerebrovascular resistance. By increasing cerebral oxygen content, maternal hyperoxygenation (MH) could theoretically improve brain development and reduce brain injury. We sought to determine whether gestational age (GA) impacts the response to MH in HLHS fetuses.
Methods:
Cerebrovascular resistance was assessed via the middle cerebral artery (MCA) pulsatility index (PI). MCA PI was sampled at baseline on room air and after 10 minutes of MH (10 liters of flow via a non-rebreather mask) between 20-41 weeks in 38 HLHS fetuses. A linear mixed effect model was performed. Significance was set at p=0.05.
Results:
GA groups 32-36 weeks and 36-41 weeks have significantly lower MCA PI, compared to GA groups less than 28 weeks. MCA PI increases by 0.2 units between 32-36 weeks and by 0.13 units between 36-41 weeks with MH (Figure 1A). No increase in MCA PI was seen below 32 weeks. Furthermore, the change in MCA PI depends upon the baseline MCA PI. Subjects with MCA PI of 1.2 at baseline have a 0.34 increase with MH (p<0.001), while there was no significant increase at higher values (Figure 1B).
Conclusion:
In the 3rd trimester, the fetal response to MH varies with GA and resting cerebrovascularresistance. These data are consistent with the hypothesis that as cerebral oxygen demand increases during the 3rd trimester, oxygen delivery in the HLHS fetus may be inadequate.
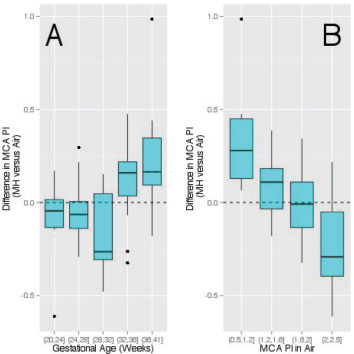
RESTING ENERGY EXPENDITURE IN INFANTS WITH SINGLE VENTRICLE CONGENITAL HEART DISEASE
Author links open overlay panelJeffrey B.AndersonMeganHorsleySuzanneSummerJessePrattEileenKingBradleyMarino
Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA
Background:
Infants with single ventricle congenital heart disease (SV) are at risk for early failure to thrive. The etiology of this failure is poorly understood and higher than normal energy expenditure has been theorized as a predictor of growth failure. We sought to measure resting energy expenditure (REE) in newborns with SV, compare these measurements to control subjects, and assess the relationship between REE and growth in the first months of life.
Methods:
We performed a prospective cohort/nested case-control study of infants with SV. Full term (>37 weeks) neonates with SV palliation at a single institution and age and gender-matched controls were included between 2010-2013. We excluded infants with chromosomalabnormalities, and major gastrointestinal, pulmonary or neurologic anomalies. REE was measured at neonatal discharge and weight-for-age z-score (WAZ) change was measured between neonatal discharge and presentation for cavopulmonary anastomosis. REE was compared between SV and control groups using an analysis of covariance model with age, gender, WAZ, length, and head circumference in the model as covariates. Pearson’s partial correlation coefficient was used to determine association between REE and WAZ change.
Results:
33 infants with SV and 26 control infants were included. The most common cardiac diagnoses in the SV group were hypoplastic left heart syndrome 18(55%) and double inlet left ventricle 5(15%). The SV and control groups were similar in gestational age, gender, and median age at the time of their REE measurements (24 vs. 25 days). The mean REE was not significantly different between the SV group (134.9 kcal/day) and the control group (139.5 kcal/day), p=0.61. Mean WAZ at the time of REE measurement was significantly lower in the SV group (-1.55 ± 1.2) than the control group (-0.17 ± 0.98), p<0.0001. There was no significant correlation between REE and WAZ changes (ρ=0.41, p=0.21, n=16).
Conclusion:
REE is similar in infants with SV at the time of discharge following initial surgical palliation compared to age and gender-matched controls. REE at neonatal discharge is not a good predictor of growth failure in the first months of life in infants with SV undergoing palliation.
PERIOPERATIVE PROGNOSTIC FACTORS FOR FONTAN PATIENTS UNDERGOING ORTHOTOPIC HEART TRANSPLANT
Author links open overlay panelChristopherBergBrentonBauerAbbieHagemanLeighReardon
David Geffen School of Medicine at UCLA, Los Angeles, CA, USA
Ahmanson/UCLA Adult Congenital Heart Disease Center, Los Angeles, CA, USA
Background:
Although the Fontan procedure offers a long-term palliative option for single-ventricle patients, orthotopic heart transplantation (OHT) remains the definitive treatment for a failing Fontan circuit. We hypothesized that there are a set of perioperative variables associated with increased risk of postoperative adverse outcomes.
Methods:
36 post-Fontan patients were identified as having undergone OHT at UCLA Medical Center from 1991 to 2014. Data was collected retrospectively and analyzed. The primary endpoint was designated as either: perioperative mortality, extended postoperative hospital stay (>30 days), or readmission within 2 weeks of discharge.
Results:
17 of 36 patients reached the primary endpoint; 8 patients suffered perioperative death after OHT, 6 patients experienced extended hospital stays, and 4 patients were readmitted within 2 weeks after discharge. Of the patients that suffered the primary outcome, 11 of these patients had an extended preoperative hospital stay (>10 days), 7 patients had an elevated MELD-XI score (≥18), and 8 patients had an extended perioperative cardiopulmonary bypass time (>4 hours). Patients with an elevated MELD-XI score (p=0.0128) or an extended cardiopulmonary bypass time (p=0.0002) carried a significantly higher risk of reaching the primary endpoint. A composite scoring system of eight criteria was used to stratify the risk of patients suffering the primary endpoint. Patients with scores of ≥3, 2, and 0-1 had a 91.1%, 33.3%, and 25% risk of reaching the primary endpoint, respectively. Patients with a score of ≥3 had a relative risk of 3.6 over patients with 0-1 points (95% CI, 1.53-8.67; p=0.0013).
Conclusion:
Failing Fontan patients undergoing OHT with elevated preoperative MELD-XI scores and/or extended perioperative cardiopulmonary bypass times are at greater risk of experiencing adverse outcomes after transplant. Additionally, a novel scoring system was devised for optimized risk stratification of suffering an adverse outcome after OHT, in which a score of ≥3 was predictive of poorer outcomes. This scoring system may allow for potential improvements in recipient evaluation during the listing process.
INVESTMENTS IN FATAL OUTCOMES IN THE INPATIENT CARE OF HYPOPLASTIC LEFT HEART SYNDROME
Author links open overlay panelShelbyKuttyQuentinKarelsAparnaKulkarniAyshaHassanYunbinXiaoMelHallDavidDanford
University of Nebraska Medical Center, Children’s Hospital and Medical Center, Omaha, NE, USA
Background:
Efforts to achieve durable survival in hypoplastic left heart syndrome (HLHS) through staged surgical palliation require sophisticated inpatient (inpt) care and are not always successful. Our purpose is to measure the investment of inpt care resources in this effort and determine how much of that investment takes place in hospitalizations that have a fatal outcome.
Methods:
The Pediatric Health Information System (PHIS) database representing 47 children’s hospitals was queried for HLHS admissions of patients (pts) <21 years old during 2004-2013. Institution, pt age, inpt deaths, billed charges (BC) and length of stay (LOS) were recorded.
Results:
In total, 11,122 HLHS admissions (mean 259±181 per institution) were identified which account for total LOS of 277,027 inpt-days and $3,928,794,660 in BC. There were 1145 inpt deaths (10.3%). Mean, interquartile range, and median were: for pt age 1.13, 0-2, and 0 years, for LOS 24.9, 6-29, and 12 days, and for BC 353,000 86,000-392,000, and 175,000 ($). LOS was greater among inpt deaths than among pts discharged alive (median 17 vs 12, p<0.0001). BC were greater among inpt deaths than among pts discharged alive (median 4.09×105 vs 1.64×105, p<0.0001). 16% of all LOS and 21% of all BC were accrued by pts who did not survive their hospitalization. These proportions show no significant change year by year.
Conclusion:
Investment of resources in inpt care of HLHS is high, disproportionately so among pts who do not survive their hospitalization, illustrating that inpt death in HLHS generally is neither swift nor inexpensive. Inpt death is a crude outcome marker, and may substantially underestimate the larger problem of investment in more general poor outcomes in HLHS manifested as early post-dismissal deaths and severe nonfatal morbidities. Nevertheless, these sobering data should alert providers and consumers that current practices often result in major resource expenditure for inpt care of HLHS which prove unsuccessful even in the short term. They highlight the need for data-driven critical review of standard practices to identify patterns of care associated with success in HLHS, and to modify approaches objectively.
THE ASSISTED BIDIRECTIONAL GLENN: AN IN VITRO AND IN SILICO STUDY OF A SURGICAL APPROACH FOR FIRST STAGE SINGLE VENTRICLE HEART PALLIATION
Author links open overlay panelRichardFigliolaMahdiEsmaily-MoghadamJianZhouTain-YenHsiaAlisonMarsden
Clemson University, Clemson, SC, USA
University of California, San Diego, San Diego, CA, USA
Background:
Outcomes following a modified Blalock-Taussig shunt (mBTS) in neonates with single ventricle physiology remain unsatisfactory. However, initial palliation with a superior cavopulmonary connection, such as a bidirectional Glenn, is discouraged due to concerns of inadequate pulmonary blood flow (PBF). We developed both experimental and numerical circulation models to test the feasibility of a novel surgical approach, whereby the flow in the bidirectional Glenn is ‘assisted’ by shunting high-energy flow from the systemic circulation.
Methods:
Realistic three-dimensional anatomical models of the neonatal mBTS and Glenn surgical sites were created and coupled with validated hydraulic multi-scale models of the complete circulation using parameters based on measurements from 23 single ventricle neonates. An ‘assisted’ bidirectional Glenn (ABG) model was also created and consisted of a shunt between the right innominate artery and superior vena cava (SVC) with a flow reducing clip near the SVC anastomosis to create a Venturi effect. Both in vitro and in silico studies were executed. Two values of pulmonary vascular resistance (PVR), normal and elevated (PVR = 2.3 and 7 WU), were tested.
Results:
The experimental and numerical results were in close agreement. The ABG provided the highest systemic oxygen saturation and oxygen delivery at both PVR levels. In addition to achieving nearly 30% higher PBF than the Glenn with 14% higher oxygen delivery than the mBTS, the ABG produced lower single ventricular workload than mBTS. SVC pressure was highest in the ABG model at high PVR (ABG:15, Glenn:11, mBTS: 3 mmHg), but at low PVR, the SVC pressure was significantly reduced (ABG:8, Glenn:6, mBTS: <3 mmHg). Experimental results using geometric variations, including shunt to venturi diameter ratio and shunt angle, show promise in lowering SVC pressures further.
Conclusion:
The ABG approach increases PBF with a modest increase in SVC and pulmonary arterial pressure. While the results demonstrate the conceptual feasibility of the ABG circulation with physical verification, further technical refinements including animal models are necessary.
LONG TERM OUTCOMES IN DOUBLE INLET LEFT VENTRICLE AND TRICUSPID ATRESIA WITH TRANSPOSED GREAT VESSELS
Author links open overlay panelDavid S.WinlawLotteFrankenManoukAdmiraalJulianAyerAjayIyengarAndrewColeChristianBrizardGaryShollerYvesd’Udekem
The Children’s Hospital at Westmead, Sydney, Australia
Royal Children’s Hospital, Melbourne, Australia
Background:
In patients with tricuspid atresia and transposed great vessels (TA-TGA) and double inlet left ventricle (DILV), the presence of systemic outflow tract obstruction and aortic archobstruction has led to varied surgical approaches including Norwood palliation or initial pulmonary artery banding with arch repair. TA-TGA has been previously shown to be associated with a worse outcome compared to a diagnosis of DILV. We sought to identify contributing factors in both the pre and post Fontan periods and define long-term outcomes. Pre and post Fontan outcomes have not previously been reported in the same patient cohort.
Methods:
214 patients were identified, 61 with TA-TGA and 153 with DILV via departmental databases and the ANZ Fontan Registry, representing the largest population-based series studied to date. Details of initial and subsequent surgical interventions and mortality were recorded. Mean post-natal follow-up was 17.4 years and similar for both groups.
Results:
Survival for the whole group was 90.2, 87.3, 84.4, 83.2 and 83.2% for 5, 10, 15, 20 and 25 years respectively, with TA-TGA faring worse than DILV (mortality 30.3% vs. 18.5%, p<0.01 at 4 years). Peri-procedural mortality accounted for the majority of the pre-Fontan deaths. There was no difference in the number of patients requiring arch reconstruction in each group. 81.6% achieved a Fontan with a higher likelihood of achieving Fontan for DILV than TA-TGA (89.9% vs. 59.6%, p = 0.02). After Fontan completion there were 8 deaths (4%). Choice of initial surgical palliation (PA band vs. Norwood) did not influence outcome.
Conclusion:
Patients with TA-TGA and DILV continue to present surgical and management challenges Survival has improved survival compared to previous smaller series, long term outcomes are determined by the quality of pre-Fontan management and differences in risk according to morphology relate to the pre-Fontan era and do not persist into the long term.
DIASTOLIC DYSFUNCTION BY DOPPLER ECHOCARDIOGRAM IS ASSOCIATED WITH MAJOR ADVERSE EVENTS IN ADULT FONTAN PATIENTS
Author links open overlay panelMakotoMoriKayokoShiodaMariaPernetzRobertElderAliciaRangoschWendyBookFredRodriguezAnuragSahuBrianKogonMichaelMcConnellCamdenHebsonMaanJokhadar
Emory University School of Medicine, Division of Cardiology, Atlanta, GA, USA
Yale School of Medicine, New Haven, CT, USA
Background:
Diastolic dysfunction severity is a well-established prognostic marker in the general population. Little is known about diastolic dysfunction severity as a prognostic marker in Fontan patients. This study evaluates correlation between diastolic function parameters and adverse events in Fontan patients with long-term follow-up.
Methods:
Retrospective review of pulsed-wave Doppler data in 104 adult Fontan patients between 2005-2014 was conducted. Dominant atrioventricular (AV) valvular flow and free-wall tissue Doppler were measured. Patients with prosthetic AV valve were excluded. Survival analysis was performed to analyze the association between adverse events (death, heart transplantation) and diastolic variables (E, e’, E/e’ ratio, and myocardial performance index (MPI)). Diastolic variables were compared by dominant ventricle type using two-sample t-test.
Results:
104 post-Fontan adult patients (71% systemic left ventricle, 72% lateral tunnel Fontan, age 27.2±7.0 years, time since Fontan operation 21.5±5.2 years) were analyzed. There were 18 adverse evens: 9 deaths, 9 transplants. Adjusting for potential confounders including dominant ventricular morphology and Fontan type, survival analysis demonstrated significant association between peak E wave velocity and major adverse event: hazard ratio=1.9 [95%CI 1.03-3.38], p=0.033. MPI, e’, or E/e’ ratio was not significantly associated with events. Means of the following variables were compared between patients with right vs. left dominant ventricles: E velocity was 67±58 vs. 69±62 cm/sec (p=0.8), e’ velocity was 7.6±3.0 vs. 9.3±2.9 cm/sec (p=0.02), E/e’ ratio was 10.1±5.3 vs 7.8±3.6 (p=0.06), and MPI was 0.63±0.32 vs 0.54±0.19 (p=0.2).
Conclusion:
Diastolic dysfunction by Doppler is characterized for the first time in adult Fontan population. Increase in E wave velocity was associated with increased risk of death or need for heart transplantation. Comparing left and right ventricle, right dominant ventricle manifested with lower e’ velocity.
BLOOD PRESSURE IN ADULT PATIENTS WITH CONGENITAL HEART DISEASE
Author links open overlay panelTomoakiMurakamiHironobuKobayashiHirokiNagamineKazuhiroShiragaShojiFukuokaHigashiKojiShigeruTatenoKawasoeYasutakaNakajimaHiromichiHiroyukiAotsukaKoichiroNiwa
Chiba Children’s Hospital, Chiba, Japan
Chiba Cardiovascular Center, Ichihara, Japan
Background:
We previously reported that the incidence of hypertension in adult patient with congenital heart disease (CHD) is almost same as that in general population. However, it could be underestimated, because the patients are still young. Moreover, we also reported that the surgical intervention for aortic arch increases pressure wave reflection, which would elevate BP. Therefore, we compared the brachial systolic BP (SBP) and the reflected wave blood pressure (SBP2) in adult patients with CHD with those in each age decade of general population.
Methods:
This study enrolled 100 adult patients with CHD. The brachial SBP and SBP2 were measured by HEM-9000AI (Omron Healthcare Co., LTD., Kyoto, Japan). The SBP and SBP2 were compared with those by age and gender in general population (Hypertens Res 2013;36:50-57). A patient whose brachial SBP/diastolic BP was over 140/90 mmHg was diagnosed as hypertension. A patient whose SBP/SBP2 was over 2SD (= 2.3%) of those by age and gender in general population was defined as high SBP/SBP2.
Results:
The patients’ age was 37.0 ± 15.0 years (20 – 76). NYHA class of the patients was I:68, II:25, III:7, IV:0. Sixteen patients were suffered from cyanosis (SpO2<95%) and their BNP was 69.7 ± 152.5 pg/ml. The SBP was 117.7 ± 20.1 mmHg and SBP2 was 105.8 ± 20.2 mmHg. Thirteen patients were diagnosed as hypertension. Twenty patients were defined as high SBP (20%) and 22 patients were defined as high SBP2 (22%).
Conclusion:
The incidence of high SBP/SBP2 in adult patients with CHD is high. Early intervention would be essential in order to avoid increment of pressure load for systemic ventricle that has been variously loaded from birth.
COARCTATION MAY BE ASSOCIATED WITH MORE RAPID AORTIC DILATION IN INDIVIDUALS WITH BICUSPID AORTIC VALVE: INSIGHTS FROM THE GENTAC REGISTRY
Author links open overlay panelMariaYatesClaudiaPedrozaWeiluHanFedericoAschGenTACConsortiumSiddharthPrakash
University of Texas Health Sciences Center at Houston, Houston, TX, USA
Background:
Bicuspid aortic valve (BAV) is associated with thoracic aortic aneurysms and dissections. The prevalence of aortic coarctation is increased in patients with BAV. We hypothesize that patients with coarctation are at increased risk for aortic complications compared to those with isolated BAV and may benefit from more intensive surveillance. We therefore compared of aortic dilation at the sinuses of Valsalva and ascending aorta in BAV subjects with and without coarctation.
Methods:
Individuals with BAV +/- coarctation were selected from the National Registry of Genetically Triggered Thoracic Aortic Aneurysms and Cardiovascular Conditions (GenTAC). Genetic syndromes were excluded. Longitudinal regression models were used to evaluate the average annual change in aortic root or ascending aortic diameters after adjustment for age, sex, BSA and previous cardiac surgery.
Results:
We included 468 subjects (49 with coarctation): 24% female, mean age 41 (IQR 25-56), mean BSA 2.15 m2 (IQR 1.73-2.10). Seventy-three subjects had multiple images with a mean interval of 1.84 years (IQR 0.9-2.42). Subjects with coarctation were significantly younger, more likely to be female and had smaller aortic diameters at baseline. The mean dilation rate of the sinuses and ascending aorta were both 1 mm/year. Rates of dilation at the sinuses (+2.4 mm/year) and ascending aorta (+2.6 mm/year) were more rapid in subjects with coarctation than in those with isolated BAV, but were not statistically significant (minimum P=0.35). These findings were similar when percent change in aortic diameter was substituted as the primary endpoint. Prior cardiac surgeries other than coarctation repairs were similar between groups and were not associated with aortic diameter or growth rate.
Conclusion:
Coarctation may be associated with increased rates of aortic dilation in BAV patients. Limitations of this study include the sparsity of data points and brief follow up intervals, as well as incomplete data on valve configuration, coarctation anatomy and surgical repair. Our results suggest that individuals with BAV and coarctation may be at increased risk for aortic complications and merit validation in larger studies.
CMR DERIVED CENTRAL AORTIC SYSTOLIC PRESSURE IS A SUPERIOR PREDICTOR OF AFTERLOAD IN REPAIRED COARCTATION
Author links open overlay panelMichael AlexanderQuailRebekahShortBejalPandyaJenniferSteedenAndrew M.TaylorVivekMuthurangu
University College London, Institute of Cardiovascular Science, London, United Kingdom
Background:
Hypertension is one of the major causes of late mortality in patients with repaired coarctationof the aorta (CoA) even in the absence of significant recoarctation. However, brachial systolic pressure (BSP) may not accurately reflect central systolic pressure (CASP), which is the driver of pathology. Recently, it has been shown that it is possible to accurately estimate CASP using CMR data and a simple exponential model of the arterial pressure-area relationship. The aims of this study were i) To demonstrate that it is feasible to measure CASP in patients with CoA and ii) To demonstrate that CASP is a better indicator of afterloadrepresented by increased LV mass (LVM); compared with conventional metrics, such as coarctation index (CI) and BSP.
Methods:
50 subjects, 34 patients with repaired CoA, mean age 28±2yrs (76% male) and 16 healthy controls, 25±2yrs (69% male) were recruited. Ascending aorta area curves were obtained using a spiral phase-contrast CMR flow sequence. CASP was derived by calibrating area curves to, brachial oscillometric, mean and diastolic pressures using a validated exponential pressure-area model. LVM was obtained using cine CMR and CI was measured from 3D angiographic data. The determinants of LVM index were assessed using multivariable linear regression analysis.
Results:
Differences between patients and controls were more significant with CASP (117±2 vs 104±2mmHg, p=0.0003) than BSP (126±3 vs 116±3mmHg, p=0.02). There were no differences between patients and controls in mean or diastolic blood pressure. LVM index was higher in patients 75.2±2.8g/m2 compared to controls 60.7±2.2g/m2, p=0.0002. In CoA patients, only gender (β=0.5, p=0.003) and CASP (β=0.4, p=0.008) were independently associated with LVM index, model R=0.69. Importantly, there were no independent associations of LVM index with BSP or CI.
Conclusion:
In this study we have shown that noninvasive CASP is an important biomarker for increased afterload following CoA repair. Importantly, conventional metrics, CI and BSP were not independently associated with LVM in this study. CASP may represent a superior target for cardiovascular risk reduction in this condition and is easily measured using CMR.
INCIDENCE AND CLINICAL PRESENTATION OF KOMMERELL DIVERTICULUM AND ANEURYSM
Author links open overlay panelJosephPoteruchaNandanAnavekarTalhaNiazAnushreeAgarwalPhillipYoungJosephDearaniNaserAmmashCaroleWarnesHeidiConnolly
Mayo Clinic College of Medicine, Rochester, MN, USA
Background:
There are limited data on incidence of Kommerell diverticulum (KD) and aneurysm (KA). We aimed to report the incidence and clinical presentation of KD and KA; and determine risk factors for development of KA.
Methods:
The Mayo Clinic radiology database was retrospectively analyzed to identify pts with aberrant subclavian artery from 1990-2014. Images were analyzed by two independent blinded reviewers to determine presence of KD and KA and clinical data was reviewed.
Results:
Demographic and clinical data are shown (Table). 863 pts with aberrant subclavian arterywere identified. Incidence of KD was 121/863 (14%) and KA was 28/863 (3%). 61% of KD pts were symptomatic including dysphagia (52%), dyspnea (34%), atypical chest pain (27%) and cough (26%). KA was present in 28/121 pts (23%). Esophageal spasm (p =0.001) and thoracic aortic aneurysm (p = 0.01) was more common in KA than KD. Univariate risk factors for KA formation were left aortic arch (AA) (p = 0.02); abdominal aortic aneurysm (p = 0.03); thoracic aortic aneurysm (TAA) (p = 0.001); esophageal spasm (p = 0.0003); and atypical chest pain (p = 0.03). Multivariate risk factors for KA formation were TAA (R = 0.33, OR = 20, p = 0.003) and left AA (R = 0.33, OR = 3, p = 0.02).
Conclusion:
This is the largest reported study on incidence and clinical presentation of pts with KD and KA. Common presenting symptoms were dysphagia, disordered sleep, dyspnea, atypical chest pain, and cough. Pts with KD as well as TAA and left AA should be screened for subsequent KA formation.
| All pts with KD | KD alone | KA | p | |
| (n = 121) | (n = 93) | (n = 28) | ||
| Demographics | ||||
| Age (years) | 50 ± 22 | 48 ± 22 | 57 ± 25 | NS |
| Male | 50 (41%) | 41 (44%) | 9 (32%) | NS |
| CAD | 14 (11%) | 10 (11%) | 4 (14%) | NS |
| Previous MI | 5 (4%) | 4 (4%) | 1 (4%) | NS |
| PVD | 6 (5%) | 5 (5%) | 1(4%) | NS |
| AAA | 5 (4%) | 2 (2%) | 3 (11%) | 0.08 |
| TAA | 5 (4%) | 1 (1%) | 4 (14%) | 0.01 |
| HTN | 48 (40%) | 36 (39%) | 12 (43%) | NS |
| HLP | 43 (36%) | 30 (32%) | 13 (46%) | NS |
| Diabetes | 13 (11%) | 10 (11%) | 3 (11%) | NS |
| Smoking | 29 (24%) | 21 (23%) | 8 (28%) | NS |
| Connective tissue disorder | 4 (3%) | 3 (3%) | 1 (4%) | NS |
| Anatomical Presentation | ||||
| Right aortic arch with left ASA | 73/121 (60%) | 60/93 (65%) | 13/28 (46%) | 0.1 |
| Left aortic arch with right ASA | 47/121 (39%) | 32/93 (34%) | 15/28 (54%) | 0.08 |
| Clinical Presentation | ||||
| Symptomatic Patients | 74/121 (61%) | 54/93 (58%) | 20/28 (71%) | 0.0001 |
| Symptoms | ||||
| Dysphagia | 39 (52%) | 30 (56%) | 9 (45%) | NS |
| Dyspnea | 25 (34%) | 20 (37%) | 5 (25%) | NS |
| Atypical Chest Pain | 20 (27%) | 12 (22%) | 8 (40%) | NS |
| Chronic cough | 19 (26%) | 13 (24%) | 6 (30%) | NS |
| Recurrent respiratory infections | 7 (9%) | 6 (11%) | 1 (5%) | NS |
| Hoarseness | 6 (8%) | 3 (6%) | 3 (15%) | NS |
| Choking spells | 6 (8%) | 3 (6%) | 3 (15%) | NS |
| Upper extremity claudication | 5 (7%) | 4 (7%) | 1 (5%) | NS |
| Esophageal spasms | 5 (7%) | 0 (0%) | 5 (25%) | 0.001 |
| Wheezing | 4 (5%) | 4 (7%) | 0 (0%) | NS |
| Weight Loss | 3 (4%) | 3 (6%) | 0 (0%) | NS |
KD, Kommerell diverticulum; KA, Kommerell aneurysm; CAD, coronary artery disease; MI, myocardial infarction; PVD, peripheral vascular disease; AAA, abdominal aortic aneurysm; thoracic aortic aneurysm; HTN, hypertension; HLP, hyperlipidemia; ASA, Aberrant subclavian artery
USE OF LARGE DIAMETER STENTS WITH MAXIMAL EXPANSION LIMITS RE-INTERVENTION IN TREATMENT OF NATIVE COARCTATION OF THE AORTA
Author links open overlay panelBrendan McCluskeySmithFranciscoGuzman-PrunedaCarlosMeryHenriJustinoAtharQureshiDhavalParekh
Texas Children’s Hospital, Houston, TX, USA
Background:
Questions remain regarding reintervention after percutaneous stent placement for native coarctation of the aorta (CoA). We describe our experience.
Methods:
All pts with native CoA treated with stent placement between 1997 and 2013 at our institution were included. Records prior to intervention and during follow-up were reviewed.
Results:
38 pts (32% female) were identified. Median age at intervention: 12.3 yrs (2-51.7 yrs), median weight: 43.7 kg (14.4-92kg). All pts had a left aortic arch with juxtaductal CoA. No periprocedural or late mortality occurred. No cases required ICU admission post-intervention. Periprocedural complications occurred in 2 pts: 1 stroke and 1 aneurysm at the stent site. Median follow-up: 3.9 yrs (8 days-10.9 yrs). 12 (%) pts required reintervention at a median of 3.5 yrs (0.9-5.45 yrs) after index procedure. Pts with stents placed before age 12 accounted for 75% of re-interventions performed to allow for somatic growth. 3 (%) pts less than 12 yrs had unplanned reintervention due to aneurysms. Stents with expandable diameter >18 mm were used in 33/38 patients. 3/5 (60%) of pts with smaller stents and 9/33 (27%) patients with larger stents required reintervention.
Complete Series, Age 2-51 yrs (n=38)
| Pre-intervention | Post-intervention | p-value | |
| Median SBP gradient at catheterization | 33.5 mmHg (8-82) | 3.0 mmHg (0-10) | <.01 |
| Mean ratio of CoA segment diameter: descending Aorta at diaphragm | 0.31 (+/-0.14) | 0.88 (+/-0.18) | <.01 |
| Presentation | Last follow-up visit | p-value | |
| Median 4 extremity SBP gradient | 38.5 mmHg (2-91) | 0.5 mmHg (0-16) | <.01 |
| pts hypertensive (SBP >95th percentile) | 34/36 (94 %) | 10/18 (56%) | |
| Re-intervention during follow-up | |||
| <12 years (n=19) | >12 years (n=19) | p-value | |
| Planned (staged or somatic growth) | 8/19 (42%) | 1/19 (5 %) | <.01 |
| Un-planned | 3/19 (16%) | 0/19 | NS |
| Total | 11/19 (58%) | 1/19 (5%) | |
SBP: systolic blood pressure
Conclusion:
Use of stents expandable to a diameter of >18mm and efforts to achieve a dilated diameter approximate to the descending aorta diameter at the diaphragm may limit the frequency of re-interventions in patients treated for native CoA. Planned and un-planned re-interventions increased under age 12.
TRICUSPID REGURGITATION IMPROVES BUT RIGHT VENTRICULAR FUNCTION DOES NOT AFTER REPAIR OF PRE-TRICUSPID VALVE LEFT-TO-RIGHT SHUNTS
Author links open overlay panelAsad A.ShahAlexisAntunezAndrewLodge
Duke University Medical Center, Durham, NC, USA
Background:
Tricuspid valve regurgitation (TR) is not uncommon in patients with pre-tricuspid valve left-to-right shunts, such as atrial septal defects and partial anomalous pulmonary venous connections. However, the natural history of unrepaired TR after repair of these shunts is not well described. The primary objective of this study was to determine whether unrepaired significant TR improved after correction of the primary defect.
Methods:
All patients with preoperative moderate or severe TR undergoing repair of a pre-tricuspid valve left-to-right shunt (without a procedure on the tricuspid valve) at a single institution between 1992 and 2012 were included. A retrospective chart review was conducted to examine patient characteristics, echocardiographic data, and post-operative outcomes.
Results:
Of 638 patients who underwent repair of a pre-tricuspid valve left-to-right shunt, 34 had moderate or severe TR preoperatively. Procedures included repair of atrial septal defects(26), partial atrioventricular canal defects (4), partial anomalous pulmonary venous connections (2), and others (2). Mean age was 38±15 years. Mean TR gradient improved from 51±15 preoperatively to 29±9 postoperatively (P<0.001). Overall, TR was improved in 24 patients, stable in 2, worse in 1, and unknown in 7. Right ventricular (RV) function failed to improve in 7 of 11 of patients with preoperative RV dysfunction.
Conclusion:
Moderate and severe TR improves without direct intervention in the majority of patients undergoing repair of pre-tricuspid valve left-to-right shunts. However, RV dysfunction does not improve in most patients. Further studies investigating risk factors for lack of improvement of TR and RV function are warranted.
PERCUTANEOUS PATENT FORAMEN OVALE OR ATRIAL SEPTAL DEFECT CLOSURE IN IMMUNOCOMPROMISED PATIENTS
Author links open overlay panelSubrataKarJamilAboulhosnAnwarTandarRubineGevorgyanNicholasMillerJonathanTobis
UCLA Medical Center, Division of Interventional Cardiology, Los Angeles, CA, USA
Background:
The safety of Patent foramen ovale (PFO) or atrial septal defect (ASD) percutaneous closure in immunosuppressed patients or with autoimmune disease is unknown. We attempted to determine if closure is safe in such patients.
Methods:
A prospective observational multicenter study was performed in 24 patients who were immunocompromised or had autoimmune disease from vasculitis, Human Immunodeficiency Virus (HIV), hepatitis, cancer, or renal transplant and underwent percutaneous PFO or ASD closure for cryptogenic stroke (9, 38%), desaturation (5, 21%), migraine (7, 29%), or a combination of these diagnoses (3, 13%). Post procedure follow-up included clinic evaluation in 3-6 months or telephone questionnaire up to 8 years (21 ± 28 months).
Results:
Of the 24 patients (53 ± 14 years), 19 had a PFO (79%), 5 had an ASD (21%), and 21 underwent closure (88%). No patient reported endocarditis, device erosion, exacerbation of migraine, or recurrent stroke. Only 1 patient in the PFO group (4%) experienced a transient neurologic deficit after closure. Of the 7 who had migraine prior to closure, 4 (57%) reported resolution of migraines. For patients who were unreachable for phone interview, mortality status was verified by the social security death index and revealed 5 deaths which were related to non-cardiac conditions in 3 cases (1 of these patients did not receive a device), 1 from metastatic pancreatic cancer, and 1 was unknown in a 77 year old woman who did not receive a device.
Conclusion:
Percutaneous PFO or ASD closure can be safely performed in patients who are immunocompromised or have autoimmune disease and suffer from clinical conditions associated with a septal defect.
IBUPROFEN FOR CLOSURE OF THE PATENT ARTERIAL DUCT IN PRETERM INFANTS
Author links open overlay panelRohit SethLoombaAndrewPelech
Children’s Hospital of Wisconsin, Milwaukee, WI, USA
Background:
Premature infants are at high risk of having persistence of ductal patency which may lead to volume overload of the pulmonary vascular bed and the left heart. Indomethacin has been utilized as an alternative to surgical ligation of patent arterial ducts but has been associated with adverse events such as bronchopulmonary dysplasia, necrotizing enterocolitis, and renal dysfunction. Ibuprofen has been suggested as a potentially safer alternative.
Methods:
A systematic review of the literature was conducted to identify studies comparing the use of ibuprofen or indomethacin for closure of patent arterial duct in preterm infants. Baseline characteristics of these studies was compared and a meta-analysis conducted. The primary was point was ductal closure with secondary end points examining potential adverse effects. Analysis was conducted separately for different routes of ibuprofen and indomethacin administration: oral versus oral, oral versus intravenous, and intravenous versus intravenous.
Results:
A total of 22 studies with 1,583 patients were included in the analysis. There was no difference noted in ductal closure rates between ibuprofen and indomethacin for comparable routes of administration as well as when oral ibuprofen was compared to intravenous indomethacin. When comparing oral ibuprofen versus oral indomethacin and intravenous ibuprofen versus intravenous indomethacin there was an association with less increase in creatinine with ibuprofen. No other significant differences iin adverse effects were noted.
Conclusion:
Oral or intravenous ibuprofen is equally effective in closing the preterm arterial duct as either oral or intravenous indomethacin. Indomethacin is associated with less increase in creatinine, thus making it a safe and effective alternative.
TAILORED CIRCULATORY INTERVENTION IN ADULTS WITH PULMONARY HYPERTENSION DUE TO CONGENITAL HEART DISEASE
Author links open overlay panelLotteCouperusIvoHenkensHubertVliegenMarkHazekampMartinSchalij
LUMC, Leiden, The Netherlands
Background:
Adult congenital heart disease (CHD) patients with pulmonary hypertension (PH) often have residual shunts. Interventions aim to optimize pulmonary flow and prevent right ventricular(RV) failure. However, eligibility for procedures depends on adaptation potential of pulmonary vasculature and right ventricle to circulatory changes. Guidelines are not sufficiently applicable to individual patients, who exhibit great diversity in cardiac disease.
Methods:
We present four adult complex CHD-PH patients with ambiguous indication for shunt adjustment. The first patient with Fallots’ tetralogy developed RV dilatation after recanalization of a Potts’ shunt that was re-closed through percutaneous aortic stenting. The second and third patient had backgrounds of palliative surgery for pulmonary atresia and ventricular septum defect (VSD). One patient underwent fenestrated VSD closure and pulmonary stenting, the other underwent an atrioseptostomy to relieve RV overload. The last patient had a monoventricular circulation and severe mitral stenosis that resulted in pulmonary venous congestion and inotropic dependence, for which an atrioseptostomy was performed.
Results:
Tailored intervention improved right heart hemodynamics and short term clinical functioning in all cases.
Conclusion:
Individual evaluation of disease characteristics is mandatory for tailored treatment. Strict registration of cases and multicenter cooperation are essential in the quest for optimal therapy.
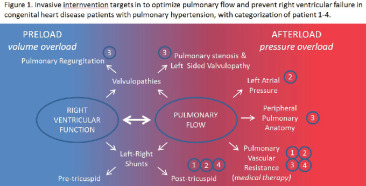
DO ANGIOTENSIN RECEPTOR BLOCKERS SLOW PROGRESSION OF AORTIC ROOT DILATION IN MARFAN’S SYNDROME?
Author links open overlay panelMehakIdreesMuhammad ShahzebKhanJahanzaibIdreesHarisRiaz
Cleveland Clinic, Cleveland, OH, USA
Dow University of Health Sciences, Karachi, Pakistan
Background:
Angiotensin receptor blockers (ARB’s) have been hypothesized to slow the progression of aortic root dilatation in Marfan’s syndrome (MFS) by virtue of decreasing transforming growth factor beta (TGF-B), the critical mediator in pathogenesis. We pooled the existing data from the prospective studies to determine if the relationship is significant.
Methods:
PubMed was searched from 1990 till present to identify prospective studies of patients with MFS in which ARBs are used as intervention. Further inclusion criteria included a follow up of at least six months and the presence of a control group. Random effects model using standardized mean difference (SMD) was created to pool the aggregate data and I2 testing was done to ascertain heterogeneity.
Results:
A total of 122 titles were screened after which 20 abstracts were considered. Out of the 5 studies identified, 2 were excluded because of the concomitant use of other interventions. Pooled overall estimates (3 studies, 94 patients) suggest that the use of ARB’s significantly slows the progression of aortic root dilatation SMD= -1.86(95% CI=-0.24 to -3.84). There was significant heterogeneity (93%) among the included studies.
Conclusion:
Use of ARB’s in MFS is associated with a significant decrease in the progression of aortic root dilatation. The results are limited by the small number of studies, statistical heterogeneity, limited duration of follow up and lack of hard clinical end points. Further studies are needed to address these limitations.
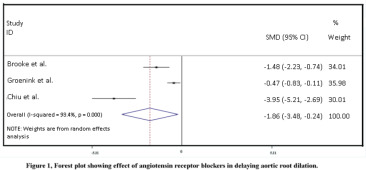
MUSTARD/SENNING OPERATION: IT IS NOT ALL “FLUTTER” ANYMORE
Author links open overlay panelElisaBradleyAliZaidiJustinMorrisonCurtisDanielsStevenKalbfleischNaomiKertesz
Nationwide Children’s Hospital, Columbus, OH, USA
The Ohio State University, Columbus, OH, USA
Background:
Complex inter-atrial baffling (Mustard/Senning operation) is a risk factor for late atrialtachyarrhythmias. We aim to characterize the source of arrhythmia, short-term RFA success, and medium-term freedom from clinically significant arrhythmia with a combined pediatric-adult EP team utilizing transbaffle access (TBA) techniques in adult patients.
Methods:
We conducted a retrospective review of consecutive adults >18 yrs of age with a prior atrialswitch operation undergoing a clinically indicated electrophysiology study (EPS) over 1 year (2013-2014). Short-term success was analyzed at 1 month and medium-term results 6 months post EPS.
Results:
Eleven patients (34 + 9 yrs, 64% men, systemic EF 37+ 8%, NYHA functional class 1.6 + 0.6) underwent an EPS. At baseline, 9 patients were taking a beta-blocker, 3 were on anti-arrhythmics, and 2 were taking digoxin. There were 12 clinically significant inducible arrhythmias in 10 patients (1 EPS cancelled: thyroid storm) who underwent 12 EPS. The most common clinically significant inducible arrhythmia was IART, which occurred in 6 (50%) EPS, followed by AVNRT (n=4, 33%) and nonautomatic focal atrial tachycardia (NAFAT) (n=2, 17%). Four patients (36%) had more than one arrhythmia, two of which required RFA for >1 arrhythmia. At the time of EPS, TBA was required in the majority of cases (n=10, 83%). The short-term success rate was 92% due to one patient with recurrent IART 12 hours after RFA. In the medium-term, 6 patients with 7 RFA (58%) remained free of clinical recurrence. Of those, there was no difference in the type of arrhythmia found at the time of EPS (IART n=3, NAFAT=2, AVNRT n=2). In the 4 patients that experienced recurrent arrhythmia, the majority (n=3) responded to medical therapy.
Conclusion:
This is the largest 1-year, single-center, cohort of adult atrial switch patients who underwent an EPS by a combined pediatric-adult EP team. We demonstrate a diverse arrhythmic substrate and highlight that IART is not always the source of clinically significant arrhythmia in this group. A combined team approach with a TBA technique offers excellent short-term success, with about half of patients remaining free of arrhythmia at medium-term follow-up.
ARRHYTHMIAS AND ASSOCIATED OUTCOMES IN ADULTS WITH CONGENITAL HEART DISEASE IN THE UNITED STATES
Author links open overlay panelDhavalKolteSahilKheraPrakashHarikrishnanChandrasekarPalaniswamyMarjanMujibWilbertAronowDiwakarJainSachinSuleAliAhmedWilliamFrishmanHowardCooperJasonJacobsonSeiIwaiGreggFonarowJulioPanza
New York Medical College, Valhalla, NY, USA
Background:
The number of hospitalizations for adults with congenital heart diseases (CHD) in the United States (U.S.) has increased over the past years. Arrhythmias are common in patients with CHD. However, data on the epidemiology of arrhythmias and associated outcomes in adults with CHD are limited.
Methods:
We used the 2002-2011 Nationwide Inpatient Sample databases to identify patients ≥18 years of age who had ICD-9-CM codes 745-747 (except 746.87, 746.89, 746.9, 747.5, 747.6, 747.8 and 747.9) for CHD. CHD were classified as simple or complex. Various arrhythmias were identified using appropriate ICD-9-CM codes. Association between arrhythmias and in-hospital outcomes (mortality, length of stay, total hospital charges) was examined using multivariable logistic or linear regression models.
Results:
From 2002 to 2011, of 777,718 adults with CHD (73.3% simple and 26.7% complex) admitted to U.S. hospitals, 24.5% had tachyarrhythmias, 7.7% had conduction disorders, and 28.8% had any arrhythmia. Serious arrhythmias or conduction disorders (ventricular tachycardia/fibrillation, Mobitz type II second-degree heart block, complete heart block, and left bundle branch block) occurred in 4.9% of adults with CHD. Arrhythmias were more common in adults with complex CHD than those with simple CHD (34.9% vs. 26.6%, p<0.001). The proportion of adults with CHD who had arrhythmias increased from 26.3% in 2002 to 31.8% in 2011 (ptrend<0.001). Similar trend was seen in adults with simple and complex CHD. Adult CHD patients with arrhythmias had significantly higher risk-adjusted in-hospital mortality (3.4% vs. 1.9%, adjusted OR 1.17, 95% CI 1.09-1.27), length of stay (7.2 vs. 5.5 days, adjusted OR 1.15, 95% CI 1.14-1.16) and total hospital charges ($76,714 vs. $48,767, adjusted OR 1.30, 95% CI 1.29-1.32) as compared to those without any arrhythmias. Similar results were seen in adults with simple and complex CHD.
Conclusion:
More than one-fourth of hospitalized adults with CHD have arrhythmias and this proportion has increased over the past several years. Arrhythmias contribute significantly to increased in-hospital mortality, length of stay, and total hospital charges in adults with CHD.
SEVERE LOSS-OF-FUNCTION SCN5A MUTATIONS ASSOCIATED WITH SINUS NODE DYSFUNCTION, ATRIAL ARRHYTHMIAS, AND POOR PACEMAKER CAPTURE
Author links open overlay panelDavidChiangJeffreyKimSantiagoValdesCaridadDe La UzYuxinFanChristinaMiyake
Baylor College of Medicine, Houston, TX, USA
Texas Children’s Hospital, Houston, TX, USA
Background:
Mutations in the SCN5A gene, which encodes the NaV1.5 channel, have been implicated in inheritable cardiac diseases, primarily long QT and Brugada syndromes. We now report an association between severe SCN5A mutations, sinus node dysfunction, atrial arrhythmiasand poor pacemaker capture.
Methods:
A retrospective chart review of all SCN5A mutations at a single center was conducted. Patients with a diagnosis of Brugada or long QT syndrome were excluded.
Results:
There were a total of 23 patients with SCN5A mutations, 15 of whom had a definitive diagnosis of Brugada or long QT syndrome. Of the remaining 8 patients, 7 were diagnosed with sinus node dysfunction, atrial arrhythmias, and poor pacemaker capture either in the atria, ventricles or both. In all 7 patients, inability to capture myocardium or excessive capture thresholds was found at pacemaker implant. Capture thresholds have remained elevated in all; however some patients have demonstrated a waxing and waning course with intermittent complete loss of capture resulting in syncope. Genetic testing revealed 6 distinct SCN5A mutations, one of which has never been previously reported. Bioinformatic analysis and literature review demonstrated: 1) a frame-shift mutation leading to an early stop codon and protein truncation, 2) a splice site mutation resulting in inclusion of an intron which then lead to early stop codon and protein truncation, 3) missense mutation resulting in a protein trafficking defect, and 4) missense mutations that may affect either NaV1.5 activation or inactivation or both. Together, all of these 6 SCN5A mutations are predicted to result in severely compromised or complete ablation of NaV1.5 function, albeit via distinct molecular mechanisms.
Conclusion:
This is the first series of poor pacemaker capture associated with SCN5A mutations. Significant decreases in NaV1.5 function appear to be involved in fluctuating capture thresholds and intermittent complete loss of pacemaker capture. Recognition of this association in a subset of patients with SCN5A mutations will be important for future management.
A PROSPECTIVE STUDY OF THE IMPACT OF MELODY VALVE IMPLANT ON THE FREQUENCY OF ARRHYTHMIAS DURING EXERCISE TESTING
Author links open overlay panelBryantPriromprintrMichaelSilkaJonathanRhodesAnjanBatra
Children’s Hospital of Los Angeles, Los Angeles, CA, USA
Children’s Hospital of Orange County, Orange, CA, USA
Background:
Percutaneous pulmonary valve implant (Melody) for conduit related pulmonary stenosis (PS) or pulmonary insufficiency (PI) has gained rapid acceptance. However, objective data regarding the benefit of this therapy with regard to the incidence of arrhythmias remains limited.
Methods:
As part of the phase I Melody valve clinical trial, 141 patients with congenital heart diseaseunderwent serial cardiopulmonary exercise testing (CPET) prior to and 6 months post implant. Arrhythmias during CPET were defined as premature ventricular contractions(PVCs) and supraventricular or ventricular tachycardia (VT). The most common anatomic subtypes were tetralogy of Fallot, aortic stenosis (post Ross procedure) and transposition variants. The mean age at implantation was 22.4±0.9 years, range 7-53 years.
Results:
Prior to Melody implant, PVC’s were common, occurring in 57 (40%) of the patients. While no subjects had sustained arrhythmias, 2 had non-sustained VT and 3 had non-sustained supraventricular tachycardia. Following Melody implant, there was no significant change in the incidence or type of arrhythmias during exercise: 38 patients (27%) had PVCs during CPET both pre and post implant, 19 patients (14%) who had PVCs pre implant did not have PVCs post implant, whereas 22 pts (16%) who did not have PVCs pre-implant did have PVCs post implant. No patient had supraventricular tachycardia and 1 different patient had non-sustained VT post implant. Subgroup analysis of PS or PI (or mixed), anatomic sub-type, and pre-implantation right ventricular dimensions did not demonstrate a significant benefit for Melody valve implant. Although right ventricular function and volume were improved following implantation, these changes were not predictive of resolution or prevention of new-onset PVCs.
Conclusion:
Melody valve implant for PS or PI did not result in resolution or prevention of PVCs or other arrhythmias during CPET despite improvement in hemodynamics. PVCs may be related to the basic heart defect, focal scarring, fibrosis or surgical suture lines rather than pulmonary valve dysfunction. A cautious appraisal of the effect of Melody valve implant on arrhythmia burden appears warranted.
TRANSCATHETER MELODY VALVE PLACEMENT IN LARGE DIAMETER BIOPROSTHESES AND CONDUITS: WHAT IS THE OPTIMAL “LANDING ZONE”?
Author links open overlay panelWilliamFinchDanielLeviMorrisSalemAbbieHagemanJamilAboulhosn
University of California, Los Angeles, Los Angeles, CA, USA
Background:
BPVs provide an ideal “landing zone” for future Melody Valve insertion. To guide surgical choice of BPV size, it is important to understand which BPV size can serve consistently as substrates for Melody valve placements.
Methods:
A database of all patients who underwent Melody implantation at UCLA or Kaiser Permanente Los Angeles from 2010 to 2014 was analyzed retrospectively. Patients with an existing BPV were stratified into those with a valve diameter of ≥27 mm or <27 mm.
Results:
One hundred and sixty patients underwent catheterization with the intention to implant a Melody valve. Melody valve implantation was performed in the pulmonary position in 52 patients with prior BPVs. The immediate procedural success rate was 100%. Immediately post-Melody the right ventricular to pulmonary artery gradient was significantly higher in the <27 mm group compared to the ≥27 mm group (14.3±3 vs 8.6±6.8, p=0.006). There was a significantly shorter time from prior valve replacement to Melody implantation in the <27mm group. There was 1 patient in whom TPVI was aborted due to inadequate landing zone in the <27 mm group, and no patients in the ≥27 mm group (p=NS).
Conclusion:
The results of this study indicate that 27 and 29 mm BPV provide a superior landing zone for Melody valve implantation with excellent immediate and intermediate term hemodynamicresults when compared to smaller bioprosthetic valves less than 27 mm.
HEMODYNAMIC EFFECTS OF PULMONARY VALVE REPLACEMENT FOR PULMONARY REGURGITATION AFTER REPAIR OF ISOLATED PULMONARY STENOSIS: A MATCHED COMPARISON WITH TETRALOGY OF FALLOT
Author links open overlay panelJouke PieterBokmaMichielWinterThomasOosterhofHubertVliegenArieVan DijkMarkHazekampDavidKoolbergenMaartenGroeninkBarbaraMulderBertoBouma
Academic Medical Center, Amsterdam, The Netherlands
University Medical Center, Leiden, The Netherlands
Background:
Pulmonary Valve Replacement (PVR) leads to a reduction of right ventricular (RV) volume in tetralogy of Fallot (TOF) but its effects are unknown in patients with isolated pulmonary regurgitation (iPR) after repair of pulmonary stenosis (PS). Our objective was to compare hemodynamic effects of PVR to determine whether TOF guidelines can be applied in iPR patients.
Methods:
In this retrospective, multicenter study we compared outcomes of all iPR (n=28, age at PVR 35±12 years, 47% male) and TOF (n=157, age at PVR 31±11 years, 62% male) patients who had undergone PVR before 2013. We compared baseline variables between both groups before we matched PS patients (n=11) in whom cardiovascular magnetic resonancewas performed before and after PVR with TOF patients in a 1:2 ratio on preoperative RV end-diastolic volume index (within 20ml/m2).
Results:
Preoperative RV and left ventricular volumes were smaller in iPR patients while RV ejection fraction was higher (p<0.05 for all). After matching, preoperative RV ejection fraction remained higher in iPR patients (52±7% versus 46±9%, p=0.038) with a further improvement after PVR (+7±11 versus 0±8, p=0.024). There was no difference in decrease of RV end-diastolic volume between patients with iPR or TOF (respectively, 136±32ml/m2 to 91±22ml/m2 and 140±31ml/m2 to 107±32ml/m2, p=0.257).
Conclusion:
When compared to matched TOF patients, iPR patients had a better preserved preoperative RV function with an additional improvement of RV EF after PVR while reduction of RV volume was similar. TOF guidelines can be used safely to assist in timing of PVR in iPR.
CATHETER-MEASURED HEMODYNAMICS OF ADULT FONTAN CIRCULATION: ASSOCIATION WITH MAJOR ADVERSE EVENT
Author links open overlay panelMakotoMoriCamdenHebsonKayokoShiodaRobertElderFredRodriguezMaanJokhadarNancyMcCabeBrianKogonMichaelMcConnellAnuragSahuWendyBook
Emory University School of Medicine, Atlanta, GA, USA
Yale School of Medicine, New Haven, CT, USA
Background:
In heart failure, high systemic vascular resistance index (SVRI) and low cardiac index (CI) predicts poor outcomes. Associations between catheter-measured hemodynamic variables and major adverse events in adults with Fontan circulation have never been examined.
Methods:
Retrospective review of cardiac catheterization data in 60 adult Fontan patients between 2002-2014 was conducted. Measured variables included central venous pressure (CVP), CI, and SVRI. The relationship between hemodynamic variables and major adverse events(death or heart transplant) was examined using survival analysis. VAS score (1 point each for varices, ascites, splenomegaly), a surrogate for signs of portal hypertension, was compared to assess potential systemic vasodilatory effect.
Results:
60 post-Fontan patients (85% systemic left ventricle, 40% atriopulmonary Fontan, age 28.0±7.2 years, time since Fontan operation 21.9±5.6 years) were analyzed. 18 experienced events: 10 deaths, 8 transplants. Comparing event vs. non-event group, mean CI was 2.8±0.9 vs. 2.4±0.5L/min/m2 (p=0.03), SVRI was 1983±1009 vs. 2381±828 dynes*s/cm5/m2, and CVP was 18.6±6.5 vs. 16.1±4.3mmHg. VAS score≥2 was present in 44% vs. 17% (p=0.002). Prevalence of relevant medication use was not different: digoxin(p=0.5), spironolactone (p=0.7), ACE-inhibitor (p=0.8), diuretics (p=0.8), hydralazine (p=0.3). After adjusting for potential confounders, there was no significant association between the hemodynamic variables and adverse events: CI with hazard ratio (HR)=1.3 [95%CI 0.7-2.2], p=0.3; SVRI with HR=1.0, CVP with HR=1.0.
Conclusion:
Adult Fontan patients who have major adverse events have a distinct hemodynamicphenotype. Alterations of CI, SVRI, or CVP typically seen an advanced heart failure were not seen in failing adult Fontan patients. Notably, a trend toward increased CI and reduced SVRI was observed in the event group. Further study is needed to understand the etiology of these distinct hemodynamic phenotypes.
OUTCOMES OF SIGNIFICANT TRICUSPID REGURGITATION AFTER CLOSURE OF ATRIAL SEPTAL DEFECT IN ADULTS
Author links open overlay panelJeong YoonJangJong-MinSongByeong JooBaeSe HunKangByung JooSunDae-HeeKimDuk-HyunKangJae-KwanSong
Asan Medical Center, Seoul, South Korea
Background:
The outcomes of significant tricuspid regurgitation (TR) and indications of tricuspidannuloplasty (TAP) in patients with atrial septal defect (ASD) have yet to be investigated.
Methods:
A total of 223 consecutive adult patients (mean age, 50 years; 51 males) who showed a significant (moderate or severe) TR before ASD closure were retrospectively enrolled, and their clinical and echocardiographic characteristics were reviewed. Surgical and transcatheter ASD closures were performed in 193 and 30 patients respectively. Among the surgical closure group, 152 and 40 patients underwent TAP and the Maze operation respectively. The primary endpoint was a combination of any cause of death, stroke, and heart failure. The secondary endpoint was a remnant of significant TR in 1 year after ASD closure.
Results:
In 1 year after ASD closure, TR jet areas decreased significantly compared to those before closures in both groups of patients with and without TAP (13.0 ± 5.0 vs 1.5±2.7 with TAP group; 10.3 ± 2.5 vs 4.8 ± 4.5 without TAP group; before vs 1 year after TR jet area [cm2], both p <0.001), but 34 patients (15.3%) showed a remnant of significant TR in 1 year after closures. The age (HR = 1.04; 95% CI = 1.02 – 1.08; p=0.003) and TAP (HR = 0.15; 95% CI = 0.07 – 0.33; p<0.001) were associated with the remnant of significant TR after 1 year. During a median follow-up after ASD closure for 4.0 years, 35 adverse events occurred. By multivariate Cox regression analysis, only the ratio of early diastolic mitral inflow velocity to mitral annuls velocity (HR = 1.07; 95% CI = 1.03 – 1.13; p=0.002) was independently associated with adverse events.
Conclusion:
A significant TR may decrease after ASD closure without TAP, but a combined TAP helps to prevent remnant of TR. Although this study does not prove a clinical benefit of TAP in our patient population, further prospective studies involving larger number of patients would be necessary.
TWELVE-YEAR FOLLOW-UP OF 213 PATIENTS WITH PERCUTANEOUS ATRIAL SEPTAL DEFECT CLOSURE GUIDED BY CMR IMAGING
Author links open overlay panelWassimShatilaRobertAertkerJonathanKochavAsvinGanapathiAndrewLodgeAnna LisaCrowleyJohnVavalleToddKieferJ. KevinHarrison
Duke University Medical Center, Durham, NC, USA
Background:
Given the limited published data, we sought to describe the long-term clinical follow-up of patients treated with device closure for secundum atrial septal defects (ASD).
Methods:
All patients undergoing percutaneous ASD closure in the adult cardiac catheterization lab at Duke between 2002 and 2014 were identified. The clinical characteristics, procedural details, and late outcomes were defined for each patient.
Results:
Between 2002 and 2014, 213 patients underwent ASD closure at a median age of 51 yrs (IQR- interquartile range: 40 yrs., 66 yrs.). Patients were selected based on pre-procedure anatomy defined by echo and cardiac magnetic resonance imaging (CMR). Devices used included Amplatzer ASO, Gore Helex, and Amplatzer Cribriform in 172 (81%), 34 (16%), and 7 (3%) patients, respectively. One device embolization occurred on post-procedure day 1 treated with surgical removal and closure. After a median follow-up of 7.2 (IQR: 4.1, 9.4) years, 18 (8.5%) died with a median duration between implantation and death of 3.3 (IQR: 1.6, 4.9) years. There was no procedural mortality or late device embolization or erosion. Three (1.4%) patients died within 1 year of the procedure. One, five, and ten year survival rates were 98.6% (97.0%, 100%), 92.7% (89.1%, 96.5%), and 90.0% (85.7%, 94.6%) respectively.
Conclusion:
Transcatheter ASD closure, employing pre-procedure anatomic selection with CMR, can be accomplished with low procedural risk and is associated with favorable long term outcome.
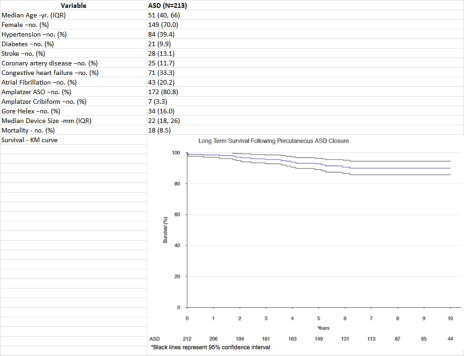
PRACTICE VARIATION IN THE MANAGEMENT OF CONGENITAL AORTIC VALVE DISEASE IN NEW ENGLAND
Author links open overlay panelMarkShwayderScottYeager
Fletcher Allen Health Care, Burlington, VT, USA
Background:
Practice variation is a significant factor in predicting and controlling health care costs. Bicuspid aortic valve (BAV) is the most common congenital heart defect, and can be associated with progressive valvular dysfunction and aortic dilation. Documenting current practice may reveal patterns of variation and may serve as a baseline against which to assess the effectiveness of interventions.
Methods:
An on-line survey open for 2 months to all pediatric and adult congenital cardiologists in New England described 3 clinical scenarios with accompanying questions about management and follow-up. Scenarios included BAV with normal valve function and aortic size, BAV with mild valve dysfunction and moderate aortic dilation, and moderate mixed valve disease with moderate aortic dilation. Utilization data included office visits, ECGs, echocardiograms, and MRIs. Each responder also provided personal information including years in practice, practice location, and practice size. Using Medicare reimbursement data, we estimated a 10 year cumulative cost, and compared this cost to the respondent’s experience and practice size.
Results:
Sixty nine of 122 polled responded (57%). There was a statistically significant difference in cost associated with caring for patients based on years in practice (p<0.05). The more experienced the practitioner, the fewer tests, office visits, and therefore costs accrued. There was also a statistically significant difference in cost with practice size (p<0.05). Larger practices tended to spend less money than did smaller practices.
Conclusion:
Significant practice variation, and therefore cost discrepancy, exists in the care for children with abnormal aortic valves. Given that this is the most common congenital heart defect, a more uniform approach to these patients could significantly decrease costs.
A MULTI-CENTER STUDY OF PRACTICE VARIATION AND RESOURCE UTILIZATION IN REFRACTORY KAWASAKI DISEASE
Author links open overlay panelJenniferLoL. LuAnnMinichLloydTaniJacobWilkesQianDingShajiMenon
University of Utah, Salt Lake City, UT, USA
Background:
There are no treatment guidelines for refractory Kawasaki disease (rKD). The purpose of this study was to assess practice variation and resource utilization for patients with rKD in a multicenter cohort.
Methods:
All patients <18 years old with rKD (defined as receiving >1 dose of IVIG) between 2007-14 were identified from the Pediatric Health Information System (45 hospitals). Data collected: demographics, medications, complications, length of stay (LOS), and charges. Multivariable regression was used to determine factors associated with LOS.
Results:
Of 14,306 episodes of KD (60% male), 21% (2,980, 63% male) had rKD. Compared to those receiving 1 dose of IVIG, rKD patients were slightly older (median age 33 vs. 32 mos), had greater LOS (5 vs. 3 days) and higher charges ($43,371 vs. $23,523) (p<0.001 for all). There was wide practice variation in the use of immunomodulators and anticoagulants in rKD. Immunomodulators included steroids 21%, infliximab 6%, cyclosporine 0.7%, abciximab 0.5%, methotrexate 0.3%, etanercept 0.2%, and rituximab 0.03%. Anticoagulants included enoxaparin 2%, warfarin 1.7%, tPA 2%, clopidogrel 2%, and dipyridamole 0.7%. Numerous factors were associated with LOS (Table).
Conclusion:
In rKD, the wide practice variation in the selection of immunomodulators and anticoagulantsmay reflect the absence of evidence and lack of consensus for optimal management. We identified predictors associated with longer LOS that may be used for counseling and resource allocation.
Factors affecting length of stay (LOS) in refractory KD (multivariable model)
| Variables | Categories | N (%) | Median LOS | Adjusted Risk Ratio (95%CI) | P-value |
| (IQR) | |||||
| Census region | Midwest | 760 (26) | 3 (2, 5) | 0.93 (0.88, 0.98) | 0.008 |
| Northeast | 412 (14) | 3 (2, 5) | 1.01 (0.97, 1.05) | 0.690 | |
| South | 1097 (37) | 3 (2, 5) | 0.98 (0.93, 1.03) | 0.460 | |
| West | 711 (24) | 3 (2, 4) | Reference | . | |
| Insurance type | Medicaid | 1102 (37) | 3 (2, 5) | 1.14 (0.96, 1.36) | 0.140 |
| Medicare | 22 (1) | 4 (3, 6) | 0.95 (0.91, 1) | 0.040 | |
| Other | 528 (18) | 3 (2, 5) | 0.93 (0.9, 0.97) | <.001 | |
| Private | 1328 (45) | 3 (2, 4) | Reference | . | |
| Intensive care unit admission | Yes | 393 (13) | 7 (4, 11) | 1.12 (1.05, 1.19) | <.001 |
| No | 2587 (87) | 3 (2, 4) | Reference | . | |
| Mechanical ventilation | Yes | 96 (3) | 13 (8, 20) | 1.41 (1.28, 1.56) | <.001 |
| No | 2884 (97) | 3 (2, 5) | Reference | . | |
| Steroids | Yes | 627 (21) | 9 (6, 13) | 1.46 (1.4, 1.52) | <.001 |
| No | 2353 (79) | 5 (4, 6) | Reference | . | |
| Other immunomodulators | Yes | 219 (7) | 10 (7, 17) | 1.35 (1.27, 1.44) | <.001 |
| No | 2761 (93) | 5 (4, 7) | Reference | . | |
| Anticoagulants (beyond aspirin) | Yes | 261 (9) | 11 (8, 19) | 1.44 (1.35, 1.54) | <.001 |
| No | 2719 (91) | 5 (4, 7) | Reference | . | |
| Seizures/neurologic sequelae | Yes | 212 (7) | 7 (5, 12) | 1.18 (1.11, 1.26) | <.001 |
| No | 2768 (93) | 5 (4, 8) | Reference | . | |
| Heart failure medications | Yes | 772 (26) | 8 (6, 12) | 1.21 (1.15, 1.26) | <.001 |
| No | 2208 (74) | 5 (4, 7) | Reference | . | |
| Shock/cardiac arrest | Yes | 277 (9) | 9 (6, 13) | 1.1 (1.03, 1.17) | 0.006 |
| No | 2703 (91) | 5 (4, 7) | Reference | . | |
| Arrhythmia | Yes | 184 (6) | 9 (6, 15) | 1.13 (1.06, 1.21) | <.001 |
| No | 2796 (94) | 5 (4, 7) | Reference | . | |
| Renal failure | Yes | 56 (2) | 7 (4, 12) | 1.18 (1.05, 1.33) | 0.006 |
| No | 2924 (98) | 5 (4, 8) | Reference | . | |
| Concomitant viral infection | Yes | 322 (11) | 7 (5, 10) | 1.14 (1.08, 1.2) | <.001 |
| No | 2658 (89) | 5 (4, 8) | Reference | . | |
| Congenital defects | Yes | 30 (1) | 4 (3, 8) | 1.31 (1.12, 1.52) | <.001 |
| No | 2950 (99) | 3 (2, 5) | Reference | . |
MULTICENTER EVALUATION OF CHARGES, LENGTH OF STAY AND MORTALITY DURING HOSPITALIZATION AFTER PEDIATRIC OPEN-HEART SURGERY ATTRIBUTABLE TO ADVERSE PATIENT-CARE EVENTS
Author links open overlay panelShaji C.MenonYingyingZhangL. LuAnnMinichTomGreeneJacobWilkesRichard E.Nelson
University of Utah, Salt Lake City, UT, USA
Background:
We sought to determine charges, lengths of stay (LOS) and mortality attributable to adverse patient-care events (APC) during hospitalization after pediatric open-heart surgery.
Methods:
Agency for Healthcare Research and Quality pediatric-specific quality indicators (PQI: 8 events) were used to identify adverse events in children <18 yrs. hospitalized for cardiac surgery with cardiopulmonary bypass from 40 US pediatric hospitals participating in the Pediatric Health Information System database (2008-2012). We constructed multivariable logistic and generalized linear regression models to identify the mortality and resource utilization (LOS and charges adjusted to 2013 US$) attributable to APCs.
Results:
The 33,787 surgeries (46% female) were grouped by age with 46% <1 yr; 29% 1-4 yrs; 16% 5-12 yrs. and 9% 13-18 yrs. LOS groups included 3% staying 1-2 days, 60% 3-7 days, 21% 8-14 days, and 16% ≥ 15 days PQI events occurred in 6% (2053). PQI events resulted in significant increases in mortality and resource utilization (Table 1). Compared to no events, hospital mortality, LOS and charges were substantially higher for postoperative sepsis, central venous catheter-related Infection, wound dehiscence and hemorrhage after pediatricopen-heart surgery.
Conclusion:
This novel study provides evidence for substantial increase in mortality and resource utilization directly attributable to APCs experienced during hospitalization after pediatricopen-heart surgery.
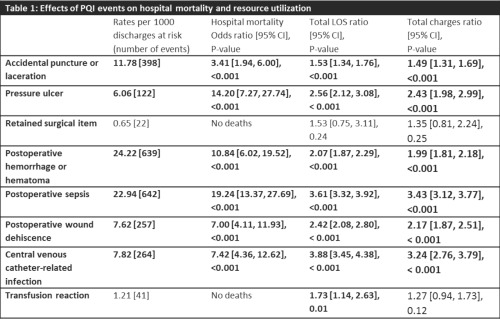
HIGH RESOURCE UTILIZATION FOR NON-CARDIAC HOSPITAL ADMISSIONS FOR ADULTS WITH CONGENITAL HEART DISEASE
Author links open overlay panelMichaelSeckelerIan D.ThomasJenniferAndrewsOmarMeziabElissaHellerTabithaMoeScottKlewer
University of Arizona, Tucson, AZ, USA
Arizona Pediatric Cardiology, Phoenix, AZ, USA
Background:
As hospitalizations for adults with congenital heart disease (CHD) are increasing, this study sought to compare costs for common non-cardiac admission diagnoses between adult patients with and without CHD.
Methods:
Retrospective review of hospital discharge data from the University HealthSystem Consortium (UHC) from January 2011 through December 2013; UHC collects discharge data from 120 academic institutions and 308 affiliated hospitals. The database was queried for patients with ICD-9 codes for moderate and severe CHD, as defined by the 32nd Bethesda Conference. Patients were stratified by age: Group 1 (18 – 29y) and Group 2 (30 – 39y). Diagnosis, direct cost, length of stay (LOS), ICU admission and mortality rates were compared for the five most common non-cardiac admission diagnoses for non-CHD and CHD patients using t-test and χ2 test, as appropriate.
Results:
The most common non-cardiac admission diagnoses are shown in the Table. Total direct cost, LOS, and ICU admission rate were higher in CHD compared to non-CHD patients for nearly all diagnoses in both groups, with no difference between CHD severity.
Conclusion:
Hospital costs for common non-cardiac diagnoses are higher for adults with CHD of at least moderate severity. Long-term survival of CHD patients is increasing and, as our study shows, they utilize a disproportionate amount of medical resources. Further characterization of CHD patient costs will be important to reduce or prevent hospitalizations in these patients.
THE IMPACT OF DEMOGRAPHIC, SURGICAL AND INTENSIVE CARE UNIT FACTORS ON LONG-TERM QUALITY OF LIFE IN CONGENITAL HEART DISEASE SURGICAL SURVIVORS
Author links open overlay panelBradleyMarinoAmyCassedyKateBrownMirjanaCvetkovicJohnCostelloRodneyFranklinJ. WilliamGaynorSimonLakerKatherineLevinsonHelenMacGloinLynnMahonyAnnetteMcQuillanKathleenMussattoDeirdreO’SheaJaneNewburgerMichelleSykesSarahTeeleGilWernovskyDennisDrotarJoWray
Ann & Robert H Lurie Children’s Hospital of Chicago, Chicago, IL, USA
Background:
Congenital heart disease (CHD) severity is associated with a lower quality of life (QOL). Given the lack of data, we sought to identify surgical and ICU factors associated with QOL scores.
Methods:
Patients from 8 centers who underwent Fontan procedure, TOF or TGA repair who participated in the Pediatric Cardiac Quality of Life Inventory (PCQLI) Testing Study were included. Surgical/ICU predictor variables were collected on all previous surgical/ICU admissions. Primary outcome variable (PCQLI patient/parent Total score) and covariates (demographics, cardiac status, medical care utilization) were obtained from the PCQLI Data Registry. ANOVA was used to test for group differences between the number of surgeries, ICU admissions and QOL. Ordinary Least Square regression was used to create multivariable surgical, ICU, and combined surgical/ICU models.
Results:
We included 572 patients: mean age 12+3yrs; CHD type Fontan 45%, TOF 29%, TGA 26%; median cardiac operations 2(1-9) and ICU admissions 3(1-9); time from most recent surgery (9+4yrs) and ICU admission (7+5yrs) to PCQLI participation. A greater number of operations and ICU admissions were associated with lower PCQLI Total score (p<0.01, both). R2 values ranged from 0.22-0.32 for multivariable surgical, ICU, and combined surgical/ICU models predicting patient and parent PCQLI Total score. In the combined QOL patient model, worse Total score was associated with non-white race, lower parental education, non-married status, younger age, greater number MD visits and surgeries, lower body temperature during surgery, and shorter time since last hospitalization (p<0.04). In the combined QOL parent model, worse Total score was associated with non-white race, non-married status, greater number MD visits/cardiac hospitalizations/medications/surgeries, shorter time since last hospitalization, more inotrope days, and neurologic complication (p<0.04).
Conclusion:
Surgical and ICU factors, demographic, and medical care utilization variables explain a modest amount of variation in QOL score in CHD surgical survivors. Research is needed to identify other factors that contribute to unexplained variability.
MORTALITY IN PATIENTS WITH TURNER SYNDROME AND HYPOPLASTIC LEFT HEART SYNDROME
Author links open overlay panelDiegoLaraMaryEthenMarkCanfieldWendyNembhardShaineMorris
Baylor College of Medicine, Houston, TX, USA
Texas Department of State Health Services, Austin, TX, USA
Background:
Patients with both hypoplastic left heart syndrome (HLHS) and Turner Syndrome (TS) have high rates of mortality. However, little is known about their long-term survival or causes of death.
Methods:
The Texas Birth Defect Registry was queried for all cases of HLHS with TS born during 1999-2007. Detailed birth, diagnostic, and survival data were obtained. Patients with HLHS with TS (TS+/HLHS) were compared to patients who had HLHS without other extracardiac birth defects or genetic disorders (TS-/HLHS). We used Kaplan-Meier and Cox Regression analyses to compare survival.
Results:
Of 542 patients with HLHS, 11 had TS, 71 had other extracardiac birth defects or genetic disorders (ECBD), and 463 had no other ECBD. Comparing those with TS+/HLHS to TS-/HLHS, 100% vs 35% were female (p<0.001), median birth weight was 2140 g (IQR 1780-2730) vs 3196 g (IQR 2807-3540, p<0.001), and median gestational age was 35 weeks (IQR 34-38) vs 39 weeks (IQR 38-39, p=0.001). There were no differences between the groups based on birth year, distance between birth hospital and surgical center, prenatal diagnosis or surgical center volume. Neonatal mortality in the TS+ group compared to the TS- group was 36% vs 27% (log rank=0.30) and infant mortality was 89% vs 51% (log rank=0.001). Ten of 11 TS+ patients died during the study period (91%). Six patients died prior to any surgery, 5 underwent Norwood, 3 died after Norwood, and 2 survived past Glenn. One post-Glenn patient was not known to have died by the end of the study period (1.4 years), and the oldest post-Glenn patient died at 1.7 years. In multivariable analysis, when controlling for preterm delivery (<37 weeks) and low birth weight (<2500 g), TS remained associated with earlier death (HR 1.99, 95% CI: 1.02-3.87). The underlying cause of death was listed as the patient’s congenital heart disease on all the death certificates; one patient had respiratory arrest after a procedural complication and one died of a dysrhythmia.
Conclusion:
TS in the presence of HLHS is associated with significant mortality, and continues to be when accounting for the lower birth weight and gestational age in these infants.
PROVISION OF TRANSITION EDUCATION AND REFERRAL PATTERNS FROM PEDIATRIC CARDIOLOGY TO ADULT CARDIAC CARE
Author links open overlay panelAnnaHarbisonStaffordGradyKevinChiSusanFernandes
Stanford University, Palo Alto, CA, USA
Background:
ACC/AHA guidelines recommend a structured preparation for and transfer to adult-oriented cardiac care for adult survivors of pediatric onset heart disease (POHD). Given this, we sought to describe the transition and transfer practices for a cohort of young adults with POHD and to determine factors associated with successful transfer to adult-oriented cardiac care.
Methods:
We performed a single center, retrospective chart review on patients >18 years of age, with POHD likely to require life long cardiac care, who were seen in outpatient pediatriccardiology (PC) between 2008-2011. Successful transfer was defined as the subsequent attendance at adult cardiology (AC) within two years of PC visit.
Results:
We identified 118 patients who met study criteria. Mean age 22.4±2.0 years, 59% male, 64% white and 40% Hispanic. Mean number of transition education topics noted was 3.3 ±1.8 out of 20. Education was documented regarding the underlying cardiac disease (89%), follow up and current medications (56%), exercise limitations (34%), dental prophylaxis (24%) and symptoms requiring prompt assessment (10%). Education regarding high-risk behaviors, pregnancy or impact of disease on offspring or on career/education was rarely noted. Recommendations for follow up were AC (57%) and PC 33%; 10% did not have a specific follow up recommendation. Of those told to transfer to AC, 79% successfully transferred. Characteristics associated with successful transfer included: prior cardiac surgery (p= 0.008), cardiac medication use (p=0.006) and frequency of follow up ≤1 year (p=0.037). One quarter of all subjects and 28% of those told to transfer to AC did not follow up within at least two years of their PC visit.
Conclusion:
Despite published guidelines, transition education appears lacking and the approach to transfer to adult cardiac care is not consistent. We found a significant number of adults remain in pediatric cardiology care and the location of a significant number of patients is unknown and may suggest they are lost to follow-up. Given the increased risk of morbidity and mortality in this patient population, standardization of transition education and transfer processes appear warranted.
ANXIETY IS MORE COMMON THAN DEPRESSION IN ADULTS WITH CONGENITAL HEART DISEASE
Author links open overlay panelLisaDengAbigail MayKhanDavidDrajpuchStephanieFullerLacey P.GleasonJonathanLudmirChristopher E.MascioSara L.PartingtonLyndaTobinYuli Y.KimAdrienneKovacs
Philadelphia Adult Congenital Heart Center, Children’s Hospital of Philadelphia and Penn Medicine, Philadelphia, PA, USA
Toronto Congenital Cardiac Centre for Adults, Peter Munk Cardiac Centre, University of Toronto, Toronto, Canada
Background:
Guidelines recommend screening for depression in patients with coronary heart disease. Adult congenital heart disease (ACHD) patients are known to be at risk of psychological problems but correlates of psychological distress are less understood. We assessed the prevalence of elevated symptoms of anxiety and depression and explored associated factors.
Methods:
Patients were enrolled from an outpatient ACHD clinic and completed validated measures including the Hospital Anxiety and Depression Scale (HADS) and two measures of quality of life: the Satisfaction with Life Scale (SWLS) and a Linear Analogue Scale (LAS). Clinical and demographic data were collected through chart review.
Results:
Of 134 patients (mean age = 35 years; 55% female), 42% had elevated anxiety (HADS-Anxiety score ≥ 8), and 12% had elevated depression (HADS-Depression score ≥ 8). Most patients with elevated depression (15/16) also had elevated anxiety. Patients with high anxiety were more likely to have undergone ≥ 2 surgical or interventional procedures (50% vs. 25%, p = 0.01). Those with high depression were more likely to be unemployed (24% vs. 8%, p = 0.05) and have a history of arrhythmia (19% vs. 7%, p = 0.04). Patients with elevated anxiety reported lower ratings on the LAS (73 vs. 80, p = 0.01) but not on the SWLS (p = 0.15). Those with elevated depression reported lower scores on both the LAS (59 vs. 79, p < 0.001) and SWLS (14 vs. 26, p < 0.001). Only 23% with elevated anxiety had a documented history of anxiety, and only 31% with elevated depression had a documented history of depression. Few patients (12%) were receiving mental health treatment at the time of the study.
Conclusion:
Among ACHD patients, elevated anxiety appears more common than elevated depression. As they have unique clinical correlates, providers are encouraged to evaluate for both depression and anxiety during clinical assessment. Further, as there was discordance between reported symptoms and documented history of depression or anxiety, it is important to explore optimal mechanisms to identify and treat mental health concerns in ACHD patients.
CONGENITAL AND ACQUIRED HEART DISEASE IN PREGNANCY
Author links open overlay panelTania C.Choreño-MachainJesusBarriosEduardo BucioReta
National Institute of Cardiology “Ignacio Chávez, Mexico City, Mexico
Background:
Several significant physiologic changes occur during pregnancy within the cardiovascular system that could become fatal in patients with a cardiac pathology. The increasing access to the health system, early diagnosis and more effective treatments have allowed a huge number of cardiopathic women reach a reproductive age and conceive.
Methods:
Cross-sectional study of pregnancies in women with congenital heart disease (CHD) assisted at the National Institute of Cardiology “Ignacio Chávez” between January 2009 and April 2014.
Results:
A total of 113 childbirths were registered at our Institute during a 5 year period. The women were grouped into the following clusters: 100 (88.49%) with CHD, nine (7.96%) with diverse cardiovascular pathologies, and four (3.53%) cardiovascular asymptomatic patients – assisted for the diagnosis of fetal heart disease. Most women (78.76%) had a good functional class at conception and delivery. Altogether, 53.98% women presented pulmonary artery hypertension at admission. There was a singleton live birth in 99.11% of cases plus one early stillbirth. Three women (2.97%) with CHD died. We recorded 56 (49.55%) urgent surgeries. Preterm C-section was performed on 43 (42.57%) CHD patients, with the birth of 53.48% small for gestational age newborn babies. During the anesthetic procedure, 19 patients developed hypertension. Regarding complications, 6.19% patients had transient uterine hypotony and 2.65% mild to moderate hemorrhagic events. The mean length of in-hospital stay was 5.3 days. All the patients received at least one prenatal fetal consultation.
Conclusion:
The maternal-fetal outcome at our Institution coincides with that of developed countries; nevertheless, we believe that there is an under record of pregnancies and the concomitant cardiovascular diseases in our country. In the years to come we will face more frequently patients with heart diseases that undergo a gestation; we intend to present the epidemiology of this entity to demonstrate that the follow-up, early diagnosis and attention by a multidisciplinary experienced team reduces the morbi-mortality associated.
COMMUNICATION PREFERENCES FOR ADVANCE CARE PLANNING IN ADULTS WITH CONGENITAL HEART DISEASE
Author links open overlay panelLisa X.DengLacey P.GleasonAbigail MayKhanDavidDrajpuchStephanieFullerLeah A.GoldbergChristopher E.MascioSara L.PartingtonLyndaTobinYuli Y.KimAdrienneKovacs
Philadelphia Adult Congenital Heart Center, Children’s Hospital of Philadelphia and Penn Medicine, Philadelphia, PA, USA
Toronto Congenital Cardiac Centre for Adults, Peter Munk Cardiac Centre, University of Toronto, Toronto, Canada
Background:
Adults with congenital heart disease (CHD) of moderate and great complexity are at risk for medical complications and premature death. While early discussion of advance care planning (ACP) is recommended, previous research suggests that it seldom occurs. The objective of this study was to investigate whether patient characteristics impact preferences for ACP communication with health care providers.
Methods:
Adults with CHD were prospectively enrolled from an outpatient clinic and completed a communication preferences survey and the Hospital Anxiety and Depression Scale. Clinical and demographic data were collected through retrospective chart review.
Results:
A total of 152 adults with CHD were included in the study. The median age was 33 years, 50% were female and 84% had CHD of moderate or great complexity. Only 13% of patients reported previous ACP discussions with providers and 21% had completed advance directives. On a scale of 0 (not important) to 10 (extremely important), patients rated ACP discussions as highly important (median rating = 7). Most patients (78%) preferred ACP discussions to be initiated before the diagnosis of a life threatening illness and 18 years was identified as the most appropriate age to have this discussion. Sixty-five percent of patients believed that they were likely to have a shorter life expectancy than individuals without CHD, and 61% favored receiving specific information about life expectancy. Patients with greater defect complexity were less interested in learning information about life expectancy (great complexity lesions 55%; moderate 68%; simple 86%, p = 0.04) and rated ACP discussions as less important (great 5.5; moderate 7.0; simple 8.0, p = 0.03). Nearly half of the patients (46%) reported elevated symptoms of anxiety. Patients with elevated anxiety scores reported greater interest in discussing ACP with their providers (8.0 vs. 6.0, p=0.001).
Conclusion:
Adults with CHD are receptive to ACP discussions and desire early communication with their providers. Patient-specific clinical characteristics such as disease complexity and anxiety inform ACP communication preferences and may help clinicians tailor these discussions.
INITIAL FEASIBILITY RESULTS OF A GROUP COPING AND RESILIENCE PROGRAM FOR ADULTS WITH CONGENITAL HEART DISEASE
Author links open overlay panelAdrienne H.KovacsAmanda C.KentnerSherry L.GraceRobertNolanCandiceSilversidesMimiBandyopadhyayJaneIrvine
University Health Network, Toronto, Canada
Background:
One-third of North American adults with congenital heart disease (CHD) have diagnosable mood or anxiety disorders; unfortunately most of these patients do not receive mental health treatment. Despite an increasing awareness of the unique psychosocial concerns of this patient population, there are no manualized psychosocial interventions. We assessed the feasibility of a randomized controlled trial (RCT) of a group intervention aimed at improving the psychosocial functioning, quality of life and resilience of adults with CHD.
Methods:
Within this feasibility study, we conducted a 2-arm pilot RCT in which patients were randomized to usual care or an 8-session group coping skills intervention. Here, we report feasibility in terms of study eligibility, recruitment, and retention. Recruitment was from a tertiary care downtown hospital that services adults with CHD from a wide geographic catchment area.
Results:
Over a 12 month period, 10 patients responded to posted study flyers. A total of 370 patients were approached in clinic by a research assistant. Half (186) were interested in learning about the study, of whom 60 (32%) provided informed consent and were enrolled in the study. The most frequent reasons for declining study participation were travel/transportation issues that would prevent attendance (43%) and the absence of psychosocial difficulties (18%). Across recruitment modalities, 42 patients met inclusion criteria and were randomly assigned. Of the 21 patients assigned to the intervention, 17 (81%) participated in group sessions, 2 (10%) were unable to attend scheduled meetings, and 2 (10%) withdrew from the study.
Conclusion:
This is the first evaluation of a manualized psychosocial intervention targeting adults with CHD. Initial feasibility results show that it is possible to successfully recruit and retain patients into an 8-week group coping skills intervention and that approaching patients in person is the most successful recruitment strategy. It is notable that a minority of patients denied psychosocial challenges. Given that travel/transportation problems limited participation for many patients, home- and/or web-based delivery should also be tested.
A PREGNANCY SURVEY: CURRENT ATTITUDE OF WOMEN WITH CONGENITAL HEART DISEASE REGARDING PREGNANCY IN NORTH AMERICA
Author links open overlay panelAarthiSabanayagamAliZaidi
Montefiore Einstein Center for Heart & Vascular Care, The Albert Einstein College of Medicine, New York, NY, USA
Montefiore Adult Congenital Heart Disease Program (MAtCH), Montefiore Einstein Heart Center, New York, NY, USA
Background:
With improved medical care more women with congenital heart disease (CHD) are now getting pregnant. Several women with CHD lack specific knowledge about their cardiac conditions and their need for specialized care during pregnancy and in the peri-partum period.
Methods:
We chose to evaluate the knowledge of women with CHD via a single cross sectional anonymous survey given to women attending the 7th National Adult Congenital Heart Association (ACHA) Conference. Fifty questions were used to assess knowledge of their cardiac conditions and need for specialized prenatal care.
Results:
A total of 77 women completed the survey. Fifty percent (N=39) had moderate and 38% (N=29) had severely complex CHD. Thirty percent (N=23) of women were told that pregnancy was contraindicated due to their underlying cardiac condition. Almost two thirds (N=50) of the women were considered to be high risk for adverse cardiovascular events. Eighty four percent (N=65) preferred their cardiologist to have trained in adult congenital heart disease, however 44% (N=34) would have been satisfied with adult cardiologists and 36% (N=28) with pediatric cardiologists providing care during pregnancy. Seventy percent (N=54) preferred having their prenatal cardiology visits at an adult facility. Two thirds (N=51) of the women had discussed cardiac complications and the risk of CHD transmission with their providers. Almost half (N=40) of the women thought they could get pregnant regardless of their condition while 11% (N=9) were not sure despite seeking regular ACHD care. Only 48% (N=37) were aware that they needed fetal echocardiograms during pregnancy and only 35% (N=27) had discussed modes of delivery with their health care providers. Seventy two percent (N=56) felt they needed high-risk obstetrics to be involved with their pregnancy and delivery.
Conclusion:
As more women with CHD are now getting pregnant, a multi-disciplinary and tailored approach with specialized care is needed for successful outcomes. Based on our results, further efforts are needed to improve the knowledge, attitudes and perceptions of women with CHD in relation to their cardiac and obstetric management during pregnancy.
GENDER DIFFERENCES IN HEALTHCARE COSTS IN THE EMERGING ADULT CONGENITAL HEART DISEASE POPULATION
Author links open overlay panelGarimaAgrawalYangLuRobertaWilliams
Children’s Hospital, Los Angeles, Los Angeles, CA, USA
Background:
It is important to understand the factors that drive costs as patients with congenital heart disease (CHD) transition from pediatric to adult health care. Gender differences in the prevalence and complexity of CHD are expressed throughout life, but it is unknown if this is reflected in healthcare costs during the transitional years.
Methods:
California State Inpatient Databases 2005-2009 were used to conduct a retrospective studyon inpatient admissions of CHD patients 10-29 years old. This population was divided into two study groups: all male admissions and all female admissions.
Results:
Males with CHD have higher inpatient admission costs than their female counterpart ages 10-29, but this cost difference narrows in the twenties. During the twenties, males have lower hospital admissions and higher mortality than females. Males also have more emergency admissions at ages 10-24 and longer length of stay (LOS) at ages 15-29. At all age groups, males have higher percentages of no insurance and unknown insurance. Females ages 10-29 have statistically significantly more admissions for atrial septal defect(ASD). Males ages 15-29 have statistically significantly more admissions for CHD surgery, arrhythmia/ congestive heart failure (CHF), and trauma; males ages 15-24 have statistically significantly more admissions for catheterization/ electrophysiology studies.
Conclusion:
The driver of healthcare utilization and costs is the gender-specific presentation of CHD. Females have lower inpatient costs than males, despite unilateral reproductive costs and more admissions in their twenties. Females generally have significantly more ASD admissions, fewer emergency admissions, and shorter LOS, all of which are associated with lower total admission costs due to low CHD complexity.
UNEXPECTED LATE CORONARY ARTERY ABNORMALITIES AFTER ARTERIAL SWITCH OPERATION FOR TRANSPOSITION OF THE GREAT ARTERIES
Author links open overlay panelTakeshiTsudaBradleyRobinsonMajeedBhatJeanneBaffaWolfgangRadtke
Nemours/Alfred I. duPont Hospital for Children, Wilmington, DE, USA
Thomas Jefferson University, Philadelphia, PA, USA
Background:
Arterial switch operation (ASO) is a common surgical intervention for d-loop transposition of the great arteries (d-TGA). The incidence of late coronary artery complications may be underestimated due to lack of clinical symptoms and limitations in non-invasive studies.
Methods:
We investigated coronary artery morphology in 28 patients with uneventful initial postoperative course out of 91 patients who underwent ASO between 1998 and 2013. Twenty six patients had coronary angiogram. We correlated the identified coronary artery abnormalities with clinical manifestation of myocardial ischemia.
Results:
Total 6 patients developed significant late coronary artery abnormalities. One asymptomatic patient died suddenly at age 3.75 years and was found to have severe left coronary artery(LCA) ostium stenosis at autopsy. Second asymptomatic patient collapsed during lacrosse game due to ventricular fibrillation at age 10 despite negative prior exercise stress test (EST) and myocardial perfusion scan. Coronary angiogram revealed severe ostium stenosis of LCA. The third patient, with exercise-induced ST-T depression and reversible myocardial perfusion defect was shown to have complete occlusion of LCA with collateral vessel formation. The fourth patient was found to have moderate ostial stenosis of LCA. The fifth patient had complete occlusion of left circumflex (LCX) artery with collateral vessel formation. The sixth patients had moderate long-segment right coronary artery (RCA) stenosis due to severe neoaortic dilatation. None of 6 patients showed clinical signs of coronary ischemia at outpatient visits and only one showed positive EST for myocardial ischemia. Six other asymptomatic patients showed trivial to mild narrowing of LCA by a routine selective coronary angiogram.
Conclusion:
Although the true incidence of coronary artery occlusion after ASO is unknown, conventional non-invasive tests including EST and nuclear myocardial perfusion scan were not reliable in detecting coronary abnormalities after ASO. We advocate that all patients after ASO warrant routine coronary image studies during late childhood before participating in competitive sports.
EXPERIMENTAL IMMUNOHISTOCHEMICAL STUDY ON PERSISTENT VASCULAR REMODELING RELATED TO DEVELOPMENT OF ARTERIOSCLEROSIS OR ATHEROSCLEROSIS IN CHRONIC KAWASAKI DISEASE PATIENTS
Author links open overlay panelKenjiHamaokaMaikoFujiiAyakoYoshiokaYukiKuchitsuAkikoOkamotoChinatsuSuzukiTomoyoYahataAkihiroNakamuraKazuyukiIkeda
Kyoto Prefectural University of Medicine, Kyoto, Japan
Background:
Atherosclerotic coronary heart disease has recently emerged as a clinical issue among young individuals with a history of Kawasaki disease (KD), which is a systemic vasculitisunique to children. However, whether or not and how KD promotes atherosclerosis remains unclear. We hypothesized that, analogous to the pathogenesis of arteriosclerosis or atherosclerosis, endothelial injury and the resultant intimal thickening are induced in coronary arteries after attenuation of vasculitis.
Methods:
We used a rabbit model of KD developed by Onouchi et al. and performed histopathologicalanalysis of the coronary arteries at acute (1, 3, 5, and 7 days) and chronic (3 months) phases of the disease.
Results:
In these rabbit models, a pan-arteritis with significant intimal cellular hypertrophy was histologically detected in the acute phase, and arterial intimal thickening was observed during the chronic phase. Immunohistochemical analysis of the coronary arteries revealed that the thickened intimal lesions observed during the chronic phase comprised abundant α-smooth muscle actin (α-SMA)-positive cells, most of which concomitantly expressed vascular cell adhesion molecule-1 and nuclear factor-κB. Although macrophages positive for RAM11 were barely detected, macrophage colony stimulating factor was strongly expressed in migrating smooth muscle cells in the intimal layer. In addition, the accumulation of proteoglycan as extracellular matrix was distinctly visible in the thickened intima, indicating progressive accumulation of lipids and proliferation of smooth muscle cells within the lesion.
Conclusion:
These findings suggest that, in KD-associated vasculitis, the migration of α-SMA-positive cells into the thickened intima might induce continuous vascular inflammation and remodeling, which might progress to coronary arteriosclerosis or atherosclerosis.
OUTCOMES FOR SURGICAL REPAIR OF KOMMERREL DIVERTICULUM AND ANEURYSM
Author links open overlay panelJosephPoteruchaNandanAnavekarTalhaNiazAnushreeAgarwalNaserAmmashJosephDearaniAlbertoPochettinoCaroleWarnesHeidiConnolly
Mayo Clinic College of Medicine, Rochester, MN, USA
Background:
Standard surgical management of Kommerell diverticulum (KD) and Kommerell aneurysm(KA) has not been established. We aimed to report our outcomes for surgical repair of KD and KA.
Methods:
The Mayo Clinic surgery database was retrospectively analyzed to identify pts with aberrant subclavian artery (ASA) operated on from 1990-2014. Surgical and clinical data were reviewed.
Results:
Surgical type and follow-up data are shown (Table). 863 pts with ASA were identified; 121 had KD and 28 had KA. Surgical repair was undertaken in 37 pts (25 with KD; 12 with KA). Carotid-subclavian transposition was the preferred technique for KA repair, nearly 70% had concomitant surgical arch intervention. Ligamentum arteriosum resection was more frequently employed in pts with KD alone (80%). Postoperative complications occurred in 19% (Table). There was one postoperative death (cardiac arrest). 5-year survival was 100% in pts with KD and 75% for pts with KA. At early and late follow-up, 89% and 79% of pts respectively had improvement of presenting symptoms.
Conclusion:
This is the largest study on outcomes of surgical repair of KD and KA. Carotid-subclavian transposition was the preferred technique for aneurysm repair. Surgical repair of KD and KA can be successfully undertaken resulting in symptomatic improvement with low mortality and morbidity.
| All pts | KD alone | KA | p | |
| (n = 37) | (n = 25) | (n = 12) | ||
| Surgery | ||||
| Carotid-subclavian transposition* | 11 (30%) | 4 (16%) | 7 (58%) | 0.01 |
| Partial arch replacement | 5 (14%) | 1 (4%) | 4 (33%) | 0.03 |
| Total arch replacement | 1 (3%) | 0 (0%) | 1 (8%) | NS |
| No arch intervention | 5 (14%) | 3 (12%) | 2 (17%) | NS |
| Aorto-subclavian intervention | 4 (11%) | 0 (0%) | 4 (33%) | 0.007 |
| Bypass | 3 (5%) | 0 (0%) | 3 (25%) | 0.03 |
| Re-implantation | 1 (3%) | 0 (0%) | 1 (8%) | NS |
| Aneurysmorrhaphy | 2 (5%) | 1 (4%) | 1 (8%) | NS |
| Ligamentum ligation | 20 (54%) | 20 (80%) | 0 (0%) | 0.0001 |
| Surgical approach | ||||
| Lateral thoracotomy | 36 (97%) | 25 (100%) | 11 (92%) | NS |
| Median sternotomy | 1 (3%) | 0 (0%) | 1 (8%) | NS |
| Follow up | ||||
| Postoperative | ||||
| Complications | 7 (19%) | 5 (20%) | 3 (33%) | NS |
| Phrenic/laryngeal nerve injury | 3 (8%) | 1 (4%) | 2 (17%) | NS |
| Chylous effusion | 3 (8%) | 3 (12%) | 0 (0%) | NS |
| Dissection | 2 (5%) | 1 (4%) | 1 (8%) | NS |
| Stroke | 0 (0%) | 0 (0%) | 0 (0%) | NS |
| Death | 1 (3%) | 0 (0%) | 1 (8%) | NS |
| Early follow-up | ||||
| Improvement in symptoms | 32 (89%) | 22 (88%) | 10 (91%) | NS |
| Reintervention | 1 (3%) | 1 (4%) | 0 (0%) | NS |
| Death | 0 (0%) | 0 (0%) | 0 (0%) | NS |
| Late follow-up | ||||
| Improvement in symptoms | 27 (79%) | 20 (80%) | 7 (78%) | NS |
| Reintervention | 1 (3%) | 1 (4%) | 0 (0%) | NS |
| Death | 2 (5%) | 0 (0%) | 2 (17%) | NS |
KD, Kommerell diverticulum; KA, Kommerell aneurysm
*, 5 pts with two step surgical approach (3 KA, 2 KD).
PROGRESSION OF RIGHT VENTRICULAR DILATION IN REPAIRED TETRALOGY OF FALLOT
Author links open overlay panelBenedettaLeonardiLamiaAit-AliaMarcelloChinaliPierluigiFestaAurelioSecinaroGiacomoPongiglione
Bambino Gesù Children’s Hospital IRRCCS, Roma, Italy
Istituto IFC-CNR, Massa, Italy
Background:
The progression of right ventricle (RV) dilation, mainly due to pulmonary regurgitation (PR) after Tetralogy of Fallot repair (rToF) with transannular (TP) or infundibular (IP) patch, varies among patients. The onset of RV dysfunction, due to its progressive dilation, is still difficult to predict. Pulmonary valve replacement (PVR) does not seem to affect RV function, if already impaired. Understanding the rate of progression of RV dilation over time could help identify the right timing for PVR in order to prevent RV dysfunction.
Methods:
118 rToF patients (mean age 19,7±10,8 years, 59% men) with TP or IP underwent repeated cardiac magnetic resonance (CMR) exams at two centers in Italy between March 2008 and March 2014. Data regarding date of surgery and type of correction were collected, in addition to CMR parameters (RV/LV dimension and function, pulmonary trunk/arteries stenosis, tricuspid regurgitation and restrictive pattern flow in the pulmonary artery).
Results:
In the whole population RV volume barely increased over time, paired with a slight RV ejection fraction reduction. TP patients (86% of whole population) showed a significantly higher rate (p=0,002) of RV dilation (36%) compared to IP ones (19%) and a lower rate of RV reduction (3% vs 25%). RV dilation was not significantly correlated with the type of first surgery (palliative shunt vs repair) or the time elapsed from surgery. Eventually pulmonary trunk/arteries stenosis or restrictive pattern did not significantly influence RV changes over time.
Conclusion:
RV dilation did not progress consistently in the majority of our rToF patients, being nearly stable over time. Significant increase in RV dimensions and concurrent impairment in function was observed in a subgroup of patients mainly composed of TP correction, regardless of the presence of a palliative shunt. The mild reduction in RV volume over time occurred in a small subgroup, without any significant correlation with RV restrictive physiology pattern.
CONTEMPORARY SINGLE-STAGE TETRALOGY OF FALLOT REPAIR: EXCELLENT SURVIVAL BUT PHYSICAL OR NEURODEVELOPMENTAL COMPROMISE IN ONE FIFTH
Author links open overlay panelEricPham-HungAnDuongAlexandraPageMichaelGrittiSaraHussainTravisWilderMikeSeedStevenMillerGlenVan ArsdellEdwardHickey
The Hospital for Sick Children, Toronto, Canada
Background:
Tetralogy of Fallot (TOF) is considered a low risk lesion because perioperative mortality has fallen dramatically. We investigated late morbidity after contemporary repair.
Methods:
All 458 TOF repairs (2000 – 2012) were analyzed using competing risks techniques. Data were abstracted from clinical records with cross-sectional follow-up in 2013. For all 233 followed locally, every clinic consultation was reviewed for evidence of physical limitation or neurodevelopment delay.
Results:
Palliative procedures were rare (33; 7%): surgical shunt=3, RVOT/PDA stent=20, RVOTballoon=10. The remaining 93% had primary repair at median age 180 days; 6% were <60 days and 2% were <30 days. Strategy: valve-sparing=65%, trans-annular patch=30%, conduit=5%. Four deaths have occurred (1%) – all surgically related – and 1 resuscitated sudden cardiac death. Freedom from re-operation was 85±2% at 8 years and late trans-catheter re-interventions (61) were undertaken in ~20% of all children within 5 years, mostly for PA stenosis. Of the 233 locally followed children, 47 (20%) have genetic syndromes. In the 186 non-syndromic children, 22% have some physical limitation or neurologic deficit and 6% have evidence of neurodevelopmental delay (table). Gestational age was the only reliable non-cardiac and non-surgical determinant of late developmental health.
Conclusion:
Future efforts should focus on mitigating risk factors – especially prematurity – that lead to physical/neurodevelopmental problems.
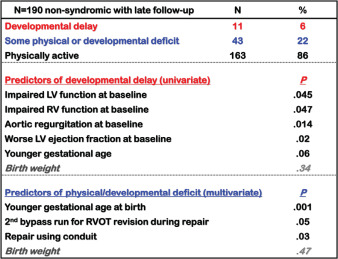
ACUTE KIDNEY INJURY FOLLOWING INFANT CARDIAC SURGERY: INCIDENCE AND PREDICTIVE FACTORS
Author links open overlay panelKurtSchumacherDanielEhrmannRebeccaReichelSunkyungYuJanetDonohueRobertGajarskiJohnCharpie
University of Michigan Congenital Heart Center, Ann Arbor, MI, USA
Background:
Infants undergoing repair of congenital heart disease (CHD) are at risk for post-operative acute kidney injury (AKI), but the incidence and outcome of AKI in this population is unknown. Furthermore, it is unknown whether AKI can be predicted from pre- and post-operative data. This study aimed to identify AKI’s incidence and outcome following infant CHD repair and determine predictive factors that could guide therapeutic interventions.
Methods:
This prospective, observational study in a pediatric cardiac ICU analyzed pre- and post-operative data in infants (< 12 months) undergoing cardiac surgery to determine the incidence and outcome of AKI (AKI Network Stage 3, or AKIN-3). Univariable analyses determined AKI’s association with an extensive list of pre-operative, operative, and post-operative patient factors. Receiver operator characteristic area under the curve (AUC) assessed associated factors’ discriminatory ability.
Results:
In 279 infants enrolled, the cumulative incidence of AKI was 0.22. Regarding pre-operative anatomic and demographic factors, AKI patients were more likely to be age < 30 days (p=.02). Associated operative and post-operative factors were minimum arterial pressure (p=.0005), maximum vasoactive inotrope score (p=.03), decreasing serum pH (p=.02), lower initial bicarbonate (p=.02), maximum serum lactate (p=.01), and emergent extracorporeal membrane oxygenation (p=.01). No factor had an AUC >.67 implying overall poor discriminant ability to predict AKI from pre- and post-operative data. AKI was associated with hospital death; 6/59 patients with AKI died compared to 7/220 non-AKI patients (odds ratio 3.43, p=.04).
Conclusion:
AKIN-3 grade AKI is common in infants following repair of CHD and associated with an increased risk of death. Unfortunately, the ability to predict AKI from pre- or early post-operative data is poor limiting clinician ability to tailor care toward preventing AKI.
POSTOPERATIVE SERUM TROPONIN TRENDS IN INFANTS UNDERGOING CARDIAC SURGERY
Author links open overlay panelJenniferSuRam KumarSubramanyanHeshamMahmoudOmarToubatJohnWoodGraceKung
Children’s Hospital of Los Angeles, Los Angeles, CA, USA
University of Southern California, Los Angeles, CA, USA
Background:
Troponin-I (TN-I) is known to be elevated following pediatric cardiac surgery, but there is lack of procedure-specific normative data. We hypothesized that extent of TN-I elevation varies with surgical complexity and persistent elevation predicts poor prognosis.
Methods:
We prospectively measured serial TN-I (preoperative, 4, 8, 12, 24, and 48 hours postoperative) in 75 infants (age < 1 year) undergoing cardiac surgery. Procedures were divided into three groups: off cardiopulmonary bypass (CPB) (n = 8), on CPB (n = 42), and on CPB with ventricular incision (VI) (n = 25).
Results:
All patients had undetectable baseline TN-I levels, which peaked on average by 4 hours after surgery, and returned to near-normal levels by 48 hours (Figure). The area under the curve (AUC) of TN-I levels over the 48-hour period was significantly different among the three surgical groups (p < 0.05), and highest in patients with VI. The AUC of TN-I increased with longer CPB time (r2 = 0.40, p < 0.0001). Of the 8 patients with persistent TN-I rise at 12 hours, 4 (50%) had postoperative complications of hypoperfusion injuries and 2 (25%) died, compared with a 10% complication rate and 3% mortality in the remaining cohort (p = 0.01 and 0.05).
Conclusion:
Our data provides benchmark values for TN-I levels following cardiac surgery in infants. Extent of TN-I elevation correlates with complexity of surgery, with highest levels in infants requiring VI. Persistent elevation in TN-I 12 hours after surgery is associated with poor outcomes.
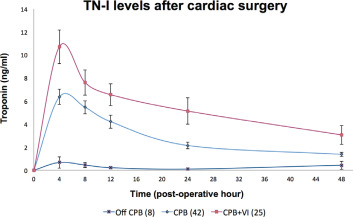
LONGITUDINAL EXERCISE PERFORMANCE IN PATIENTS WITH D-LOOP TRANSPOSITION OF THE GREAT ARTERIES AFTER ARTERIAL SWITCH OPERATION
Author links open overlay panelJoseph D.KueblerMing HuiChenJonathanRhodes
Boston Children’s Hospital, Boston, MA, USA
Background:
The first patients to undergo a successful arterial switch operation (ASO) for d-transposition of the great arteries are now entering their fourth decade of life. Past studies of ASO survivors’ exercise function have yielded conflicting results. We therefore undertook this study to describe the current function of ASO survivors, to identify factors related to inferior exercise performance and to determine whether their exercise function tends to deteriorate over time.
Methods:
Patients with palliative surgery prior to ASO, ventricular hypoplasia or severe valvar dysfunction were excluded from the study. Data from cardiopulmonary exercise tests (CPX) in which the peak respiratory exchange ratio was <1.09 were also excluded. We identified 113 patients who met entry criteria and had 186 CPX at our institution between 1/2002 and 1/2013; 41 patients had at least 2 qualifying CPX.
Results:
Mean age at the time of the initial test was 16.7 ± 0.7 years. Peak oxygen consumption (VO2) averaged 84.3 ± 2.4 %predicted. Peak VO2 was lower among patients with repaired ventricular septal defects (81.9 ±3.6 vs. 86.2 ± 2.9 %predicted; p<0.05) and among patients with ≥moderate pulmonary artery stenoses (77.2 ± 4.9 vs. 86.5 ±2.5 %predicted; p < 0.05). Surgery prior to 1991 was also associated with a lower peak VO2 (81.0 ±3.4 vs. 87.0 ± 3.0 %predicted; P<0.01). The mean % predicted peak heart rate was 91.7 ± 1.1%, with no significant difference between any of the subgroups. Non-diagnostic exercise-induced STT changes developed in 10 patients (12 studies). In the subgroup with at least 2 exercise tests, the annual decline in %predicted peak VO2 was quite slow (-0.76 percentage points/year; p=0.04 vs. expected normal age-related decline).
Conclusion:
The exercise capacity of ASO survivors is well preserved and is only mildly reduced compared to normal subjects. Moreover, there is only a slight deterioration in exercise capacity over time. VSD repair, residual right sided obstructive lesions, and earlier surgical era are associated with worse exercise performance.
THREE-DIMENSIONAL EVALUATION OF REGIONAL RIGHT VENTRICULAR CURVATURE IN REPAIRED TETRALOGY OF FALLOT
Author links open overlay panelWaseemCossorFrancescoMaffessantiKarimaAddetiaVictorMor-AviKeigoKawajiDavidRobersonKarinDillPeterVargaRobertoLangAmitPatel
University of Chicago, Chicago, IL, USA
Advocate Children’s Hospital, Oak Lawn, IL, USA
Background:
Patients with repaired Tetralogy of Fallot (rTOF) often have residual pulmonic valveabnormalities and surgical scars, leading to maladaptive remodeling of the right ventricle(RV). We hypothesized that 3D analysis of regional RV shape may provide new insight into RV remodeling in these patients.
Methods:
CMR (1.5T Philips) was performed on 17 subjects with rTOF (age 9-53), and 10 controls (age 23-43). RV end-systolic and end-diastolic endocardial borders were manually traced on contiguous short-axis cine slices, and a 3D model was constructed using custom software. Local endocardial curvature, indexed to RV volume, was mapped in color onto the 3D endocardial surface (figure). Regional curvature was calculated for the RV inflow, outflow, trabecular, free wall, and septal segments. The parameters from rTOF patients were compared to those obtained from controls.
Results:
Compared to controls, patients with rTOF had: (1) higher global curvature (0.55 ± 0.05 vs. 0.39 ± 0.08, p <0.01); (2) convex septal curvature, as opposed to concave in controls (0.18 ± 0.14 vs. -0.12 ± 0.09, p<0.01); (3) higher free-wall (0.64 ± 0.04 vs. 0.57 ± 0.07, p=0.01) and trabecular (0.60 ± 0.08 vs. 0.31 ± 0.09, p<0.01) curvature with less pronounced differences in the inflow (0.55 ± 0.07 vs. 0.51 ± 0.07, p=0.07) and outflow (0.37 ± 0.09 vs. 0.47 ± 0.14, p=0.14) regions.
Conclusion:
Novel 3D analysis of RV endocardial curvature in patients with rTOF demonstrates significant variation in regional remodeling.
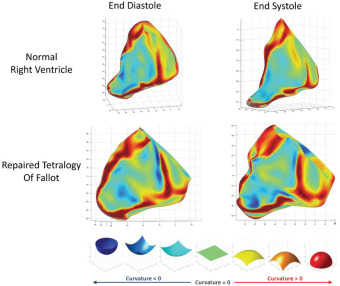
WIDE COMPLEX TACHYCARDIA IN A PATIENT WITH EPSTEIN’S ANOMALY AND AN UNDERLYING EPSILON WAVE
Author links open overlay panelShane PaulPrejeanCharlesSmith
Louisiana State University Internal Medicine Residency, Baton Rouge, LA, USA
Louisiana Cardiology Associates, Baton Rouge, LA, USA
Background:
Ebstein’s anomaly (EA) is a group of malformations involving the tricuspid valve and right ventricle (RV) resulting in incompetence of the valve and atrialization of the proximal RV. Clinical manifestations include cyanosis, right-sided heart failure, arrhythmia and sudden cardiac death. The most common presentation in adults is arrhythmia.
Case:
A twenty-eight year old male with a history of EA presented to the emergency department with the complaint of “heart racing.” He reported acute onset of palpitations associated with dizziness and diaphoresis. He was found to be tachycardic and hypotensive. Electrocardiogram (EKG) revealed wide complex tachycardia (Figure 1). He received cardioversion with successful conversion to normal sinus rhythm. Following cardioversion a second EKG demonstrated an epsilon wave in lead V1(Figure 1). Further history obtained uncovered a history of supraventricular tachycardia (SVT) requiring ablation in the past. An electrophysiology study was negative for an accessory pathway, but revealed inducible ventricular tachycardia. After and ICD was placed, patient was discharged on Sotolol and Metoprolol.
Methods:
N/A
Results:
N/A
Conclusion:
We demonstrate an uncommon presentation of a rare disease in adults. EP study was used to differentiate SVT with aberrancy from ventricular tachycardia. The case is also the first to demonstrate an epsilon wave in a patient with EA, a finding which can be explained by the abnormal architecture of the atrialized portion of the right ventricle.
POOR RIGHT VENTRICULAR EXERCISE RESERVE PREDICTS HEART FAILURE AND ARRHYTHMIA IN ADULTS WITH CONGENITAL RIGHT HEART DISEASE
Author links open overlay panelAdaStefanescuAmiBhattJohnSerfasSaraTabtabaiJoshuaRuffDoreenYeh
Massachusetts General Hospital, Boston, MA, USA
Background:
Poor exercise capacity and failure to augment right ventricular (RV) ejection fraction (EF) with exercise predicts poor outcome in patients with left ventricular systolic heart failure (HF) but has not been investigated in adults with congenital heart disease and RV pathology.
Methods:
We performed a retrospective analysis of adults with congenital RV disease who had undergone cardiopulmonary exercise test (CPET) and EF assessment during exercise (by standardized radionucleotide ventriculography). Students’ paired T-test was used for continuous variables and Fisher’s exact test for categorical variables.
Results:
The cohort included 135 CPETs (Table 1; mean follow-up 1.2 years). Tetralogy of Fallot, Ebstein anomaly, and pulmonic stenosis were the most common diagnoses. Patients with poor RV exercise reserve were more likely to have a lower peak oxygen uptake (pVO2) and lower baseline left ventricular EF. Patients who failed to augment RV EF had a higher likelihood of developing HF (OR 5.4, 95% CI 1.14-50.5, p=0.01) and arrhythmia (OR 3.2, 95% CI 0.9-14, p=0.03). EF during exercise provided additional information: of the 20 patients who had an adverse outcome despite an adequate pVO2>20cc/kg/min, 11 had abnormal RV EF response and were thus identified as having an abnormal CPET by the addition of ventriculography.
Conclusion:
Evaluation of RV EF response during exercise identifies patients at higher risk of an adverse outcome.
| Characteristic | Overall | RV EF does not augment
(delta 0 or less) |
RV EF augments
by 5% or more |
p-value |
| Patients with measured RV EF at CPET | 135 | 67 | 38 | |
| Age
(mean +/- SD) |
40.8
+/-12.8 |
41 | 38.7 | 0.19 |
| Female gender | 49.6% | 60.3% | 37.8% | 0.01 |
| NYHA class 2 or greater | 53.9% | 60% | 37.8% | 0.04 |
| CPET results | ||||
| Peak VO2
(cc/kg/min; mean +/- SD) |
20.3
+/- 6.3 |
19.3 | 21.7 | 0.02 |
| RV EF at rest | 40.4 | 41.2 | 41.2 | 0.5 |
| LV EF at rest | 62.3 | 59.8 | 67.0 | 0.002 |
| Other imaging variables | ||||
| QRS width | 131 | 130 | 132 | 0.62 |
| Indexed RV end diastolic volume by MRI (cc/m2) | 118 | 119 | 107 | 0.2 |
| Dilated RV by echocardiogram | 75% | 74.2% | 65.6% | 0.47 |
| More than moderate pulmonary regurgitation on TTE | 32.2% | 32.2% | 23.3% | 0.46 |
| Outcome | ||||
| Combined outcome of HF and arrhythmia | 40% | 42.9% | 24.3% | 0.024 |
| Heart Failure | 18.9% | 22.4% | 5.4% | 0.010 |
| Arrhythmia | 23.8% | 28.5% | 10.8% | 0.015 |
NEW TREATMENT OPPORTUNITIES IN PULMONARY HYPERTENSION AND CONGENITAL HEART DISEASE
Author links open overlay panelIlja MarkBlokAnneliekevan RielMark J.SchuuringArieVan DijkBarbaraMulderBertoBouma
Academical Medical Center, Amsterdam, The Netherlands
University Medical Center Nijmegen, Nijmegen, The Netherlands
Background:
Endothelin receptor antagonists are regarded a cornerstone in treatment of pulmonary arterial hypertension associated with congenital heart disease (PAH-CHD). Currently macitentan, a potential successor of the widely applied bosentan, is being introduced. A recent trial has proven its outstanding effects on exercise capacity and mortality, compared to placebo. However a direct clinical comparison with bosentan is lacking. Using our large longitudinal cohort of PAH-CHD patients, we aim to provide insight in potential benefits of switching bosentan to macitentan.
Methods:
In this multicenter prospective cohort study, all adult PAH-CHD patients on bosentan are scheduled to switch to macitentan with continuation of study protocol measurements. These include laboratory tests, 6-minute walk tests (6-MWT), cardiopulmonary exercise tests, echocardiography, MRI and quality of life questionnaires at regular intervals during follow-up. All measurements will be compared with previously collected prospective data during bosentan treatment using paired samples t-tests.
Results:
From 2006 a total of 84 PAH-CHD patients started bosentan, of whom 44 patients are currently still alive (mean age 46±14 years, follow-up 6.2±2.6 years, 46% male, 36% Down syndrome). Currently 25 patients were switched to macitentan. No serious adverse eventswere reported. Three months macitentan treatment resulted in improved 6-MWT (429±110 to 438±122 meters, mean values) and resting saturation (83 to 86%, median values) although non-significant. However macitentan reduced NT-pro-BNP (1143 to 804 ng/L, median values, p=0.05) and high sensitive Troponin-T (0.016 to 0.010 µg/L, median values, p=0.01). These and additional results after treatment switch will be presented.
Conclusion:
This is the first study to provide important clinical and safety information on the effect of switching bosentan to macitentan in adult PAH-CHD patients. After three months of macitentan treatment in the first 25 patients significant declines in cardiac markers NT-pro-BNP and Troponin-T are already apparent.
REGIONAL RIGHT VENTRICULAR EJECTION FRACTION AND CARDIAC OUTPUT IN REPAIRED TETRALOGY OF FALLOT
Author links open overlay panelWaseem J.CossorFrancescoMaffessantiKarimaAddetiaVictorMor-AviKeigoKawajiDavidRobersonKarinDillRobertoLangAmitPatel
University of Chicago, Chicago, IL, USA
Advocate Children’s Hospital, Oak Lawn, IL, USA
Background:
Patients with repaired Tetralogy of Fallot (rTOF) have changes in global and regional right ventricular (RV) function due to residual pulmonic valve stenosis and insufficiency, anatomic defects, surgical scar or conduction delays. Global RV volumes and ejection fraction (EF) obtained from Cardiovascular Magnetic Resonance (CMR) are used for clinical decision making in rTOF. We hypothesized that 3D analysis of regional function would provide new insights into RV remodeling in rTOF.
Methods:
In 17 rTOF patients (Age 9-53) vs. 10 healthy controls (age 23-43) we compared regional RV EF and cardiac output (CO). CMR (1.5T Philips) was performed and RV end-systolic and end-diastolic endocardial borders were manually traced on contiguous short-axis cine slices. A 3D model was constructed using custom software to measure RV global and regional volume, EF and CO.
Results:
Compared to controls, rTOF patients had: 1. Higher global RV volume and lower global RV EF; 2. Lower EF in the inflow and outflow regions with relative sparing of the EF in the trabecular region; 3. Increased regional contribution to CO in the trabecular region, reduced contribution in the inflow region, and relatively unchanged contribution in the outflow region (Table).
Conclusion:
In contrast to controls, the global RV CO in patients with rTOF is more dependent on contributions from the trabecular region and less so from the inflow and outflow regions.
| rTOF | Control | p | |
| RV ejection fraction (EF%) | mean ± SD | mean ± SD | |
| Global RV | 44 ± 7% | 54 ± 8% | 0.01 |
| RV outflow | 37 ± 10% | 48 ± 9% | 0.01 |
| RV inflow | 41 ± 10% | 55 ± 8% | < 0.01 |
| RV trabecular | 49 ± 13% | 55 ± 11% | 0.26 |
| RV regional CO (as % of total RV CO) | |||
| RV outflow | 18 ± 8% | 21 ± 6% | 0.24 |
| RV inflow | 37 ± 10% | 45 ± 5% | 0.018 |
| RV trabecular | 45 ± 12% | 33 ± 8% | 0.01 |
ELECTIVE BALLOON PULMONARY VALVULOPLASTY IN THE NEWBORN WITH TETRALOGY OF FALLOT
Author links open overlay panelMohamedLeyeNagibDahdahJoaquimMiro
CHU Sainte Justine, Montréal, Canada
Background:
In tetralogy of Fallot (TOF), the risk of cyanotic spells can lead to emergency systemic-pulmonary shunt. The development of the pulmonary artery and the onset of cyanotic spells are conditioned by the volume of the trans-valvular flow.
Methods:
We conducted a retrospective study to determine whether elective primary pulmonary valvuloplasty (EPPV) in the neonate 1) allows a better development of the pulmonary artery; 2) reduces the risk of cyanotic spells or the use of emergency surgery; 3) increase the possibilities of conservative surgery of the pulmonary valve. TOF who received EPPV within the first month of live were compared to an observational group (OBS).
Results:
There were 48 patients (19 EPPV and 29 OBS) with a trend for lower birth O2-saturation in EPPV (89±5.7% vs 94±5.9%; p=0.07). Pulmonary valve z-score was comparable (-2.17±1.43 vs -1.87±1.54; p=0.513) as well as Nakata index (120.9±41.6 vs 147.4±50.1 mm2/m2; p=0.62). Pulmonary valve z-score remained comparable at surgery (-1.63±1.83 vs -1.09±1.75; p=0.603) and the Nakata index increased equally by 45.1±97.8 vs 18.6±56.8; p=0.293). Cyanotic spells and palliative shunts occurred equally in both groups (3 vs 2; p=0.372, and 1 vs 1; p=1.0, respectively). The need for trans-annular patch was higher in EPPV however (78.9 % vs 34.5%; p=0.03).
Conclusion:
Despite appropriate growth of the pulmonary arteries following neonatal EPPV in TOF, there was no significant decrease of cyanotic spells, or the need for transannular patch.
CONTEMPORARY TRANSCATHETER PATENT DUCTUS ARTERIOSUS CLOSURE: RESULTS OF THE LARGEST RETROSPECTIVE STUDY TO DATE
Author links open overlay panelManishBansalCandiceLiCharlesMullinsHenriJustino
Texas Children’s Hospital/Baylor College of Medicine, Houston, TX, USA
Background:
Results of transcatheter patent ductus arteriosus (PDA) closure using contemporary devices at a large pediatric center.
Methods:
Retrospective review of all patients (pts) undergoing transcatheter closure of PDA. Data collected included demographic, clinical, angiographic and echocardiographic parameters.
Results:
From 04/2002 to 05/2012, 489 pts underwent catheterization (cath) for PDA closure, at a median (range) age = 2.4 yrs (2 wks-42 yrs) and weight = 12.55 kg (2.5-110). Minimal ductal diameter = 2.2 mm (0.5-7.4). PDA morphology was type A (61%), E (17.5%), D (8%), C (8%) and B (1%). Most common implants were coils, in 252 cases (51%), with multiple coils in 49 (19% of all coil cases). PDA minimum diameter was most important predictor of need for multiple coils (1.49 vs. 2.3 mm, p=0.001) in single vs. multiple coil cases. Other implants used were Amplatzer Duct Occluder (ADO) (n=232, 46%), Amplatzer Vascular Plug II (6, 1.2%), Gianturco-Grifka sack (4, 0.8%),Amplatzer Muscular VSD Device (1, 0.2%). Embolization of the implant occurred in 13 pts (2.6%); 11 coils were retrieved at same cath, 1 coil left in a lower lobe pulmonary artery, 1 ADO retrieved at repeat cath. There were no major procedural complications (death, stroke, or urgent surgery). 6 pts (1.2%) required repeat cath for residual PDA,5 to place additional coils, 1 to retrieve embolized ADO device with placement of another ADO. Follow up (mean 2 yrs, n= 295) showed 100% PDA closure. There was no instance of significant obstruction (Doppler peak velocity > 3 m/s) across the aorta, and only 1 case across the left pulmonary artery requiring no intervention. No pt developed endocarditis, or required device explant or any other device-related surgery.
Conclusion:
This series of transcatheter PDA closure is larger than any single- or multi-center published to date, and affirms that PDA occlusion with contemporary implants is extremely successful. The reintervention rate, albeit very low, is mainly related to residual leaks due to coils, and is virtually non-existent with other devices. Patients undergoing transcatheter PDA closure nowadays are assured of a 100% long-term closure rate, and an extremely low incidence of complications.
PERCUTANEOUS PULMONARY VALVE IMPLANTATION: A SYSTEMATIC REVIEW OF SAFETY OUTCOMES
Author links open overlay panelRhandersonCardosoMohammadAnsariDanielGarciaCarlosAlfonso
Eduardo De Marchena, University of Miami, Miami, FL, USA
Background:
Percutaneous pulmonary valve implantation (PPVI) has emerged as a highly effective alternative to surgical revision in congenital heart disease patients with right ventricle outflow tract (RVOT) stenosis and/or regurgitation. Reports of safety outcomes in PPVI vary widely in the literature, likely due to heterogeneity in patient characteristics and surgical substrates. We aimed to perform a systematic review of adverse events following PPVI and estimate the overall incidence of PPVI complications.
Methods:
PubMed, EMBASE and Cochrane Central were searched for studies that reported procedural and long-term complications of PPVI. No restrictions were made to the type of valve used (Melody/Edwards SAPIEN). Baseline demographic and surgical data were collected. The overall rate of PPVI complications was calculated amongst all studies that met inclusion criteria.
Results:
A total of 19 studies and 1,151 patients were included. The most common complication observed was stent fracture, seen in 12.9% of patients. Surgical conversion was required in 1.5% of PPVI procedures. In a follow up that ranged from 4 to 30 months, reintervention and explantation were needed in 10% and 4.6% of cases, respectively. The incidence of bacterial endocarditis and RVOT tear was 2.9% each. Other complications of PPVI occurred in less than 1% of cases and include: guidewire injury, perforation of the pulmonary arterybranches, hemothorax, valve embolization, stent migration, and ventricular arrhythmias. Procedure-related mortality was exceedingly rare and occurred in only 3 patients (0.3%).
Conclusion:
In summary, we report the overall rate of complications following PPVI in pooled data from previously published studies. The inclusion of heterogeneous patient populations with different sample sizes and baseline characteristics increases the validity of our findings. These results can be used by physicians and patients in the evaluation of risks and benefits associated with PPVI.
IMPACT OF PERSISTENT RIGHT TO LEFT SHUNT IN DEVICE-OCCLUDED ATRIAL SEPTAL DEFECTS
Author links open overlay panelMichaelZdradzinskiAbrahamAbernethyKathrynStackhouseRachelElkinMohamedHalaneWaelElMallahRichardKrasuski
The Cleveland Clinic, Cleveland, OH, USA
Background:
Percutaneous device occlusion is the gold standard for repair of secundum atrial septal defects (ASD). The prevalence and impact of residual shunt after device closure is poorly understood.
Methods:
From a prospective, single institution database of 447 patients undergoing ASD device closure, we identified 414 patients with technically adequate bubble studies prior to closure. Follow-up echos were available at 1 month in 373, 3 months in 315 and 1 year in 220 patients. Survival in the latter cohort was assessed through careful review of electronic medical records and confirmed using the Social Security Death Index.
Results:
Right to left shunting (RLS) was present in 14% at 1 month, 16% at 3 months and 14% at 1 year. Patients with RLS at 1 year were similar to those without shunt in age, gender, ASD size (22±6 vs 21±13), hemodynamics and comorbidities. RLS patients were more likely to be Caucasian (77% vs 46%, p=0.003). More patients with RLS tended to have enlarged right atria (75% vs 54%, p=0.093) and right ventricles (93% vs 79%, p=0.118) at baseline. During follow-up 3 patients with RLS underwent re-attempt at closure and 2 underwent surgery. Over a median follow-up of 6.7 years, 17% with RLS at 1 year died compared to 4% without shunt (p=0.014). Kaplan-Meier analysis was similarly significant (Graph). Hazard ratio for RLS was 3.6 (95% confidence interval 1.1 to 11.4, p=0.041).
Conclusion:
Persistent shunt after device closure of secundum ASD is common and appears to negatively impact long-term survival.
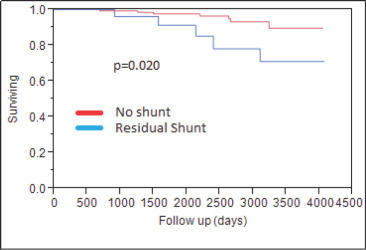
COMPLICATIONS FROM ULTRASOUND GUIDED FEMORAL ARTERIAL ACCESS IN PEDIATRIC CARDIAC CATHETERIZATION: A PROSPECTIVE SINGLE CENTER COHORT STUDY
Author links open overlay panelJohnAlexanderBenjaminWallerThomasYohannanAgrawalVijaykumarHannahLloydMarshaStewert-SellersShyamSathanandam
University of Tennessee, Memphis, TN, USA
Le Bonheur Children’s Hospital, Memphis, TN, USA
Background:
Acute loss of arterial pulse (LOP) is a known complication in children following arterial access for cardiac catheterization. In the modern era of using ultrasound guided femoral arterial access (UGFAA),the incidence of LOP in children has not been described. The incidence of LOP requiring treatment when UGFAA is not employed in children ranges between 4% and 8%. The objectives of this study was to describe the incidence of and identify risk factors for LOP in children who had UGFAA during cardiac catheterization.
Methods:
A prospective study was performed including all cardiac catheterizations using UGFAA in children (≤18 years) over a 20 months period. All patients underwent ultrasound and Doppler evaluation prior to and at the end of the procedure. Treatment for LOP was initiated if there was documented thrombus or if there was absence of Doppler pulsations an hour after the completion of the procedure. Multivariate analysis was performed to identify independent risk factors for LOP.
Results:
UGFAA was obtained in 486 catheterization procedures on 427 children. LOP was identified in 33 cases (6.8%). However, an occlusive thrombus by ultrasound was diagnosed in only 9 patients (1.8% of all cases). The LOP reversed in 10 cases within an hour with a strong Doppler signal. The remaining 23 patients were treated for LOP (4.7%). Children ≤18 months were at higher risk for LOP (25/33; OR = 5.3, 95% CI: 2.3 – 12.3, P < 0.001). In children ≤18 months the incidence of LOP was 10.48% and for LOP requiring treatment was 7.5%. Younger age (P < 0.001) and less % change in distal Doppler velocity (P < 0.001) were the only significant independent predictors for LOP. Number of access attempts, time required to obtain access, operator experience, sheath size, sheath exchanges, activated clotting time, hemoglobin, cardiac output, contrast dose, procedure length, etc., were not found to be significant factors.
Conclusion:
The overall incidence of LOP requiring treatment of 4.7% and 7.5% in Children ≤18 months is lower than reported when UGFAA is not used. Children ≤18 months were at higher risk. There were no other independent predictors and hence LOP after catheterization is likely multifactorial in etiology.
IMPACT OF PULMONARY HYPERTENSION ON RIGHT HEART REMODELING FOLLOWING DEVICE CLOSURE OF ATRIAL SEPTAL DEFECTS
Author links open overlay panelMichael JohnZdradzinskiAbrahamAbernethyRachelElkinKathrynStackhouseMohammedHalaneWaelElMallahRichardKrasuski
The Cleveland Clinic, Cleveland, OH, USA
Background:
Our group has previously shown that pulmonary hypertension (PH) at the time of atrial septal defect (ASD) closure negatively affects survival. The impact of PH on subsequent right heart remodeling in these patients is not known.
Methods:
From a prospective, single institution database of 447 patients undergoing ASD device closure, we identified 311 patients with adequate echocardiograms to serially (post-procedure, 3 month and 1 year) assess right heart structure and function. PH was defined by mean pulmonary artery pressure ≥25 mmHg at catheterization or right ventricular (RV) systolic pressure of ≥40 mmHg by echo. RV size and systolic function by echo were defined as normal (0), mild (1), moderate (2) and severely abnormal (3).
Results:
PH was present at closure in 26% of the cohort. PH patients were older (59.6±16.1 vs 45.6±14.8 years, p<0.001) but otherwise similar demographically including balloon occlusionsizes (19.7±7.3 vs 18.8±6.3 mm. p=0.34). >mild RV enlargement was present in 46% of PH patients vs. 30% of non-PH, p=0.02. >mild RA enlargement was present in 31% of PH vs. 14% non-PH, p<0.001. >mild RV systolic dysfunction was present in 26% of PH vs. 6% of non-PH, p<0.001. RV systolic pressure was expectedly greater in PH (55.6±18.0 vs 31.8±8.2 mmHg, p<0.001) and pressure drop was greater at each follow-up (-15.9 vs -4.2, p<0.001 by 1 year). RV systolic function improved significantly more by 1 month in PH (0.3 vs 0.0 grade improvement, p=0.03), though this difference waned over time (0.4 vs 0.2, p=0.24 at 1 year). RV size (-0.9 vs -1.0, p=0.68) and RA size (-0.4 vs -0.6, p=0.31) decreased similarly over time; and by 1 year >mild RV enlargement was present in 15% of PH vs 1% of non-PH (p<0.001) and >mild RV systolic dysfunction was present in 6% of PH vs 0% of non-PH patients (p=.050).
Conclusion:
Despite reducing RV systolic pressure to a greater extent in patients with PH, closure of ASD has similar effects on right heart remodeling and does not appear to lessen the differences present in right ventricular size and function.
PATIENT-SPECIFIC SIMULATION OF RIGHT VENTRICLE OUTFLOW TRACT CONDUIT BALLOON ANGIOPLASTY USING CARDIAC MRI-DERIVED 3D VIRTUAL MODELS TO ASSESS THE RISK OF CORONARY ARTERY COMPRESSION DURING TRANSCATHETER PULMONARY VALVE REPLACEMENT
Author links open overlay panelPuneetBhatlaSujataChakravartiAchiauLudomirskyMichaelArgillaPhillipBermanDoffMcElhinneyVittoriaFlamini
New York University Medical Center, New York, NY, USA
Background:
Transcatheter pulmonary valve replacement (TPVR) with the Melody™ valve is frequently considered in patients with right ventricular outflow tract (RVOT) conduit obstruction. TPVR carries a risk of coronary artery (CA) compression. This risk is evaluated by CA angiographyand simultaneous balloon dilation prior to TPVR. No MRI or CT based predictors exist to assess this risk. We hypothesized that finite element (FE) balloon dilation simulations on patient-specific virtual models (VM) generated using MRI data could predict CA compression during TPVR.
Methods:
All patients who underwent pre-catheterization MRI and attempted TPVR at our institution from 06/13 to 06/14 were included (n=3). 3D VM were created from MRI data, using Mimics, 3-Matic and Meshmixer software. A FE simulation of balloon conduit angioplasty was implemented retrospectively in ABAQUS for each of the VM. Balloon expansion was modeled as rigid body dilation using linear elastic constitutive model to a dimension equal to 100% of the original RVOT conduit diameter.
Results:
The FE balloon simulation accurately predicted the presence (III) or absence (I, II) of CA compression in all 3 patients (Figure 1). 3D VM were also successful in delineating the CA origin and course in relation to the RVOT conduit in all cases.
Conclusion:
FE-simulation of conduit balloon angioplasty using MRI derived 3D VM offers a potential method for predicting the likelihood of CA compression in TPVR candidates and may improve patient selection.
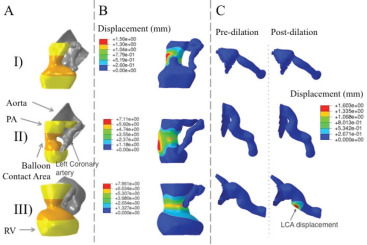
CANDIDACY FOR DEVICE CLOSURE OF COMPLEX MUSCULAR VENTRICULAR SEPTAL DEFECTS: NOVEL APPLICATION OF RAPID PROTOTYPING AND VIRTUAL 3D MODELS DERIVED FCARDIAC CT AND MRI
Author links open overlay panelPuneetBhatlaSujataChakravartiShi-JoonYooOmarThabitDoffMcElhinneyAchiauLudomirsky
New York University Medical Center, New York, NY, USA
Background:
Complex muscular ventricular septal defects (CMVSD) are often difficult to surgically close and managed by device closure. The pre-intervention imaging is crucial in defining the anatomy and aids in patient selection. We hypothesized that 3D physical and virtual models in patients with CMVSD is feasible, would assist in patient selection and aid in the successful device closure.
Methods:
Virtual and physical 3D models on 3 patients with CMVSD were generated from CT or MRIdata, using Mimics, and 3-Matic software. The first patient had history of complicated and unsuccessful prior device closures, with residual shunt. Two physical models, with and without devices in situ were printed (Figure 1A) for this patient. Two virtual models were generated in the other two patients.
Results:
The location, size, trabeculations, papillary and muscle bundles were clearly visualized in all patients. The two physical models were extensively studied, resulting in successful device closure of the residual VSD. The virtual model on patient 2 identified RV papillary musclesadjacent to the CMVSD (Figure 1B) precluding device closure. The patient 3 model identified muscle bundles crowding the VSD suggesting potential for spontaneous closure.
Conclusion:
Construction of 3D models in patients with CMVSD is feasible, assists in appropriate patient selection and allows for extensive examination and planning. This may facilitate a focused and informed procedure and improve the potential for successful closure.