EARLY HEMODYNAMIC CHANGES AFTER FETAL AORTIC STENOSIS VALVULOPLASTY ARE ASSOCIATED WITH BIVENTRICULAR CIRCULATION AT BIRTH
Aaron Prosnitz, Monika Drogosz, Audrey Marshall, Carol Benson, Louise Wilkins-Haug, Wayne Tworetzky and Kevin Friedman
vol. 69 no. 11 Supplement 554
DOI:
https://doi.org/10.1016/S0735-1097(17)33943-8
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Aaron Prosnitz,
- Monika Drogosz,
- Audrey Marshall,
- Carol Benson,
- Louise Wilkins-Haug,
- Wayne Tworetzky and
- Kevin Friedman
- Boston Children’s Hospital, Boston, MA, USA
Background: In fetuses with severe mid-gestational aortic stenosis, fetal aortic valvuloplasty (FAV) can promote left ventricular growth and function, and may prevent progression to hypoplastic left heart syndrome. Previous small studies suggest that post-intervention LVEF and the presence of antegrade transverse arch flow (ATAF) several weeks after intervention are associated with biventricular outcome. We evaluate if FAV is associated with acute changes in left heart hemodynamic function, and if these changes are associated with biventricular circulation (BVC) after birth.
Methods and Results: We reviewed all technically successful FAV cases between 2000 and 2016 (n=101). FAV occurred at a mean gestational age of 24.6 weeks (19.0-31.4), with post-FAV echocardiograms occurring 0-2 days later. Of the live births (n=94), BVC was achieved in 42 subjects (45%).
Measures of left heart physiology were markedly abnormal pre-FAV and improved post-FAV. ATAF was present in 0 subjects pre-FAV and increased to 65 subjects (65%) post-FAV (p<0.0001). Pre-FAV, 86 subjects (89%) had entirely left-to-right PFO flow and 10 (10%) had bidirectional flow. Post-FAV, the number of subjects with bidirectional PFO flow increased to 20 (24%) (p=0.007). LVEF increased from 24.7% (standard deviation ±12.0) to 32.7% (±15.2) (p<0.0001). LV systolic pressure decreased from 59.1 mm Hg (±17.3) to 50.9 mm Hg (±18.6) (p=0.007). AR ≥ mild was present in 3 subjects (3%) pre-FAV and 51 subjects (53%) post-FAV (p<0.0001). MR ≥ moderate was present in 8 subjects (8%) pre-FAV and 40 subjects (41%) post-FAV (p<0.0001).
Univariate analysis demonstrated that a change in PFO flow from left-to-right to bidirectional (OR 3.62, 95% CI 1.05-12.5, p=0.041), an increase in LVEF (OR 1.05, 95% CI 1.00-1.09, p=0.037), and gaining ATAF (OR 7.5, 95% CI 2.5-22.3, p<0.0001) were associated with BVC. In multivariable analysis, gaining ATAF was the only variable that remained significantly associated with BVC.
Conclusions: Technically successful FAV in subjects with fetal aortic stenosis is associated with immediate improvements in left heart physiology that are predictive of biventricular outcome.
Footnotes
- Oral Contributions
- Room 146 C
- Sunday, March 19, 2017, 8:12 a.m.-8:22 a.m.
- Session Title: Highlighted Original Research: Congenital Heart Disease and the Year in Review
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 908-04
CHARACTERISTICS, RISK FACTORS & OUTCOMES OF EXTRACORPOREAL MEMBRANE OXYGENATION USE IN THE PEDIATRIC CARDIAC INTENSIVE CARE UNIT
Marissa Brunetti, Lauren B. Retzloff, Jessica L. Lehrich, J. William Gaynor, Sara Pasquali, David Bailly, Susan Davis, Darren Klugman, Joshua Koch, Javier Lasa and Michael Gaies
vol. 69 no. 11 Supplement 556
DOI:
https://doi.org/10.1016/S0735-1097(17)33945-1
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Marissa Brunettia,b,
- Lauren B. Retzloffa,b,
- Jessica L. Lehricha,b,
- J. William Gaynora,b,
- Sara Pasqualia,b,
- David Baillya,b,
- Susan Davisa,b,
- Darren Klugmana,b,
- Joshua Kocha,b,
- Javier Lasaa,b and
- Michael Gaiesa,b
- aChildren’s Hospital of Philadelphia, Philadelphia, PA, USA
- bUniversity of Michigan, Ann Arbor, MI, USA
Background: Extracorporeal Membrane Oxygenation (ECMO) is used to support pediatric patients with medical and surgical cardiac disease. We aimed to characterize ECMO use across a multicenter cohort.
Methods: Retrospective analysis of the Pediatric Cardiac Critical Care Consortium (PC4) clinical registry was performed to describe ECMO frequency and outcomes. Within strata of medical and surgical hospitalizations, we identified risk factors associated with ECMO use through multivariate logistic regression.
Results: Across 23 hospitals, there were 14,526 eligible hospitalizations from 8/1/14-6/30/16, of which 449 (3.1%) included at least 1 ECMO course. ECMO was used in 120 (2.4%) medical and 329 (3.5%) surgical hospitalizations. Low cardiac output was the most common ECMO indication in both groups. Extracorporeal cardiopulmonary resuscitation (E-CPR) was used in 42% of medical and 32% of surgical ECMO courses. Risk factors associated with ECMO use in the medical group included acute heart failure and higher vasoactive inotropic score at admission (both p<0.0001). Stroke (15%) and renal failure (15%) were the most common ECMO complications in the medical group. Risk factors associated with post-operative ECMO use in the surgical group included younger age, extra-cardiac anomalies, pre-operative morbidity, higher STAT category, bypass time, and early post-operative mechanical ventilation and arrhythmias (within 2 hours) (all p<0.05). Bleeding requiring re-operation (25%) was the most common ECMO complication in the surgical group. Hospital mortality was 63% in the medical group and 50% in the surgical group with E-CPR mortality rates of 83% and 50%, respectively.
Conclusions: This is the first multicenter study describing contemporary ECMO use and outcomes in pediatric CICU patients with all forms of cardiac disease. ECMO is a rare therapy, yet mortality remains high, highlighting the importance of identifying levers to improve care. We identified unique high-risk subgroups to target for quality initiatives within medical and surgical patients.
Footnotes
- Oral Contributions
- Room 146 C
- Sunday, March 19, 2017, 8:38 a.m.-8:48 a.m.
- Session Title: Highlighted Original Research: Congenital Heart Disease and the Year in Review
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 908-08
AORTIC VALVE REPAIR IN THE PEDIATRIC POPULATION: MIDTERM OUTCOMES COMPARING LEAFLET REPAIR USING AUTOLOGOUS PERICARDIUM VERSUS PORCINE INTESTINAL SUBMUCOSA (CORMATRIX®)
Meena Nathan, Rebecca Beroukhim, Kimberlee Gauvreau, Ann Demeritt, Edward Marcus, Tal Geva, Christopher Bairdand Pedro del Nido
vol. 69 no. 11 Supplement 557
DOI:
https://doi.org/10.1016/S0735-1097(17)33946-3
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Meena Nathana,b,
- Rebecca Beroukhima,b,
- Kimberlee Gauvreaua,b,
- Ann Demeritta,b,
- Edward Marcusa,b,
- Tal Gevaa,b,
- Christopher Bairda,b and
- Pedro del Nidoa,b
- aBoston Children’s Hospital, Boston, MA, USA
- bHarvard Medical School, Boston, MA, USA
Background: While aortic valve repair (AoVR) is considered the most appropriate therapy in pediatric population, mid/long term outcomes have been disappointing from progressive dysfunction of currently available leaflet substitute material. We aim to compare outcomes of AoVR with autologous pericardium (AP) vs, porcine intestinal submucosa- CorMatrix(CM)
Methods: Consecutive patients from 2008 to 2010 who underwent AoVR (full/partial leaflet replacement, edge augmentation, leaflet patch, predominantly in single leaflet) were studied. Clinical and echo data (read in corelab by 2 readers) were collected preoperatively, at discharge and for up to 5 years post discharge. Time to reintervention (RI) was analyzed by cox regression. Progression of aortic regurgitation (AR) and stenosis (AS) was compared between AP and CM from discharge to latest followup.
Results: There were 26 CM and 49 AP patients followed for a median of 3.2 (IQR 0.9, 5) years. Baseline characteristics were similar between groups. There were 12 (46%) RI in CM vs.13 (27%) in AP group. On univariable analysis, age, weight, and CM use predicted RI. On multivariable modeling CM had a shorter time to RI (HR 3.5, CI 1.5, 7.8; p=0.003) adjusted for age and type of leaflet repair (figure).
Conclusions: Aortic valve repair with CM is associated with earlier time to reintervention. In the current era, autologous pericardium remains the best alternative for AoVR. The search for replacement material, particularly those with growth potential continues.
Footnotes
- Oral Contributions
- Room 146 C
- Sunday, March 19, 2017, 8:51 a.m.-9:01 a.m.
- Session Title: Highlighted Original Research: Congenital Heart Disease and the Year in Review
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 908-10
SAFETY AND FEASIBILITY OF MELODY TRANSCATHETER PULMONARY VALVE REPLACEMENT IN THE NATIVE RIGHT VENTRICULAR OUTFLOW TRACT: A MULTICENTER STUDY
Mary Hunt Martin, Jeffery Meadows, Bryan Goldstein, Lisa Bergersen, Athar Qureshi, Shabana Shahanavaz, Jamil Aboulhosn, Darren Berman, Lynn Peng, Matthew Gillespie, Aimee Armstrong, Cindy Weng and Robert Gray
vol. 69 no. 11 Supplement 558
DOI:
https://doi.org/10.1016/S0735-1097(17)33947-5
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Mary Hunt Martina,b,
- Jeffery Meadowsa,b,
- Bryan Goldsteina,b,
- Lisa Bergersena,b,
- Athar Qureshia,b,
- Shabana Shahanavaza,b,
- Jamil Aboulhosna,b,
- Darren Bermana,b,
- Lynn Penga,b,
- Matthew Gillespiea,b,
- Aimee Armstronga,b,
- Cindy Wenga,b and
- Robert Graya,b
- aUniversity of Utah, Salt Lake City, UT, USA
- bPrimary Children’s Hospital, Salt Lake City, UT, USA
Background: Melody Transcatheter Pulmonary Valve Replacement (TPVR) is FDA approved within right ventricular to pulmonary artery (RV-PA) conduits; however, >80% of patients needing pulmonary valve replacement do not have a conduit. Therefore, Melody TPVR has been adopted clinically to treat native (non-conduit) right ventricular outflow tracts (nRVOT). Safety, feasibility and factors associated with successful nRVOT TPVR have not been studied.
Methods: This is a multicenter, retrospective review of all patients presenting for nRVOT TPVR. Pre-procedural imaging (MRI and echo) and cath data were collected.
Results: Of 229 patients (mean age 21 years, range 4-67) from 11 centers, 132 (58%) had successful TPVR. The remaining 97 (42%) did not receive TPVR due to large nRVOT (n=67), aortic root or coronary compression (n=18) and not clinically indicated (n=12). There were no deaths and 5 (2%) serious complications: stent embolization requiring surgery (4) and arrhythmia requiring cardioversion (1).
Factors associated with successful TPVR included higher TPVR volume center, pre-cath pulmonary stenosis, and no prior transannular patch. Pre-cath MRI measurements were significantly different in the implanted vs. not-implanted groups (Table).
Conclusions: TPVR in the nRVOT is safe, however, nearly half the patients are found not to be candidates, mainly due to large RVOT size. Improved understanding and use of MRI data as well as availability of larger devices may improve success rates for nRVOT TPVR.
Footnotes
- Oral Contributions
- Room 146 C
- Sunday, March 19, 2017, 9:04 a.m.-9:14 a.m.
- Session Title: Highlighted Original Research: Congenital Heart Disease and the Year in Review
- Abstract Category: 11. Congenital Heart Disease: Therapy
- Presentation Number: 908-12
RE-INTERVENTION DURING THE INTERSTAGE PERIOD: A REPORT FROM THE NATIONAL PEDIATRIC CARDIOLOGY QUALITY IMPROVEMENT COLLABORATIVE
Matthew William Buelow, Nancy Rudd, Jena Tanem, Pippa Simpson, Peter Bartz and Garick Hill
vol. 69 no. 11 Supplement 559
DOI:
https://doi.org/10.1016/S0735-1097(17)33948-7
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Matthew William Buelowa,b,
- Nancy Rudda,b,
- Jena Tanema,b,
- Pippa Simpsona,b,
- Peter Bartza,b and
- Garick Hilla,b
- aChildren’s Hospital of Wisconsin, Milwaukee, WI, USA
- bMedical College of Wisconsin, Milwaukee, WI, USA
Background: Single ventricle heart disease with aortic arch hypoplasia has high morbidity and mortality, with the greatest risk seen in the interstage period. Residual lesions often require catheter based or surgical re-intervention to minimize risk. We sought to describe the types, frequency, and risk factors for re-intervention, between stage 1 palliation and stage 2 palliation, utilizing the National Pediatric Cardiology Quality Improvement Collaborative (NPC-QIC) database.
Methods: The NPC-QIC database, consisting of patients discharged home after stage 1 palliation from 53 centers in the United States, was queried. The primary risk factor of interest was shunt type and the primary outcome was re-intervention.
Results: Of the 1156 patients, 580 patients (50.2%) had a re-intervention. There was no difference in total rate of re-intervention between those with a modified BT shunt (MBTS)(52.5%) and those with an RV-PA shunt (RVPAS)(48%, p=0.17). The MBTS group had increased re-intervention during stage 1 hospitalization (23% vs 16%; OR: 1.6 (95% CI: 1.2-2.2), p=0.002). Those with a MBTS underwent aortic arch re-intervention more frequently than those with an RVPAS (p<0.005), while patients with an RVPAS had increased re-intervention on the shunt and the pulmonary arteries (p=0.02) following discharge. Post operative mechanical ventilation > 14 days (p<0.01) was the only risk factor associated with re-intervention by multivariable analysis, regardless of shunt type.
Conclusions: Re-intervention between stage I and stage 2 palliation is common. There is no difference in the total frequency of re-intervention between patients with a MBTS and an RVPAS, though the types and timing of re-intervention did vary between shunt types. Longitudinal assessment of the NPC-QIC database will be important to identify long term outcomes of patients requiring re-intervention.
Footnotes
- Oral Contributions
- Room 146 C
- Sunday, March 19, 2017, 9:17 a.m.-9:27 a.m.
- Session Title: Highlighted Original Research: Congenital Heart Disease and the Year in Review
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 908-14
RED BLOOD CELL DISTRIBUTION WIDTH AND OUTCOMES IN FONTAN PATIENTS
Georges Ephrem, Amirhossein Esmaeeli, Jennifer Gerardin, Anita Saraf, Salim Hayek, Staci Jennings, Agasha Katabarwa, Fred Rodriguez, Arshed Quyyumi and Wendy Book
vol. 69 no. 11 Supplement 560
DOI:
https://doi.org/10.1016/S0735-1097(17)33949-9
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Georges Ephrema,b,
- Amirhossein Esmaeelia,b,
- Jennifer Gerardina,b,
- Anita Sarafa,b,
- Salim Hayeka,b,
- Staci Jenningsa,b,
- Agasha Katabarwaa,b,
- Fred Rodrigueza,b,
- Arshed Quyyumia,b and
- Wendy Booka,b
- aEmory University School of Medicine, Atlanta, GA, USA
- bSibley Heart Center Cardiology, Atlanta, GA, USA
Background: Fontan palliation results in late multi-organ co-morbidity. However, predictors of worse prognosis are lacking. We evaluated the association of red blood cell distribution width (RDW) with functional capacity and inflammatory biomarkers shown to be elevated in adult Fontan patients compared with age-matched controls.
Methods: Data from adult Fontan patients enrolled in a prospective registry were analyzed. RDW was assessed in relation to total distance walked on 6 minute walk test and biomarkers of general and pathway-specific inflammation. RDW greater than the upper limit of normal (14.4%) was considered elevated.
Results: Of the 79 patients (median age 29.5 years, 49% male, 19% black, 59% total cavopulmonary connection, and Fontan time 22 years) 31 (39%) had high RDW. Compared to low RDW, high RDW was associated with lower hemoglobin (14.4 g/dL vs 15.9 g/dL; p=0.011) and lower 6-minute walk distance (411 m vs 454 m, p=0.038) (Table part A). In the subgroup with biomarker data (n=22), high RDW correlated with higher levels of urokinase-type plasminogen activator receptor (sUPAR) compared to normal RDW (Table part B).
Conclusions: In this single center study of adult Fontan patients, high RDW was associated with poorer functional status and higher levels of sUPAR, an inflammatory biomarker. Studies with larger sample size are warranted to elucidate the prospect of this inexpensive, readily available biomarker in risk classification and prognostication of Fontan patients.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Friday, March 17, 2017, 10:00 a.m.-10:10 a.m.
- Session Title: Congenital Heart Disease: To the Third Decade and Beyond
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1131M-03
THE SYSTEMIC RIGHT VENTRICLE IN TRANSPOSITION OF THE GREAT ARTERIES: WHAT CAN WE LEARN FROM SERIAL IMAGING?
Matthew J. Lewis, Michiel Winter, Alexandra Van Dissel, Jonathan Ginns, Noa Zemer-Wassercug, Barbara Mulder and Marlon Rosenbaum
vol. 69 no. 11 Supplement 561
DOI:
https://doi.org/10.1016/S0735-1097(17)33950-5
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Matthew J. Lewisa,b,
- Michiel Wintera,b,
- Alexandra Van Dissela,b,
- Jonathan Ginnsa,b,
- Noa Zemer-Wassercuga,b,
- Barbara Muldera,b and
- Marlon Rosenbauma,b
- aColumbia University Medical Center, New York, NY, USA
- bAMC, Amsterdam, The Netherlands
Background: Adult patients with congenitally corrected transposition of the great arteries (ccTGA) and D-transposition of the arteries (D-TGA) after a Mustard or Senning repair develop systemic right ventricular (SRV) dilation. However, the time frame and risk factors for progressive SRV enlargement remain unclear. We assessed the hypothesis that progressive SRV enlargement would be present and associated with patient specific factors over serial cardiac MRIs (CMR).
Methods: A retrospective study of all patients age>18 years with a SRV who underwent serial CMRs at Columbia University Medical Center and the University of Amsterdam Academic Medical Center was performed. Ventricular size and function was assessed by CMR. Clinical and echocardiographic variables were also assessed.
Results: 105 patients (65% male), with a mean age of 32 ± 9 years met inclusion criteria. 29 (28%) had ccTGA and 76 (72%) had undergone a Mustard or Senning repair. 28 (27%) were on an ACE-inhibitor, 21 (20%) were on a beta-blocker, and 23 (22%) were obese. Mean time between CMRs was 3.5 ± 1.6 years. Mean right ventricular end-diastolic volume (RVEDV) and right ventricular end-systolic volume (RVESV) were significantly different between the first and second CMR (243 ml vs. 255 ml, p=0.0002 and 142 ml vs. 162 ml, p<0.0001). There was no significant change in right ventricular ejection fraction. In a multivariable regression model of change in RVEDV that included follow-up duration, obesity, ≥ moderate tricuspid regurgitation (TR), gender and diagnosis, only follow-up duration (β=6.2, p=0.002) and obesity (β=14.8, p=0.047) were significant. In the same model with change in RVESV as the outcome, follow-up duration (β=5.9, p=0.046) and obesity (β=23.2 p=0.043) remained the only significant covariates. Ace-inhibitor and beta-blocker use were not significantly associated with either change in RVEDV or RVESV.
Conclusions: In our multicenter cohort of patients with D-TGA and ccTGA, progressive SRV enlargement was observed by CMR. Obesity, but not TR, was associated with a greater degree of SRV dilation over the study period. These results may have implications on how patients with a SRV are followed.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Friday, March 17, 2017, 10:15 a.m.-10:25 a.m.
- Session Title: Congenital Heart Disease: To the Third Decade and Beyond
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1131M-05
OUTCOMES OF DIRECT CURRENT CARDIOVERSION IN ADULTS WITH CONGENITAL HEART DISEASE
Alexander C. Egbe, Samuel Asirvatham, Suraj Kapa, Heidi Connolly and Naser Ammash
vol. 69 no. 11 Supplement 562
DOI:
https://doi.org/10.1016/S0735-1097(17)33951-7
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Alexander C. Egbe,
- Samuel Asirvatham,
- Suraj Kapa,
- Heidi Connolly and
- Naser Ammash
- Mayo Clinic, Rochester, MN, USA
Background: Few data exist on direct current cardioversion (DCCV) in adult patients with congenital heart disease (CHD).
Methods: This was a retrospective case-control study of 279 adults with CHD and 279 adults without CHD (control group) who had elective DCCV for atrial arrhythmias at the Mayo Clinic Cardioversion Unit from 2001 through 2013. Control patients were matched by sex and arrhythmia type. Our objective was to compare DCCV procedural failure (failure to terminate the presenting arrhythmia) and arrhythmia recurrence between CHD and non-CHD patients
Results: In the CHD group (mean age, 55±20 years; 166 [59%] were men), the most common diagnosis was Fontan physiology (61; 22%). Transesophageal echocardiography (TEE) was performed before DCCV in 216 patients (77%); 162 (58%) had atrial flutter, and 117 (42%) had atrial fibrillation. Patients in the control group were older (mean age, 72±14 years; P<.001). Procedural failure occurred in 38 patients (14%) in the CHD group and in 20 (7%) in the non-CHD group (P=.01). There were no deaths or thromboembolic complications. The CHD group had a higher rate of arrhythmia recurrence (83% vs 66% at 60 months, P=.001). The multivariable risk factors for procedural failure were Fontan palliation and spontaneous echocardiographic contrast; the risk factors for arrhythmia recurrence were Fontan palliation and atrial fibrillation. When Fontan patients were excluded from the analysis, the outcome of DCCV (failure and recurrence rates) was similar for the CHD and non-CHD groups despite the age difference between the cohorts.
Conclusions: Outcomes after DCCV were similar for CHD and non-CHD patients, with the exception of Fontan patients. DCCV is safe in adults with CHD when performed in a specialized unit with safety precautions such as verification of adequacy of anticoagulation and frequent use of TEE to exclude intracardiac thrombus before DCCV.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Friday, March 17, 2017, 10:30 a.m.-10:40 a.m.
- Session Title: Congenital Heart Disease: To the Third Decade and Beyond
- Abstract Category: 11. Congenital Heart Disease: Therapy
- Presentation Number: 1131M-07
PREVALENCE AND INCIDENCE OF HEART FAILURE IN ADOLESCENTS AND ADULTS WITH REPAIRED TETRALOGY OF FALLOT
Andreas P. Kalogeropoulos, Panagiotis Savvoulidis, Anita Saraf, Fred Rodriguez, Trenton Hoffman, Cheryl Raskind-Hood, Carol Hogue and Wendy Book
vol. 69 no. 11 Supplement 563
DOI:
https://doi.org/10.1016/S0735-1097(17)33952-9
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Andreas P. Kalogeropoulosa,b,
- Panagiotis Savvoulidisa,b,
- Anita Sarafa,b,
- Fred Rodrigueza,b,
- Trenton Hoffmana,b,
- Cheryl Raskind-Hooda,b,
- Carol Hoguea,b and
- Wendy Booka,b
- aEmory University, Atlanta, GA, USA
- bSibley Heart Center, Atlanta, GA, USA
Background: Data on the prevalence and incidence of heart failure (HF) among adolescents and adults with repaired tetralogy of Fallot (rToF) are limited.
Methods: We identified 524 patients age 10 or older who received services for repaired tetralogy of Fallot (ICD9-CM code 745.2; repair was identified through codes V13.65 and V15.1) in our institution between 2008 and 2014 (cohort inception). Prevalent HF was defined as presence of ICD9-CM codes 428, 402.X1, 404.X1, and 404.X3 (Medicare definition) at cohort entry. Incident HF was defined as new HF-associated services after cohort entry.
Results: Median age was 32 years (Q1-Q3: 24-42); 55.3% were female; 69.5% were white, 19.7% black, and 10.9% of other or unknown race. Prevalence of HF at cohort entry was 203/524 (38.7%), with significantly higher rates after age 20 and exceeding 50% among those over age 40, Fig. 1. Among the 321 patients without HF at entry, 163 received HF-related services over a median of 3.0 (0.8-5.5) years. By 5 years, 50.2% of patients received new HF-related services. Risk for HF was higher among those of age 40 or older (Fig. 2) and did not differ in female vs. male patients (hazard ratio [HR] 1.02; 95%CI: 0.74-1.40; P=0.90). However, blacks had significantly higher risk for HF vs. whites (HR: 1.68; 95%CI: 1.18-2.38; P=0.004) in age- an sex-adjusted models.
Conclusions: In a contemporary rToF population of adolescents and adults, HF prevalence increased sharply with age and 5-year incidence was 50% with higher rates among blacks and those over age 40.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Friday, March 17, 2017, 10:45 a.m.-10:55 a.m.
- Session Title: Congenital Heart Disease: To the Third Decade and Beyond
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1131M-09
OUTCOMES OF NON-CARDIAC PROCEDURES IN ADULT FONTAN PATIENTS
Alexander C. Egbe, Heidi Connolly, Carole Warnes, Arooj Khan and Sameh Said
vol. 69 no. 11 Supplement 564
DOI:
https://doi.org/10.1016/S0735-1097(17)33953-0
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Alexander C. Egbe,
- Heidi Connolly,
- Carole Warnes,
- Arooj Khan and
- Sameh Said
- Mayo Clinic, Rochester, MN, USA
Background: Limited data exist about the outcomes of non-cardiac procedures (NCP) in Fontan patients.
Methods: Retrospective review of NCPs in adult Fontan patients performed at Mayo Clinic, 1990-2015. To describe procedural outcomes after NCP in Fontan patients, and compare outcomes to two control groups: patients with repaired congenital heart disease and biventricular circulation (CHD-BiV) and patients with no heart disease (NHD).
We matched the procedure in the Fontan patients to similar procedures in CHD-BiV patients and NHD patients. The controls were matched by age (±5 years), gender, procedure type, and year of procedure (±5 years). Cyanosis defined as saturation <90%. Procedural hypoxia defined as saturation <80% or a drop in saturation >10% from baseline.
Results: 154 adult Fontan patients underwent 538 NCPs, age 30±8 years. The most common procedures were esophagogastroduodenoscopy 135(25%), dental extraction 50(9%), and bronchoscopy 35(7%). The following types of sedation and anesthesia were used: moderate/deep sedation in 256 (48%), general anesthesia in 51(10%), minimal sedation in 105 (20%), local anesthesia 75 (14%), and regional anesthesia in 51 (9%) procedures.
There were 93 procedural complications in 79 procedures (15%). These complications were (arrhythmia requiring intervention 9, hypotension 14, bradycardia 8, hypoxia 38, heart failure requiring intravenous diuretics 2, acute renal failure 3, bleeding requiring blood transfusion 1, unplanned procedures for placement dialysis lines 2, readmission within 72 hours, unplanned hospitalization for hypoxia 8, and unplanned transfer to intensive care unit 1). Baseline cyanosis was the only multivariable risk factor for procedural complications (HR 1.87, 95% CI 1.14-3.67, P=0.04).
Matched cohorts of 282 procedures were selected for each group. Procedural complications were more common in the Fontan group (18%) compared to the CHD-BiV group (5%) and NHD group (1.4%), P<0.001.
Conclusions: Complications after NCPs was more common in Fontan patients, and baseline cyanosis was a risk factor for complications. All-cause mortality was low presumably because of a multi-disciplinary care approach used in this center.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Friday, March 17, 2017, 11:00 a.m.-11:10 a.m.
- Session Title: Congenital Heart Disease: To the Third Decade and Beyond
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1131M-11
NEUROCOGNITIVE IMPAIRMENT IS COMMON IN THE ADULT WITH CONGENITAL HEART DISEASE: IDENTIFICATION USING A NOVEL CLINICAL QUESTIONNAIRE
Scott Cohen, Ashley Leverenz, Michael Reis, Laura Umfleet, Salil Ginde, Peter Bartz and Michael Earing
vol. 69 no. 11 Supplement 565
DOI:
https://doi.org/10.1016/S0735-1097(17)33954-2
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Scott Cohen,
- Ashley Leverenz,
- Michael Reis,
- Laura Umfleet,
- Salil Ginde,
- Peter Bartz and
- Michael Earing
- Medical College of Wisconsin, Milwaukee, WI, USA
Background: Children with congenital heart disease (CHD) and adults with acquired heart disease are at an increased risk of neurocognitive impairment. The prevalence of neurocognitive impairment and its risk factors in the adult congenital heart disease (ACHD) population is not well described.
Methods: The Wisconsin Adult Congenital Heart Disease (WAtCH) Program recently began screening ACHD patients to identify those at high risk of having neurocognitive impairments. Screening consists of using a validated neuro-oncology screening instrument that has been modified for the ACHD population. It consists of 10 questions answered on a Likert scale that measure a subject’s self perceived competence in 8 neurocognitive domains (attention, memory, language, executive functioning, independence in activities of daily living, math, processing speed and reading). Patients who answer this survey in a predetermined high risk fashion are then referred for a formal neurocognitive evaluation. Demographic information, type of CHD, number of surgeries and medications at the time of the survey are obtained by chart review.
Results: In the pilot phase of the neurocognitive screening program 310 patients (49% males) completed the screening process. The average age of patients who underwent screening was 30 years (range: 17-69 years). For the cohort, 57 (18%) patients had no prior cardiac surgeries, 85 (28%) one surgery, 77 (25%) two, and 91 (29%) at least three surgeries. Of those screened, 106 (34%) met the high risk criteria for a formal neurocognitive evaluation. Patients who met the high risk criteria had undergone a greater number of prior cardiac surgeries (2.2 vs 1.7, p=0.008) and were more likely to have severe complexity CHD (p=0.006). Of those patients that met the high risk criteria, the neurocognitive domains in which they had the worst perceived functioning were math and attention.
Conclusions: Our pilot data, confirms there is a high prevalence of ACHD patients that qualify for neurocognitive testing. Simple screening questionnaires may help identify those patients at high risk and allow for timely and appropriate referral for formal neurocognitive evaluation, diagnosis and therapy.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Friday, March 17, 2017, 11:15 a.m.-11:25 a.m.
- Session Title: Congenital Heart Disease: To the Third Decade and Beyond
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1131M-13
TWENTY YEAR TRENDS IN MATERNAL AND PERINATAL COMPLICATIONS IN PREGNANT WOMEN WITH HEART DISEASE
Samuel C.B. Siu, Mathew Sermer, Jennifer Mason, Rachel Wald, Jack Colman and Candice Silversides
vol. 69 no. 11 Supplement 566
DOI:
https://doi.org/10.1016/S0735-1097(17)33955-4
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Samuel C.B. Siua,b,
- Mathew Sermera,b,
- Jennifer Masona,b,
- Rachel Walda,b,
- Jack Colmana,b and
- Candice Silversidesa,b
- aWestern University, London, Canada
- bUniversity of Toronto, Toronto, Canada
Background: Pregnant women with heart disease are at increased risk of complications. At our centre, management algorithms for this population have been implemented since 2001. However, the impact of standardized care on outcomes has not been evaluated.
Methods: We prospectively recorded baseline and outcomes data on consecutive pregnant women with heart disease referred to our centre from 1994 to 2014. We compared the frequency of complications in women followed during 2 time periods: 1994-2001 and 2001-2014. Risk of cardiac complications was assessed using the validated Canadian Pregnancy and Heart Disease Study (CARPREG) and the modified World Health Organization (WHO) risk classifications. Cardiac (maternal death, heart failure, arrhythmia, or stroke) and perinatal (small-for-gestational-age birth weight or premature birth) complications were recorded.
Results: The study group comprised of 1434 pregnancies in women with heart disease; 65% of pregnancies were in women with congenital heart disease. There was no significant baseline differences between women that underwent pregnancy prior to 2001 (n=415) and those that underwent pregnancy after 2001 (n=1019), with respect to maternal age, prior history of cardiac events, or underlying cardiac diagnosis. The proportion of women in the highest CARPREG/WHO risk group was higher pre 2001 compared to post 2001 (24% vs. 19%; p=0.041). Maternal mortality was rare (0.3%) and, along with perinatal mortality (2%), remained unchanged during the entire 20 year period. While there was no overall change in cardiac complications between the pre 2001 and post 2001 (15% vs. 14%, p=0.4) periods, a reduction in cardiac complications occurred in the highest risk CARPREG/WHO group (35% pre 2001 vs. 22% in the post 2001, p=0.025). Perinatal complication rate was not significantly different between the pre 2001 (32%) and the post 2001 period (31%).
Conclusions: During the past 20 years, pregnancy in women with heart disease has been associated with unchanged low maternal mortality. However, there continues to be significant morbidity in both mother and baby. The high perinatal complication rate highlights the need for new management strategies.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Friday, March 17, 2017, 11:30 a.m.-11:40 a.m.
- Session Title: Congenital Heart Disease: To the Third Decade and Beyond
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1131M-15
LONG-TERM FOLLOW-UP IN ADULT SURVIVORS OF PULMONARY ATRESIA WITH INTACT VENTRICULAR SEPTUM
Christine Bui, Wilson Lam, Wayne Franklin and Peter Ermis
vol. 69 no. 11 Supplement 567
DOI:
https://doi.org/10.1016/S0735-1097(17)33956-6
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Christine Bui,
- Wilson Lam,
- Wayne Franklin and
- Peter Ermis
- Texas Children’s Hospital, Baylor College of Medicine, Houston, TX, USA
Background: Early childhood palliation for pulmonary atresia with intact ventricular septum (PA-IVS) can range from biventricular repair to single ventricle palliation. This study aims to evaluate the need for additional interventions long-term in a survivor cohort of adult PA-IVS patients following initial surgical palliation.
Methods: All patients 18 years of age and older with a diagnosis of PA-IVS seen in the adult congenital cardiology clinic at our institution from 2010 – 2016 were included. Charts were retrospectively reviewed for initial surgical repair, demographics, and long-term co-morbidities.
Results: Thirty-seven PA-IVS adults were identified. The mean age was 24.4 (18-43) years. Initial surgical repair was a Fontan operation (18, 49%), a 1.5 ventricular repair (5, 14%), or a biventricular repair (14, 38%). Mean follow-up after initial palliation was 18.9 (12-36) years. There were no deaths within the study period (2010-2016). One patient required cardiac transplantation 13 years after initial palliation. Seventeen patients (46%) required re-intervention at an average of 13.3 (3-34) years following initial palliation. Four (22%) Fontan patients required a Fontan revision. Three (60%) patients with 1.5 ventricular repair required conduit replacement, stent implantation, or angioplasty. Ten (71%) biventricular patients required re-intervention; pulmonary valve replacement was the most common (n=8, one percutaneous), followed by tricuspid valve repair or replacement (n=4, one percutaneous). Atrial arrhythmias were present in 13 (35%) and ventricular arrhythmias in 9 (24%) patients. Three patients had clinically significant liver disease.
Conclusions: We report the largest cohort of adult survivors with palliated PA-IVS following initial palliation. During a limited study interval, there was no mortality. While surgical or catheter-based re-interventions were often performed, the need for re-intervention in this group was much less than previously reported (46% vs 100%). Additional studies are needed that could illustrate the optimal timing and indication for re-intervention in PA-IVS patients.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Friday, March 17, 2017, 11:45 a.m.-11:55 a.m.
- Session Title: Congenital Heart Disease: To the Third Decade and Beyond
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1131M-17
GROWTH DYNAMICS OF AORTA IN BICUSPID AORTIC VALVE PATIENTS FROM INFANCY TO YOUNG ADULT AGE
Talha Niaz, Joseph Poterucha, Jonathan Johnson, Timothy Olson and Donald Hagler
vol. 69 no. 11 Supplement 568
DOI:
https://doi.org/10.1016/S0735-1097(17)33957-8
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 30, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Talha Niaz,
- Joseph Poterucha,
- Jonathan Johnson,
- Timothy Olson and
- Donald Hagler
- Mayo Clinic, Rochester, MN, USA
Background: Bicuspid aortopathy has been a center point of interest in patients with bicuspid aortic valve (BAV). Our aim was to study the age wise growth of aorta in patients with isolated BAV from infancy to young adult age.
Methods: The Mayo Clinic echocardiography database was retrospectively analyzed to identify pediatric and young adult patients (≤ 22 years) diagnosed with BAV from 1990-2015. All echocardiograms performed prior to any intervention on aortic valve or aorta were analyzed for aortic measurements formatted as z-scores.
Results: We identified a total of 1010 patients with BAV, out of which 619 had isolated BAV. The distribution of morphology of cusp fusion in isolated BAV was right-left fusion (RL) in 419 (67.7%), right-non coronary fusion (RN) in 197 (31.8%) and left-non coronary fusion (LN) in 3 (0.5%) subjects. Mid-ascending aorta was abnormally dilated (defined as z-score > 2) during pediatric and young adult age, and it was present even during the first year of life in patients with RN fusion. Moreover patients with RN fusion had significantly larger mid-ascending aorta diameter than patients with RL fusion (p<0.001). There was no significant sinus of Valsalva dilation, though patients with RL fusion had larger sinus of Valsalva diameter as compared to RN fusion (p<0.04). There was a period of peak growth of aorta around 8 years of age.
Conclusions: Abnormal dilation of ascending aorta begins in childhood and shows interesting growth patterns from infancy to adolescence into adulthood.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Friday, March 17, 2017, 3:45 p.m.-3:55 p.m.
- Session Title: Predicting Outcomes in Pediatric Heart Disase
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1171M-03
INSURANCE TYPE IS ASSOCIATED WITH LONGER HOSPITAL DURATION BUT SIMILAR MORTALITY AMONG CHILDREN UNDERGOING CONGENITAL HEART SURGERY
Kathleen Ryan, Claudia Algaze, Charlotte Sakarovitch, Thomas Do, Vamsi Yarlagadda, Susan Fernandes, Doff McElhinney, Stephen Roth, Catherine Krawczeski and Andrew Shin
vol. 69 no. 11 Supplement 569
DOI:
https://doi.org/10.1016/S0735-1097(17)33958-X
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Kathleen Ryan,
- Claudia Algaze,
- Charlotte Sakarovitch,
- Thomas Do,
- Vamsi Yarlagadda,
- Susan Fernandes,
- Doff McElhinney,
- Stephen Roth,
- Catherine Krawczeski and
- Andrew Shin
- Lucile Packard Children’s Hospital at Stanford, Palo Alto, CA, USA
Background: Recent studies have shown public health insurance (HI) programs are associated with worse postoperative outcomes among pediatric surgical patients. We aimed to determine if this relationship exists among children undergoing congenital heart surgery.
Methods: Children undergoing congenital heart surgery between January 1, 2012 and December 31, 2013 were identified within the Pediatric Health Information System database. All patients aged <21 years undergoing congenital heart surgery classifiable by Risk Adjustment in Congenital Heart Surgery (RACHS-1) score were included. We evaluated the risk-adjusted association between HI type and in-hospital mortality and hospital length of stay (LOS) using multivariable hierarchical regression models. We adjusted for variables selected based upon expected clinical risk or potential confounding effect [RACHS-1, race, ethnicity, gender, age, baseline complex chronic condition (CCC) and Pediatric Medical Complexity Algorithm].
Results: We analyzed 15,696 pediatric cardiac surgical admissions. Patients with public insurance (n=7272, 46%) were more likely to be younger (14 [4,55] vs 23 [4,84] months, p<0.001), Hispanic (26% vs 7%, p<0.001), non-white (49.3% vs 37.5%, p<0.001) and have CCC (Gastrointestinal 10.7% vs 7.0%; Hematologic or Immunologic 4.3% vs 3.2%; metabolic 2.9% vs 2.1%; respiratory 4.5% vs 3.6%, p<0.001). The risk-adjusted odds ratio for in-hospital mortality was not significant (OR=1.59, p=0.086). The mean LOS among public HI patients was 9.5 (±12.4) days and 8.0 (±9.8) days among private (p=0.001). Children with public HI had longer adjusted LOS (β=0.69 days, p<0.001).
Conclusions: Despite disparities in other pediatric surgical procedures, we found no difference in mortality based on primary payer status in children undergoing congenital heart surgery. We did find children with public HI were more likely to have CCC. Nonetheless, adjusted risk analysis showed that public insurance programs were associated with longer hospital duration.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Friday, March 17, 2017, 4:00 p.m.-4:10 p.m.
- Session Title: Predicting Outcomes in Pediatric Heart Disase
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1171M-05
RISK STRATIFICATION OF CHILDREN UNDERGOING VALVE-SPARING REPAIR OF TETRALOGY OF FALLOT
Sophie C. Hofferberth, Sitaram Emani, Minmin Lu, Lynn A. Sleeper, Fatima Lunze, Gerald Marx, Christopher Baird, Pedro del Nido and Meena Nathan
vol. 69 no. 11 Supplement 570
DOI:
https://doi.org/10.1016/S0735-1097(17)33959-1
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Sophie C. Hofferberth,
- Sitaram Emani,
- Minmin Lu,
- Lynn A. Sleeper,
- Fatima Lunze,
- Gerald Marx,
- Christopher Baird,
- Pedro del Nido and
- Meena Nathan
- Boston Children’s Hospital, Harvard Medical School, Boston, MA, USA
Background: Patient-based determinants of pulmonary valve (PV) function post valve-sparing repair (VSR) of tetralogy of Fallot (ToF) are unknown. We developed a risk score for structural valve deterioration (SVD) in patients undergoing VSR of ToF.
Methods: All patients who underwent VSR of ToF at <1 year of age were assessed. Multivariable Cox regression was used to develop a risk score for SVD; defined as a composite endpoint of PV reintervention, PV peak gradient ≥ 40mmHg and ≥ moderate PV regurgitation.
Results: From 2007-2015, 207 consecutive patients (median age: 98 days, IQR: 72, 129) underwent VSR of ToF. PV morphology was tricuspid in 37 (18%), bicuspid in 151 (73%) and unicuspid in 18 (9%) patients. Median PV annulus Z-score was −2.1 (IQR: −2.4, −1.6). Freedom from SVD was 65%, 50% and 40% at 1, 3 and 5 years post VSR. Univariate analysis showed PV annulus Z score <-1.77 (p≤0.001), uni- or bicuspid PV morphology (p=0.002), dysplastic leaflets, (p=0.007) and younger age (p=0.009) were associated with SVD. Multivariable analysis identified PV annulus size (HR 0.46, CI 0.32, 0.68; p<0.001) and unicuspid PV morphology (HR 3.78, CI 1.74, 8.24; p=0.003) as independent predictors of SVD. Patients in the upper risk score categories (50-<75%tile, ≥75%tile) were more likely to develop SVD (Figure 1, p≤0.001).
Conclusions: VSR of ToF is associated with a high incidence of SVD. Risk stratification based on PV anatomy identifies patients at high-risk of early valve failure post VSR, this may be useful to guide therapy.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Friday, March 17, 2017, 4:15 p.m.-4:25 p.m.
- Session Title: Predicting Outcomes in Pediatric Heart Disase
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1171M-07
STABLE INCIDENCE OF ENDOCARDITIS IN PEDIATRIC PATIENTS BEFORE AND AFTER THE 2007 ENDOCARDITIS PROPHYLAXIS GUIDELINES
Stephen Dolgner and Titus Chan
vol. 69 no. 11 Supplement 571
DOI:
https://doi.org/10.1016/S0735-1097(17)33960-8
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Stephen Dolgner and
- Titus Chan
- Seattle Children’s Hospital, Seattle, WA, USA
Background: Endocarditis is a rare but potentially devastating form of acquired heart disease that can have a significant impact on pediatric patients, particularly those with pre-existing congenital heart disease. The 2007 American Heart Association endocarditis guidelines substantially decreased the number of patients for whom endocarditis prophylaxis was recommended. Previous studies have examined changes in the proportions of hospitalized patients but national estimates of pediatric endocarditis hospitalizations have not been performed.
Methods: Hospital admissions with the diagnosis of endocarditis in patients <21 years old from the Kids’ Inpatient Database were identified from the following years: 2000, 2003, 2006, 2009, 2012. Patients were divided into groups based on age, underlying congenital heart disease, and etiologic organism, if available. Descriptive comparisons were made over time.
Results: Overall, the national estimates for endocarditis hospitalizations did not change dramatically from 2000 to 2012 and ranged between 913 and 1093 cases per year. The average annual national endocarditis hospitalization rates before and after the 2007 guidelines were 12.7 and 11.7 per 1,000,000 children, respectively. The proportion of endocarditis patients with congenital heart disease was also stable between 38-44% (p=0.44). The endocarditis bacteriology was also stable over this time interval, with the most frequently identified pathogen being Staphylococcus(35-41%, p=0.23). There was an increase in endocarditis cases in patients between 17 and 20 years old from 276 cases in 2000 to 394 cases in 2012 (p<0.001), but the percentage of patients with congenital heart disease in these older patients remained similar. There was an increase in mean length of stay by 1.1 days every three years (p=0.01), and mean cost increased by 50% from 2003 to 2012 in 2012 dollars (from $61,491 in 2003 to $92,211 in 2012).
Conclusions: Despite decreasing use of antibiotic prophylaxis since the 2007 endocarditis guidelines, there has been a stable incidence of endocarditis hospitalizations in all patients groups and specifically in patients with underlying congenital heart disease.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Saturday, March 18, 2017, 12:30 p.m.-12:40 p.m.
- Session Title: Therapeutic Advances in Congenital Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1220M-03
SAFETY OF ENALAPRIL IN INFANTS: DATA FROM THE PEDIATRIC HEART NETWORK INFANT WITH SINGLE VENTRICLE TRIAL
Kanika Mathur, Jacqueline Lamour, Daphne Hsu and Scott I. Aydin
vol. 69 no. 11 Supplement 572
DOI:
https://doi.org/10.1016/S0735-1097(17)33961-X
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Kanika Mathur,
- Jacqueline Lamour,
- Daphne Hsu and
- Scott I. Aydin
- Children’s Hospital at Montefiore, Bronx, NY, USA
Background: Angiotension converting enzyme (ACE) inhibitor therapy has been shown to improve ventricular function and clinical outcomes in adult patients with heart failure. Despite the lack of safety and efficacy data, empiric use of ACE inhibitor therapy is common in infants and children with cardiomyopathy and congenital heart disease. The Pediatric Heart Network Infant with Single Ventricle (ISV) trial provides the opportunity to describe the safety and adverse effects of enalapril in a large group of infants with complex congenital heart disease.
Methods: Neonates with a single ventricle (SV) were prospectively enrolled in a randomized trial of enalapril vs. placebo. Patients were followed to 14 months of age and data including demographics, survival, drug administration and safety were collected. Descriptive statistics and univariate analyses were performed using student t-test, chi-square, Mann-Whitney-U, and Fisher’s exact tests.
Results: The ISV trial randomized 230 patients, 185 of whom completed the study. Median age at drug initiation was 19 days [7, 46]. Initial enalapril dose was 0.025 – 0.05 mg/kg/dose and mean dose was 0.31 ± 0.13 mg/kg/day. There was no significant difference in mean percent change in blood pressure (BP) from baseline to lowest BP at initiation of drug (-11 ± 11 vs. −12 ± 11, p = 0.51) between placebo and enalapril. There was no difference in percent change in BP during re-initiation of study drug after the Glenn or any temporary stop (-9 ± 12 vs. −10 ± 11, p = 0.55). There was no difference in percent change of BP during all dose adjustments (-11 ± 7 vs. −12 ± 8, p = 0.39). The number of patients who suffered hyperkalemia (49% vs. 57%, p = 0.24), renal dysfunction (0% vs. 3%, p = 0.12), or neutropenia (33% vs. 28%, p = 0.39) was no different between the placebo and enalapril cohorts. There was no difference in the number of reported adverse events (23% vs. 28%, p = 0.45), temporary stops (31% vs. 34%, p = 0.67), or permanent stops (47% vs. 37%, p = 0.14) between placebo and enalapril groups.
Conclusions: In this group of infants with a SV, enalapril use was not associated with significant adverse events. Enalapril use appears to be low risk in infants and children with significant heart disease.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Saturday, March 18, 2017, 12:45 p.m.-12:55 p.m.
- Session Title: Therapeutic Advances in Congenital Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1220M-05
ASSOCIATION OF FRACTURES WITH FUROSEMIDE THERAPY IN PEDIATRIC MEDICAID PATIENTS WITH CONGENITAL HEART DISEASE
Ji Haeng Heo, Karen L. Rascati, Keila Lopez and Brady Moffett
vol. 69 no. 11 Supplement 573
DOI:
https://doi.org/10.1016/S0735-1097(17)33962-1
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- aThe University of Texas at Austin, Austin, TX, USA
- bTexas Children’s Hospital, Houston, TX, USA
Background: Furosemide is a loop diuretic that may cause a loss of bone mineral density, and thus an increased incidence of bone fractures. Congenital heart disease (CHD) patients are often placed on furosemide. The purpose was to determine the association of furosemide therapy with the incidence of bone fractures in pediatric CHD patients.
Methods: Data were extracted from Texas Medicaid databases. Pediatric patients aged < 12 years diagnosed with CHD, cardiomyopathy, or heart failure (2008 – 2014; median follow-up 3 years) were included. Patients taking furosemide were categorized into two groups: (1) Furosemide-Adherent group (Medication Possession Ratio (MPR) ≥ 70%), and (2) Furosemide Non-adherent group (MPR < 70%). A third group of patients was matched to the furosemide user groups by employing propensity score matching. A multivariate logistic regression and Cox proportional hazard model with a Kaplan-Meier plot (time-to-fracture) were used to compare the three groups, controlling for baseline demographics and clinical characteristics.
Results: After matching, 3,912 patients (Furosemide-Adherent: 254, Furosemide Non-Adherent: 724, No Furosemide: 2,934) were identified. The incidence of fractures was highest for the furosemide-adherent group (9.06%; 23/254), followed by the Furosemide Non-Adherent group (7.18%; 52/724), which were both higher than for patients who did not receive furosemide (5.04%; 148/2,934) (p <0.001). Using logistic regression, (reference group = no furosemide) both furosemide groups were more likely to have fractures compared to the reference; Furosemide-Adherent OR=1.87 (95% CI: 1.17 −2.98), p=0.009; Furosemide-Non-Adherent OR=1.53 (95% CI: 1.10-2.14), p=0.011. In the Cox proportional hazard model, the risk of fractures for the furosemide-adherent group was significantly higher compared to the no furosemide group (HR=1.56; 95% CI: 1.01-2.42), p=0.049.
Conclusions: Our results indicated that furosemide therapy in children with CHD was associated with an increased risk of bone fractures. Clinicians who treat patients with heart disease should be aware of the increased risk of fractures and screen for bone disease in this patient population.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Saturday, March 18, 2017, 1:00 p.m.-1:10 p.m.
- Session Title: Therapeutic Advances in Congenital Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1220M-07
EFFECT OF OBESITY AND UNDERWEIGHT STATUS ON PERIOPERATIVE OUTCOMES IN PATIENTS WITH CONGENITAL HEART DISEASE: AN ANALYSIS OF DATA FROM THE SOCIETY OF THORACIC SURGEONS CONGENITAL HEART SURGERY DATABASE
Michael L. O’Byrne, Sunghee Kim, Christoph Hornik, Babatunde Yerokun, Roland Matsouaka, Jeffrey Jacobs, Marshall Jacobs and Richard Jonas
vol. 69 no. 11 Supplement 574
DOI:
https://doi.org/10.1016/S0735-1097(17)33963-3
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 30, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Michael L. O’Byrnea,b,
- Sunghee Kima,b,
- Christoph Hornika,b,
- Babatunde Yerokuna,b,
- Roland Matsouakaa,b,
- Jeffrey Jacobsa,b,
- Marshall Jacobsa,b and
- Richard Jonasa,b
- aChildren’s National Medical Center, Washington, DC, USA
- bDuke University School of Medicine, Durham, NC, USA
Background: Obesity is increasingly prevalent in the congenital heart disease population. The effect of obesity and body-mass index (BMI) on perioperative outcomes has not been evaluated. We sought to study the association between BMI and perioperative outcomes following congenital heart operations in children and young adults.
Methods: A multicenter retrospective cohort study was performed using data from the Society of Thoracic Surgeons Congenital Heart Surgery Database of children and young adults between 10-35 years undergoing any cardiac operation from 1/2010 to 12/2015. The primary exposure was BMI percentile, adjusted for age and sex. The primary outcomes were operative mortality and composite outcome (operative mortality, major complications, post-operative hospital length of stay >14 days, and wound infection/dehiscence). The association between BMI percentile and primary outcomes was assessed using multivariate mixed effects models adjusting for demographic, preoperative and operative factors including STS-EACTS Mortality Category.
Results: Of 18,337 subjects undergoing index operations at 118 centers, 16% were obese (BMI percentile>95%), 15% overweight (85-95%), 53% normal weight (15-85%), 7% underweight (5-15%), and 9% were severely underweight (5thpercentile). The observed risks of operative mortality (p=0.04) and composite outcome (p<0.0001) were higher in severely underweight and obese subjects than in normal weight subjects. Risk of unplanned cardiac operation and reoperation for bleeding was higher with severely underweight BMI. Risk of wound infection/dehiscence was higher in obese subjects. In multivariate analysis, the association between BMI and operative mortality was not significant. Obese (OR: 1.21, 95% CI: 1.05-1.39), underweight (OR: 1.33, 95% CI: 1.11-1.60), and severely underweight subjects (OR: 1.53, 95% CI: 1.31-1.79) were at increased risk of the composite outcome.
Conclusions: Obese and underweight BMI were associated with increased risk of composite adverse outcome independent of other risk factors. Further research is necessary to determine whether BMI represents a modifiable risk factor for perioperative outcome.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Saturday, March 18, 2017, 1:15 p.m.-1:25 p.m.
- Session Title: Therapeutic Advances in Congenital Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1220M-09
IMPROVED EXERCISE PERFORMANCE IN PEDIATRIC FONTAN PATIENTS AFTER CARDIAC REHABILITATION
Samuel G. Wittekind, Wayne Mays, Yvette Gerdes, Sandra Knecht, John Hambrook, William Border and John Jefferies
vol. 69 no. 11 Supplement 575
DOI:
https://doi.org/10.1016/S0735-1097(17)33964-5
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Samuel G. Wittekind,
- Wayne Mays,
- Yvette Gerdes,
- Sandra Knecht,
- John Hambrook,
- William Border and
- John Jefferies
- Cincinnnati Children’s Hospital Medical Center, Cincinnati, OH, USA
Background: Patients with Fontan circulation have impaired exercise capacity. Cardiac rehabilitation (CR) has shown promise in improving peak exercise performance in this population, but its role in improving submaximal exercise performance has not been shown to date. We assessed the hypothesis that participation in CR will be associated with improved exercise performance in pediatric Fontans, and that this change will be mediated by increased efficiency in oxygen delivery and ventilation during submaximal effort.
Methods: In this prospective study, pediatric Fontans were recruited from cardiology clinic at Cincinnati Children’s Hospital Medical Center. Participants completed two 60 minute sessions per week for 12 weeks. Safety was assessed by counting adverse events during CR sessions. Anthropometrics and cardiopulmonary exercise test (CPET) parameters were measured at baseline and at last CR visit then compared with a paired sample t-test for statistical significance (p<0.05).
Results: Ten pediatric Fontans completed the study. The mean age was 12 (minimum 8, maximum 16) years at enrollment and 40% were male. Five had tricuspid atresia and 5 had hypoplastic left heart syndrome. No serious adverse events occurred during CR sessions. Total working capacity increased by a mean of 1497 kpm (95% CI, 947 to 2047; p<0.001), peak indexed oxygen consumption increased by a mean of 3.7 mL/kg/min (95% CI, 1.5 to 5.9; p=0.004), and peak oxygen pulse increased by a mean of 0.9 mL/beat (95% CI, 0.4 to 1.4; p=0.004). The mean respiratory exchange ratio did not change significantly. The significant difference in oxygen pulse became evident in stage 2 of submaximal exercise. The slope for the volume of expired ventilation to the volume of carbon dioxide production (VE/VCO2 slope) improved by a mean of 4.5 (95% CI, −0.6 to −8.4; p<0.03).
Conclusions: In conclusion, we demonstrated significant improvements in both submaximal and peak exercise performance in pediatric Fontans undergoing prescribed exercise therapy with no serious adverse events. These changes are mediated, at least in part, by more efficient oxygen delivery (lower HR and higher oxygen pulse) and ventilation (VE/VCO2 slope).
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Saturday, March 18, 2017, 1:30 p.m.-1:40 p.m.
- Session Title: Therapeutic Advances in Congenital Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1220M-11
MATERNAL BLOOD TRACE ELEMENT LEVELS AND RISKS FOR FETAL CONGENITAL HEART DEFECTS IN GUANGDONG, CHINA
Yanqiu Ou, Michael S. Bloom, Liu Xiaoqing and Lin Shao
vol. 69 no. 11 Supplement 576
DOI:
https://doi.org/10.1016/S0735-1097(17)33965-7
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- aGuangdong Cardiovascular Institute, Guangzhou, People’s Republic of China
- bGuangdong General Hospital, Guangdong Academy of Medical Sciences, Guangzhou, People’s Republic of China
Background: Exposure to toxic trace elements, including heavy metals, is an important public health concern. Few studies have assessed if individual and multiple trace elements simultaneously affect cardiac development. The current study evaluated the association between maternal blood lead (Pb), cadmium (Cd), chromium, copper, mercury, and selenium (Se) levels and congenital heart defects (CHDs) in offspring.
Methods: This hospital-based case-control study included 120 case and 108 control infants. A single maternal peripheral blood draw was made during gestational weeks 17-40 and used to determine trace element levels by inductively couple plasma mass spectrometry. Multivariable logistic regression was used to assess associations and interactions between individual and multiple trace elements and fetal CHDs, adjusted for confounding variables, including maternal age, parity, folic acid intake, cigarette smoking, living in a newly renovated home, maternal BMI, and gestational week at blood sample collection.
Results: In a model including all measured trace elements and adjusted for confounders, maternal Pb (OR=22.60, 95% CI: 5.26, 97.10) and Se (OR=0.26, 95% CI: 0.09, 0.78) were significant predictors of CHDs, and interactions were suggested for CHDs with Pb, Se, and Cd. Similar associations were detected for subgroups of CHDs, including septal and atrioventricular septal defects, conotruncal defects, and right ventricle outflow tract obstruction.
Conclusions: Higher maternal blood Pb and lower maternal blood Se were important dose-dependent predictors of CHDs, overall and for specific groups of lesions. There was suggestive interaction between studied elements. Our results suggest that even under the current standard, Pb exposure poses an important health threat. These data can be used for developing interventions and identifying high risk pregnancies for referral to fetal echocardiography and intensive prenatal monitoring.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Saturday, March 18, 2017, 3:45 p.m.-3:55 p.m.
- Session Title: Impact of Prenatal Environment on Congenital Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1259M-03
UMBILICAL ARTERIAL BLOOD FLOW IN THE THIRD TRIMESTER AND ITS ASSOCIATION WITH CLINICAL AND NEURODEVELOPMENTAL OUTCOMES IN CHILDREN WITH CRITICAL NEONATAL CONGENITAL HEART DISEASE
Jayani Abeysekera, Dora Gyenes, Charlene Robertson, Gwen Alton, Irina Dinu, Dianne Creighton, Joseph Atallah, Ivan Rebeyka and Lisa Hornberger
vol. 69 no. 11 Supplement 577
DOI:
https://doi.org/10.1016/S0735-1097(17)33966-9
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 30, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Jayani Abeysekera,
- Dora Gyenes,
- Charlene Robertson,
- Gwen Alton,
- Irina Dinu,
- Dianne Creighton,
- Joseph Atallah,
- Ivan Rebeyka and
- Lisa Hornberger
- University of Alberta, Edmonton, Canada
Background: Children with congenital heart disease are at increased risk of adverse long-term neurodevelopmental outcomes believed in part secondary to a prenatal insult. Altered fetal middle cerebral arterial (MCA) Dopplers suggestive of brain sparing (low Pulsatility Index, PI) as well as placental pathology have been documented in fetal heart disease. In this study, we investigated the relationship between MCA and umbilical arterial, UA, flow patterns in fetal transposition of the great arteries (TGA) and hypoplastic left heart syndrome (HLHS) on growth and 2-year neurodevelopmental outcomes.
Methods: We identified children with d-TGA and HLHS within the Western Canadian Complex Pediatric Therapies Follow-Up Program who had a 3rd trimester fetal echocardiogram between October 2004 and August 2014. Participants with inadequate fetal Doppler data or death prior to 2-year follow-up were excluded. MCA and UA PI measurements were obtained via offline analysis of 3rd trimester fetal echocardiograms. The relationship with birth and 2 year somatic measures, and 2 year Bayley Scales of Infant and Toddler Development III composite scores were analyzed using two-sided Pearson correlations (r).
Results: Children with d-TGA (n=24) and HLHS (n=36) were included. MCA PI did not correlate with birth somatic measures or 2-year neurodevelopmental outcomes. UA PI, however, inversely correlated birth and 2 year head circumference (r=-0.36, p=0.005 and r=-0.25, p=0.05), length (r=-0.27, p=0.039 and r=-0.40, p=0.001) and weight (r=-0.31, p=0.015 and r=-0.44, p=0.001), and 2-year cognitive (r=-0.30, p=0.019), language (r=-0.30, p=0. 022) and motor scores (r=-0.27, p=0.04).
Conclusions: A higher UA PI, suggestive of placental insufficiency, in fetal HLHS and d-TGA is associated with worse 2-year growth and neurodevelopmental outcomes. This could represent an additional insult that contributes to long-term outcomes in critical neonatal heart disease. Understanding these risk factors allows for early identification and intervention to ultimately improve outcomes and decrease disease burden.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Saturday, March 18, 2017, 4:00 p.m.-4:10 p.m.
- Session Title: Impact of Prenatal Environment on Congenital Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1259M-05
MATERNAL EXOSOMAL MIRNAS IN DIABETES CONTRIBUTE TO THE CARDIAC DEVELOPMENT DEFICIENCY
Ruijing Shi, Wenbin Cai, Xueying Zhou, Lianbi Zhao, Guodong Yang and Lijun Yuan
vol. 69 no. 11 Supplement 578
DOI:
https://doi.org/10.1016/S0735-1097(17)33967-0
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- aDepartment of Ultrasound Diagnostics, Tangdu Hospital, Fourth Military Medical University, Xi’an, People’s Republic of China
- bDepartment of Biochemistry and Molecular Biology, Fourth Military Medical University, Xi’an, People’s Republic of China
Background: Maternal diabetes mellitus induces an increased risk of congenital heart defects (CHD), however, the exact mechanisms are still not fully illustrated. Exosomes have been found to cross physiological barriers and are implicated in multiple pathophysiological functions, suggesting that exosomes might contribute to embryonic cardiac development deficiency if we can confirm their capacity to cross the placental barrier.
Methods: Diabetic pregnant C57BL/6 mice were induced by injection of streptozotocin (STZ) before mating. Circulating exosomes from the diabetic pregnant mice or the control mice were harvested before purification for further analysis and in vivo delivery. MiRNAs inside the exosomes were analyzed by RNA-seq. Exosomes or the analogue gold nanoparticles were fluorescently labeled before tail vein injection for in vivo distribution analysis. To explore the roles of diabetic maternal exosomes in cardiac development, the exosomes from diabetic pregnant mice were delivered into normal pregnant mice and cardiac development was analyzed by echocardiography or histology.
Results: Compared with the control normal mice, diabetic pregnant mice displayed significant changes of the exosome counts and contents in the blood, which correlate with the increased cardiac developmental defect. RNA-seq analysis revealed that multiple miRNAs changed more than 10 folds, and bioinformatics revealed their implication in regulating Wnt and other developmental pathways. Moreover, fluorescence labeled exosomes and gold nanoparticles could cross the placenta barrier and infiltrated into the embryonic organs/tissues, including the heart, especially during the early stages of embryonic development. Injection of diabetic maternal exosomes strikingly increased the risk of CHD in the normal recipient pregnant mice.
Conclusions: Maternal exosomal miRNAs in diabetes could cross the maternal-fetal barrier and the aberrant miRNAs in the exosomes may contribute to the cardiac development deficiency. Our study would provide new insights in CHD prevention and treatment.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Saturday, March 18, 2017, 4:15 p.m.-4:25 p.m.
- Session Title: Impact of Prenatal Environment on Congenital Heart Disease
- Abstract Category: 11. Congenital Heart Disease: Therapy
- Presentation Number: 1259M-07
RED CELL DISTRIBUTION WIDTH PREDICTS ADVERSE OUTCOMES IN ADULTS WITH CONGENITAL HEART DISEASE: RESULTS FROM THE BOSTON ADULT CONGENITAL HEART BIOBANK
Laith Alshawabkeh, Saurabh Rajpal, Michael Landzberg, Catherine Gray, Fred Wu, Georges Ephrem and Alexander Opotowsky
vol. 69 no. 11 Supplement 579
DOI:
https://doi.org/10.1016/S0735-1097(17)33968-2
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Laith Alshawabkeh,
- Saurabh Rajpal,
- Michael Landzberg,
- Catherine Gray,
- Fred Wu,
- Georges Ephrem and
- Alexander Opotowsky
- Boston Children’s and Brigham & Women’s Hospitals, Boston, MA, USA
Background: Red cell distribution width (RDW) is a strong predictor of adverse outcomes in diverse populations. We investigated the prognostic value of RDW as a marker of risk in adults with congenital heart disease (CHD).
Methods: To test our hypothesis that RDW is a predictor of death or non-elective cardiovascular hospitalization, we prospectively enrolled 702 adults with CHD between 2012 and 2016 to investigate the association between RDW and outcomes. Survival analysis was used to model the relationship between RDW and the outcomes of interest.
Results: Mean age was 38.7±13.5 years and 49.9% were female. Most patients had either moderately (42.5%) or severely complex (38.8%) CHD. Median RDW was 13.7% [interquartile range 13.3 – 14.3%, RDW>15% in 84/702]. Median follow up for the combined outcome in 530 patients with longitudinal data was 364 days; there were 18 deaths and 60 non-elective cardiovascular hospitalizations; higher RDW was associated with an increased hazard for the combined outcome (HR per +1SD RDW=1.6, 95%CI 1.4 – 1.8, p<0.0001) and for mortality alone (HR=2.0, 95%CI 1.6 – 2.5, p<0.0001) (Figure). RDW was an independent predictor of the combined outcome after adjusting for age, sex, CHD complexity, hemoglobin, cyanosis, and estimated glomerular filtration rate (HR=1.4, 95%CI 1.2-1.7, p<0.0001).
Conclusions: Elevated RDW is an independent predictor of death or non-elective cardiovascular hospitalizations in adults with CHD.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Sunday, March 19, 2017, 9:45 a.m.-9:55 a.m.
- Session Title: Things That Matter in Adult Congenital Heart Disease
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1302M-03
GENDER DIFFERENCES IN RATES OF HOSPITALIZATIONS FOR DECOMPENSATED HEART FAILURE AMONG ADULTS WITH CONGENITAL HEART DISEASES IN THE UNITED STATES: A 15 YEAR EXPERIENCE
Ghanshyam Palamaner Subash Shantha, Anita Kumar, Kongkiat Chaikriangkrai, Chakradhari Inampudi, Gardar Sigurdsson and Michael Giudici
vol. 69 no. 11 Supplement 580
DOI:
https://doi.org/10.1016/S0735-1097(17)33969-4
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Ghanshyam Palamaner Subash Shantha,
- Anita Kumar,
- Kongkiat Chaikriangkrai,
- Chakradhari Inampudi,
- Gardar Sigurdsson and
- Michael Giudici
- University of Iowa Hospitals and Clinics, Iowa City, IA, USA
Background: There is scant data with regards to the gender differences in the rates of hospitalizations for decompensated heart failure (DHF) among adult patients with congenital heart diseases (CHD) in the United States. In this retrospective cohort study we assessed gender differences in hospitalization rates for DHF among adult patients with CHD in the United States and further assessed the temporal trends in the last 15 years.
Methods: National Inpatient Sample (NIS), a publically available dataset, reports data on 8 million hospitalizations from about 1000 hospitals from 46 states. From this, we abstracted data on 192,444 consecutive patients with CHD hospitalized from 1998 – 2012 (study cohort). From this study cohort, we further abstracted data on the rates of hospitalizations for DHF and assessed gender differences in hospitalization rates over 3 periods: 1998 – 2002, 2003 – 2007 and 2008 – 2012.
Results: Of the 192,444 study cohort participants, 101,367 (53%) were women (W) and 91,077 (47%) were men (M). Men were significantly older compared to women (M: 47 years, W: 44 years, P = 0.033). Hospitalization rates for DHF were significantly higher in women than men (W: 76% vs M: 62%) (P < 0.001) in the total cohort. Temporal trends over the 15 year period (1998 – 2012) consistently showed higher hospitalization rates for DHF in women compared to men [(1998 – 2002: W – 71%, M – 66%), (2003 – 2007: W – 77%, M – 61%), (2008 – 2012: W – 78%, M – 62%)]. Multi-variate logistic regression analysis [(adjusted for age, diabetes diagnosis (DM), hypertension diagnosis (HTN), previous stroke] showed significantly increased odds of hospitalizations (Odds Ratios ranging from 1.22-1.27) for DHF in women compared to men in the CHD cohort over all the 3 time periods.
Conclusions: Our analysis suggests that women with CHD have consistently had an increased probability of hospitalization for DHF compared to men for the last 15 years in the United States. Our findings are in contrary to the available literature that supports a better prognosis among women with heart failure compared to their male counterparts among heart failure patients without CHD. The reason behind this discrepancy is not known and deserves further investigation.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Sunday, March 19, 2017, 10:00 a.m.-10:10 a.m.
- Session Title: Things That Matter in Adult Congenital Heart Disease
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1302M-05
OUTCOMES OF CARDIAC PACING IN THE ADULT FONTAN POPULATION
Geoffrey Huntley, Heidi Connolly, Sameh M. Said, Carole Warnes, Christopher McLeod and Alexander C. Egbe
vol. 69 no. 11 Supplement 581
DOI:
https://doi.org/10.1016/S0735-1097(17)33970-0
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Geoffrey Huntley,
- Heidi Connolly,
- Sameh M. Said,
- Carole Warnes,
- Christopher McLeod and
- Alexander C. Egbe
- Mayo Clinic, Rochester, MN, USA
Background: Cardiac pacing can be challenging after a Fontan operation, and there are limited data about pacing in adults with Fontan palliation.
Methods: A retrospective review of adult Fontan patients followed at Mayo Clinic between 1994 and 2014 was conducted in order to determine the risk factors for pacing and occurrence of device-related complications (DRC) and pacemaker reinterventions. DRC was defined as lead failure, lead recall, lead thrombus/vegetation, or device related infection. Cardiovascular adverse event (CAE) was defined as venous thrombosis, stroke, death, or heart transplant.
Results: Out of 439 adult Fontan patients, 166 (38%) required pacing (79 and 87 had pacemaker implantation in childhood and adulthood, respectively). At initial implantation, 114 patients (69%) received epicardial leads, and 52 patients (31%) received endocardial leads. Initial pacing mode was atrial (n=52, 31%), ventricular (n=30, 18%), and dual chamber (n=84, 51%). Risk factors for pacing included atrial arrhythmia (hazard ratio [HR] 2.21, 95% confidence interval [CI] 1.33-5.11, P=0.04) and reoperation (HR 1.98, CI 1.16-6.12, P=0.02). There were 129 reinterventions (lead failure 39, lead recall 6, generator change 62, defibrillator upgrade 4, cardiac surgery 18). Excluding generator changes, the reintervention rate was 3.3% per year. There were 48 DRCs (lead failure 31, lead recall 6, lead thrombus/vegetation 5, and infection 6), yielding a DRC rate of 2.4% per year. Pacemaker implantation in childhood was a risk factor for DRC (HR 2.01, CI 1.22-5.63, P=0.03). There were 70 CAE (venous thrombosis 5, stroke 11, transplant 8, and death 46), yielding a rate of 3.5% per year. DRC, CAE, and reintervention rates were comparable between epicardial and endocardial leads.
Conclusions: More than one-third of adult Fontan patients referred to the Mayo Clinic required pacing. Atrial arrhythmias and reoperations were risk factors for pacemaker implantation. Outcomes of epicardial and endocardial leads were comparable.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Sunday, March 19, 2017, 10:15 a.m.-10:25 a.m.
- Session Title: Things That Matter in Adult Congenital Heart Disease
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1302M-07
TIMELY DETECTION OF PULMONARY ARTERIAL HYPERTENSION IN PATIENTS WITH REPAIRED CONGENITAL HEART DISEASE: INTERIM RESULTS FROM THE ACHD-QUERI REGISTRY
Michael Landzberg, Curtis Daniels, Paul Forfia, Anatoly Langer, Vallerie McLaughlin, Mona Selej, Marjan Sepassi, Mary Tan and Gary Webb
vol. 69 no. 11 Supplement 582
DOI:
https://doi.org/10.1016/S0735-1097(17)33971-2
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Michael Landzberg,
- Curtis Daniels,
- Paul Forfia,
- Anatoly Langer,
- Vallerie McLaughlin,
- Mona Selej,
- Marjan Sepassi,
- Mary Tan and
- Gary Webb
- Canadian Heart Research Centre, Toronto, Canada
Background: Patients (pts) with repaired congenital heart disease (rCHD) remain at risk of developing PAH, which is diagnosed per established guidelines by right heart catheterization (RHC). ACHD-QuERI, a US-based, observational, multicenter, longitudinal screening registry (clinicaltrials.gov NCT01659411) developed to facilitate timely detection of PAH in adults with rCHD, is the first registry to prospectively follow high-risk rACHD pts. Baseline (BL) and 1-year (y) interim results are reported.
Methods: Pts aged ≥18 y with rCHD ≥1 y from enrollment, history of a large defect prior to closure and at high risk for PAH by ECHO measures were eligible. Physical exam, ECG, ECHO, WHO functional class (FC), 6 minute walk distance (6MWD), and SpO2 are prospectively collected to evaluate progression to PAH. Pop-up reminders of pt-specific evidence-based (clinical, ECG, ECHO) recommendations for PAH detection appeared to clinicians onscreen at data entry.
Results: Overall, 221 pts were eligible for analysis; mean (SD) age was 43.9 (15.9) y and 72.0% were women. At BL (n=219), 82.2% of pts were classified FC I and at 1 y 88.6% (n=140) remained in FC I. At BL, 49.8%, 28.8%, 24.7%, and 23.7% had arrhythmia (palpitations, atrial fibrillation or flutter), exertional dyspnea, were current/former smokers, and had hypertension, respectively. SpO2 (98±4%) did not change between BL (n=203) and 1 y (n=140). Pts who underwent a 6MWD test at BL (48/219) and 1 y (18/139) walked a mean (SD) 434 (109) m and 479 (115) m, respectively. Per pop-up recommendation, ECHO (per ECG high-risk PAH findings) was performed for majority of pts at BL (74.1%, 20/27) but not at 1 y (25.0%, 2/8). RHC (per ECHO high-risk PAH findings) was recommended for 83/216 (38.4%) pts at BL and 44/104 (42.3%) at 1 y; however, at BL and at 1 y, RHC was performed for 7/83 (8.4%) and 1/44 (2.3%), respectively. Primary reason for a clinician not performing nor planning to perform ECHO or RHC was belief that their management was appropriate.
Conclusions: In ACHD-QuERI, data up to 1 y suggest RHC is underutilized in rCHD pts who are at high-risk for PAH (per ECHO). Through reminders, ACHD-QuERI aims to improve PAH screening among ACHD patients at risk for PAH. 3-y follow-up is ongoing.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Sunday, March 19, 2017, 12:30 p.m.-12:40 p.m.
- Session Title: Finding Out What Works in Pediatric and Congenital Heart Disease
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1312M-03
MORPHOLOGICAL APPEARANCE AND REPAIR STRATEGIES OF TRICUSPID REGURGITATION IN PATIENTS WITH UNIVENTRICULAR HEART AND A SYSTEMIC RIGHT VENTRICLE
Masamichi Ono, Melchior Burri, Julie Cleuziou, Jelena Pabst von Ohain, Elisabeth Beran, Martina Strbad, Alfred Hager, Christian Schreiber and Rüdiger Lange
vol. 69 no. 11 Supplement 583
DOI:
https://doi.org/10.1016/S0735-1097(17)33972-4
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Masamichi Ono,
- Melchior Burri,
- Julie Cleuziou,
- Jelena Pabst von Ohain,
- Elisabeth Beran,
- Martina Strbad,
- Alfred Hager,
- Christian Schreiber and
- Rüdiger Lange
- German Heart Center Munich, Munich, Germany
Background: Tricuspid regurgitation (TR) remains a risk for staged palliation in patients with a systemic right ventricle. This study was performed to determine the morphology of the tricuspid valve (TV) in these patients leading to TR and to describe surgical management.
Methods: Among 460 patients who underwent a total cavopulmonary connection between 1994 and 2015, 155 patients with a systemic right ventricle had a TV as a single atrioventricular valve. Diagnoses included HLHS in 105 patients, mitral atresia (MA) and DORV in 17, MA and TGA in 6 and single TV with a single ventricle in 27. In patients who required TV surgery, timing of surgery, pathophysiology of TR, and outcomes were evaluated.
Results: Forty patients (26%) needed TV surgery. Timing of initial TV surgery was before or at stage II in 11 patients (28%), between stage II and III in 3 (7%) and at stage III in 26 (65%). TR was due to one or more of the following pathologies: dysplastic leaflet in 26 patients (65%), leaflet prolapse in 20 (50%), restrictive leaflet in 12 (30%), chordal anomaly in 8 (20%), and cleft in 7 (18%). For leaflet prolapse and dysplasia, the anterior leaflet was most commonly affected (62%). Regurgitation was most commonly detected at the anteroseptal (AS) commissure in 22 patients (55%). TV repair was performed in 36 patients (90%) using leaflet reconstruction in 26 (65%), commissuroplasty in 24 (60%), complete/partial annuloplasty in 17 (43%), and cleft closure in 7 (18%). TV replacement with a mechanical valve was required in 4 patients (10%). A second TV surgery was necessary in 12 patients (30%) and a third in 3 (8%). Freedom from reoperation on the TV was 65.5% at 5 years. Finally, 5 of 36 patients (14%) who had undergone initial TV repair needed TV replacement at the second (4) or the third (1) TV surgery, while 31 patients (86%) kept their own TV.
Conclusions: TR is a common problem in patients with univentricular heart and a systemic right ventricle. Most often it is the result of dysplastic, prolapsing or restrictive leaflets and emanates from the AS commissure. Surgical repair is challenging and may require more than one attempt. Severe regurgitation may require earlier intervention but is most commonly performed at stage III.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Sunday, March 19, 2017, 12:45 p.m.-12:55 p.m.
- Session Title: Finding Out What Works in Pediatric and Congenital Heart Disease
- Abstract Category: 11. Congenital Heart Disease: Therapy
- Presentation Number: 1312M-05
REDUCTION IN INTERSTAGE GROWTH FAILURE IN INFANTS WITH HYPOPLASTIC LEFT HEART SYNDROME AND IMPACT ON STAGE 2 OUTCOMES: A REPORT FROM THE NATIONAL PEDIATRIC CARDIOLOGY QUALITY IMPROVEMENT COLLABORATIVE
Jeffrey B. Anderson, David Brown, Megan Horsley, Katherine Bates, Samuel Hanke, Stacey Lihn, James Tweddell and Carole Lannon
vol. 69 no. 11 Supplement 584
DOI:
https://doi.org/10.1016/S0735-1097(17)33973-6
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Jeffrey B. Anderson,
- David Brown,
- Megan Horsley,
- Katherine Bates,
- Samuel Hanke,
- Stacey Lihn,
- James Tweddell and
- Carole Lannon
- Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA
Background: Growth failure (GF) is common in infants with hypoplastic left heart syndrome (HLHS) and is associated with poor short term outcomes. We sought to demonstrate changes in growth failure in infants cared for at National Pediatric Quality Improvement Collaborative (NPC-QIC) sites and to demonstrate the effect of interstage GF on outcomes at stage 2 palliation.
Methods: Retrospective analysis of NPC-QIC registry data from patients at 60 different clinical sites enrolled between 2009-16. Primary outcome was interstage growth failure (GF), defined as change in weight-for-age z-score of ≤ −0.5 between stage 1 (s1P) discharge and stage 2 palliation (s2P). Statistical process control was used to assess changes in collaborative GF. Secondary outcome was length of stay following s2P. Patient and center-related factors were assessed for association with GF and longer post-operative s2P hospitalization. Appropriate classical statistical methods were used in univariable and multivariable analyses.
Results: There were 1,869 infants enrolled in the NPC-QIC registry in this period; 63% male with 92.5% surviving to s2P. Statistical process control demonstrated significant reduction in infants experiencing GF from 18% to 10%. In multivariable modeling infants who experienced interstage GF had a longer median s2P length of stay (10 days; IQR 2-80) compared to those not experiencing GF (8 days; IQR 2-187), p=0.001. Other factors independently associated with longer s2P length of stay included longer s1P length of stay (p<0.001), moderate or greater tricuspid regurgitation at s1P discharge (p<0.001) and clinical site (p<0.001). Several independent factors associated with GF were identified: concomitant presence of a non-cardiac anomaly (p=0.002), moderate or greater tricuspid regurgitation at s1P discharge (p<0.04), and longer interstage (p=0.03).
Conclusions and Implications: Through this collaborative effort, GF has improved in infants with HLHS. Infants experiencing interstage GF have longer post-operative stays following s2P. GF is more common in infants with non-cardiac anomalies, moderate or greater tricuspid regurgitation as well as those with longer interstage periods.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Sunday, March 19, 2017, 1:00 p.m.-1:10 p.m.
- Session Title: Finding Out What Works in Pediatric and Congenital Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1312M-07
RISK OF CATASTROPHIC OUTCOME FOLLOWING CARDIAC CATHETERIZATION FOR PULMONARY HYPERTENSION: AN ANALYSIS OF DATA FROM THE IMPACT REGISTRY
Michael L. O’Bvrne, Kevin Kennedy, Joshua Kanter, John Berger and Andrew Glatz
vol. 69 no. 11 Supplement 585
DOI:
https://doi.org/10.1016/S0735-1097(17)33974-8
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- aChildren’s National Medical Center, Washington, DC, USA
- bThe Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Background: Cardiac catheterization is the gold standard test for hemodynamic assessment of patients with pulmonary hypertension (PH). The risk of this procedure in children with PH is uncertain. PH registries report mortality risks of 0-0.06%, while an estimate of the risk of catastrophic adverse events <1 day from catheterization using administrative data from a broader range of pediatric hospitals was 3.5%. We sought to utilize a national clinical registry to measure the risk of catastrophic adverse outcome and identify risk factors for those events.
Methods: A multicenter retrospective cohort study was performed using data from the IMPACT® registry of subjects up to 21 years with PH undergoing catheterization from 1/2011 to 12/2015. Subjects were identified using a combination of diagnostic codes and hemodynamic parameters. Using multivariable logistic regression, the association between pre-specified covariates and the risk of a composite outcome (death within 1 day of catheterization, cardiac arrest, or initiation of mechanical circulatory support following cardiac catheterization) was assessed.
Results: 9,010 procedures performed in 6,669 subjects with PH at 74 centers were studied. Median age was 3 years (IQR: 0-11). The etiology of PH was primary pulmonary hypertension in 23%, congenital heart disease 53%, status post heart transplantation 16%, cardiomyopathy 6%, and pulmonary vein stenosis 6%. Median pulmonary vascular resistance was 4.1 WU m2 (IQR: 2.6-6.5). 2% had undergone a cardiac operation in the prior 30 days, 14% received mechanical ventilation, and 13% received inotropes. In terms of procedural risk, 49% of procedures were in the lowest risk IMPACT® risk category. The observed risk of composite outcome was 1.2%, and death before discharge was 4.7%. Younger age, lower systemic arterial oxygen saturation, and receipt of inotropic agents were associated with increased risk of adverse outcome.
Conclusions: The risk of catastrophic adverse outcome following cardiac catheterization in PH patients in IMPACT®was significantly higher than that reported from PH-specific registries. Further research is necessary to determine to degree to which this risk is modifiable.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Sunday, March 19, 2017, 1:15 p.m.-1:25 p.m.
- Session Title: Finding Out What Works in Pediatric and Congenital Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1312M-09
PREVALENCE AND RISK FACTORS ASSOCIATED WITH CHRONIC KIDNEY DISEASE IN PATIENTS WITH SINGLE VENTRICLE CONGENITAL HEART DISEASE AFTER FONTAN PALLIATION
Sheetal Patel, David Kwiatkowski, Adin-Cristian Andrei, Ankita Devareddy, Catherine Krawczeski, Barbara J. Deal, Craig Langman and Bradley Marino
vol. 69 no. 11 Supplement 586
DOI:
https://doi.org/10.1016/S0735-1097(17)33975-X
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Sheetal Patela,b,
- David Kwiatkowskia,b,
- Adin-Cristian Andreia,b,
- Ankita Devareddya,b,
- Catherine Krawczeskia,b,
- Barbara J. Deala,b,
- Craig Langmana,b and
- Bradley Marinoa,b
- aAnn & Robert H. Lurie Children’s Hospital of Chicago, Chicago, IL, USA
- bLucile Packard Children’s Hospital, Palo Alto, CA, USA
Background: Single ventricle congenital heart disease patients s/p Fontan operation are at risk for chronic kidney disease (CKD). We sought to estimate the prevalence of and risk factors for CKD in Fontan survivors.
Methods: This was a two-center cross sectional study of Fontan survivors between 01/08 and 07/16. The primary outcome was presence of CKD defined by estimated Glomerular Filtration Rate (eGFR) of <90ml/min/1.73m2 derived using serum creatinine based age appropriate eGFR equations. Group comparisons used Chi-square and t-tests. Multivariable models to predict eGFR were created using stepwise variable selection and aggregation across bootstrap samples.
Results: 404 Fontan survivors were included: male 61%; age 13.3 yrs (2.3 – 49.9); time from Fontan 10 yrs (0.02- 36.8); dominant ventricle 44% left; Fontan type [71% external conduit (EC), 14% lateral tunnel (LT), 15% atrio-pulmonary; 8% of EC and 68% of LT had fenestration]. CKD was present in 44% (176/404) of patients (pts). Older age correlated with lower eGFR in both pediatric (n=280, r=-0.23; p<0.001) and adult (n=124, r=-0.35; p<0.001) pts. Patients with CKD had higher single ventricular end diastolic pressure (7±3 vs. 6+2 mmHg; p=0.007), higher SVC mean pressure (11+3 vs. 9+3 mmHg; p=0.002), lower SVC oxygen saturation (70±8 vs. 72+6; p=0.05) and higher indexed pulmonary vascular resistance (1.5+0.7 vs. 1.3+0.5 Woods units; p=0.048) at time of pre-Fontan cath. Pts with CKD were more likely to have EC Fontan (p=0.005), less likely to have fenestration (p=0.012), more likely to have ascites (p=0.014) and require Sildenafil therapy (p=0.041). Multivariate regression revealed that lower eGFR is associated with older age (-1.2 per yr; p<0.001) and sildenafil use (-9; p=0.004) in pediatric pts; and with longer duration since Fontan (-1.9 per yr; p<0.001) and EC Fontan type (-11.3; p<0.001) in adult pts.
Conclusions: By 10 yrs after the Fontan; almost half of the survivors develop CKD. Increasing age is associated with progressively lower eGFR. Worse pre-Fontan hemodynamic factors, Fontan type and absence of fenestration are associated with the development of CKD. Our data suggest a need for more intense screening for CKD in Fontan survivors.
Footnotes
- Moderated Poster Contributions
- Congenital Heart Disease and Pulmonary Hypertension Moderated Poster Theater, Poster Hall, Hall C
- Sunday, March 19, 2017, 1:30 p.m.-1:40 p.m.
- Session Title: Finding Out What Works in Pediatric and Congenital Heart Disease
- Abstract Category: 11. Congenital Heart Disease: Therapy
- Presentation Number: 1312M-11
LONG-TERM TRANSPLANT-FREE SURVIVAL FOLLOWING SURGERY FOR COARCTATION OF THE AORTA: A STUDY FROM THE PEDIATRIC CARDIAC CARE CONSORTIUM
Matthew Oster, Courtney McCracken, Melinda Cory, John Hunting and Lazaros Kochilas
vol. 69 no. 11 Supplement 587
DOI:
https://doi.org/10.1016/S0735-1097(17)33976-1
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- aEmory University, Atlanta, GA, USA
- bChildren’s Healthcare of Atlanta, Atlanta, GA, USA
Background: The objective of this study was to determine the transplant-free survival of infants with coarctation of the aorta (CoA), the most common critical congenital heart defect.
Methods: We performed a retrospective cohort study of infants (<1 year of age) undergoing surgical intervention for CoA between 1982 and 2003 at 48 centers in 27 US states in the Pediatric Cardiac Care Consortium. Outcomes were determined from the National Death Index and the United Network for Organ Sharing through 2014. Children with associated cardiac lesions other than left-sided lesions, ventricular septal defect (VSD), patent ductus arteriosus, and atrial septal defect were excluded. We used parametric survival methods and Cox proportional hazard models to analyze outcomes.
Results: Of 2030 eligible patients with a median follow-up of 17.5 years, there were 119 deaths prior to transplant and 1 transplant, yielding an overall transplant-free survival of 94.1%. (Figure) Compared to those with simple CoA, hazard of mortality/transplant was 1.8 times higher in patients with a VSD (95% CI 1.18 – 2.82; p = 0.007) and 3.5 times higher in patients with a syndrome (95% CI 2.08 – 5.95; p < 0.001). There was no difference in transplant-free survival in patients with additional left-sided lesions vs. those with simple CoA (HR = 1.13; 95% CI 0.65 – 1.96; p = 0.67).
Conclusions: Transplant-free survival for CoA is excellent, particularly for those without a VSD or a known syndrome. Studies are underway to compare outcomes based on type of repair.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 10:00 a.m.-10:45 a.m.
- Session Title: Congenital Heart Disease: Progress in Pediatric Heart Surgery
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1101-009
THE AORTIC PERFUSION SCORE: A NOVEL SCORING SYSTEM TO PREDICT DEATH OR TRANSPLANT IN CHILDREN WITH PULMONARY ATRESIA WITH INTACT VENTRICULAR SEPTUM
Rohit Seth Loomba and Andrew Pelech
vol. 69 no. 11 Supplement 588
DOI:
https://doi.org/10.1016/S0735-1097(17)33977-3
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Rohit Seth Loomba and
- Andrew Pelech
- Children’s Hospital of Wisconsin, Milwaukee, WI, USA
Background: Pulmonary atresia with intact ventricular septum (PAIVS) is a unique congenital malformation of the heart in which patients may undergo single-, two-, or 1 ½- ventricle repair. Size of the tricuspid valve annulus, morphology of the right ventricle, and presence of ventriculo-coronary connections (VCCs) can all impact the selection of appropriate palliative strategy. We developed the aortic perfusion score (APS), a novel scoring system based on anterograde coronary perfusion with the aim of being able to identify patients at risk for death or transplant.
Methods: A retrospective study of patients at our institution was conducted. Patients were included if an initial catheterization was done prior to any intervention. Each patient was assigned an APS. In this system, each of the named coronaries (left anterior descending, left circumflex, right main, and posterior descending) had a maximum of 100 points they could be assigned. If the entire length of the coronary was being supplied via the aortic root then the coronary would receive 100 points, if only a percentage of it were receiving supply from the aortic root then it would receive that many points. If there was to-fro flow in the coronary due to VCCs then the coronary artery’s score was halved. These were then summated for a maximum score of 400. ROC analysis was done to determine a cutoff point predictive of a composite endpoint of death or transplant. A univariate logistic regression was conducted with the endpoint as the dependent variable and the APS as the independent variable.
Results: A total of 64 patients were included in the analysis with 10 reaching the endpoint of death or transplant. At most recent follow-up 31% of patients had undergone single ventricle, 13% 1 ½ ventricle repair, 30 two-ventricle, 17% shunt, and 9% transplant palliation. An APS of 227.5 predicted the endpoint with a sensitivity of 90% and a specificity of 83%.
Conclusions: The APS is a scoring method which can be used to predict a composite endpoint of death or transplant in patients with PAIVS and may be helpful in selecting patients that should be listed for transplant. Additional multicenter studies may help further refine the scoring system.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 10:00 a.m.-10:45 a.m.
- Session Title: Congenital Heart Disease: Progress in Pediatric Heart Surgery
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1101-010
CONGENITAL HEART SURGERY IN PATIENTS WITH TRISOMY 13 ASSOCIATED WITH LOWER IN-HOSPITAL MORTALITY
Katherine Kosiv, Jeffrey Gossett, Shasha Bai and Ronnie Collins
vol. 69 no. 11 Supplement 589
DOI:
https://doi.org/10.1016/S0735-1097(17)33978-5
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- aUniversity of Arkansas for the Medical Sciences, Little Rock, AR, USA
- bArkansas Children’s Hospital, Little Rock, AR, USA
Background: Congenital heart disease (CHD) occurs in about 80% of patients with Trisomy 13 (T13), but surgical repair has not been offered to these patients in most centers because of low median survival. Data on congenital heart surgery (CHS) for T13 are lacking.
Methods: Nationally distributed data from 44 pediatric hospitals in the 2004 to 2015 Pediatric Health Information System (PHIS) database were used to identify patients with hospital admissions with an International Classification of Diseases-9th Revision code for T13 and CHD. Data were restricted to newborns admitted < 14 days of age. In-hospital mortality, length of stay (LOS) and adjusted total costs were compared between infants undergoing CHS and those treated medically.
Results: Of 644 infants with T13 identified, 471 had CHD (73%). Median age at admission was <1 day (IQR: 0, 1). CHS was performed in 39/471 (8% with CHD). Median LOS for the CHS group was 30 days (19, 68) versus 8 days (4, 19) in the non-surgical group (p<0.001). Mortality was 49% lower in the CHS group (28% versus 55%, p<0.001). Median hospital cost was 302% higher in the CHS group ($133,858 versus $33,299, p<0.001).
Conclusions: In-hospital mortality occurs in greater than half of neonates with T13 by less than one week of age. CHS in these patients is associated with decreased in-hospital mortality. Hospital costs are significantly increased in those who underwent CHS largely due to increased hospital LOS.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 10:00 a.m.-10:45 a.m.
- Session Title: Congenital Heart Disease: Progress in Pediatric Heart Surgery
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1101-011
EARLY HYDRODYNAMIC ASSESSMENT OF INTESTINAL SUB-MUCOSA BIOSCAFFOLD FOR MITRAL VALVE REPLACEMENT
Omkar Mankame, Lilliam Valdes-Cruz, Steven Bibevski, Frank Scholl, Ivan Baez and Sharan Ramaswamy
vol. 69 no. 11 Supplement 590
DOI:
https://doi.org/10.1016/S0735-1097(17)33979-7
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Omkar Mankamea,b,
- Lilliam Valdes-Cruza,b,
- Steven Bibevskia,b,
- Frank Scholla,b,
- Ivan Baeza,b and
- Sharan Ramaswamya,b
- aFlorida International University, Miami, FL, USA
- bJoe DiMaggio Children’s Hospital, Hollywood, FL, USA
Background: Infants and children with severe valve lesions have limited surgical options. It has been shown that acellular porcine small intestinal submucosa (PSIS) scaffolds support cell infiltration and tissue remodeling after implantation. Our group has implanted custom-made PSIS valves in 4 infants with critical valve disease unable to receive standard valves. Short term follow-up is promising. The purpose of this study was to conduct early assessment on acute in vitro functionality and hydrodynamics of custom PSIS mitral valves compared to commercially available trileaflet porcine bioprosthetic valves (BPV).
Methods: Bi-leafet PSIS (Diameter = 19 mm; n = 2) and tri-leaflet bioprosthetic (Diameter = 21mm; n = 3; BPV) control valves were tested in a pulse duplicator system (Vivitro Laboratories, Victoria, Canada) fitted with flow and pressure transducers. PSIS material (Cormatrix, Roswell, GA) was manually assembled into bi-leaflet valves and sutured into Dacron conduits. Holders tailored for each valve were 3-D printed. The valves-in-holders were press-fitted into the mitral location within the pulse duplicator. A 0.9% saline solution was introduced through the atrium chamber to fill the loop. A flow waveform representating the left ventricular outflow tract was selected. Heart rate = 70 beats/min stroke volume = 80 ml/beat. Ten cycles were recorded and averaged for each valve. Hydrodynamic metrics were subsequently computed. The testing protocol was repeated for BPVs.
Results: Mean diastolic Del_P (mmHg): BPV = 7.34 ± 0.41; PSIS = 8.11 ± 0.59 (NS). Qrms (ml/s): BPV = 230.8 ± 2.16; PSIS = 223.4 ±
4.21 (NS). EOA (cm2): BPV = 1.65 ± 0.04; PSIS = 1.51 ± 0.09 (NS), systolic %RF: BPV = 3.0 ± 0.5; PSIS = 3.7 ± 1.7 (NS) and closing energy loss: BPV = 31.8 ± 3.9; PSIS = 53.4 ± 23.4 (NS).
Conclusions: Mitral PSIS bi-leaflet valves were found to have similar hydrodynamics to a commercially-available BPV (Edwards Lifesciences, Irvine, CA; p > 0.05 in all metrics). A larger sample size is needed to confirm robust functionality of PSIS valves observed here. Subsequent assessment of PSIS bi-leaflet valve growth if successful, may lead to a potential breakthrough in treatment of critical congenital mitral valve disease.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 10:00 a.m.-10:45 a.m.
- Session Title: Congenital Heart Disease: Progress in Pediatric Heart Surgery
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1101-012
A RED CELL PRESERVATION STRATEGY REDUCES POSTOPERATIVE TRANSFUSIONS IN PEDIATRIC HEART SURGERY PATIENTS
Meena Nathan, Brielle Tishler, Kimberlee Gauvreau, Gregory S. Matte, Robert J. Howe, Linda Durham, Sharon Boyle, Derek Mathieu, Francis Fynn-Thompson, James Dinardo and Juan Ibla
vol. 69 no. 11 Supplement 591
DOI:
https://doi.org/10.1016/S0735-1097(17)33980-3
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Meena Nathana,b,
- Brielle Tishlera,b,
- Kimberlee Gauvreaua,b,
- Gregory S. Mattea,b,
- Robert J. Howea,b,
- Linda Durhama,b,
- Sharon Boylea,b,
- Derek Mathieua,b,
- Francis Fynn-Thompsona,b,
- James Dinardoa,b and
- Juan Iblaa,b
- aBoston Children’s Hospital, Boston, MA, USA
- bHarvard Medical School, Boston, MA, USA
Background: As part of a blood conservation initiative at our center, we began routine use of cell saver (CS) for all congenital heart surgery (CHS) performed on cardiopulmonary bypass (CPB) in 2014. The aim of this study is to compare transfusion rates prior to (preCS) and in the first (CS1) and second (CS2) year after this initiative.
Methods: Consecutive patients < 18 years undergoing CHS on CPB were included as 3 one year cohorts defined above. We excluded patients who required VAD/ECMO or second surgical operation on CPB at index admission. Baseline characteristics, use of blood intraoperatively and postoperatively, and postoperative albumin use were compared between groups using nonparametric methods.
Results: The three groups had similar baseline characteristics. Blood use was significantly higher in preCS group as compared to the other two groups both intra and postoperatively. The rate of albumin use decreased significantly with time. There was a trend towards decreased blood bank charges.
Conclusions: Cell saver implementation significantly decreased perioperative blood and albumin use. The ongoing improvement over time indicates the learning curve associated with any dramatic change in practice.
Clinical Implication: Reduction in blood and albumin use reduces development of reactive antibodies and other transfusion related complications. Future quality initiatives will be directed towards further reduction in blood and albumin use by development of transfusion threshold.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 10:00 a.m.-10:45 a.m.
- Session Title: Congenital Heart Disease: Progress in Pediatric Heart Surgery
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1101-013
VALIDATION OF TECHNICAL PERFORMANCE SCORE FOR LONG-TERM OUTCOMES IN CONGENITAL HEART SURGERY: 10 YEAR FOLLOW-UP DATA
Meena Nathan, Steven Colan, Jane Newburger, Hua Liu, Kimberlee Gauvreau, Brielle Tishler and Pedro del Nido
vol. 69 no. 11 Supplement 592
DOI:
https://doi.org/10.1016/S0735-1097(17)33981-5
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Meena Nathana,b,
- Steven Colana,b,
- Jane Newburgera,b,
- Hua Liua,b,
- Kimberlee Gauvreaua,b,
- Brielle Tishlera,b and
- Pedro del Nidoa,b
- aBoston Children’s Hospital, Boston, MA, USA
- bHarvard Medical School, Boston, MA, USA
Background: Technical Performance Score (TPS), an echocardiographic/clinical based tool that measures residua after congenital cardiac surgery, has been associated with in hospital and midterm outcomes. We sought to validate the ability of TPS to predict long-term outcomes.
Methods: We followed consecutive patients from 06/2005 to 06/2006 who had congenital heart surgery on cardiopulmonary bypass and survived to discharge for 10 years. TPS was assigned as Class 1 (no residua), Class 2 (minor residua), Class 3 (major residua or predischarge reintervention for major residua). Transplant-free survival and post discharge reinterventions were analyzed using Cox regression.
Results: Of 676 subjects, 357 (53%) were male, and median age at surgery 1.1 (IQR 0.2, 5.7) years. There were 163 (24%) post discharge reinterventions and 41 (6.1%) deaths/transplants. On multivariable modeling, Class 2 (HR 1.6, CI 1.1, 2.3; p=0.02), and Class 3 TPS (HR 2.8, CI 1.8, 4,4; p<0.001) had shorter time to reintervention. Class 3 TPS also had a greater hazard of death/transplant (HR 4.2, CI 1.9, 8.9; p<0.001). Transplant-free survival and freedom from reintervention are represented in figure.
Conclusions: Ten years after congenital heart surgery, presence of minor or major residua is associated with post discharge reintervention; and presence of major residua with mortality. The TPS enables identification of patients at risk for reintervention or death, allowing closer monitoring and timely intervention to improve outcomes.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 10:00 a.m.-10:45 a.m.
- Session Title: Congenital Heart Disease: Progress in Pediatric Heart Surgery
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1101-014
S-NITROSOHEMOGLOBIN LEVELS AFTER TRANSFUSION PREDICT OUTCOME OF PEDIATRIC BYPASSSURGERY
Faisal Matto, Peter Kouretas, Richard Smith, Jacob Ostrowsky, Anthony Cina, Douglas Hess, Jonathan Stamler and James D. Reynolds
vol. 69 no. 11 Supplement 593
DOI:
https://doi.org/10.1016/S0735-1097(17)33982-7
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Faisal Mattoa,b,
- Peter Kouretasa,b,
- Richard Smitha,b,
- Jacob Ostrowskya,b,
- Anthony Cinaa,b,
- Douglas Hessa,b,
- Jonathan Stamlera,b and
- James D. Reynoldsa,b
- aCase Western Reserve University, Cleveland, OH, USA
- bUniversity Hospitals, Cleveland, OH, USA
Background: Allogenic transfusion during pediatric cardio-pulmonary bypass can replace a significant portion of a child’s blood volume with banked red blood cells (RBCs). Within hours of procurement, RBCs exhibit impairments in nitric oxide (NO)-based vasodilation and oxygen delivery capability reflected in declines in S-nitrosohemoglobin (SNO-Hb). Thus, administration of even freshly stored blood may impair tissue oxygenation and worsen outcome.
Methods: In this prospective observational study we tracked the relationship between circulating SNO-Hb levels and post-transfusion outcomes in 20 children <12 months of age undergoing surgical repair of congenital cardiac defects. Per hospital protocol, all subjects received washed RBCs that had been stored for < 5 days.
Results: Intra-operative transfusion volume directly correlated with post-operative ventilator time and ICU stay and was associated with a decline in kidney tissue oxygenation and SNO-Hb levels even as arterial oxygen content increased. Accordingly, post-operative SNO-Hb levels inversely correlated with transfusion volume (increase in Hb) and renal function, i.e. the lower the SNO-Hb levels the worse the estimated glomerular filtration rate. Finally, regression analysis identified circulating SNO-Hb levels as an inverse predictor of outcome.
Conclusions: In young children undergoing cardiac surgery, large volume transfusion negatively impacts circulating SNO-Hb levels and is associated with worse outcome. Follow-on studies are required to validate SNO-Hb as an independent prognostic biomarker of transfusion response and to determine if maintenance of RBC-derived NO bioactivity can confer therapeutic benefit.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 10:00 a.m.-10:45 a.m.
- Session Title: Congenital Heart Disease: Progress in Pediatric Heart Surgery
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1101-015
PREDICTION TOOL FOR CONGENITAL HEART SURGERY LENGTH OF STAY
Matthew DiOrio, Catherine Allan, Ravi Thiagarajan, Kimberlee Gauvreau, Meena Nathan, Derek Mathieu, Aditya Kaza, James Dinardo, Jean Connor, John Mayer, Puja Banka, Jason Thornton, John Triedman and Lisa Bergersen
vol. 69 no. 11 Supplement 594
DOI:
https://doi.org/10.1016/S0735-1097(17)33983-9
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Matthew DiOrio,
- Catherine Allan,
- Ravi Thiagarajan,
- Kimberlee Gauvreau,
- Meena Nathan,
- Derek Mathieu,
- Aditya Kaza,
- James Dinardo,
- Jean Connor,
- John Mayer,
- Puja Banka,
- Jason Thornton,
- John Triedman and
- Lisa Bergersen
- Boston Children’s Hospital, Boston, MA, USA
Background: In response to increasing demand to optimize hospital resource use, we developed a methodology to predict extended length of stay (LOS) in the cardiac intensive care unit (CICU) following surgery for congenital heart disease.
Methods: Patients undergoing congenital heart surgery at Boston Children’s Hospital between 2007 and 2014 were identified. Clinical variables and established Surgical LOS Categories (SLC) were prospectively recorded based on surgical intervention performed. A model was built to predict the outcome post-operative CICU LOS > 7 days.
Results: The cohort included 6,242 cases categorized into 5 Surgical LOS categories with a C statistic of 0.77 for the outcome CICU LOS > 7 days. Explanatory value increased with inclusion of patient preoperative status as determined by age, ventilator dependence, and admission status (C statistic = 0.84, Table 1). Additional patient and procedural characteristics did not significantly increase model prediction.
Conclusions: Using a model comprised of basic patient characteristics, we have developed a robust method for predicting if a patient will remain in the CICU longer than seven days.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 10:00 a.m.-10:45 a.m.
- Session Title: Congenital Heart Disease: Progress in Pediatric Heart Surgery
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1101-016
TECHNICAL PERFORMANCE SCORE CAN PREDICT POST-DISCHARGE REINTERVENTIONS IN PARTIAL AND TRANSITIONAL ATRIOVENTRICULAR SEPTAL DEFECT REPAIR
Brielle Tishler, Kimberlee Gauvreau, Steven Colan, Pedro del Nido and Meena Nathan
vol. 69 no. 11 Supplement 595
DOI:
https://doi.org/10.1016/S0735-1097(17)33984-0
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- aBoston Children’s Hospital, Boston, MA, USA
- bHarvard Medical School, Boston, MA, USA
Background: Repair of partial or transitional atrioventricular septal defects (P/T AVSD) has excellent outcomes; however, late reinterventions remain a concern. Technical Performance Score (TPS) measures residua post repair and has been associated with early/mid-term outcomes after congenital cardiac surgery. We investigated TPS as a predictor of outcomes in P/T AVSD repair.
Methods: Single center retrospective review of P/T AVSD repair from 7/2000 to 11/2015. Intraoperative and discharge TPS were assigned based on echocardiographic criteria: class 1-no residua, class 2-minor residua, and class 3-major residua or reintervention for major residua. Intensive care unit (ICU)/hospital length of stay and post-discharge reintervention were analyzed using Cox regression.
Results: Of 183 patients, 124 (68%) and 59 (32%) underwent P/T AVSD repair respectively. Median age was 1.5 (IQR 0.6, 3.8) years, median weight was 9.7 (IQR 6.6, 14.1) kg, and 96 (52%) were female. There were 20 (11%) post-discharge reinterventions. On multivariable modeling, patients with class 3 TPS spent more days in the ICU (HR 0.33, CI 0.19, 0.58; p<0.001) and hospital (HR 0.38, CI 0.22, 0.64; p<0.001) and had shorter time to post-discharge reintervention (HR 8.76, CI 1.03, 74.7, p=0.05); table.
Conclusions: TPS may identify those with prolonged ICU/hospital stay and post-discharge reinterventions, providing feedback on areas of improvement in technique and identification of patients who warrant closer follow-up.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 10:00 a.m.-10:45 a.m.
- Session Title: Congenital Heart Disease: Progress in Pediatric Heart Surgery
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1101-017
THE ASSOCIATION OF TECHNICAL PERFORMANCE WITH POSTOPERATIVE COMPLICATIONS AND HOSPITAL COSTS FOR THE NORWOOD OPERATION
Kimberly E. McHugh, Sara Pasquali, Mark Scheurer, Matthew A. Hall and Meena Nathan
vol. 69 no. 11 Supplement 596
DOI:
https://doi.org/10.1016/S0735-1097(17)33985-2
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- aMedical University of South Carolina, Charleston, SC, USA
- bChildren’s Hospital Boston, Boston, MA, USA
Background: Technical performance scores (TPS) have been associated with both clinical outcomes and hospital costs in the congenital heart surgery population. However, the impact of TPS on costs in important subgroups, such as single ventricle patients (who account for the highest costs overall in this population) remains unclear. We evaluated the TPS-cost relationship in a multicenter Norwood cohort.
Methods: Clinical data from the Single Ventricle Reconstruction (SVR) trial were linked with cost data from Children’s Hospital Association’s CaseMix Database. TPS (optimal, adequate, inadequate) was assigned based on pre-defined criteria using the SVR dataset. The relationship of TPS with hospital costs was modeled, adjusting for baseline patient characteristics. Postoperative complications were also examined.
Results: A total of 266/555 (48%) SVR patients across 9 centers had both TPS and cost data available. Overall, 73% were classified as optimal TPS, 13% adequate, and 14% inadequate. In adjusted analysis, both total costs and the number of complications were more than 2 times higher in those with inadequate vs. optimal TPS (ratio between groups 2.3, 95% CI 1.6-3.3, p<.001, and 2.2, 95% CI 1.4-3.2, p<.001, respectively). Adjusted costs across TPS groups are shown in Figure 1.
Conclusions: Patients with inadequate Norwood TPS had more complications and higher hospital costs. These data suggest efforts geared toward improving TPS may have the potential to improve outcomes and reduce costs of care.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 10:00 a.m.-10:45 a.m.
- Session Title: Congenital Heart Disease: Progress in Pediatric Heart Surgery
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1101-018
RESIDUAL ATRIOVENTRICULAR VALVE REGURGITATION PRE-DISCHARGE IS ASSOCIATED WITH POST-DISCHARGE REINTERVENTIONS FOLLOWING COMPLETE ATRIO VENTRICULAR SEPTAL DEFECT REPAIR
Rinske Ijsselhof, Kimberlee Gauvreau, Pedro del Nido and Meena Nathan
vol. 69 no. 11 Supplement 597
DOI:
https://doi.org/10.1016/S0735-1097(17)33986-4
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- aBoston Children’s Hospital, Boston, MA, USA
- bUniversity Medical Center Utrecht, Utrecht, The Netherlands
Background: We have shown previously that technical performance score (TPS) is associated with post-discharge (DC) reinterventions (RI) in patients who undergo complete atrio ventricular septal defect (CAVSD) repair. The aim of this study is to determine which subcomponents of TPS can best predict post-DC RI.
Methods: Patients who underwent CAVSD repair between 2000 and 2016 were included. The final TPS (class 1-no residua, class 2-minor residua, class 3-major residua or RI pre-DC for residua) were assigned based on the summation of the subcomponent score for DC echocardiograms and certain clinical criteria as previously described. Follow-up (FU) data for up to 16 years were retrospectively collected. Nonparametric methods were used to determine association between the subcomponents of TPS and post-DC RI.
Results: A total of 331 patients were included in the analysis. There were 211 (60%) females. Median age at surgery was 3.2 (IQR: 2.4, 4.2) months. Fifty-four (16%) had class 1 TPS, 217 (66%) Class 2, 60 (18%) Class 3. There were 34 (10%) post-DC RI. Median FU was 2.6 (IQR: 0.09, 7.9) years. On nonparametric analysis, left atrioventricular valve (AVV) regurgitation, right AVV regurgitation and abnormal conduction were strongly associated with post-DC RI.
Conclusions: Pre-DC left and right AVV regurgitation and abnormal conduction at DC are among the subcomponents that are strongly associated with post-DC RI following CAVSD repair. TPS can serve as important tool for identifying patients at risk for RI.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 10:00 a.m.-10:45 a.m.
- Session Title: Congenital Heart Disease: Progress in Pediatric Heart Surgery
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1101-019
GENERAL ANESTHESIA RISK IN WILLIAMS BEUREN SYNDROME PATIENTS IN THE CURRENT ERA
Mark D. Levin and Beth A. Kozel
vol. 69 no. 11 Supplement 598
DOI:
https://doi.org/10.1016/S0735-1097(17)33987-6
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Mark D. Levin and
- Beth A. Kozel
- National Institutes of Health, Bethesda, MD, USA
Background: Williams-Beuren syndrome (WBS) patients have increased risk of sudden death, and these events are frequently associated with general anesthesia. We sought to determine the cardiopulmonary resuscitation (CPR) frequency in WBS patients as well as correlated risk factors associated with CPR need in this population.
Methods: We administered an online survey in collaboration with the Williams Syndrome Association to WBS patient families regarding their family member’s experience with anesthesia. Statistical analysis was performed on data from 649 WBS individuals, reflecting 1872 anesthesia events.
Results: CPR was performed during or shortly after 2.1% (40/1872) of WBS anesthesia procedures while 5% (33/649) of WBS individuals had at least one anesthesia-associated CPR event. 97.5% (39/40) of CPR episodes occurred in individuals with supravalvar aortic stenosis (29/40) or peripheral pulmonic stenosis (28/40). Twenty occurred in individuals with both diagnoses. Eleven events occurred in patients with coronary abnormalities, 10 in patients with ventricular septal defects, and 6 in patients with left ventricular hypertrophy. Pulmonary hypertension was present in 4 of 40 cases, while right ventricular hypertrophy was present in seven. Thirty of forty CPR cases were associated with either cardiac catheterization or CT surgical cases. In 21 of 40 episodes, the first CPR event occurred in the OR or cath lab; the remaining episodes occurred within 72 hours of the procedure. Nine individuals reported multiple code events following a single procedure. There were no significant differences between those having and those not having CPR events with respect to the following: gender, pre-procedural hydration duration, arrhythmia or sleep apnea history.
Conclusions: Anesthesia- associated CPR in a multi-center pediatric study was ∼2/30,000. CPR was performed in 2% of our cohort. While elevated compared to the general population, these data suggest WBS anesthesia risk in the current era is less than that reported during prior surgical eras. CPR event risk factors, such as biventricular outflow tract obstruction, may be helpful in identifying WBS patients at highest risk of negative outcome.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 10:00 a.m.-10:45 a.m.
- Session Title: Congenital Heart Disease: Progress in Pediatric Heart Surgery
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1101-020
ARRHYTHMIA BURDEN & OUTCOMES IN EISENMENGER SYNDROME
Shankar Baskar, Philippa Horne, Samantha Fitzsimmons, Philip Khoury, Joseph Vettukattill, Koichiro Niwa, Teiji Agaki, Mark Spence and Gruschen Veldtman
vol. 69 no. 11 Supplement 599
DOI:
https://doi.org/10.1016/S0735-1097(17)33988-8
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 30, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Shankar Baskar,
- Philippa Horne,
- Samantha Fitzsimmons,
- Philip Khoury,
- Joseph Vettukattill,
- Koichiro Niwa,
- Teiji Agaki,
- Mark Spence and
- Gruschen Veldtman
- Cincinnati Children’s Hospital, Cincinnati, OH, USA
Objective: Patients with Eisenmenger syndrome (ES) have a shorter life-span than the general population. A significant proportion develop arrhythmia and some, sudden death. Despite these observations, studies characterizing arrhythmias and their prognostic value in ES are lacking.
Methods: This retrospective study included patients aged ≥ 18 years of age with ES from Southampton University Hospital, the Japanese Adult Congenital Heart group and Belfast, Northern Ireland. Information was collected from chart review and arrhythmias were noted from clinical encounters, electrocardiograms and Holter study reviews.
Results: A total of 167 patients, 95 females, 63 males (gender not available in 9 patients) were included in this study. The mean age was 37 ± 10 years (range: 18 – 63 years) with a majority in NYHA functional class II or III (57% and 32% respectively) and mean oxygen saturation of 85±7 %. Twenty eight patients (17%) had a documented history of arrhythmia: paroxysmal supraventricular tachycardia (8 patients, 29%), atrial fibrillation (6 patients, 21%), atrial fibrillation and flutter (2 patients, 7%), non-sustained ventricular tachycardia (6 patients, 21%) and sustained ventricular tachycardia (6 patients, 21%). Twenty-five of the patients (15%) were on anti-arrhythmic therapy and 77 patients (49%) were on disease targeting therapy for pulmonary hypertension. Downs syndrome was present in 76 patients (46%). Patients with arrhythmia were older [p=0.01] and were more likely to have atrioventricular valvar regurgitation [Odds ratio: 4.33]. Arrhythmias were found to independently predict all-cause mortality [p=0.004] and sudden death in bivariate analysis [p=0.03]. Disease targeting therapy was a protective factor against all-cause mortality in logistic regression analysis [Odds ratio: 0.31], while anti-arrhythmics predicted sudden death [Odds ratio: 6.24].
Conclusions: Arrhythmias are common among patients with ES, with atrio-ventricular valve regurgitation being a risk-factor. Arrhythmias may predict sudden death, the risk of which is not reduced by being on anti-arrhythmics.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 10:00 a.m.-10:45 a.m.
- Session Title: The Story of the Adult Congenital Heart Disease Patient and EP
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1102-021
SAFETY OF TRANSVENOUS LEAD REMOVAL IN ADULT CONGENITAL HEART DISEASE IN THE US
Xiaofan Guo, Robert Hayward, Eric Vittinghoff, Sun Yong Lee, Ian Harris, Mark Pletcher and Byron Lee
vol. 69 no. 11 Supplement 600
DOI:
https://doi.org/10.1016/S0735-1097(17)33989-X
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Xiaofan Guoa,b,
- Robert Haywarda,b,
- Eric Vittinghoffa,b,
- Sun Yong Leea,b,
- Ian Harrisa,b,
- Mark Pletchera,b and
- Byron Leea,b
- aUniversity of California, San Francisco, San Francisco, CA, USA
- bThe First Hospital of China Medical University, Shenyang, People’s Republic of China
Background: There is a growing population of adult congenital heart disease (CHD) patients in the United States. Data are scarce on outcomes of transvenous lead removal (TLR) in adult CHD.
Methods: We used Healthcare Cost and Utilization Project Nationwide Inpatient Sample to identify TLR procedures in adult patients with and without CHD 2005 to 2012. Outcomes included in-hospital mortality and complications. Multivariable logistic regression models and hierarchical models adjusted for clinical and hospital- related confounders were used in analysis.
Results: We found 101,568 adult patients undergoing TLR, 1175 with simple CHD, 536 with complex CHD and 670 with unspecified CHD. Simple atrial septal defect or patent foramen ovale was the most common congenital defects (871 cases in total). A total of 74.8% CHD patients underwent TLR procedure in teaching hospital. Also, CHD patients who had TLR procedure were more likely to be admitted in hospitals with large bed size and high volume than non-CHD patients (Both P<0.001). Compared to patients without CHD, CHD was associated with a higher risk of any complication even after adjusting for device infection (OR 1.56, 95% CI 1.17-2.07, P=0.003). Simple and complex CHD were associated with 1.6 and 2.0fold risk for any TLR-related complication respectively (OR 1.64, 95% CI 1.09-2.47, P=0.018 for simple CHD; OR 2.01, 95% CI 1.24-3.26, P=0.005 for complex CHD). CHD was not associated with increased risk of in-hospital mortality (adjusted odd ratio [aOR] 1.23, 95% confidence interval [CI] 0.67-2.27, P=0.500).
Conclusions: Despite being more likely to be sent to high volume teaching hospitals, adults with simple and complex CHD undergoing TLR are more likely to have complications without comcommitent increased mortality when compared to patients without CHD. This higher risk should be considered when discussing TLR in adults with CHD.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 10:00 a.m.-10:45 a.m.
- Session Title: The Story of the Adult Congenital Heart Disease Patient and EP
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1102-022
ACQUIRED LONG-TERM CARDIAC RHYTHM AND CONDUCTION ABNORMALITIES AFTER ARTERIAL SWITCH OPERATION
Takeshi Tsuda, Jeanne Baffa, Bradley Robinson, Rami Kharouf, Abdul Bhat and Joel Temple
vol. 69 no. 11 Supplement 601
DOI:
https://doi.org/10.1016/S0735-1097(17)33990-6
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Takeshi Tsuda,
- Jeanne Baffa,
- Bradley Robinson,
- Rami Kharouf,
- Abdul Bhat and
- Joel Temple
- Nemours/Afred I. duPont Hospital for Children, Wilmington, DE, USA
Background: Arterial switch operation (ASO) is commonly indicated for d-loop transposition of the great arteries (d-TGA) in early infancy. Incidence and clinical significance of long-term electrical abnormalities after ASO has not been well studied.
Methods: We retrospectively reviewed medical records of 99 patients (65 male) with d-TGA and Taussig-Bing anomaly who have been followed as outpatients after ASO for more than 1 year (from 1998 to 2015). ECG and echocardiogram were routinely obtained in all patients. Holter ECG, exercise stress test (EST), and electrophysiological study (EPS) were performed in selective patients.
Results: Follow-up period ranged from 1 to 23 years (10.1 ± 6.2). Sinus bradycardia was seen in 5 patients; 2 patents underwent atrial pacemaker implantation. Complete right bundle branch block (CRBBB) was seen in 13 patients, including 10 patients with surgical closure of ventricular septal defect (VSD). Left bundle branch block (LBBB) was noted in 1 patient. Two patients had first-degree AV block, but none developed advanced heart block. Atrial tachycardia (AT) was noted in 2 patients; one patient underwent EPS and electrical ablation. Variable frequency of isolated monomorphic premature ventricular complexes (PVCs) was noted in 12 patients (from < 1 % to 16% of total heart beats by Holter ECG); 1 was found to have non-sustained ventricular tachycardia (NS-VT) with exercise-induced PVCs who complained recurrent chest pain. Three patients developed syncope; 1 with sustained polymorphic VT detected by a loop monitor, 1 with ventricular fibrillation (VF) during exercise secondary to severe obstruction of proximal left coronary artery, and 1 with prolonged sinus pause (15 sec). One with polymorphic VT and the other with VF had an implantable cardioverter defibrillator (ICD) and coronary recanalization surgery with ICD, respectively.
Conclusions: The incidence of electrical abnormalities after ASO is not infrequent and may be underestimated unless specifically investigated. Electrical abnormalities occurred with or without associated coronary artery abnormalities. Long-term surveillance of the electrical abnormalities is warranted after ASO.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 10:00 a.m.-10:45 a.m.
- Session Title: The Story of the Adult Congenital Heart Disease Patient and EP
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1102-023
PREVALENCE AND PREDICTORS OF ATRIAL TACHYARRHYTHMIAS IN ADULT FONTAN PATIENTS
Anushree Agarwal, Aarthi Sabanayagam, Ahmed Kheiwa, Colin Cunnington, Ian Harris, Edward Gerstenfeld, Charles McCulloch, Elyse Foster, Zian Tseng, Lucas Zier, Petra Jenkins, Jaspal Dua, Devinda Karunaratne, Sahrkaw Muhyaldeen, Amir Zaidi, Adam Fitzpatrick, Clifford Garratt, Bernard Clarke, Andreas Hoschtitzky and Vaikom Mahadevan
vol. 69 no. 11 Supplement 602
DOI:
https://doi.org/10.1016/S0735-1097(17)33991-8
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Anushree Agarwala,b,
- Aarthi Sabanayagama,b,
- Ahmed Kheiwaa,b,
- Colin Cunningtona,b,
- Ian Harrisa,b,
- Edward Gerstenfelda,b,
- Charles McCullocha,b,
- Elyse Fostera,b,
- Zian Tsenga,b,
- Lucas Ziera,b,
- Petra Jenkinsa,b,
- Jaspal Duaa,b,
- Devinda Karunaratnea,b,
- Sahrkaw Muhyaldeena,b,
- Amir Zaidia,b,
- Adam Fitzpatricka,b,
- Clifford Garratta,b,
- Bernard Clarkea,b,
- Andreas Hoschtitzkya,b and
- Vaikom Mahadevana,b
- aUniversity of California San Francisco, San Francisco, CA, USA
- bManchester Royal Infirmary, Central Manchester University Hospitals NHS Trust, Manchester, United Kingdom
Background: Fontan surgery provides palliation for single ventricle patients. A late complication is the development of atrial tachyarrhythmias (AT). This study aims to establish incidence and identify predictors of AT in Fontan patients with long-term follow-up.
Methods: Retrospective review of medical records from 2 tertiary academic institutions identified 113 Fontan patients ≥ 18 years.
Results: Mean age was 31 ± 7years, 54% females; 37% atriopulmonary (AP) Fontan, 31% lateral tunnel (LT), and 32% extracardiac (EC). Mean follow-up was 31± 7 yrs and time since Fontan surgery was 23± 6 yrs. We estimated that by age 35 yrs over half will have AT. Incidence of AT was 57% in AP, 27% in LT and 16% in EC groups at follow-up. Patients with AT more likely had AP Fontan (57% vs. 22%, p<0.0001) and New York Heart association (NYHA) class II/III (46%vs.25%, p=0.04) than those without. Kaplan-Meier curve shows that median time to AT was dependent on gender and age at the time of Fontan surgery (Figure). Multivariate Cox regression analysis showed no effect of Fontan type, NYHA class, but confirmed female gender (hazard ratio (HR) 0.4; p=0.008) and increasing age at Fontan surgery as independent predictors of reduced HR (0.8; p<0.001).
Conclusions: There is a significant, increased atrial tachyarrhythmia burden in adult Fontan patients that is dependent on gender and age at Fontan surgery. These patients continue to pose significant challenges as adults and long-term close follow with defined management strategies is crucial.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 10:00 a.m.-10:45 a.m.
- Session Title: The Story of the Adult Congenital Heart Disease Patient and EP
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1102-024
WORSE OUTCOMES IN HOSPITALIZATIONS OF WOMEN WITH TURNER SYNDROME COMPARED TO WOMEN WITHOUT TURNER SYNDROME
Isani Singh, Lindsey M. Duca, David Kao and Amber Khanna
vol. 69 no. 11 Supplement 603
DOI:
https://doi.org/10.1016/S0735-1097(17)33992-X
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online December 1, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Isani Singh,
- Lindsey M. Duca,
- David Kao and
- Amber Khanna
- University of Colorado, Aurora, CO, USA
Background: While studies show Turner Syndrome (TS) patients are at an increased risk for cardiovascular (CV) complications, outcomes of hospitalized TS patients are yet to be explored.
Methods: Cases of TS and comparable controls were acquired from an administrative database of inpatient hospitalizations. TS cases were matched 1:4 to controls based on primary ICD-9 diagnosis code. The study population was comprised of 14,890 women (n=2978 TS; n=11,912 non-TS) aged 20-80 years hospitalized from 2006-2012 in 8 states. Patients hospitalized for a CV indication (cardiomyopathy, heart failure, arrhythmia, hypertension, atherosclerosis, or ischemic heart disorders) included 2,110 women (n=424 TS; n=1,686 non-TS). Conditional logistic regression models were used to investigate association between TS and mortality, discharge disposition, and length of stay in hospitalized patients after adjusting for age, race, insurance group, and Charlson Comorbidity Index (CCI).
Results: Overall, the odds of mortality were 44% higher in TS patients compared to matched controls (Odds Ratio (OR): 1.44, 95% Confidence Interval (CI): 1.02 – 2.02, p = 0 .04). The odds of being discharged to home were reduced by 32% in TS patients compared to matched controls (OR = 0.68, 95% CI: 0.60 – 0.78, p < 0.0001). Likelihood of mortality was significantly higher in patients with TS and a CV primary diagnosis compared to matched controls with a CV primary diagnosis (OR = 3.10, 95% CI: 1.27 – 7.57, p = 0.01). TS patients were also more likely to have a longer than average length of stay (> 4 days) than controls (OR = 1.42, 95% CI: 1.03 – 1.95, p = .03). In those hospitalized with a CV disorder, the odds of being discharged home were lower in patients with TS compared to matched controls (OR = 0.55; 95% CI: 0.38 – 0.80, p = .001).
Conclusions: TS patients have worse outcomes than non-TS patients hospitalized with the same condition. These discrepancies are larger in patients hospitalized for CV diagnoses.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Adult Patients With Congenital Heart Disease: How Do They Compare?
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1142-009
RISK OF STROKE IN ADULT PATIENTS WITH CONGENITAL HEART DISEASE COMPARED WITH THE GENERAL POPULATION: A DANISH NATIONWIDE POPULATION-BASED COHORT STUDY
Mette Glavind Bülow Pedersen, Morten Olsen, Morten Schmidt, Henning B. Laursen, Søren Johnsen and Nicolas Madsen
vol. 69 no. 11 Supplement 604
DOI:
https://doi.org/10.1016/S0735-1097(17)33993-1
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Mette Glavind Bülow Pedersena,b,
- Morten Olsena,b,
- Morten Schmidta,b,
- Henning B. Laursena,b,
- Søren Johnsena,b and
- Nicolas Madsena,b
- aDepartment of Clinical Epidemiology, Aarhus University Hospital, Aarhus N, Denmark
- bHeart Institute, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA
Background: Congenital heart disease (CHD) is associated with known risk factors for stroke such as cardiac arrhythmias and heart failure. The incidence and mortality of stroke in adults with CHD remains incompletely understood.
Methods: Using population-based Danish nationwide registries, we identified all individuals diagnosed with CHD between 1963 and 2012. Patients were included if alive and living in Denmark at the minimum age of 30 years. Using the Danish Civil Registration system, we created a general population comparison cohort by matching 10 individuals to each CHD subject on sex and birth year. Follow-up started at the age of 30 years and continued until a first stroke diagnosis, emigration, or death, whichever came first. Using Cox proportional-hazards regression, we computed hazard ratios (HRs) as estimates of the relative risk of stroke and 30-day mortality in adults with CHD compared with the general population, adjusted for sex and birth year.
Results: We identified 10,113 adults with CHD and 97,672 comparison cohort members. The risk of stroke among adults with CHD was more than two-fold increased compared with the general population (adjusted HR=2.2, 95% CI: 2.0-2.5). The 30-day stroke mortality was 11% for the 507 CHD subjects and 9.9% for the 3,115 comparison cohort members. This difference in risk corresponded to a 40% increased 30-day stroke mortality compared with the general population after adjustment for sex and birth year (HR=1.39, 95% CI: 1.04-1.86). CHD severity did not modify stroke mortality (mild to moderate CHD: HR=1.50, 95% CI: 1.05-2.14. Severe CHD and univentricular heart: HR=1.47, 95% CI: 0.81-2.67).
Conclusions: Adults with CHD had an increased risk of both experiencing and dying from a stroke.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Adult Patients With Congenital Heart Disease: How Do They Compare?
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1142-010
OBSTRUCTIVE SLEEP APNEA IN ADULT CONGENITAL HEART DISEASE: WHO IS AT RISK?
Benjamin Hendrickson, Damilola Olatunji, David Briston, Pamela Goldsmith, Matthew Granger, Trisha Gribble, Krista Kukovec, Renee Schnug, Rami Khayat, Curtis Daniels and Elisa Bradley
vol. 69 no. 11 Supplement 605
DOI:
https://doi.org/10.1016/S0735-1097(17)33994-3
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Benjamin Hendricksona,b,
- Damilola Olatunjia,b,
- David Bristona,b,
- Pamela Goldsmitha,b,
- Matthew Grangera,b,
- Trisha Gribblea,b,
- Krista Kukoveca,b,
- Renee Schnuga,b,
- Rami Khayata,b,
- Curtis Danielsa,b and
- Elisa Bradleya,b
- aOhio State University, Columbus, OH, USA
- bNationwide Children’s Hospital, Columbus, OH, USA
Background: Obstructive sleep apnea (OSA) is common in patients with cardiovascular disease. In patients with adult congenital heart disease (ACHD), risk for OSA is not well described. We aimed to define ACHD patients at high risk for OSA.
Methods: ACHD patients (≥18 yo, not peripartum) were offered participation in cardiology clinic (survey duration: 8 weeks). An e-questionnaire comprised of OSA screening tools was administered (Epworth Sleepiness Scale, Berlin and STOP-BANG questionnaires) and demographic data was collected.
Results: A total of 150 patients participated (male n=75(50%), 36±15 yo, BMI 28+8). Of these, 19(13%) had an established diagnosis of OSA, 41(30%) were high risk on at least one and 11(8%) on >2 OSA screening tools. Older age was associated with increased risk for OSA or formal OSA diagnosis (1-screen positive 31±11yo, ≥2-screen positive 33±15yo, OSA 48+16yo, p<0.001). Serial increases in BMI were seen across high risk and OSA groups (No OSA/low risk 26+6kg/m2, 1-screen positive 29±8kg/m2, >2-screen positive 31±7kg/m2, OSA 36±11kg/m2, p<0.001). Patients with moderate/severe CHD were more likely to test high risk or have known OSA compared to simple CHD (X2=5.8, p<0.05, Fig 1).
Conclusions: This is the first prospective study evaluating the presence or risk for OSA in a diverse ACHD population. Half of patients with moderate/severe ACHD had a diagnosis of, or were high risk for OSA, compared to one-third of those with simple ACHD. Younger, leaner patients were found to be at less risk.
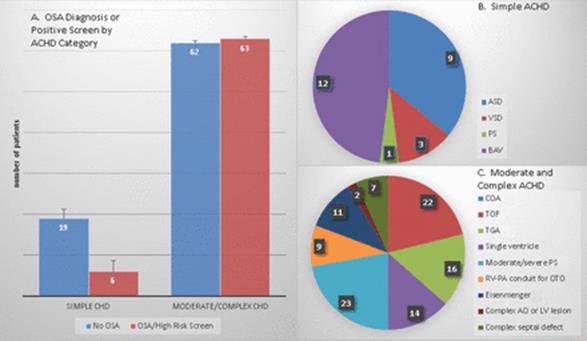
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Adult Patients With Congenital Heart Disease: How Do They Compare?
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1142-011
MORTALITY IN PREGNANT WOMEN WITH CONGENITAL HEART DISEASE: A SUBANALYSIS OF THE CALIFORNIA PREGNANCY-ASSOCIATED MORTALITY REVIEW
Aarthi Sabanayagam, Anushree Agarwal, Christy MacCain, Elizabeth Lawton, Elliot Main, Afshan Hameed, Ian Harrisand Elyse Foster
vol. 69 no. 11 Supplement 606
DOI:
https://doi.org/10.1016/S0735-1097(17)33995-5
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Aarthi Sabanayagam,
- Anushree Agarwal,
- Christy MacCain,
- Elizabeth Lawton,
- Elliot Main,
- Afshan Hameed,
- Ian Harrisand
- Elyse Foster
- University of California San Francisco, San Francisco, CA, USA
Background: Heart disease accounts for ∼10% of mortality and morbidity during pregnancy. Congenital heart disease (CHD) is the most common cardiac condition affecting women during pregnancy. Despite improvements in survival and quality of life for patients with CHD, pregnancy remains high risk or even contraindicated in some of these women.
Methods: Maternal mortality rates increased from 2002-2006 in California. The California Pregnancy-Associated Mortality Review identified 917 women who died while pregnant or within the first year of delivery. All available inpatient and outpatient records for women with CHD were reviewed. Deaths were deemed pregnancy related if death was directly related or aggravated due to the physiological changes of pregnancy and/or its management (n=286).
Results: Eight women (mean age was 26.6 +/- 7.4 years, 6 Hispanic and 2 African American) were identified with CHD (Eisenmenger’s=2, Congenital Corrected Transposition of the Great Vessels=1, Tetralogy of Fallot = 1, Ventricular septal defect = 1, Atrial septal defect = 2, Bicuspid Valve/Severe aortic stenosis = 1). The first prenatal visit occurred at a mean of 12.7 +/-6.2 weeks. Average gestational age at the time of delivery was 33.8 +/- 5.5 weeks. Six of these women were aware of their cardiac diagnosis prior or during their pregnancy and 6 underwent emergent C-section. Three women died of sudden cardiac death and 1 within the first 24 hours of delivery. Six deaths were thought to be pregnancy related and 5 were within 6 weeks of delivery. Retrospective use of the ZAHARA risk model predicted an increased risk (>=7.5%) of cardiovascular events in 5 women.
Conclusions: This descriptive series gives a rare insight into the events surrounding death in this unique population. Despite seeking early prenatal care, these women had less than ideal follow-up for their CHD during pregnancy. The progression of the underlying disease process once these women presented was rapid if not instantaneous. This underscores the importance of a multidisciplinary team of specialized cardiologists, high-risk obstetricians in following these patients throughout pregnancy as well as in the early post-partum period.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Adult Patients With Congenital Heart Disease: How Do They Compare?
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1142-012
EXERCISE CAPACITY AFTER REPAIR OF EBSTEIN ANOMALY IN ADULTS: THE CONE ERA
Brandon Morrical, Joseph Dearani, David Driscoll and Nathaniel Taggart
vol. 69 no. 11 Supplement 607
DOI:
https://doi.org/10.1016/S0735-1097(17)33996-7
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Brandon Morrical,
- Joseph Dearani,
- David Driscoll and
- Nathaniel Taggart
- Mayo Clinic, Rochester, MN, USA
Background: The circumferential “cone” repair has become the preferred method of repairing Ebstein anomaly of the tricuspid valve (TV). Reported surgical outcomes have been excellent. However, there have been no recent studies examining exercise or functional capacity in patients who have undergone tricuspid valve surgery in the modern era.
Methods: We performed a retrospective chart review of all patients with Ebstein anomaly who underwent TV surgery at Mayo Clinic between 6/07 and 1/15. We compared pre and postsurgical echos, exercise tests, and clinic visits. Statistical analysis was done using paired t-test and one-way ANOVA.
Results: TV surgery was done in 322 patients. Among this cohort, 32 patients met criteria of native TV repair or replacement and maximal pre and postsurgery exercise tests. Nineteen patients had valve repairs, and 13 had valve replacements. The average age was 41 years old (range 18-64), and consisted of 69% females. Surgery resulted in significant reduction in tricuspid regurgitation (p = 0.0001) and right ventricular size (p = 0.0003), with 72% of patients having trivial or no tricuspid regurgitation after surgery. There was a significant improvement in NYHA functional class (p = 0.001), with 69% of patients categorized as NYHA class I after surgery. No significant difference was found in functional aerobic capacity (FAC), metabolic equivalents (METs), or exercise time. There was a trend toward a decreased VO2 max after surgery (p = 0.056). Peak heart rate during exercise declined after surgery (p = 0.032). Those who had a PFO or ASD closed during surgery had improved minimum saturations during exercise (p = 0.045), though they did not have any difference in measured exercise capacity. There was no significant difference between those that had repair or replacement of the TV.
Conclusions: In our cohort, patients who had TV repair or replacement for Ebstein anomaly had improved NHYA function class. However, patient-described function was not reflected in measured exercise capacity, despite excellent surgical results by echo. Further follow-up and more consistent testing may provide more reliable information regarding these patients’ exercise and functional capacity.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Adult Patients With Congenital Heart Disease: How Do They Compare?
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1142-013
FACTORS ASSOCIATED WITH COMPLETION OF ADVANCED DIRECTIVES IN ADULTS WITH CONGENITAL HEART DISEASE
Nancy H. Klein, Whitney Osborne, Rachel Steury, Seiji Ito, Ruth Phillippi and Anitha John
vol. 69 no. 11 Supplement 608
DOI:
https://doi.org/10.1016/S0735-1097(17)33997-9
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Nancy H. Klein,
- Whitney Osborne,
- Rachel Steury,
- Seiji Ito,
- Ruth Phillippi and
- Anitha John
- Children’s National Health System, Washington, DC, USA
Background: It is recommended that all patients (pts), especially with a chronic health condition, have some form of advanced directives (AD) as part of their long-term health planning. Barriers to AD completion in the adult congenital heart disease (ACHD) population are not well defined; we evaluated factors associated with completion of AD in the general ACHD population.
Methods: From Sep 2015 to Aug 2016, 341 pts (46% male) completed clinical questionnaires regarding completion of a living will (LW), durable power of attorney (POA) or discussion regarding end-of-life care with family. Questionnaires also included: age, gender, race, education, marital status, children, and depression and anxiety screening (PHQ-4 inventory).
Results: Mean age was 31 ± 10 years (yrs). Disease complexity was classified as: mild (17%), moderate (52%), and severe (31%). Fifty eight pts (17.0%) had a LW or POA, 63 pts (18.5%) had discussed their wishes with family, and 220 pts (64.5%) did not have an AD. 37 pts (10.9%) had both discussed their wishes with family and also had a LW and/or POA completed. Advanced education (p<0.01), older age (p<0.01), white race (p=0.01), and living with a spouse (p<0.01) or child (p=0.02) was significantly associated with completion of a LW or POA. Disease complexity was not significant associated with completion of AD (p=0.06). Eighteen pts (5%) had screening depression scores ≥ 3 and 38 pts (11%) had screening anxiety scores ≥ 3, warranting further work-up. There was no correlation with AD completion and anxiety or depression scores. After controlling for age, patients with an associate degree or higher were nearly twice as likely to have completed a LW, POA, or discussed with family (OR 1.8, 95% CI=1.3-2.5). Reasons for not completing AD included: lack of knowledge (n=26, 11.8%), no time for completion (n=18, 8.2%), and not knowing where to start (n=82, 37.3%).
Conclusions: ACHD patients have low rates of AD completion. Older patients with education higher than a high school diploma had higher rates of completion while disease severity had no association. Further education about the importance of AD is needed, with an emphasis on addressing potential disparities and access to resources.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Adult Patients With Congenital Heart Disease: How Do They Compare?
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1142-014
DECREASED HEPATIC ELASTICITY IN YOUNG ADULTS AFTER BIVENTRICULAR REPAIR OF CONGENITAL HEART DISEASE
Shaija Shelby, David Danford, Jonathan Cramer, Angela Yetman, Shane Tsai, Ling Li, Scott Fletcher, Ruben Quiros-Tejeira and Shelby Kutty
vol. 69 no. 11 Supplement 609
DOI:
https://doi.org/10.1016/S0735-1097(17)33998-0
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Shaija Shelbya,b,
- David Danforda,b,
- Jonathan Cramera,b,
- Angela Yetmana,b,
- Shane Tsaia,b,
- Ling Lia,b,
- Scott Fletchera,b,
- Ruben Quiros-Tejeiraa,b and
- Shelby Kuttya,b
- aUniversity of Nebraska Medical Center, Omaha, NE, USA
- bChildrens’ Hospital and Medical Center, Omaha, NE, USA
Background: Hepatic dysfunction is a recognized complication in single ventricle heart disease, however it is unknown if patients with repaired biventricular heart disease (BHD) are prone to hepatic changes manifested as elevated stiffness. We measured hepatic stiffness and vascular Doppler indices using ultrasound (US) and shear wave elastography (SWE) in a BHD cohort.
Methods: BHD patients and normal controls were recruited for hepatic US with SWE. US-SWE system (SuperSonic Imagine) and transducers enabled generation of transient shear waves with real-time B-mode imaging. Using Q-box plug-in with OsiriX, stiffness measurements were expressed as Young’s Modulus (kPa). Doppler measurements were made in celiac and superior mesenteric arteries, and main portal vein. These were peak velocities, velocity time integral, resistive, pulsatility and acceleration indices (RI, PI, AI), and portal vein flow volume. Comparisons were made between BVD, controls and a historical cohort of Glenn and Fontan patients.
Results: Fifty-eight subjects were prospectively studied: 28 BHD (8 female, age 27.2±4.3 years, weight 78.3±22 kg) and 30 controls (23 female, age 27.4±3.8 years, weight 70.0±17 kg). Diagnoses were tetralogy of Fallot/pulmonary atresia (n=14), transposition of great arteries (n=13), and anomalous pulmonary venous return (n=1). BHD had lower superior mesenteric artery PI (2.47 vs. 2.94, p=0.05) and higher main portal vein PI (0.70 vs. 0.50, p=0.008) compared to controls. No association was seen in stiffness or other indices with age, gender, or time since surgical repair. Hepatic stiffness (kPA) was 8.0 ± 2.1 in BHD, 6.8 ± 2.3 in Glenn (n=20, age 2±1 years) and 15.6 ± 5.1 in Fontans (n=41, age 14±6 years); differences between BHD and Fontan were significant (p<0.001), whereas between BHD and Glenn was not (p=0.11).
Conclusions: Decreased hepatic elasticity occurs in some young adults with repaired BHD. Although the cause is not established, considerations include pre-or peri-operative hepatic congestion early in life, and/or chronic right heart burden later after repair. Further research is required to determine if these patients will ultimately suffer from clinically relevant liver disease.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Adult Patients With Congenital Heart Disease: How Do They Compare?
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1142-015
RIGHT AND LEFT VENTRICULAR MECHANICS ARE ALTERED IN ADOLESCENTS AND ADULTS LATE AFTER REPAIR OF SUBARTERIAL VENTRICULAR SEPTAL DEFECTS
Sit-Yee Kwok, Susanna Yeung, Wing Yi Li and Yiu-Fai Cheung
vol. 69 no. 11 Supplement 610
DOI:
https://doi.org/10.1016/S0735-1097(17)33999-2
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Sit-Yee Kwok,
- Susanna Yeung,
- Wing Yi Li and
- Yiu-Fai Cheung
- University of Hong Kong, Hong Kong, Hong Kong
Background: There is increasing concern of ventricular dysfunction in patients late after repair of perimembranous ventricular septal defect (VSD). We tested the hypothesis that right (RV) and left ventricular (LV) mechanics are altered in patients late after surgical closure of subarterial VSD and determined the associated risk factors.
Methods: Twenty-nine patients aged 23.5±7.0 years, at 11.7±7.7 years after surgery, and 29 age-matched controls were studied. Global RV and LV function was assessed using M-mode, tissue Doppler, and speckle tracking echocardiography, while contractile function of RV outflow was assessed by determining its shortening fraction (SF).
Results: Residual aortic regurgitation was trivial/mild in 20 (68.9%) patients and moderate in 1 (3.4%). QRS duration (101±17 ms vs 91±9 ms, p=0.01) was significantly longer in patients than controls. Compared with controls, patients had significantly lower tricuspid annular systolic (p=0.003) and diastolic (p<0.001) velocities, isovolumic acceleration (p<0.001), and RV global longitudinal systolic strain (p=0.011), systolic strain rate (p=0.007), and late diastolic strain rate (p=0.04), and greater ratio of transtricuspid to tricuspid annular early diastolic velocities (p<0.001). Furthermore, their RV outflow SF (42.7±10.0 % vs 49.7±7.5 %, p=0.004) was reduced. For LV function, patients had significantly lower shortening fraction (p<0.001), global longitudinal systolic strain (p=0.006), systolic strain rate (p=0.003), and early (p=0.047) and late (p=0.04) diastolic strain rates than controls. The RV and LV systolic strain and systolic and diastolic strain rates were significantly associated (all p<0.05). For the entire cohort, QRS duration (r=-0.34, p=0.011), and RV outflow SF (r=0.40, p=0.002) were found to correlate significantly with LV systolic strain and tended to correlate with RV systolic strain (r=-0.23, p=0.097 and r=0.25, p=0.07, respectively).
Conclusions: Right and left ventricular systolic and diastolic mechanics are significantly impaired and interrelated in patients after subarterial VSD repair, which in part may be related to prolonged QRS duration and RV outflow dysfunction.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Adult Patients With Congenital Heart Disease: How Do They Compare?
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1142-016
COST-ANALYSIS OF OUTPATIENT CARDIAC CATHETERIZATION IN INFANTS WITH SINGLE VENTRICLE CONGENITAL HEART DISEASE
Jamie Colombo, Michael Spaeder, Jeffrey Vergales and Michael Hainstock
vol. 69 no. 11 Supplement 611
DOI:
https://doi.org/10.1016/S0735-1097(17)34000-7
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Jamie Colombo,
- Michael Spaeder,
- Jeffrey Vergales and
- Michael Hainstock
- University of Virginia, Charlottesville, VA, USA
Background: Cardiac catheterization (CC) is performed in patients with single ventricle congenital heart disease (SVCHD) to aid in hemodynamic assessment, intervention and surgical planning. Outpatient CC reduces anxiety to patients and families and decreases cost. Given the morbidity and mortality associated with interstage SVCHD, substantial post-procedural variability exists and best practices remain unclear. The objective of this study was to investigate the economic implications of outpatient cath with potential readmission vs. universal 23-hour overnight observation in infants with SVCHD.
Methods: We performed a retrospective review of patients less than one year of age with SVCHD who underwent CC from 2007-2015 at our institution. A decision-tree based cost analysis was performed utilizing known procedural and in-hospital costs. Stochastically-based sensitivity analyses were then performed to challenge base-case estimates.
Results: The baseline cost of same day discharge + probability of readmission cost was less than the cost for 23-hour observation + the probability of accruing a longer hospitalization, given our readmission rate of 3% ($5,660 vs. $10,003). The readmission rate of outpatient CC would need to increase to 71% for costs to equilibrate to that of universal 23-hour observation (Figure 1).
Conclusions: Outpatient CC for infants with SVCHD demonstrates lower attributed cost compared to universal 23-hour observation, given the low rate of readmission.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Congenital Heart Disease: Advances in Quality Improvement for Pediatric Cardiac Care
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1143-017
REVENUE RETURN ON INVESTMENT FOR CENTER INVOLVEMENT IN A QUALITY IMPROVEMENT COLLABORATIVE FOR A RARE DISEASE: NATIONAL PEDIATRIC CARDIOLOGY QUALITY IMPROVEMENT COLLABORATIVE
Jeffrey B. Anderson, David Brown, Stacey Lihn, James Tweddell, Jesse Hansen, Mark McDonald, Greg Lubiani and Carole Lannon
vol. 69 no. 11 Supplement 612
DOI:
https://doi.org/10.1016/S0735-1097(17)34001-9
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Jeffrey B. Anderson,
- David Brown,
- Stacey Lihn,
- James Tweddell,
- Jesse Hansen,
- Mark McDonald,
- Greg Lubiani and
- Carole Lannon
- Cincinnati Children’s Hospital, Cincinnati, OH, USA
Background: Clinical centers in the National Pediatric Quality Improvement Collaborative (NPC-QIC) partner with parents of children with hypoplastic left heart syndrome (HLHS) to improve care and outcomes. Collaboration in NPC-QIC requires a cost for participating centers.
Our objective was to estimate return on investment for a center participating in NPC-QIC.
Methods: The NPC-QIC registry data provided mortality outcomes from participating centers between 2006-2014. Financial data from a single center was used to estimate administrative costs associated with involvement in the collaborative (e.g. annual participation fees, personnel, and travel costs) and revenue associated with caring for infants with HLHS who survived through their first birthdays (based on internal billing records normalized to 2014 dollars). Data on patients who exclusively received their inpatient and outpatient care at this single institution between 2004-2014 and who survived to their first birthday were analyzed.
Results: From 2006-2014 there was a 40% reduction (9.8%-5.5%) in interstage mortality across participating centers, correlating with one less death per 23 patients. Annual single center administrative costs for NPC-QIC involvement were $38,271. At this center there were 69 patients with HLHS who survived to one year of life during the study period. At 12 months of life the median revenue was $488,944 ($28,261 – 3,813,187) per patient.
Conclusions and Implications: Improved patient outcomes matter to parents and clinicians. Reassuring to institutions is that participation in NPC-QIC not only leads to improved patient outcomes but that the potential revenue associated with improved results for a center significantly outweighs the cost of involvement in NPC-QIC.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Congenital Heart Disease: Advances in Quality Improvement for Pediatric Cardiac Care
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1143-018
STANDARDIZING THE CARE OF OUTPATIENT PEDIATRIC SYNCOPE AND DIZZINESS: A LESSON IN UTILIZATION AND CHARGE REDUCTION
Christopher Statile, Samuel Hanke, Richard Czosek, Enisa Handlon, James Brown, Amy Donnellan and Jeffrey Anderson
vol. 69 no. 11 Supplement 613
DOI:
https://doi.org/10.1016/S0735-1097(17)34002-0
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Christopher Statile,
- Samuel Hanke,
- Richard Czosek,
- Enisa Handlon,
- James Brown,
- Amy Donnellan and
- Jeffrey Anderson
- Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA
Background: Variability in medical practice is associated with higher cost without improved outcome. Our aim was to standardize the evaluation and treatment of dizziness/syncope and track resultant cost savings.
Methods: A multidisciplinary team developed a care algorithm using best evidence and expert consensus for evaluation of otherwise healthy pediatric patients with dizziness or syncope. Quality improvement methods guided acceptance and implementation of the algorithm into our cardiology clinics. Primary outcome measure was weekly mean charge per patient, primarily driven by the number of cardiac tests ordered. Total charges were compared using patient billing data. Statistical process control charts evaluated the system over time. Baseline data (11/2015-3/2016) were collected and data were monitored after implementation of the algorithm through 8/2016.
Results: There were 104 patients identified during the baseline period: median age 14.3 years (2.9-8.4), with 9 patients (9%) <8 years; 64% female; 82% Caucasian. After algorithm implementation, there were 279 patients evaluated: median age 15 years (1.4-19), with 27 patients (10%) <8 years; 63% female; 85% Caucasian. There was a dramatic shift in mean charge per patient from $1,784 to $1,098 (Figure), driven primarily by reduction in testing beyond an electrocardiogram.
Conclusions: Standardization of evaluation for pediatric patients presenting with dizziness/syncope resulted in a significant charge decrease for our patients.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Congenital Heart Disease: Advances in Quality Improvement for Pediatric Cardiac Care
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1143-019
MAKING PERIOPERATIVE HANDOFF COMMUNICATION COUNT BY IMPROVING SAFETY AND QUALITY IN A NEW CONGENITAL HEART PROGRAM
Pooja Nawathe, Nicole Berndsen, Veena Sivarajan, Vincent Olshove, Ken Catchpole and Alistair Phillips
vol. 69 no. 11 Supplement 614
DOI:
https://doi.org/10.1016/S0735-1097(17)34003-2
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Pooja Nawathe,
- Nicole Berndsen,
- Veena Sivarajan,
- Vincent Olshove,
- Ken Catchpole and
- Alistair Phillips
- Cedars Sinai Medical Center, Los Angeles, CA, USA
Background: Coordination among units, staff and equipment for a congenital cardiac surgical patient requires a strategic process. Structured handoff processes enhance teamwork, communication and patient outcomes. Transitioning patients from the operating room (OR) to the congenital cardiac intensive care unit (CCICU) is a critical time to relay what transpired during the peri-operative course. The handoff process was developed for seamless communication, and enhancement of coordination of care amongst the team.
Methods: This was a prospective, interrupted time series observational study, in the CCICU. Two observers evaluated handoff process based on occurrence, flow and clinical disruptions. Flow and clinical disruptions include 5 different categories scored zero to five. Clinically significant events were evaluated at 6 and 24 hours.
Results: The study included 29 patients. Two defined groups were used, Group 1 (Gp1); n=16 prior to establishing a handoff process and Group 2 (Gp2); n=13 after the establishment of the handoff process. Completion of handoff was significantly less in Gp2 (mean 23.5 mins ±8, median 20 min), vs. Gp1 (mean 33.5±14, median 32.5). Flow disruptions showed no significant difference although cut in half (mean Gp1=1.5, mean Gp2= 0.8, p= 0.12). With the handoff process in place, treatment errors 6 hours post-operatively had a significant reduction (mean Gp1= 0.8, mean Gp2= 0.2, p= 0.02). Disruption in handoff occurred frequently due to equipment problems in both groups (Gp1 43.8%, Gp2 38.5%), while logistical problems reduced in Gp2 (Gp1 50%, Gp2 0%). There was enhanced handoff use (31.3% vs. 7.7%), decreased hemodynamic instability at 6 hours post-operatively (18.8% vs. 0%), reduction in drug errors (12.5% vs.7.7%).
Conclusions: By using quality improvement methodology to design and implement a new direct OR-CCICU structured multidisciplinary verbal handoff, we achieved improvements in patient safety and efficiency. Handoff communication was enhanced, with fewer errors and content omissions. The new process improved communication and goal alignment amongst the team members.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Congenital Heart Disease: Advances in Quality Improvement for Pediatric Cardiac Care
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1143-020
TREATMENT OF CONGENITAL CORONARY FISTULA
Fabiola Sozzi, Nicolas Hugues, Laura Iacuzio, Francois Bourlon, Filippo Civaia, Gilles Dreyfus and Vincent Dor
vol. 69 no. 11 Supplement 615
DOI:
https://doi.org/10.1016/S0735-1097(17)34004-4
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Fabiola Sozzia,b,
- Nicolas Huguesa,b,
- Laura Iacuzioa,b,
- Francois Bourlona,b,
- Filippo Civaiaa,b,
- Gilles Dreyfusa,b and
- Vincent Dora,b
- aCardiothoracic Centre, Montecarlo, Monaco
- bOspedale Maggiore Policlinico, Milan, Italy
Background: Congenital coronary artery fistulas (CAF) with significant clinical impact are extremely rare vascular anomalies. Little data are available.
Aim: To determine the outcome of percutaneous closure of large hemodynamically significant CAF in young patients.
Methods: We retrospectively analysed 11 patients (median age at intervention 21 years, 3 females) affected by relevant congenital CAF, diagnosed by echocardiogram and cardiac catheterization. All patients underwent percutaneous closure and were followed for a mean period of 3 years.
Results: The clinical presentation of CAF was characterized by symptoms in 7/11 cases. In the other 4 cases CAF was incidentally diagnosed by echocardiogram. In most cases the fistulas were originating from the left coronary artery (LCA) [7/11]. The right heart was the most common site of drainage (8/11). Multiple fistulas were found in 3 patients. No-one had other congenital disorders associated. All patients were treated with percutaneous transcatheter embolization. During follow-up, no patient died. In 1 case a retrograde thrombosis of the fistula with acute myocardial infarction occurred after 1 month and was treated with thrombectomy and coronary bypass. No other major adverse cardiac events were recorded.
Conclusions: Percutaneous closure of significant coronary fistulas is associated with low event-rate and excellent prognosis.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Innovations in Pediatric Catheterization and EP: Mending, Fixing and Predicting
- Abstract Category: 11. Congenital Heart Disease: Therapy
- Presentation Number: 1144-021
PERCUTANEOUS PATENT FORAMEN OVALE CLOSURE BENEFIT: IS RIGHT PATIENT SELECTION THE ANSWER?
Luis Almeida-Morais, Lidia Sousa, Antonio Fiarresga, Ana T. Timoteo, Jose Diogo Martins, Filipa Ferreira, Jose Alberto Oliveira, Cristina Soares, Ana Agapito, Fatima Pinto and Rui Ferreira
vol. 69 no. 11 Supplement 616
DOI:
https://doi.org/10.1016/S0735-1097(17)34005-6
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Luis Almeida-Morais,
- Lidia Sousa,
- Antonio Fiarresga,
- Ana T. Timoteo,
- Jose Diogo Martins,
- Filipa Ferreira,
- Jose Alberto Oliveira,
- Cristina Soares,
- Ana Agapito,
- Fatima Pinto and
- Rui Ferreira
- Centro Universitário de Cardiologia, Hospital de Santa Marta, Lisbon, Portugal
Background: Patent foramen ovale (PFO) closure global benefits for cryptogenic stroke secondary prevention remain controversial. The Risk of Paradoxical Embolism (RoPE) study developed a score to improve patient selection. It’s our purpose to assess the validity of this score to predict long-term outcomes.
Methods: From 2000-2014, all consecutive patients submitted to percutaneous PFO closure were included in a prospective registry in a university centre. The primary endpoint was ischemic cerebral events (ICE) recurrence and secondary endpoints were all cause mortality and new onset atrial fibrillation (AF).
Results: 403 patients were submitted to PFO closure (females 52.1%, mean age 44.7±10.9 yo). Mean follow-up: 6.4±3.7 years. Immediate success: 97%. 8 deaths, 23 ICE and 17 new onset AF cases were reported. Smoking (OR 3.3, 95% CI 1.2-8.5, p=0.014), coronary disease (CD) (OR 6.7, 95% CI 1.9-23.1, p=0.003), low RoPE score (≤6) (OR 6.5, 95% CI 1.5-28.2, p=0.012) and left atrial dimension (OR 1.1, 95%CI 1.0-1.2, p=0.037) were predictors of primary endpoint. After multivariate analysis, low RoPE score (OR 5.6, 95% CI 1.3-24.5, p=0.024) and CD (OR 7.7, 95% CI 1.9-30.3, p=0.033) remained independent predictors. All cause mortality and new onset AF were significantly higher in the low RoPE score group (p<0.05).
Conclusions: RoPE score was shown to be an independent long-term predictor of ICE recurrence and a score ≤6 identifies patients with significantly higher mortality and ischemic events recurrence risk.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Innovations in Pediatric Catheterization and EP: Mending, Fixing and Predicting
- Abstract Category: 11. Congenital Heart Disease: Therapy
- Presentation Number: 1144-022
OUTCOME OF PREOPERATIVE ELECTROPHYSIOLOGY STUDY IN PATIENTS WITH EBSTEIN ANOMALY
Alexander C. Egbe, Vidhushei Yogeswaran and Heidi Connolly
vol. 69 no. 11 Supplement 617
DOI:
https://doi.org/10.1016/S0735-1097(17)34006-8
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Alexander C. Egbe,
- Vidhushei Yogeswaran and
- Heidi Connolly
- Mayo Clinic, Rochester, MN, USA
Background: There are limited data about outcomes of preoperative electrophysiology studies (EPS) in patients with Ebstein Anomaly.
Methods: This is a descriptive study of all adults (>18 years) that underwent preoperative EPS at Mayo Clinic, 2000-2014. Data from clinic notes, EPS, and surgical notes were reviewed. Study objective was to determine outcomes of preoperative EPS in this population.
Results: Preoperative EPS were performed in 41 patients; mean age 43±15 year, males 23 (56%). All had a history of palpitations; 12/41 (29%) had a prior cardiac surgery, and 9 of which were tricuspid valve (TV) surgeries. A documented arrhythmia was present in 29/41 (71%), and these arrhythmias were atrial flutter in 4, atrial fibrillation in 1, ectopic atrial tachycardia (EAT) in 2, Wolf Parkinson White syndrome in 14, and other types of supraventricular tachycardia in 8.
Catheter ablation was performed at the time of EPS in 13/41 (32%), and these ablations were for EAT in 2, atrial flutter in 4, accessory pathway mediated tachycardia in 8, and slow pathway modification in 4. All patients underwent surgery (TV repair n=29 and TV replacement n=12), and there was 1 perioperative death. Concomitant surgical arrhythmia procedures were performed in 32/41 (78%) and these procedures were right atrial maze in 25; biatrial maze in 6; and division of accessory pathway in 1. Antiarrhythmic drugs and anticoagulation were discontinued after 3 months postoperative in 31 patients.
Follow-up data were available in 38, and arrhythmia recurrence (AR) occurred in 14/38 patients (37%) within 49±14months of follow-up. Freedom from AR was 78% at 36 months, and there was no difference between the catheter ablation group vs the arrhythmia surgery group, 77% vs 78%, P=.65.
Conclusions: Outcomes of catheter ablation during preoperative EPS was comparable to surgical arrhythmia therapy on mid-term follow-up. A larger cohort with a control arm will be required to evaluate the role of preoperative EPS in this population.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Innovations in Pediatric Catheterization and EP: Mending, Fixing and Predicting
- Abstract Category: 11. Congenital Heart Disease: Therapy
- Presentation Number: 1144-023
DUCTAL ORIGIN OF AN ISOLATED PULMONARY ARTERY: INITIAL STENTING FOLLOWED BY UNIFOCALIZATION
Navaneetha Sasikumar, Kyong-Jin Lee, Lee Benson and Rajiv Chaturvedi
vol. 69 no. 11 Supplement 618
DOI:
https://doi.org/10.1016/S0735-1097(17)34007-X
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Navaneetha Sasikumar,
- Kyong-Jin Lee,
- Lee Benson and
- Rajiv Chaturvedi
- The Hospital for Sick Children, Toronto, Canada
Background: Primary surgical repair of an isolated pulmonary artery can be difficult because of the small vessel and reperfusion pulmonary edema. We evaluated a strategy of primary stenting of the ductal origin of the pulmonary artery followed by later complete repair.
Methods: Retrospective analysis of patients identified from the interventional and surgical databases between 2001 and 2016. Data are presented as median (range), unless otherwise stated.
Results: Twenty-one ducts were stented in 19 patients [age: 13 (2-997) days, weight: 5.98(3.6-13.3) kg]. Ten patients were receiving prostaglandins. Sixteen ducts arose from the innominate artery contralateral to the side of the aortic arch. Ducts required 1 (n=15), 2 (n=4) or 3 (n=2) stents, with 23% deployed by an antegrade approach. Pulmonary edema developed in 53%. ICU and hospital stays were 1 (0-110) days and 4 (1-110) days, respectively. Early in the series, one patient died in the first 24 hours from unrecognized pulmonary overcirculation. Three patients required balloon dilation of the stent prior to surgery. The pulmonary artery distal to the stented duct grew, z-score (mean ± sd): −1.79 ± 1.4 (pre-stent) to −0.71 ± 1.1 (pre-surgery), p=0.02. Surgical unifocalization has been completed in 15 without mortality, 117 (40-210) days after stenting. Post-operatively 5/15 patients required re-interventions.
Conclusions: Ductal stenting secured blood flow to the isolated pulmonary artery without bypass and allowed pulmonary artery growth prior to complete surgical repair. Close monitoring is required for pulmonary edema and high pulmonary blood flow in the first 24 hours after stenting.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Friday, March 17, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Innovations in Pediatric Catheterization and EP: Mending, Fixing and Predicting
- Abstract Category: 11. Congenital Heart Disease: Therapy
- Presentation Number: 1144-024
HYPOPLASTIC LEFT HEART SYNDROME WITH INTACT OR RESTRICTIVE ATRIAL SEPTUM:WHAT HAPPENS AFTER SURVIVAL?
Brian Snarr, Michael Liu, Benjamin Zielonka and Jack Rychik
vol. 69 no. 11 Supplement 619
DOI:
https://doi.org/10.1016/S0735-1097(17)34008-1
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Brian Snarr,
- Michael Liu,
- Benjamin Zielonka and
- Jack Rychik
- The Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Background: Hypoplastic left heart syndrome (HLHS) with intact or restrictive atrial septum (IRAS) represents a subset of patients with single ventricle cardiac disease (SVCD) associated with higher mortality. In recent years, management strategies have been developed for catheter-based creation of an inter-atrial communication in the prenatal or immediate postnatal period. Despite these advances, mortality still remains high. For those who survive, little is known about the long term morbidity and overall outcome. We sought to characterize the long-term outcome for those who underwent fetal or postnatal catheter-based intervention for IRAS.
Methods: We performed a retrospective study reviewing all patients presenting to our center with a prenatal diagnosis of HLHS or other SVCD between 2004 and 2012. Those with HLHS or other right-dominant SVCD with IRAS who received either prenatal or immediate postnatal catheter-based intervention upon their atrial septum were identified. This cohort was followed longitudinally to death or 6 months post-Fontan and outcomes were characterized.
Results: Nearly 500 patients with HLHS or SVCD were identified. Among those, 19 patients underwent fetal (2) or immediate postnatal (17) catheter-based intervention. There were 10 patients (53%) that survived to 6 months post-Fontan. Gestational age, birth weight, fetal AV valve regurgitation and fetal ventricular function were not found to be significantly different from non-survivors. Compared to survivors without IRAS, there was no significant difference in length of stay (LOS) from birth to discharge, or combined total LOS through 6 months post-Fontan.
Conclusions: The mortality for patients with IRAS undergoing catheter-based intervention still remains high with only 50% survival. Prenatal variables such as ventricular function and AV valve regurgitation were not found to be significant risk factors associated with survival. Once patients survive, however, their overall hospital course through Fontan palliation does not appear to be significantly different from their non-IRAS counterparts.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Congenital Heart Disease: Innovations in Single Ventricle Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1182-009
RIGHT VENTRICULAR REMODELLING IN HYPOPLASTIC LEFT HEART SYNDROME: IMPACT OF THE NORWOOD AND HYBRID PROCEDURES
Kandice Mah, Jesus Serrano Lomelin, Luke Eckersley, Lily Lin, Timothy Colen, Edythe Tham, Harald Becher, Luc Mertens and Nee Scze Khoo
vol. 69 no. 11 Supplement 620
DOI:
https://doi.org/10.1016/S0735-1097(17)34009-3
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Kandice Maha,b,
- Jesus Serrano Lomelina,b,
- Luke Eckersleya,b,
- Lily Lina,b,
- Timothy Colena,b,
- Edythe Thama,b,
- Harald Bechera,b,
- Luc Mertensa,b and
- Nee Scze Khooa,b
- aStollery Children’s Hospital, Edmonton, Canada
- bSickkids, Toronto, Canada
Background: Right ventricular (RV) remodeling in hypoplastic left heart syndrome (HLHS) begins prenatally and continues through staged palliations. The impact of cardiopulmonary bypass (CPB) timing on HLHS RV remodeling, early in Norwood-Sano vs. later in Hybrid palliation, is unclear.
Methods: Echocardiograms of HLHS patients undergoing stage-1 Norwood or Hybrid (Jan 2007 – Dec 2011) were longitudinally analyzed at Pre & Post-stage 1, Pre & Post-Glenn, and Pre-Fontan. We assessed RV fractional area change (FAC), vector velocity imaging for longitudinal & derived circumferential deformation (peak radial displacement/end-diastolic diameter), and deformation ratio (longitudinal/circumferential). Generalized Estimation Equations assessed temporal changes for each group and compared the interventions for each parameter. Independent T-test assessed outcomes.
Results: Hybrids (n=20) and Norwoods (n=27) had similar age, clinical status and echocardiogram parameters Pre-stage 1. Longitudinal analysis showed FAC was unchanged in Norwoods, while Hybrids decreased Pre-Glenn (p = 0.03) with return to baseline Pre-Fontan. Post stage 1, Norwoods increased circumferential and decreased longitudinal deformation (p<0.05), with a further increase in circumferential deformation Post-Glenn. Hybrids Post-stage 1 (no CPB) had similar change in contraction pattern, however circumferential deformation returned to baseline Pre-Glenn while longitudinal strain rate remained reduced (p<0.0001). Post-Glenn, Hybrids (after exposure to their first, and longer CPB), showed a decrease in both circumferential and longitudinal deformation (p<0.05). Comparing between interventions, Norwoods had greater circumferential (p<0.05) but similar longitudinal deformation post-stage 1 and Pre-Glenn. No other differences were found Post-Glenn including early clinical outcomes.
Conclusions: HLHS Hybrids had similar change in RV contraction pattern as Norwoods post stage-1, suggesting inherent RV remodeling during early adaptation to single ventricle physiology. CPB at Norwood appears to modify this process by increasing reliance on RV circumferential contraction to maintain function.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Congenital Heart Disease: Innovations in Single Ventricle Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1182-010
IS A PULSATILE GLENN AN ADEQUATE ALTERNATIVE FOR LONG-TERM PALLIATION IN PATIENTS WITH SINGLE VENTRICLE PHYSIOLOGY?
Carlos M. Mery, Martin A. Chacon-Portillo, Huirong Zhu, Heather Dickerson, Iki Adachi, Jeffrey Heinle, Lauren Kane, Emmett McKenzie and Charles Fraser
vol. 69 no. 11 Supplement 621
DOI:
https://doi.org/10.1016/S0735-1097(17)34010-X
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Carlos M. Mery,
- Martin A. Chacon-Portillo,
- Huirong Zhu,
- Heather Dickerson,
- Iki Adachi,
- Jeffrey Heinle,
- Lauren Kane,
- Emmett McKenzie and
- Charles Fraser
- Texas Children’s Hospital, Baylor College of Medicine, Houston, TX, USA
Background: There are limited studies analyzing pulsatile Glenns (PG) as a palliation strategy for complex single ventricle (SV) patients. This study sought to determine their outcomes at a single institution.
Methods: All SV pts who underwent PG from 1995-2016 were included. Failure was defined as takedown, transplant or death. Further palliation (FP) was defined as Fontan, 1.5 or biventricular repair. Risk factors were assessed by Cox multivariable competing risk analyses.
Results: 78 pts underwent PG at age 8.8 mos (86 days – 14 yrs). 28% had heterotaxy, 19% had genetic syndrome, 23% had abnormal inferior vena cava. There were 3 operative mortalities (4%). FP was performed in 40 pts (51%), 3 were 1.5 and one was biventricular repair [time-to-palliation 4 yrs (2-10)]. PG failure occurred in 9 pts (12%) with 7 total mortalities. 5- and 10-year overall survival was 90% and 86%. At median follow-up 6 yrs (1 mo-13 yrs), 29 pts (37%) remained with PG (age 7 yrs [7 mos-18 yrs], oxygen saturation 84% [74-90]). Preop moderate or severe atrioventricular valve regurgitation (AVVR) was predictor of PG failure (HR 6.1, 1.4-27.5). Reaching FP was less likely with AVVR (HR 0.2, 0.1-0.7) and heterotaxy or genetic syndrome (HR 0.5, 0.27-0.94).
Conclusions: Complex SV pts palliated with PG have a favorable long-term prognosis without reducing their suitability for FP, while delaying the consequences of a Fontan circulation. In some pts, PG is a suitable alternative to Fontan palliation, allowing some to reach adolescence.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Congenital Heart Disease: Innovations in Single Ventricle Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1182-011
DETECTION OF HEART FAILURE WITH PRESERVED EJECTION FRACTION IN SINGLE VENTRICLE PHYSIOLOGY: INSIGHTS FROM THE PEDIATRIC HEART NETWORK FONTAN CROSS-SECTIONAL STUDY PUBLIC USE DATASET
Shahryar Chowdhury, Eric Graham, Carolyn Taylor, Geoffrey Forbus, Andrew Savage and Andrew Atz
vol. 69 no. 11 Supplement 623
DOI:
https://doi.org/10.1016/S0735-1097(17)34012-3
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Shahryar Chowdhury,
- Eric Graham,
- Carolyn Taylor,
- Geoffrey Forbus,
- Andrew Savage and
- Andrew Atz
- Medical University of South Carolina, Charleston, SC, USA
Introduction: Patients with single ventricle physiology frequently demonstrate decreased exercise tolerance after the Fontan operation. The objective of this study was to investigate the contribution of diastolic function to exercise function in these patients.
Methods: Core-lab echocardiograms and exercise test results were obtained from the publically-available Pediatric Heart Network Fontan Cross-sectional Study database. Exercise function was quantified as % predicted peak VO2. Ejection fraction (EF) was considered abnormal if < 50%. End-diastolic volume (EDV) was indexed to body surface area1.4. Diastolic function was defined as abnormal lateral E:e’/EDV was > 10th percentile. Patients were divided into three groups: 1 = normal EF and normal diastolic function, 2 = normal EF with abnormal diastolic function, and 3 = decreased EF with normal diastolic function. There were an inadequate number of patients with both abnormal EF and diastolic dysfunction to be included in the analysis.
Results: 185 patients (61% left, 29% right, 10% mixed ventricular dominance) had EF, lateral E:e’/EDV, and peak VO2measured. Differences between groups are reported in the Table.
Conclusions: Single ventricle patients with abnormal diastolic function and preserved EF had worse exercise capacity than patients with both normal and abnormal EF. Diastolic dysfunction appears to be an important limitation to exercise function in this population. Echocardiography may be useful in detecting this subset of patients.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Congenital Heart Disease: Innovations in Single Ventricle Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1182-013
ASSOCIATION OF INCREASED TOTAL ATRIAL VOLUME WITH CLINICAL HEART FAILURE STATUS IN HYPOPLASTIC LEFT HEART SYNDROME
Angela Kelle, Govinda Paudel, Muhammad Qureshi, Megan O’Byrne and Patrick O’Leary
vol. 69 no. 11 Supplement 624
DOI:
https://doi.org/10.1016/S0735-1097(17)34013-5
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online December 1, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Angela Kelle,
- Govinda Paudel,
- Muhammad Qureshi,
- Megan O’Byrne and
- Patrick O’Leary
- Mayo Clinic, Rochester, MN, USA
Background: Increased left atrial volume predicts mortality in adults with heart failure (HF). Implications of increased atrial volume in complex congenital heart disease are less well understood. We sought to determine if increased atrial volume is associated with clinical HF in hypoplastic left heart syndrome (HLHS).
Methods: Subjects in a prospective HLHS research program were classified as having no HF or clinical HF [NYHA class ≥3, growth failure, cardiomegaly (cardiothoracic ratio >0.6 on X-ray), or hepatomegaly (edge >2.5 cm below costal margin)]. Atrial volumes were measured by transthoracic echocardiogram (TTE) at end systole by area-length method and indexed to body surface area.
Results: Criteria for HF were met in 16/75 clinic visits [(21%); 6/18 post stage 2 palliation (pre-Fontan) and 10/57 post Fontan completion]. In the entire cohort, those with HF had ∼50% greater RA volume (p = 0.04). Pre-Fontan subgroup analysis showed association between all atrial volumes and HF; total atrial volume index (RAV + LAV) >43 ml/m2predicted clinical HF with 86% sensitivity and 80% specificity. Post-Fontan, no association was seen between total atrial volume and HF status.
Conclusions: Total atrial volume by TTE in pre-Fontan HLHS patients is a marker of clinical HF, with volume index >43/m2 predicting HF status with good sensitivity and specificity. Atrial volumes are less closely associated with HF post Fontan, likely secondary to multiple factors (sample heterogeneity, altered RA compliance/geometry).
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Congenital Heart Disease: Innovations in Single Ventricle Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1182-014
DOES TRICUSPID ANNULAR PLANE SYSTOLIC EXCURSION (TAPSE) ADEQUATELY DESCRIBE RIGHT VENTRICULAR FUNCTION IN HYPOPLASTIC LEFT HEART SYNDROME?
Ololade Akintoye, Curtis Travers, William Border, Christopher J. Petit, Erik Michelfelder and Ritu Sachdeva
vol. 69 no. 11 Supplement 625
DOI:
https://doi.org/10.1016/S0735-1097(17)34014-7
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Ololade Akintoyea,b,
- Curtis Traversa,b,
- William Bordera,b,
- Christopher J. Petita,b,
- Erik Michelfeldera,b and
- Ritu Sachdevaa,b
- aEmory University School of Medicine, Atlanta, GA, USA
- bChildren’s Health Care of Atlanta, Atlanta, GA, USA
Background: The role of tricuspid annular plane systolic excursion (TAPSE) in evaluating right ventricular (RV) function in hypoplastic left heart syndrome (HLHS) has not been fully explored. We sought to evaluate the relation between TAPSE and RV fractional area change (FAC) and cardiac index (CI) during the inter-stage period.
Methods: TAPSE and FAC measured within7 days of pre-Glenn catheterization from Dec 2008 to Mar 2016 were analyzed. TAPSE z-score was calculated using published normal values for structurally normal hearts. Normal RV systolic function was defined as FAC ≥ 40%. TAPSE was correlated with FAC and CI derived by Fick.
Results: Among 86 subjects, patient characteristics, TAPSE, and TAPSE aged- based z-score were similar between those with normal (N = 55) and reduced (N = 31) RV function (Table). There was no significant correlation between FAC and TAPSE or TAPSE z-score (r=0.13, 0.08, respectively). The TAPSE z-score in those with normal FAC was lower than structurally normal hearts (μ = −3.97, p < 0.001). In those with simultaneous cardiac catheterization (N = 36), there was no significant correlation between either TAPSE and CI (r=0.26, p = 0.121) or RVFAC and CI (r = 0.30, p = 0.073).
Conclusions: In HLHS, TAPSE was significantly lower than normal values even in those with normal FAC. Lack of correlation with FAC suggests that TAPSE does not fully describe global RV function. Neither TAPSE nor FAC correlated with CI, and are likely too simplistic to describe ventricular-vascular interactions.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Congenital Heart Disease: Innovations in Single Ventricle Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1182-015
IMPACT OF HOME MONITORING PROGRAM ON INTERSTAGE MORTALITY AND STAGE II OUTCOMES
Monique Gardner, Laura Mercer-Rosa, Katherine Bates, Alyson Stagg, Shobha Natarajan, Anita Szwast, Jessica (Jie) Tang, Stephanie Fuller, Christopher Mascio, Desiree Fleck, Deborah L. Torowicz, Therese Giglia, Jonathan Rome and Chitra Ravishankar
vol. 69 no. 11 Supplement 626
DOI:
https://doi.org/10.1016/S0735-1097(17)34015-9
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Monique Gardner,
- Laura Mercer-Rosa,
- Katherine Bates,
- Alyson Stagg,
- Shobha Natarajan,
- Anita Szwast,
- Jessica (Jie) Tang,
- Stephanie Fuller,
- Christopher Mascio,
- Desiree Fleck,
- Deborah L. Torowicz,
- Therese Giglia,
- Jonathan Rome and
- Chitra Ravishankar
- Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Introduction: In shunt dependent single ventricle (SV) patients, mortality remains high in the interstage (IS) period between discharge after neonatal surgery and stage II. Conflicting reports exist regarding the impact of monitoring programs on IS mortality. We sought to evaluate the impact of a single center’s Infant Single Ventricle Management and Monitoring Program (ISVMP) on IS mortality and stage II outcomes.
Methods: In this retrospective cohort study, we compared contemporary patients enrolled in the ISVMP with historical controls. We excluded patients who were not discharged (6 ISVMP, 8 controls) or died after neonatal surgery (22 ISVMP, 19 controls). Mortality was compared using logistic regression analysis and survival curves using log rank test.
Results: Our cohort included 168 subjects in ISVMP (2011-2015) and 171 controls (2007-2010). Hypoplastic left heart syndrome (HLHS) was present in 49% ISVMP and 51% controls. The two groups did not differ by anatomy, gender, race, or presence of genetic syndrome. There was a reduction in IS mortality in the ISVMP subjects (8/168, 4.8%) versus controls (21/171, 12.3%) (OR 0.36, p=0.02). When limited to those with HLHS, the odds of death remained 3 times as high for controls (p=0.03). Even though subjects in ISVMP underwent stage II earlier (median 138, IQR 126-161 days) versus controls (161, IQR 135-188 days, p=<0.001), lower mortality in ISVMP was not simply attributable to shorter IS period. Survival curve comparison by log rank revealed a hazard ratio of 2.73 (95% CI 1.21; 6.17) in control versus ISVMP (p=0.02). After stage II, there was no difference between ISVMP and controls in mortality (1.9% vs. 3.3%, p=0.44), length of stay (median 7 days for both groups, p=0.37) and rate of re-operation (1.8% vs. 1.2%, p=0.64).
Conclusions: In our study, implementation of the ISVMP improved IS survival in shunt dependent SV patients and this difference is not simply a function of a shorter IS period. Younger age at stage II did not affect postoperative mortality or morbidity. Further analysis is underway to evaluate factors that affect IS mortality and stage II outcomes, and to assess additional outcomes including growth, resource utilization, and late mortality.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Congenital Heart Disease: Innovations in Single Ventricle Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1182-016
STANDARDIZATION OF PERI-OPERATIVE MANAGEMENT AFTER NORWOOD OPERATION HAS NOT IMPROVED 1 YEAR OUTCOMES
Shilpa Shah, Steven Schwartz, Andrew Goodwin, Osami Honjo, Glen Van Arsdell, Mike Seed, Jennifer Russell and Alejandro Floh
vol. 69 no. 11 Supplement 627
DOI:
https://doi.org/10.1016/S0735-1097(17)34016-0
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 30, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Shilpa Shah,
- Steven Schwartz,
- Andrew Goodwin,
- Osami Honjo,
- Glen Van Arsdell,
- Mike Seed,
- Jennifer Russell and
- Alejandro Floh
- Hospital for Sick Children, Toronto, Canada
Background: In efforts to improve survival following the stage 1 Norwood operation, our institution adopted a comprehensive treatment approach that included standardization of surgery, perioperative management, and a dedicated interstage home surveillance program. We hypothesized this would improve one-year survival with preserved ventricular function (VF) and atrio-ventricular valve function (AVVF) in patients undergoing the Norwood operation.
Methods: This retrospective cohort study compared patients who underwent stage 1 palliation October 2012-January 2015 (Group 1) with historical (Group 2) controls. Patients’ clinical status was extracted from the medical record. VF and AVVF were determined from echocardiograms closest to one year of age. VF was preserved if normal or mildly reduced and AVVF if mildly regurgitant or better. The primary outcome was transplant-free survival with preserved ventricular function (VF) and AVV function at 1 year.
Results: 69 patients (27 Group 1, 42 Group 2) were included. More group 1 patients had diagnosed extracardiac syndromes (5% vs 22%, p=0.05). At stage 1, group 1 had longer circulatory arrest times (26 vs 19 min p=0.02), decreased 14-day freedom from open chest (6.3 vs 8.6 days, p=0.01), and a decrease in 100 hospital-free days (40 vs 55 days p=0.01). Group 1 had a trend toward higher transplant-free survival at stage 2 (85% vs 73%, p=0.25). At 1 year follow-up (median 14 months, IQR 11-18), there was no significant difference in transplant-free survival (70.4% vs 64%, p=0.6) or transplant-free survival with preserved VF and AVVF (55% vs 52%; group 1 vs 2; p=0.627). Of survivors without preserved VF/AVVF, 83% had moderate or severe AVVR and 16% had moderate ventricular dysfunction. Regression analysis demonstrated that shorter duration of open chest (p=0.01) and inclusion in group 1 (p=0.04) were predictors of good VF/AVVF at 1 year.
Conclusions: Implementation of a structured comprehensive management strategy was not associated with improved transplant-free survival at one year, with or without preserved VF and AVVF. A paradigm shift in treatment strategy is required to improve long term survival in this vulnerable population.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Congenital Heart Disease: Innovations in Single Ventricle Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1182-017
INTERSTAGE RESOURCE UTILIZATION OF INFANTS WITH SINGLE VENTRICLE: RESULTS OF A CROSSOVER STUDY
Lori Erickson, Kimberly Reid, Amy Ricketts, Bryan Beaven, Suma Goudar, Amy Lay, Richard Stroup, James O’Brien and Girish Shirali
vol. 69 no. 11 Supplement 628
DOI:
https://doi.org/10.1016/S0735-1097(17)34017-2
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Lori Erickson,
- Kimberly Reid,
- Amy Ricketts,
- Bryan Beaven,
- Suma Goudar,
- Amy Lay,
- Richard Stroup,
- James O’Brienand
- Girish Shirali
- Children’s Mercy Kansas City, Kansas City, MO, USA
Background: Since 2014, we have monitored interstage infants with single ventricle (SV) at home with CHAMP, a tablet PC with cloud-based instant analytic algorithms. This study identifies predictors of high resource utilization (HRU) readmissions.
Methods: From 5/14 to 6/15, SV infants were enrolled in a crossover study comparing traditional binder to CHAMP. All were discharged with the binder; they were randomized to receive CHAMP instead of binder 1 or 2 months after discharge. One month after randomization, caregivers chose either binder or CHAMP for the remainder of the interstage. Charts were reviewed for neonatal characteristics, readmission data including events prior to readmission, length of stay (LOS), ICU LOS and charges. High resource utilization (HRU) were defined as the 25% of readmissions that were associated with the greatest ICU LOS, and were compared to all others (Low resource utilization (LRU)).
Results: 31 infants were monitored for 4911 interstage days. There were no interstage deaths and 73 readmissions. HRU did not differ from LRU in neonatal characteristics (Table). HRU were significantly more likely to be unplanned, at a younger age, and associated with a longer delay from clinical change to readmission. HRU had higher charges, LOS, and more cardiac and general surgeries.
Conclusions: Interstage SV infants are at high risk for readmissions. Delays in care are associated with HRU; CHAMP may help decrease delays. This study may provide the basis for predictive analytic algorithms.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Congenital Heart Disease: Innovations in Single Ventricle Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1182-018
FROM FETUS TO FONTAN: A SINGLE CENTER EXPERIENCE OF RESOURCE UTILIZATION FOR PATIENTS DIAGNOSED WITH SINGLE VENTRICLE CARDIAC DEFECTS
Benjamin Zielonka, Michael Liu, Brian Snarr, Xuemei Zhang and Jack Rychik
vol. 69 no. 11 Supplement 629
DOI:
https://doi.org/10.1016/S0735-1097(17)34018-4
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Benjamin Zielonka,
- Michael Liu,
- Brian Snarr,
- Xuemei Zhang and
- Jack Rychik
- The Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Background: Single ventricle cardiac defects (SVCD) require the highest neonatal expenditures of any congenital birth defect. Advances in prenatal diagnosis have facilitated prenatal and perinatal management of SVCD, but little is known about the total resources required to care for a patient from fetal diagnosis through Fontan palliation (FP). We sought to characterize the resource utilization for patients with SVCD from fetal diagnosis through death, complete staged palliation, or transplant.
Methods: We reviewed patients with a prenatal diagnosis of SVCD from 2004-2012. Only patients delivered with intent to treat who received cardiac care exclusively at our institution were included. Patients undergoing staged repair were followed until death or 6 months post-FP. Transplant recipients and patients who did not complete FP at the time of data collection were censored at 3.43 years. Primary endpoints included the total number of days hospitalized, number of echocardiograms, and total cardiac catheterizations, expressed in patient-years. The resource utilization of patients who survived and died during the period of staged repair were then compared using negative binomial regression.
Results: A cohort of 204 patients met inclusion criteria. 154 (75.5%) patients survived and 50 (24.5%) died during the study period. The median duration of follow-up was 3.23 years. The median days hospitalized per patient-year was 23.24. The median number of echocardiograms and catheterizations per patient-year was 6.70 and 0.76 respectively. Death during staged repair was associated with a greater resource burden. Patients who died spent more days hospitalized per patient-year (332.09 vs. 16.51; p<.0001), and had more echocardiograms (51.06 vs. 5.75; p<.0001) and catheterizations per patient-year (3.94 vs. 0.66; p<.0001).
Conclusions: Our study quantifies the specific resources used from fetal diagnosis through the period of staged repair. Mortality during staged repair was associated with disproportionate resource utilization. Further investigation into prenatal determinants of resource utilization will enable more comprehensive counseling for expectant families of patients with SVCD.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Congenital Heart Disease: Innovations in Single Ventricle Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1182-019
PREVALENCE OF ELEVATED BODY MASS INDEX AND ITS ASSOCIATION WITH CLINICAL FEATURES IN ADULT FONTAN PATIENTS
Anushree Agarwal, Aarthi Sabanayagam, Ahmed Kheiwa, Colin Cunnington, Lucas Zier, Charles McCulloch, Ian Harris, Elyse Foster, Dougal Atkinson, Angela Bryan, Petra Jenkins, Jaspal Dua, Michael Parker, Devinda Karunaratne, John A. Moore, Jeffery Meadows, Bernard Clarke, J. Andreas Hoschtitzky and Vaikom Mahadevan
vol. 69 no. 11 Supplement 631
DOI:
https://doi.org/10.1016/S0735-1097(17)34020-2
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Anushree Agarwala,b,
- Aarthi Sabanayagama,b,
- Ahmed Kheiwaa,b,
- Colin Cunningtona,b,
- Lucas Ziera,b,
- Charles McCullocha,b,
- Ian Harrisa,b,
- Elyse Fostera,b,
- Dougal Atkinsona,b,
- Angela Bryana,b,
- Petra Jenkinsa,b,
- Jaspal Duaa,b,
- Michael Parkera,b,
- Devinda Karunaratnea,b,
- John A. Moorea,b,
- Jeffery Meadowsa,b,
- Bernard Clarkea,b,
- J. Andreas Hoschtitzkya,b and
- Vaikom Mahadevana,b
- aUniversity of California San Francisco, San Francisco, CA, USA
- bManchester Royal Infirmary, Central Manchester University Hospitals NHS Trust, Central Manchester, United Kingdom
Background: Elevated body mass index (BMI) is increasingly affecting adults with congenital heart disease. The effect of an increased BMI with respect to clinical variables has not been evaluated in adult Fontan patients.
Methods: Retrospective review of medical records from 2 tertiary academic institutions identified 68 Fontan patients ≥ 18 years for whom BMI data was available.
Results: Mean BMI was 24±4 kg/m2 with 6% being underweight (BMI <18.5), 54% normal (18.5 – <25), 31% overweight (25 – <30) and 9% obese (≥ 30). Patients with BMI ≥ 25 kg/m2 were significantly older (34 ± 9 vs. 31 ± 7 yrs, p=0.03), had higher Fontan (16 ± 3 vs.14 ± 6 mm Hg, p=0.04) and pulmonary capillary wedge pressures (PCWP, 12 ± 3 vs. 9 ± 3 mm Hg, p=0.03) and lower peak oxygen consumption (VO2, 18±5 vs. 22±4 ml/Kg/min, p=0.005), minute ventilation (Ve, 44 ± 10 vs. 58 ± 21 L/min, p=0.03) and Ve/Vco2, (33 ± 7 vs. 36 ± 4, p=0.03) on cardiopulmonary exercise testing (CPET). There were no differences in gender, Fontan type, ventricular type and function, arrhythmia burden, New York Heart Association status, other echocardiographic, hemodynamic or CPET variables. Linear regression graph showed a linear correlation between BMI and the significant clinical variables (Figure).
Conclusions: Overweight/obesity is highly prevalent in adult Fontan patients. Higher BMI is associated with poor hemodynamics and aerobic capacity. This might correlate with worse health outcomes in this patient population, although further study is needed to determine this.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Fontan in the Modern World
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1183-021
MACITENTAN USE AS SERIAL THERAPY IN FAILING FONTAN PHYSIOLOGY
Tabitha Grace Moe
vol. 69 no. 11 Supplement 632
DOI:
https://doi.org/10.1016/S0735-1097(17)34021-4
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Tabitha Grace Moe
- Phoenix Children’s Hospital, Phoenix, AZ, USA
Background: Single ventricle terminal palliation with a completed cavopulmonary anastomosis is well understood to case myriad comorbidities including Fontan associated liver disease, systemic systolic ventricular failure, and protein losing enteropathy with accompanying ascites. The presence of elevated pressures within the cavopulmonary circuit logically precipitates sequelae. The first sign of which may be a reduction in exercise tolerance.
Methods: We evaluated 6 patients in a single-center with elevated pressures (defined as >15 mmHg) who had previously been on a stable dose of sildenafil 20mg by mouth three times daily with new initiation of macitentan 10mg daily. They were followed for a minimum of 6 months following initiation of therapy.
Results: 4 patients improved their baseline 6 minute walk duration by 20% (>80m) over the course of 6 month follow up. 2 patients had decreased frequency of the need of abdominal paracentesis to > 1 month intervals, and albumin levels increased in each of these patients. No patients reported significant side effects.
Conclusions: This small pilot study is suggestive that serial addition of macitentan to sildenafil in patients with Fontan physiology and elevated Fontan pressures is safe, and in some cases helpful. More study is needed to determine longer term benefits including delay and reversal of hepatic fibrosis and congestive hepatic hepatopathy as well as improvement in exercise tolerance.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Fontan in the Modern World
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1183-022
TOWARDS A BETTER PREDICTIVE MODEL OF ADVERSE EVENTS IN ADULT FONTAN PATIENTS
- Abigail Simmons, Wendy Book, Kayoko Shioda, Makoto Mori and Robert Elder
vol. 69 no. 11 Supplement 633
DOI:
https://doi.org/10.1016/S0735-1097(17)34022-6
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- aYale University School of Medicine, New Haven, CT, USA
- bEmory University School of Medicine, Atlanta, GA, USA
Background: The Fontan palliation causes chronic hepatic congestion and carries a risk of late-adverse cardiac events. VAST and Model for End-stage Liver Disease eXcluding INR (MELD-XI) scores are validated risk-assessment tools in this group. This study investigates whether a combination of these clinical (VAST) and lab-based models (MELD-XI) would improve prediction of adverse cardiac events in Fontan patients.
Methods: Retrospective, two-center study of adult Fontan patients between 2001-16. Adverse events were defined as cardiac death/heart transplantation. VAST score (1 point each Varices, Ascites, Splenomegaly and Thrombocytopenia, range 0-4), MELD-XI score [11.76 (loge creatinine) + 5.112 (loge total bilirubin) + 9.44] and combined M-VAST score (range 0-5), for which a MELD-XI ≥13 was counted as a +1 to VAST score, were compared as predictors of adverse events using receiver operating characteristics (ROC) analysis. Optimal cut-off points were identified using Yoden index. Scores were calculated at a period of outpatient stability. Non-event cohort was censored at last clinical evaluation.
Results: VAST and MELD-XI scores were available in 160 adult patients. After a mean follow-up of 22 yrs, 23 (14%) experienced an adverse event. The event cohort was older (38.7 ±10.3 vs. 31.6 ±8.0 years, p=0.0049), had higher VAST scores (2.2 ±1.2 vs. 0.8 +/-1.0, p<0.0001) and higher MELD-XI scores (12.5 ±3.3 vs. 11.1 ±2.3, p=0.049) compared to non-event cohort. ROC curve for VAST alone as a predictor of adverse events yielded an AUC of 0.80 with the optimal cutoff of ≥2. ROC curve for MELD-XI score yielded an AUC of 0.66 with the optimal cutoff of ≥13. ROC curve for the M-VAST score yielded an improved AUC of 0.82 with the optimal cutoff of M-VAST ≥2. Compared to VAST alone, M-VAST improved sensitivity from 0.70 to 0.78 but decreased specificity from 0.79 to 0.72. Kaplan-Meier analysis with strata divided at M-VAST ≥2 demonstrated improved event free survival of the lower score strata (log rank =0.0002).
Conclusions: Incorporating a MELD-XI into the VAST score, thus combining laboratory and clinical variables, improves the ability to predict death and cardiac transplant in adult Fontan patients.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Fontan in the Modern World
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1183-023
CARDIOPULMONARY EXERCISE TEST IN ADULTS WITH PRIOR FONTAN OPERATION: THE PROGNOSTIC VALUE OF SERIAL TESTING
Alexander C. Egbe and Heidi Connolly
vol. 69 no. 11 Supplement 634
DOI:
https://doi.org/10.1016/S0735-1097(17)34023-8
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Alexander C. Egbe and
- Heidi Connolly
- Mayo Clinic, Rochester, MN, USA
Background: There are limited data about the prognostic valve of cardiopulmonary exercise test (CPET) in adults with prior Fontan operation.
Methods: Retrospective review of adults with prior Fontan operation who had treadmill CPET at Mayo Clinic, 1994-2013. The study objective was to determine the role of CPET indices in predicting cardiovascular adverse events (CAE) defined as death, cardiac surgery or transcatheter interventions.
Patients with loss of follow-up defined as ≥2 years without clinical follow-up were excluded. The results of serial CPETs were reviewed, and patients with CPETs meeting the following criteria were selected for analysis: maximum effort on serial CPETs, minimum of 3-year interval between CPETs, and absence of CAE between CPETs.
Results: 145 patients met inclusion criteria for the study; mean age at baseline CPET was 24±3 years; mean age at Fontan operation was 11±5 years; and 91 (63%) were males.
Baseline peak oxygen consumption (VO2) was 22.7±5.4 ml/kg/min (63±11% predicted), peak heart rate was 135±31 beats per minute, and oxygen saturation at peak exercise was 86±7%. Serial CPETs were performed in 71/145 patients (49%); mean duration between CPETs was 3.8±0.3 years. The % predicted peak VO2 decreased by 1.7±0.9 percentage points/year.
CAE (deaths n=22; cardiac surgery n=45; transcatheter interventions n=38) occurred in 69/145 patients (48%) within 8±3 years. Decline in % predicted peak VO2 ≥3 percentage point/year was the only predictor of 5-year risk of CAE (HR 2.79, 95% CI 1.37-3.21, P=.01).
Conclusions: Serial CPET is prognostic of CAE in the adult Fontan population, and can be used to risk stratify these patients.
Legend: Kaplan-Meier curves comparing freedom from CAE for patients with decline in %predicted peak VO2 ≥3 percentage point/year (blue) vs those with decline in %predicted peak VO2 <3 percentage point/year (red). The second CPET marks the beginning of time zero (at risk period).
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Fontan in the Modern World
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1183-024
UTILITY OF GENETIC TESTING IN INFANTS WITH ISOLATED CONGENITAL HEART DISEASE
Kaitlin L’Italien, Sara Fitzgerald-Butt, Janet Simsic, Kim McBride, Jessica Bowman and Vidu Garg
vol. 69 no. 11 Supplement 635
DOI:
https://doi.org/10.1016/S0735-1097(17)34024-X
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Kaitlin L’Italien,
- Sara Fitzgerald-Butt,
- Janet Simsic,
- Kim McBride,
- Jessica Bowman and
- Vidu Garg
- Nationwide Children’s Hospital, Columbus, OH, USA
Background: Recent advances in technology, and a greater demonstration of the genetic contributors to congenital heart disease (CHD), have resulted in an expansion of genetic screening among infants with CHD. However, the utility of this screening strategy has not been well studied. We aimed to determine the incidence of pathogenic genetic findings in isolated vs non-isolated CHD answering the question “whom should we test, and which test should we send?
Methods: A retrospective review analyzing infants less than 1 year of age with CHD admitted to our cardiac ICU (January 2010 -December 2014) was performed. Patients who had renal/head ultrasounds and genetic testing (karyotype, FISH, or chromosomal microarray (CMA)) were divided into high and low risk groups. The high risk group included those with additional malformations, family history (FH) of CHD, or CHD known to be of high risk for genetic syndromes (i.e. conotruncal heart disease). Patients with isolated CHD were considered low risk.
Results: Of 446 patients who met study criteria, 278 were considered high risk, while 168 were low risk. A pathogenic finding was identified in 134 of 278 (48%) high risk patients. Only 5 of 168 (2.9%) low risk patients were found to have a pathogenic finding (negative predictive value (NPV) =97%). Of patients who had a karyotype performed, 96 (54.8%) of the high risk patients (n=176) had abnormal karyotype versus none of the 76 low risk patients (NPV=100%). In patients who had CMA, 29 of 157 (18.5%) high risk patients had pathogenic findings vs 5 of 145 (3.4%) low risk patients (NPV=96.5%). The 5 abnormalities found in low risk patients were not known genetic syndromes and did not affect management in infancy.
Conclusions: Analysis of one of the largest CHD populations using modern genetic testing methods, we found a high rate of pathogenic genetic abnormalities in patients with CHD and additional malformations, positive FH, or CHD subtypes associated with genetic syndromes. Thus, karyotype and CMA testing of these high risk infants appears to be of high yield. We found a low rate of pathogenic findings in isolated CHD suggesting that testing during early infancy may not be indicated, and required only if additional concerns arise.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Congenital Heart Disease: New Diagnostic Approaches in Congenital Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1231-009
EXOME SEQUENCING REVEALS NOVEL VARIANTS IN TMEM59L AND KLHL26 ASSOCIATED WITH A FAMILIAL CASE OF EBSTEIN’S ANOMALY AND LEFT VENTRICULAR NONCOMPACTION
Lauren North, Donna Mahnke, Karl Stamm, Huan Ling Liang, Richard J. Willes, Michele Frommelt, Michael Mitchell and Aoy Tomita-Mitchell
vol. 69 no. 11 Supplement 636
DOI:
https://doi.org/10.1016/S0735-1097(17)34025-1
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Lauren Northa,b,
- Donna Mahnkea,b,
- Karl Stamma,b,
- Huan Ling Lianga,b,
- Richard J. Willesa,b,
- Michele Frommelta,b,
- Michael Mitchella,b and
- Aoy Tomita-Mitchella,b
- aMedical College of Wisconsin, Milwaukee, WI, USA
- bChildren’s Hospital of Wisconsin, Milwaukee, WI, USA
Background: Ebstein’s Anomaly (EA) is a complex congenital heart defect (CHD) of the tricuspid valve that has significant morbidity and mortality. Most cases are of sporadic origin, however several familial cases have been described. It has been associated with myosin heavy chain 7 (MYH7), transcription factor NKX2.5, and recently, alpha-tropomyosin (TPM1). Our study describes a family spanning three generations with six members affected by EA.
Methods: Echocardiography was performed to characterize cardiac anatomy. Whole exome sequencing (WES) was performed on five family members: three affected and two unaffected. INDEL and SNP variants were detected and annotated. Genetic variants were filtered for rarity (≤1% Exome Variant Server, NHLBI GO Exome Sequencing Project), predicted deleterious/damaging effect, and observed expression and/or association with cardiac or muscle development. Variants were further evaluated with Sanger Sequencing in all family members (n=12) to determine inheritance pattern.
Results: Our investigation revealed six family members with EA, of which all also had left ventricular noncompaction (LVNC) and three also had atrial septal defect (ASD). Additionally, there were two non-viable pregnancies due to known CHD detected prenatally. WES and Sanger sequencing revealed neighboring variants on KLHL26 and TMEM59L, both located on chromosome 19, which followed an autosomal dominant inheritance pattern in coordination with EA phenotype (p<0.05 Fisher exact test).
Conclusions: Never before has such a large familial study of Ebstein’s Anomaly occurring with Left Ventricular Noncompaction been described. Through WES we have identified two rare variants in KLHL26 and TMEM59L that segregate with EA. Multiple family members affected by EA were found to also have LVNC, which supports reports in the literature of these two phenotypes occurring together. The ability to genetically characterize this family will aid in future diagnosis and management of multiple family members. Our approach validates the importance of translational research in medicine when approaching complex diseases.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Congenital Heart Disease: New Diagnostic Approaches in Congenital Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1231-010
MODIFIED NEWBORN PULSE OXIMETRY SCREENING FOR OUT-OF-HOSPITAL BIRTHS
Devyani Chowdhury and Katie Williams
vol. 69 no. 11 Supplement 637
DOI:
https://doi.org/10.1016/S0735-1097(17)34026-3
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- aCardiology Care for Children, Lancaster, PA, USA
- bClinic for Special Children, Strasburgh, PA, USA
Background: Newborn pulse oximetry screening at 24-48 hours of life is recommended to detect critical congenital heart disease (CCHD), but cyanosis can also be due to pulmonary pathology and neonatal infections. Infants born out of hospital often lack a prenatal assessment with ultrasound, have variable rates of maternal GBS testing, and are typically observed only for a few hours after delivery, necessitating a modified pulse oximetry screening protocol.
Methods: Infants had pulse oximetry screening at 1-3 hours of life (“early screen”) and again at 24-48 hours (“standard screen”) by trained midwives. Midwives were provided training and reliable pulse oximeters (Massimo) to perform the screening. The current AAP-endorsed algorithm for interpreting results was used at both screenings. Midwives followed infants for at least 6 weeks to identify any missed cardiopulmonary pathology or infectious illnesses.
Results: 399 term infants (52% male, average weight 8.0 ± 1 pounds) were screened following parental consent. Prenatal ultrasound was completed for 45% of infants with no CHD identified. 65% of mothers were tested for GBS colonization and 22% of those tested were positive. Early and standard screens were performed and interpreted correctly for 74% and 79% percent of infants, respectively. The early screen identified one newborn with CHD (0.25% positive rate). An additional infant with CHD was identified due to inability to obtain a reliable reading at the early screen and murmur and poor feeding at standard screen. One newborn failed the standard screen but further evaluation was deferred and the infant remained well (false positive rate 0.25%). At 6 week follow up no additional cardiopulmonary pathology or infections were detected in the cohort.
Conclusions: Preliminary data suggest a combined early and standard newborn pulse oximetry screen can be implemented to detect CHD in out of hospital births with a low false positive rate. Midwives have varied levels of education and training therefore may have a learning curve to implement the protocol accurately. Ongoing study will determine if this is an effective “wellness screen” to detect any additional pulmonary pathology and neonatal infections.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Congenital Heart Disease: New Diagnostic Approaches in Congenital Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1231-011
VARIATION IN PRENATAL DIAGNOSIS OF CONGENITAL HEART DEFECTS IN A POPULATION-BASED STUDY IN SOUTHERN CHINA
Yanqiu Ou, Jian Zhuang and Xiaoqing Liu
vol. 69 no. 11 Supplement 638
DOI:
https://doi.org/10.1016/S0735-1097(17)34027-5
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- aGuangdong Cardiovascular Institute, Guangzhou, People’s Republic of China
- bGuangdong General Hospital, Guangdong Academy of Medical Sciences, Guangzhou, People’s Republic of China
Background: Variability in prenatal diagnosis for congenital heart defect (CHD) has been documented in other countries, but has not been examined in detail across China. This study was aimed to evaluate prenatal diagnosis rate (PDR) in stillbirths and livebirths with CHD in southern China.
Methods: This population-based study enrolled all fetuses and infants with CHD included in the Guangdong Registry of CHD (2004-2014). We analyzed PDR according to the type of defect and geographic region. Defects were classified in hierarchical fashion into 1) “primary targets” for screening, including the seven categories of CHD that usually present in newborns with hypoxemia; 2) “secondary targets” for screening, including another seven types of CHD that sometimes present with hypoxemia; 3) minor defects, including other specified defects.
Results: We identified 9877 babies from 39 sites in 20 cities across southern China. The PDR for total CHD, primary and secondary targets was 22%, 57% and 74%, respectively. The three lesions diagnosed most frequently were severe pulmonary stenosis, double outlet right ventricle and hypoplastic left heart syndrome. Total anomalous pulmonary venous connection presented with the least PDR among critical CHDs. The PDR in primary and secondary targets increased every year, specifically, from 25% (2004) to 70% (2014). There was significant geographic variation in PDR across the province (range 0% – 44%, P < 0.001). Factors associated with increased PDR included lesions co-existing with extra-cardiac or chromosomal defects, increased complexity, identifiable on 4-chamber view and maternal residence in developed regions. More than 80% stillbirths with primary and secondly targets were diagnosed prenatally.
Conclusions: There is significant variability in the rates of prenatal diagnosis for critical CHD in southern China related to defect type and region. The findings raise concern for improving fetal imaging and referral protocols, population access to care, and developing fetal intervention to prevent death in utero.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Congenital Heart Disease: New Diagnostic Approaches in Congenital Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1231-012
IMPACT OF MATERNAL DIABETES ON FIRST & EARLY SECOND TRIMESTER FETAL CARDIOVASCULAR HEALTH
Dora Gyenes, Jesus Serrano-Lomelin, Venu Jain, Claudine Bohun, Winnie Savard, Angela McBrien and Lisa Hornberger
vol. 69 no. 11 Supplement 639
DOI:
https://doi.org/10.1016/S0735-1097(17)34028-7
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Dora Gyenes,
- Jesus Serrano-Lomelin,
- Venu Jain,
- Claudine Bohun,
- Winnie Savard,
- Angela McBrien and
- Lisa Hornberger
- University of Alberta, Edmonton, Canada
Background: Maternal diabetes mellitus (DM), which affects 6-7% of pregnancies, is associated with fetal myocardial hypertrophy and altered diastolic function later in gestation, but its impact on the fetal heart earlier in gestation has received minimal attention. We sought to determine if maternal DM impacts fetal heart function at 8-15 weeks of gestation and to elucidate the role of maternal glycemic control.
Methods: Pregnancies complicated by DM and gestational age-matched healthy controls (1 DM: 2 controls) were prospectively recruited to undergo early fetal echocardiography. Pulsed Doppler-derived parameters of left (LV) and right ventricular function and the fetal circulation were compared between the groups. Maternal hemoglobin A1C values at <12 weeks gestation were collected.
Results: In total, 45 DM and 90 control pregnancies were studied (mean gestational age 12.4±1.5 weeks for both). The LV Tei index was significantly increased in fetuses of DM pregnancies (DM 0.52±0.14 vs control 0.43±0.11, p<0.001)(Figure). Other functional parameters did not differ between the groups, and A1C did not correlate with any functional parameter in our DM cohort.
Conclusions: Our pilot study suggests that maternal DM impacts global LV function of the 8-15 week fetus. Lack of correlation with maternal A1C suggests either a more complex relationship between maternal glucose control and fetal cardiac function or the presence of co-existing factors in the DM pregnancy.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Congenital Heart Disease: New Diagnostic Approaches in Congenital Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1231-013
THE INCREMENTAL BENEFIT OF COLOR TISSUE DOPPLER IMAGING IN FETAL RHYTHM ASSESSMENT
Silvia Alvarez, Paul Brooks, Nee Scze Khoo, Timothy Colen and Lisa Hornberger
vol. 69 no. 11 Supplement 640
DOI:
https://doi.org/10.1016/S0735-1097(17)34029-9
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Silvia Alvarez,
- Paul Brooks,
- Nee Scze Khoo,
- Timothy Colen and
- Lisa Hornberger
- Stollery Children’s Hospital, Edmonton, Canada
Background: Accurate fetal arrhythmia diagnosis is key for effective management. Traditional echo-based techniques used in fetal arrhythmia (FA) assessment (M mode and PW Doppler) require adequate fetal position and cursor alignment to define temporal relationships between atrial (A) and ventricular (V) events. Whether color tissue Doppler imaging (TDI) facilitates FA diagnosis and is of added value to standard techniques has not been fully explored.
Methods: We prospectively recruited 34 pregnant women diagnosed with FA to undergo color TDI following fetal echo assessment. Multiple beat TDI clips of the 4-chamber in any orientation were recorded (Frame rate ≥ 180fps). Observer was blinded to outcome. Sample-volumes were placed on atrial and ventricular wall to display simultaneous trace of A and V activity. Timing of cardiac cycle events were supplemented by frame-by-frame analysis of the 2D image, including AV valve closure. Intervals A-A, V-V, A-V and V-A were measured with high temporal resolution from the color TDI dataset tracing.
Results: Thirty-two of 34 pregnancies with FA were captured on TDI with most diagnosis made within 5 minutes of analysis. FA include: 17 tachycardias (2 atrial flutter, 10 ectopic atrial tachycardia, 3 AV re-entry tachycardia, 2 ventricular tachycardia); 6 bradycardias (3 complete AV block (AVB), 2-1° AVB including 1 evolving to 2° and 3° AVB, 1 sinus bradycardia); 9 with ectopic beats (7 atrial, 2 ventricular). All FA diagnosis by TDI concurred with the primary diagnosis by standard techniques. Thirteen (40%) FA had additional findings on TDI, including demonstrating 2° AVB instead of atrial bigeminy with block, more than one type of ectopy and intermittent V-A conduction in ventricular tachycardia. TDI was most helpful in supraventricular tachycardia with consistent evaluation of A-V and V-A intervals and the changing relationship of A and V rates facilitating mechanism assessment in 7 (47%) in whom standard techniques could not.
Conclusions: Color TDI with offline analysis permits rapid and accurate definition of FA mechanism and provides new information in a substantial proportion (40%) of affected pregnancies.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Congenital Heart Disease: New Diagnostic Approaches in Congenital Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1231-014
LEFT ATRIAL STIFFNESS: A NEW NONINVASIVE INDEX THAT MAY SERVE AS A SURROGATE MARKER OF LEFT VENTRICULAR DIASTOLIC DYSFUNCTION IN CHILDREN
Jeremy Zuckerberg, Michael Quartermain, Stanford Ewing and Anirban Banerjee
vol. 69 no. 11 Supplement 641
DOI:
https://doi.org/10.1016/S0735-1097(17)34030-5
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Jeremy Zuckerberg,
- Michael Quartermain,
- Stanford Ewing and
- Anirban Banerjee
- University of Pennsylvania School of Medicine, Philadelphia, PA, USA
Background: Guidelines for evaluating left ventricular (LV) diastolic dysfunction in adults, often do not apply in children. We hypothesize left atrial (LA) stiffness may serve as a noninvasive surrogate of LV diastolic dysfunction in children with cardiomyopathy (CMP).
Methods: We studied 41 CMP patients (ages 0.4-18yrs) with dilated (n=21), hypertrophic (n=13) and restrictive (n=7) types. These CMP patients also had elevated PCWP >13mmHg noted at cardiac catheterization. Patients with normal PCWP (<12mmHg), who underwent catheterization for small patent ductus arteriosus (n=14), mild coarctation (n=9), pulmonary stenosis (n=8) or Kawasaki disease (n=3) with no LV hypertrophy or dilatation and normal LV function, served as controls (ages 0.5-22yrs). LA peak strain was measured by speckle tracking echocardiography and E/e’ recorded from apical 4-chamber views. LA stiffness=E/e’÷Peak LA strain (%-1).
Results: In CMP group, PCWP was significantly higher (19.0±4.9 vs 8.9±2.0mmHg, p<0.01), LA strain was significantly decreased (16.9±12.0 vs 52.2±22.8%, p<0.01) and LA stiffness was significantly increased (1.4±1.3 vs 0.13±0.11%-1, p<0.01). From receiver operator characteristic curves, cutoff value for LA stiffness was 0.27%-1 (Fig. 1), sensitivity 100% & specificity 94%.
Conclusions: LA stiffness was significantly increased and yielded a distinct cutoff value in pediatric CMP with elevated PCWP. LA stiffness may serve as surrogate of elevated PCWP and LV diastolic dysfunction in children.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Congenital Heart Disease: New Diagnostic Approaches in Congenital Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1231-015
RIGHT VENTRICULAR CONTRACTILE RESERVE IS REDUCED IN CHILDREN AND ADOLESCENTS WITH TETRALOGY OF FALLOT: A STRESS ECHOCARDIOGRAPHIC STUDY
Shivani M. Bhatt, Elizabeth Goldmuntz, Okan Elci, Michael McBride, Stephen Paridon and Laura Mercer-Rosa
vol. 69 no. 11 Supplement 642
DOI:
https://doi.org/10.1016/S0735-1097(17)34031-7
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Shivani M. Bhatt,
- Elizabeth Goldmuntz,
- Okan Elci,
- Michael McBride,
- Stephen Paridon and
- Laura Mercer-Rosa
- The Children’s Hospital of Philadelphia, Philadelphia, PA, USA
Background: Pulmonary insufficiency (PI) and right ventricular (RV) dysfunction are long-term complications in repaired tetralogy of Fallot (rTOF). We sought to investigate changes in PI and RV function that occur with exercise in this patient population.
Methods: Subjects with rTOF presenting for cardiopulmonary exercise test underwent rest and peak exercise echocardiograms. RV contractile reserve was defined as the change in RV global longitudinal strain from rest to peak exercise. PI was assessed with the diastolic to systolic time velocity integral ratio (DSTVI) from Doppler interrogation in the pulmonary artery. Exercise measures included the percent-predicted maximal oxygen consumption (%mVO2), maximum work, and oxygen pulse.
Results: We enrolled 32 patients (age 16.4 ± 4.9 years, 66% male). RV strain was diminished at rest and decreased further at peak exercise (reduced contractile reserve). At peak exercise, the DSTVI decreased, indicating an improvement in PI. This decrease was associated with better maximum work and greater oxygen pulse. A decrease in the diastolic/systolic velocity ratio correlated with better %mVO2. Contractile reserve was not associated with exercise parameters. (Table)
Conclusions: Patients with rTOF have abnormal response to exercise with reduced contractile reserve. The association of reduced PI with superior exercise performance, independent of contractile reserve, warrants further study to understand the diastolic contribution to exercise in rTOF.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Congenital Heart Disease: New Diagnostic Approaches in Congenital Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1231-016
MITRAL VALVE PHASE CONTRAST IMAGING IS A MORE REPRODUCIBLE METHOD OF DETERMINING CARDIAC REST PERIODS FOR WHOLE-HEART CORONARY MAGNETIC RESONANCE ANGIOGRAPHY IN CONGENITAL HEART DISEASE THAN 4 CHAMBER CINE
Maria Batsis, Gerald Greil, Animesh Tandon and Tarique Hussain
vol. 69 no. 11 Supplement 643
DOI:
https://doi.org/10.1016/S0735-1097(17)34032-9
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 30, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Maria Batsis,
- Gerald Greil,
- Animesh Tandon and
- Tarique Hussain
- University of Texas Southwestern Medical Center, Dallas, TX, USA
Background: Whole heart coronary magnetic resonance angiography (CMRA) offers detailed cardiac morphology in congenital heart disease (CHD). This imaging is performed during the cardiac rest periods. These are assessed visually using a high-temporal resolution, 4-chamber (4CH) cine. We evaluated the reproducibility of this measurement compared to a novel approach using mitral valve inflow phase contrast (MVIPC) imaging.
Methods: Consecutive patients with CHD undergoing CMRA who had both 4CH & MVIPC at 60 phases were retrospectively evaluated. Two independent observers evaluated the end-systolic & mid-diastolic intervals with both methods (Figure 1). Inter- & intra-observer variability for each method were scored, as well as CMRA quality (Scale 1 to 4; with 4 representing best quality). A linear mixed-effect model was used to compare variability between the methods & account for patient random effects & for within-patient variability.
Results: CMRAs of 25 patients were analyzed (mean age 14.76±6.3 years). The MVIPC method showed that inter-observer variability was 5.4% lower (95% CI 3.7,7.2%, p<0.0001) than the 4CH & intra-observer variability was 3.9% lower (95% CI 2.4,5.4%, p<0.0001). The time taken to determine the rest periods was equal for both methods (4CH 57.6±26.0 sec, MVIPC 52.5±36.3 sec, p=0.4). Image quality scores were comparable to the published literature (median= 3, IQR 3-4).
Conclusions: MVIPC is as fast but more reproducible than 4CH for defining cardiac rest periods for CMRA in CHD.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Congenital Heart Disease: New Diagnostic Approaches in Congenital Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1231-017
SHORT AXIS DIASTOLIC VENTRICULAR AREA RATIO AS A NEW INDEX IN SCREENING PATIENTS WITH REPAIRED TETRALOGY OF FALLOT
Dala Zakaria, Sean Lang, Elijah Bolin, Jeffrey Gossett, Mallikarjuna Rao Rettiganti and Thomas Collins
vol. 69 no. 11 Supplement 644
DOI:
https://doi.org/10.1016/S0735-1097(17)34033-0
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Dala Zakaria,
- Sean Lang,
- Elijah Bolin,
- Jeffrey Gossett,
- Mallikarjuna Rao Rettiganti and
- Thomas Collins
- University of Arkansas for Medical Sciences, Little Rock, AR, USA
Background: Right ventricular (RV) end-diastolic volume measured by cardiovascular magnetic resonance imaging (CMR) is a criterion for pulmonary valve replacement in patients with tetralogy of Fallot (TOF). We sought to assess the ability of the ratio of echocardiographic, short-axis right and left ventricular end-diastolic area in predicting RV volume on CMR.
Methods: We retrospectively reviewed the echocardiograms of all patients with TOF who underwent CMR at our institution from 2011-2015 and also had an echocardiogram within 6 months of the CMR. The short-axis RV and left ventricular (LV) end-diastolic areas (EDA) were measured and the ratio of the two was calculated. Results were compared with CMR RV end-diastolic volume index (RVEDVi) and RV/LV end-diastolic volume ratio. The sensitivity and specificity values predicting RV volumes >150 ml/m2 were calculated.
Results: Sixty-six patients met inclusion criteria. There were 54 patients with RVEDVi <150 ml/m2 and 12 with RVEDVi >150 ml/m2. RV: LV EDA and CMR RV: LV end-diastolic volume ratio correlated strongly (r= 0.76, p<0.0001). An RV: LV EDA ≥1.88 had an 81% specificity to detect RV volume index >150 ml/m2. An RV: LV EDA ≥1.57 had 90% sensitivity to predict RVEDVi >150 ml/m2 (area under the curve=0.74, confidence interval, 1.5-27.9; p=0.012).
Conclusions: Short-axis RV: LV EDA correlates well with RV volume as measured by CMR. This new measure can be used to predict optimal timing for CMR in anticipation of surgical repair.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Congenital Heart Disease: New Diagnostic Approaches in Congenital Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1231-018
FEASIBILITY OF RAPIDLY CREATING HIGH RESOLUTION VIRTUAL THREE-DIMENSIONAL MODELS OF ANOMALOUS AORTIC ORIGIN OF CORONARY ARTERIES
Kelly Nicol, Anthony Costa, Shubhika Srivastava and Santosh Uppu
vol. 69 no. 11 Supplement 645
DOI:
https://doi.org/10.1016/S0735-1097(17)34034-2
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Kelly Nicol,
- Anthony Costa,
- Shubhika Srivastava and
- Santosh Uppu
- Mount Sinai School of Medicine, New York, NY, USA
Background: Morphological criteria that result in inducible ischemia with anomalous aortic origin of coronary artery (AAOCA) have been postulated but not confirmed. Computational fluid dynamics (CFD), finite element analysis (FEA) on virtual AAOCA three-dimensional models (3DM) could elucidate the mechanism of flow alteration. Our objective is to test feasibility creating 3DM of various AAOCA’s and usable mesh for simulation analysis.
Methods: Data from CT angiograms (voxel size 0.6-0.9 mm) was transferred to Seg3D2 to be resampled and to isolate the AAOCA. Median filtering was used to remove noise while preserving edge integrity, followed by Otsu thresholding for segmentation and labeling of the AAOCA. Extraneous portions were manually deleted before application of a connected component filter. Final label maps (voxel size 0.2 mm) were transformed into mesh-based models with the marching cubes technique. Meshlab was used for visualization of the coronary ostia and course.
Results: Twelve 3DM & mesh models were successfully created using our method, visualization of the ostia and proximal intramural course was possible in these models (figure). This process took about 20 minutes each.
Conclusions: Rapid high resolution 3DM and usable mesh of AAOCA for simulation analysis using traditional cardiac CT data is feasible using our methods. This technique will lay the foundation for CFD and simulation of inducible ischemia using FEA analysis.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Congenital Heart Disease: New Diagnostic Approaches in Congenital Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1231-019
CARDIOVASCULAR HEALTH OF OFFSPRING OF DIABETIC MOTHERS FROM THE FETUS THROUGH LATE INFANCY STAGES
Victor Do, Tina Ojala, Timothy Colen, Silvia Goncalvez-Alvarez, Sandra Davidge, Jesus Serrano-Lomelin and Lisa Hornberger
vol. 69 no. 11 Supplement 646
DOI:
https://doi.org/10.1016/S0735-1097(17)34035-4
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Victor Do,
- Tina Ojala,
- Timothy Colen,
- Silvia Goncalvez-Alvarez,
- Sandra Davidge,
- Jesus Serrano-Lomelin and
- Lisa Hornberger
- University of Alberta, Edmonton, Canada
Background: Infants of diabetic mothers (IDMs) develop left ventricular(LV) hypertrophy and mild diastolic dysfunction prenatally, and are at increased risk of adult cardiovascular disease(CVD). Whether fetal changes truly resolve or persist, contributing to long-term CVD has not been explored. The aims of our study were to determine if IDMs have myocardial hypertrophy and diastolic dysfunction in late infancy, have increased aortic stiffness, and if cardiovascular pathology of IDMs is associated with worse maternal glycemic control.
Methods: We longitudinally investigated myocardial and vascular health by echocardiography in offspring of pregestational DM pregnancies both prenatally (3 each, 20-40 weeks) and in infancy (2-6 weeks & 6-12 months). We compared LV posterior(LVPW) and septal(IVS) wall thickness, systolic and diastolic function and aortic stiffness (pulse wave velocity, PWV) between IDMs and pre and postnatal age-matched controls from healthy pregnancies, and collected maternal A1c values.
Results: 36 IDMs and 36 controls were prospectively recruited. Increased LVPW and IVS was present in DM fetuses from the midtrimester that persisted through both early and late infancy (p<0.01, all ages). Although increased LV Tei index was present in late gestation in IDMs, and mild diastolic pathology in early infancy, by late infancy LV function was comparable to controls. PWV was increased in late infancy in IDMs (3.7+/-1.2 vs 2.2+/-0.5m/s, p <0.01) which correlated with LVPW and IVS (R2 0.82 & 0.87, respectively, p <0.05). Late infancy PWV also correlated with 3rdtrimester A1c (R2 = 0.83, p<0.05), but LVPW and IVS did not. Systolic and diastolic blood pressure did not differ between groups.
Conclusions: IDMs display persistence of LV hypertrophy through late infancy. Aortic stiffness is increased in IDMs in late infancy which relates to late gestation maternal glycemic control.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Congenital Heart Disease: New Diagnostic Approaches in Congenital Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1231-020
LONG-TERM CARDIOVASCULAR OUTCOMES IN PATIENTS WITH ANOMALOUS CORONARY ARTERIES WISUALIZED BY CORONARY CT ANGIOGRAPHY: THE CONFIRM (CORONARY CT ANGIOGRAPHY EVALUATION FOR CLINICAL OUTCOMES: AN INTERNATIONAL MULTICENTER) REGISTRY
Subhi Al’Aref, Khalil Anchouche, Ashley Beecy, Heidi Gransar, Briain O. Hartaigh, Mahn Won Park, Asim Rizvi, Ji Hyun Lee, Donghee Han, Hadi Mirhedayati Roudsari, Daniel Berman, Tracy Callister, Augustin DeLago, Martin Hadamitzky, Joerg Hausleiter, Mouaz Al-Mallah, Matthew Budoff, Philipp Kaufmann, Gilbert Raff, Kavitha Chinnaiyan, Filippo Cademartiri, Erica Maffei, Todd Villines, Yong-Jin Kim and on behalf of the CONFIRM Investigators
vol. 69 no. 11 Supplement 647
DOI:
https://doi.org/10.1016/S0735-1097(17)34036-6
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Subhi Al’Aref,
- Khalil Anchouche,
- Ashley Beecy,
- Heidi Gransar,
- Briain O. Hartaigh,
- Mahn Won Park,
- Asim Rizvi,
- Ji Hyun Lee,
- Donghee Han,
- Hadi Mirhedayati Roudsari,
- Daniel Berman,
- Tracy Callister,
- Augustin DeLago,
- Martin Hadamitzky,
- Joerg Hausleiter,
- Mouaz Al-Mallah,
- Matthew Budoff,
- Philipp Kaufmann,
- Gilbert Raff,
- Kavitha Chinnaiyan,
- Filippo Cademartiri,
- Erica Maffei,
- Todd Villines,
- Yong-Jin Kim,
- on behalf of the CONFIRM Investigators
- Weill Cornell Medical College, New York, NY, USA
Background: Anomalous origin of coronary arteries (ACA) in young adults are thought to confer high mortality risk, but the clinical significance of incidentally discovered anomalous coronaries in middle-aged adults is not well characterized. We examined the clinical characteristics and 5-year outcomes of patients with ACA by Coronary CT Angiography (CCTA).
Methods: From a total of 12,086 patients enrolled in the long-term CONFIRM registry, 79 had ACA. These patients were age- and gender-matched to 79 patients with normal coronary anatomy. Multivariable Cox regression was performed for major adverse cardiovascular events (MACE) defined as all-cause death and non-fatal MI.
Results: Of the patients with ACA, the mean age was 57.7±14.1, and 56% were men. 83 MACE events were observed over 5 years of follow-up. Compared with patients with normal coronary anatomy, those with ACA had a lower prevalence of obstructive plaque (>50% stenosis) in the right coronary artery (32.9% vs. 15.8%, P =0.01), with no difference in other coronary arteries. Multivariable Cox regression revealed no association between ACA and MACE (HR 1.12, 95% CI: 0.42-3.04; P =0.82).
Conclusions: Patients with incidental ACA on CCTA experienced similar cardiovascular outcomes as compared with those with normal coronary artery anatomy. These findings suggest that the presence of incidental ACA in middle age may not confer worse outcomes.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Things That Begin With an “A” in Adult Congenital Heart Disease: What Is Aorta, Artery and Anomalous?
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1232-021
ISOLATED SINGLE CORONARY ARTERY IN ADULT POPULATION: A CONTEMPORARY CLASSIFICATION
Rajan Kumar, Archana Sinha and Jamshid Shirani
vol. 69 no. 11 Supplement 648
DOI:
https://doi.org/10.1016/S0735-1097(17)34037-8
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Rajan Kumar,
- Archana Sinha and
- Jamshid Shirani
- Saint Luke’s University Health Network, Bethlehem, PA, USA
Background: Isolated single coronary artery (iSCA), qualified by absence of other major congenital anomalies, is rarely encountered during invasive coronary angiography [ICA (0.014-0.066%)] yet poses diagnostic and therapeutic challenges. Certain subtypes of iSCA are also associated with myocardial ischemia and sudden cardiac death. Early classifications, based on ICA and autopsy (Ogden 1970, Lipton 1979, Shirani/Roberts 1993), were limited by small number of cases and poor spatial display of 2-dimensional ICA. Coronary CT angiography (CCTA) and MRI have rapidly expanded number and subtypes of iSCA with exquisite anatomic details.
Methods: Exhaustive literature search identified 713 adults with iSCA (age 57±14 years, 58% men). There has been rise in reported cases of iSCA with 523 (73%) cases reported in last two decades. Demographic, clinical and coronary anatomy data were collected. Diagnoses were made by ICA [n=391 (55%)], CCTA [n=52 (7%)], ICA+CCTA [n=191 (27%)], autopsy [n=54 (7%)], ICA+MRI or CCTA+MRI or ICA+CCTA+MRI [n=25 (4%)].
Results: Single coronary ostium (SCO) was located in right [R-SCO, n=383 (54%)] or left [L-SCO, n=317, (44%)] coronary sinuses or in ascending aorta [high take-off, n=13 (2%)]. Overall, 15 L-SCO, 18 R-SCO and 3 high take-off variations were identified. Among 36 variations, 4-15% could not be categorized by existing classifications. Myocardial ischemia was reported in 524 (73%) and was caused by atherosclerotic CAD [n=366 (70%)] or was direct result of coronary anomaly [n=158 (30%)]; 258 (36%) underwent coronary intervention [percutaneous: n=187 (26%), surgical: n=71 (10%)].
Conclusions: Attempts at incorporating novel variations of iSCA have been challenging due to limitations of existing classifications. A comprehensive and contemporary classification of iSCA is proposed that can easily accommodate new and as yet unreported (potential) variations. Detailed knowledge of coronary anatomy is relevant to identification of malignant variants and to planning and performing coronary interventions in adults with iSCA.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Things That Begin With an “A” in Adult Congenital Heart Disease: What Is Aorta, Artery and Anomalous?
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1232-022
THE RAC SIGN: RETROAORTIC ANOMALOUS CORONARY ARTERY VISUALIZATION BY TRANSTHORACIC ECHOCARDIOGRAPHY
Chance M. Witt, Leslie Elvert, Ewa Konik, Naser Ammash, David Foley and Thomas Foley
vol. 69 no. 11 Supplement 649
DOI:
https://doi.org/10.1016/S0735-1097(17)34038-X
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Chance M. Witt,
- Leslie Elvert,
- Ewa Konik,
- Naser Ammash,
- David Foley and
- Thomas Foley
- Mayo Clinic, Rochester, MN, USA
Background: An unrecognized tubular structure was noted on the transthoracic echocardiogram (TTE) of several patients (image, panels A and C). This appeared to correlate with a retroaortic anomalous coronary artery identified on a patient’s computed tomography (CT) study (image, panels B, D and E). We aimed to determine if this sign on TTE (panel A) was consistently associated with this coronary anomaly.
Methods: Adult patients with a retroaortic anomalous coronary on CT who also had a TTE from 2005-2015 were included. A matched control group with normal coronary arteries on CT was identified. TTE from both groups were reviewed by blinded investigators who indicated the presence of the sign in question, dubbed the RAC sign. These results were compared to the known coronary anatomy.
Results: There were 49 patients with the anomaly on CT matched with 49 patients with no coronary anomalies. In patients with an anomaly, the RAC sign was present in 31 echocardiograms (63%) compared to its presence in only 3 patients (6%) with normal coronaries (p < 0.001). Thus, the RAC sign has a sensitivity of 63.3% and specificity of 93.9% for indicating the presence of a retroaortic anomalous coronary artery. Only 1 (2.0%) clinical TTE report noted the presence of a coronary anomaly.
Conclusions: The RAC sign is highly specific for the presence of a retroaortic anomalous coronary artery. Due to the potential for adverse events associated with the anomaly, this sign should not be dismissed as artifact, as may have occurred previously.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 3:45 p.m.-4:30 p.m.
- Session Title: Things That Begin With an “A” in Adult Congenital Heart Disease: What Is Aorta, Artery and Anomalous?
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1232-024
BIOMARKER PROFILE IN ADULTS WITH FONTAN CIRCULATION
Anita Saraf, Christine De Staercke, Fred Rodriguez, Andreas Kalogeropoulos, Andrea Knezevic, Jennifer Gerardin, Georges Ephrem, Salim Hayek, Staci Jennings, Agasha Katabarwa, Arshed Quyyumi and Wendy Book
vol. 69 no. 11 Supplement 650
DOI:
https://doi.org/10.1016/S0735-1097(17)34039-1
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 30, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Anita Saraf,
- Christine De Staercke,
- Fred Rodriguez,
- Andreas Kalogeropoulos,
- Andrea Knezevic,
- Jennifer Gerardin,
- Georges Ephrem,
- Salim Hayek,
- Staci Jennings,
- Agasha Katabarwa,
- Arshed Quyyumi and
- Wendy Book
- Emory University School of Medicine, Atlanta, GA, USA
Background: Fontan palliation causes systemic changes in hemodynamics resulting in multi-organ co-morbid conditions. We evaluated biomarker levels representative of various systemic pathways in stable Fontan patients in comparison with healthy controls.
Methods: We compared 23 stable Fontan patients, mean age 32.4 ± 9.02 yr, 46.9% female, 82.6% black, BMI of 26.6 ± 5.3 and 47.8% with an atriopulmonary connection (APC) and compared them with 19 controls of similar age, race, gender and BMI profile without known chronic disease. Means of biomarker values and their 95% confidence intervals were calculated for each group and results for both were evaluated for significance using the Wilcoxon tests. Functional status of Fontan patients was assessed by 6-minute walk distance (6MWD).
Results: Fontan patients had mean 6MWD of 456.1 ± 58.5 m, and mean baseline SpO2 of 91.6 ± 4.9%. Mean time from Fontan was 19.9 ± 9.5 yr. Despite being medically stable, a variety of systemic biomarkers were dysregulated as compared to controls (Table 1). Inflammatory marker IL-1a, VEGF, NT-pro-ANP and cTroponin-1 were differentially regulated in patients with APC versus total cavopulmonary connection (TCPC).
Conclusions: Functionally stable Fontan patients have dysregulation of multiple systemic pathways in comparison to healthy controls, as reflected in the assayed biomarkers. Differences in the type of dysregulated biomarkers between the APC and TCPC group suggest differences in the pathophysiology within Fontan patients.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Sunday, March 19, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Redefining the “F” Word
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1270-009
ATRIAL DIASTOLIC “SUCTION”: AN IMPORTANT CONTRIBUTOR TO FONTAN CIRCULATION
Amitabh C. Pandey, Tarun Tandon, Poulina Uddin and Allen Johnson
vol. 69 no. 11 Supplement 651
DOI:
https://doi.org/10.1016/S0735-1097(17)34040-8
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Amitabh C. Pandey,
- Tarun Tandon,
- Poulina Uddin and
- Allen Johnson
- Scripps Clinic, La Jolla, CA, USA
Background: Current iterations of the Fontan circulation (FC) have no antegrade atrial or ventricular contribution to pulmonary blood flow. Systemic cardiac output (CO) is maintained by systemic atrial and ventricular function. The contribution of systemic atrial (SA) systole to systemic ventricular (SV) mechanics is well defined. Atrial diastolic mechanics have more recently been evaluated, with careful attention to echo doppler analysis of pulmonary venous (PV) S and D flow patterns. We observed in our patients with FC presence of PV S waves in the absence of a pulmonary ventricle. This suggested atrial diastolic “suction” could be a significant contributor to CO and decreasing pulmonary arterial, pulmonary venous (PV), and systemic venous pressure.
Methods: For four FC patients: Dynamic changes in relative F atrial volume were measured by frame by frame planimetry (apical 4 chamber view) converting derived radius to volume. Dynamic delta AV was temporally correlated (ECG as baseline) with PV velocities. PV D velocity/flow profile (VFP) was temporally matched with mitral valve (MV) VFP and delta LAV during early diastole: trans-mitral atrial VFP during atrial systole were correlated with delta LAV during atrial systole. Trans-mitral E VFP was assumed to be “conduit” flow; MV A flow VFP was correlated with atrial delta V during atrial systole PV S flow and simultaneous delta LAV are presumed to be secondary to atrial “suction.” Atrial emptying or filling fraction was calculated as maximal atrial volume – minimal atrial volume/maximum atrial volume. Mean atrial filling fraction was 49% and is ascribed to atrial “suction.” Delta atrial volume during MV A wave was 48% of atrial emptying fraction, and “conduit” flow accounted for 52%. PV S wave flow was equal to PV D wave flow.
Results: Mean atrial filling fraction was 49% and is ascribed to atrial suction. Delta atrial volume during MV A wave was 48% of atrial emptying fraction, and conduit flow accounted for 52%. PV S wave flow was equal to PV D wave flow.
Conclusions: In “clearing” pulmonary circulation in FC, atrial “suction” appears to be a very important contributor to systemic CO, dependent of course on the presence of preceding atrial contraction.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Sunday, March 19, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Redefining the “F” Word
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1270-010
PREVALENCE AND PREDICTORS OF PACEMAKER PLACEMENT IN ADULT FONTAN PATIENTS
Anushree Agarwal, Aarthi Sabanayagam, Ahmed Kheiwa, Colin Cunnington, Edward Gerstenfeld, Charles McCulloch, Ian Harris, Zian Tseng, Elyse Foster, Petra Jenkins, Jaspal Dua, Devinda Karunaratne, Sahrkaw Muhyaldeen, Amir Zaidi, Adam Fitzpatrick, Clifford Garratt, Bernard Clarke, Andreas Hoschtitzky and Vaikom Mahadevan
vol. 69 no. 11 Supplement 652
DOI:
https://doi.org/10.1016/S0735-1097(17)34041-X
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 30, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Anushree Agarwala,b,
- Aarthi Sabanayagama,b,
- Ahmed Kheiwaa,b,
- Colin Cunningtona,b,
- Edward Gerstenfelda,b,
- Charles McCullocha,b,
- Ian Harrisa,b,
- Zian Tsenga,b,
- Elyse Fostera,b,
- Petra Jenkinsa,b,
- Jaspal Duaa,b,
- Devinda Karunaratnea,b,
- Sahrkaw Muhyaldeena,b,
- Amir Zaidia,b,
- Adam Fitzpatricka,b,
- Clifford Garratta,b,
- Bernard Clarkea,b,
- Andreas Hoschtitzkya,b and
- Vaikom Mahadevana,b
- aUniversity of California San Francisco, San Francisco, CA, USA
- bManchester Royal Infirmary, Central Manchester University Hospitals NHS Trust, Manchester, United Kingdom
Background: Fontan palliation has improved survival for single ventricle patients. A late complication is bradyarrhythmia requiring pacemaker. This study aims to establish the incidence and identify predictors of pacemaker need in patients ≥ 18 years with long-term followup.
Methods: Retrospective review of medical records from 2 tertiary academic institutions identified 93 adult Fontan patients.
Results: Mean age was 31 ± 7yrs, 46% females (32% atriopulmonary (AP), 32% lateral tunnel (LT), 36% extracardiac (EC)). Mean follow-up was 31±7 years and follow-up since Fontan surgery was 23±6 yrs. Pacemaker insertion rate was 24.9% for AP, 24.8% for LT and 23.4% for EC Fontan. We estimated that over half of the Fontan patients will have pacemakers by age 38 yrs Compared to those without pacemaker, patients with pacemaker (45%) more likely had AP Fontan (48% vs. 20%, p=0.007) and New York Heart association (NYHA) class II/III (45%vs.18%, p=0.01). After Fontan surgery, median time to pacemaker was 28 years for all patients, with earlier requirement among EC/LT patients (26 vs. 31 years for AP) (Figure). Multivariate Cox regression analysis showed no effect of gender, NYHA II/III class, age at Fontan although EC Fontan was an independent predictor (hazard ratio 2.5; p=0.04).
Conclusions: There is an increasing need for PM in adult Fontan patients that is dependent on the type of Fontan. These patients continue to pose significant challenges as adults and further studies for optimal management and prevention are needed.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Sunday, March 19, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Redefining the “F” Word
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1270-011
USE OF NOVEL ORAL ANTICOAGULANTS IN ADULT FONTAN PATIENTS
Justin Georgekutty, Amir Kazerouninia, Peter Ermis, Dhaval Parekh, Wayne Franklin and Wilson Lam
vol. 69 no. 11 Supplement 653
DOI:
https://doi.org/10.1016/S0735-1097(17)34042-1
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Justin Georgekuttya,b,
- Amir Kazerouniniaa,b,
- Peter Ermisa,b,
- Dhaval Parekha,b,
- Wayne Franklina,b and
- Wilson Lama,b
- aTexas Children’s Hospital, Houston, TX, USA
- bBaylor College of Medicine, Houston, TX, USA
Background: Thromboembolic complications are a leading cause of morbidity and mortality in patients with Fontan physiology. Current clinical practice for prevention and treatment of these complications involves the use of vitamin K antagonists and/or antiplatelet agents. Novel oral anticoagulants (NOACs) are gaining more widespread use in adult patients with nonvalvular heart disease given the lack of a need for dietary modification, no lab monitoring and fewer drug-drug interactions. We report the use of NOACs in a cohort of adult Fontan patients.
Methods: A retrospective analysis of a cohort of adult Fontan patients on NOAC therapy was conducted. Demographics, underlying anatomy, NOAC used, indication for therapy, duration of therapy, thromboembolic events and bleeding events were obtained from the medical record. A CHA2DS2-VASc and HAS-BLED score were assigned to each patient based on clinical data available on the day of initiation of NOAC therapy. The study was approved by the Institutional Review Board of Baylor College of Medicine.
Results: Nineteen patients (10 women) were prescribed NOAC therapy with apixaban (N=13), rivaroxaban (N=4) and dabigatran (N=2) at a median age of 32 years (18-50). The primary indication for therapy was current arrhythmia (N=11), post arrhythmia procedure (N=3), thrombosis (N=3) and cyanosis with right to left shunting (N=2). The median CHA2DS2-VASc score was 1 (0-3) and HAS-BLED score was 2 (0-3). The median duration of therapy was 7 months (1-46) with a total of 225 patient months on therapy. There were no thromboembolic complications. Three patients had easy bruising, one patient had occasional hemorrhoid bleeding which was present prior to therapy and one patient had gastrointestinal bleeding related to biliary tree stenting. None of these patients required cessation of therapy. Thirteen patients remain on active NOAC therapy.
Conclusions: NOAC therapy in adults with Fontan palliation may be considered as a safe alternative for the prevention and treatment of thromboembolic complications. Further investigation is required to investigate long term safety and outcomes of NOACs in the Fontan population.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Sunday, March 19, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Redefining the “F” Word
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1270-012
ADULTS WITH CONGENITAL HEART DISEASE: LOST IN CARE
Jennifer Gerardin, Cheryl Raskind-Hood, Trenton Hoffman, Andrew Well, Fred Rodriguez, Andreas Kalogeropoulos, Carol Hogue and Wendy Book
vol. 69 no. 11 Supplement 654
DOI:
https://doi.org/10.1016/S0735-1097(17)34043-3
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Jennifer Gerardina,b,
- Cheryl Raskind-Hooda,b,
- Trenton Hoffmana,b,
- Andrew Wella,b,
- Fred Rodrigueza,b,
- Andreas Kalogeropoulosa,b,
- Carol Hoguea,b and
- Wendy Booka,b
- aDivision of Cardiology, Department of Medicine, Emory University School of Medicine, Atlanta, GA, USA
- bDepartment of Epidemiology, Rollins School of Public Health, Emory University, Atlanta, GA, USA
Background: Transfer of congenital heart disease (CHD) care from the pediatric to adult setting has been identified as a priority and is associated with better outcomes. Many CHD patients may fail to transfer. The goal of this study was to assess the percentage of CHD patients who transferred out of pediatric care to appropriate ACHD care.
Methods: We studied CHD patients age 16-30, primarily living in five metropolitan Atlanta counties, initially seen at least once in 1 of 3 pediatric Georgia healthcare systems during 2008-2010. We analyzed whether these CHD patients transferred to adult care during 2008-2015, and whether the adult provider was an ACHD cardiologist.
Results: Among 1,514 pediatric patients, 23.7% [(358/1514)*100] transferred into an adult health care system; distribution of adult providers seen is presented in Table 1. Only 19.7% appropriately transferred care to an ACHD cardiologist [(299/1514)*100], with an average of 14.4 months between last pediatric visit and first ACHD visit. 6% of those who transitioned to an ACHD provider later returned to see a pediatric provider at least once.
Conclusions: The majority of ACHD patients do not transfer to ACHD care. Those that successfully transfer do so at an appropriate interval. Recommendations from health care providers have been shown to be a significant reason for patients to seek ACHD care. Adult health care providers, including cardiologists, should be alerted to the need for screening patients for CHD and transferring care to ACHD providers.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Sunday, March 19, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Redefining the “F” Word
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1270-013
LATE COMPLICATIONS AND CARDIOPULMONARY PERFORMANCE IN ADULTS WITH FONTAN PHYSIOLOGY: RV-DOMINANT VERSUS THOSE WITH LV-DOMINANT OR UNSEPTATED VENTRICLES
Christoph Haller, Susan L. Roche, Rachel Wald, Simone Bartelse, Eric Pham-Hung, Candice Silversides, Erwin Oechslin, Jack Colman and Edward Hickey
vol. 69 no. 11 Supplement 655
DOI:
https://doi.org/10.1016/S0735-1097(17)34044-5
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Christoph Hallera,b,
- Susan L. Rochea,b,
- Rachel Walda,b,
- Simone Bartelsea,b,
- Eric Pham-Hunga,b,
- Candice Silversidesa,b,
- Erwin Oechslina,b,
- Jack Colmana,b and
- Edward Hickeya,b
- aThe Hospital for Sick Children, Toronto, Canada
- bUniversity Health Network, Toronto, Canada
Background: Do adult Fontans with RV-dominant single ventricle physiology (RV) have worse prognosis versus patients with LV-dominance (LV) or unseptated ventricles?
Methods: 180 adult Fontans (median age 25) were reviewed. Endpoints relating to Fontan failure and exercise capacity were compared. Additional comparisons used propensity-matched pairs near-identical by diagnosis, age and era. Risk-adjustment was via parametric models.
Results: A: RV (N=54) versus LV and unseptated ventricles (N=103 and 23 respectively).
B1: Matched pairs: 51 RV versus 51 LV.
B2: Of the 23 HLHS patients, 16 were matched against 16 LV.
Conclusions: Young adults with RV-dominant Fontans have comparable rates of late complications during early adulthood. Worse function and valve regurgitation is concerning for the longer term.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Sunday, March 19, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Redefining the “F” Word
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1270-014
CARDIOPULMONARY EXERCISE TESTING FOR SURGICAL RISK STRATIFICATION IN ADULTS WITH CONGENITAL HEART DISEASE
Joshua Kovach, Trevor L. Birkey, Jennifer E. Dixon, Roni Jacobsen, Pippa Simpson, Melodee Nugent, Ke Yan and Salil Ginde
vol. 69 no. 11 Supplement 656
DOI:
https://doi.org/10.1016/S0735-1097(17)34045-7
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Joshua Kovacha,b,
- Trevor L. Birkeya,b,
- Jennifer E. Dixona,b,
- Roni Jacobsena,b,
- Pippa Simpsona,b,
- Melodee Nugenta,b,
- Ke Yana,b and
- Salil Gindea,b
- aChildren’s Hospital of Wisconsin, Milwaukee, WI, USA
- bMedical College of Wisconsin, Milwaukee, WI, USA
Background: Adults with congenital heart disease (ACHD) often require repeat cardiothoracic surgery, which can result in significant morbidity and mortality. Currently there are few preoperative risk assessment tools available. In the general adult population, preoperative cardiopulmonary exercise testing (CPET) has predictive value for postoperative morbidity and mortality after major non-cardiac surgery. The utility of CPET for risk assessment in ACHD patients referred for surgery has not been evaluated.
Methods: Retrospective chart review was conducted on 78 ACHD patients who participated in CPET less than 12 months prior to major cardiothoracic surgery at Children’s Hospital of Wisconsin between January, 2005 and December, 2015. Minimally invasive procedures, single ventricle physiology, and heart transplant patients were excluded. Demographic information, CPET results, and perioperative surgical data were collected for each patient and analyzed. Spearman correlations (rho) are given.
Results: The median age of the study population was 25 years (range 17-58 years), and 55% were males. Postoperative length of stay correlated with increased VE/VCO2 slope (rho = 0.27, p = 0.039), while prolonged intubation was associated with decreased exercise time (rho = −0.34, p = 0.003), decreased heart rate response (rho = −0.30, p = 0.009), and decreased peak VO2 (rho = −0.26, p = 0.049). Postoperative complications were documented in 56% of patients, including arrhythmia, persistent pleural effusion, infection, and prolonged bleeding. There were trends noted between postoperative complications and some measurements of exercise capacity, such as peak metabolic equivalent of task, respiratory quotient, and heart rate response, but these did not meet statistical significance.
Conclusions: In a relatively young ACHD cohort, measures of exercise capacity significantly correlated with postoperative length of stay and duration of ventilation. A larger study is required to further define the relationship between exercise capacity and postoperative morbidity in ACHD patients.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Sunday, March 19, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Redefining the “F” Word
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1270-015
EVALUATION OF RIGHT VENTRICULAR FUNCTION IN FONTAN PHYSIOLOGY USING FEATURE TRACKING MAGNETIC RESONANCE STRAIN, STRAIN RATE AND WALL MOTION DELAY
Akio Inage
vol. 69 no. 11 Supplement 657
DOI:
https://doi.org/10.1016/S0735-1097(17)34046-9
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 30, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Akio Inage
- Sakakibara Heart Institute, Tokyo, Japan
Background: Patients are commonly affected by ventricular dysfunction after Fontan palliation. Reliable quantification of ventricular function was hampered by complex ventricular anatomy and physiology. Cine-based feature tracking strain (FTS) is a new technique to assess cardiac function from cardiac magnetic resonance (CMR). The objective of this study was to investigate into FTS in single right ventricle subjects after Fontan palliation undergoing CMR.
Methods: Right ventricular end-diastolic and end-systolic volumes (SVEDV and SVESV), stroke volume (SV), and ejection fraction (EF) were measured offline (Medis QMass advanced edition, the Netherlands) as conventional function parameters. Offline global longitudinal and circumferential strain/SR (GLS/GLSR and GCS/GCSR), and radial strain/SR were performed (TomTec Image Arena, Germany) using FTS. As well, anterior to posterior wall motion delay (<130ms; APWMD) analysis was calculated on the short-axis view at the basal level, and bilateral wall motion delay (<90ms; BLWMD) on the 4-chamber view at the basal and mid levels.
Results: 25 Fontan subjects with right ventricular morphology (mean age 18.4+/-9.6 years, post Fontan period 15.3+/-8.4 years) underwent a CMR study. Basal GCS/GCSR (-11+/-9 %, −0.8+/-0.5 1-s) were lower than it at the mid (-17+/-6 %, −1.1+/-0.5 1-s; p=0.02) and apical (-26+/-9 %, −1.9+/-1.0 1-s; p=0.001 and 0.003) levels. Basal GCS/GCSR were correlated with grade of atrioventricular valvular regurgitation (mild; r=0.53, moderate; r=0.63, severe; r=0.65). There were correlations between GLS/GLSR and GCS/GCSR, and SVEDV (r=0.53 to 0.71). At the mid and apical levels, there were correlations between GCS/GCSR and SVESV, and EF (r=0.68 to 0.79 and r=0.51 to 0.77). There was also correlation between GLSR and SV (r=0.71). BLWMD was found for 17 cases (67%) at the basal and 14 cases (56%) at mid levels, and APWMD for 6 cases (22%) at the basal level.
Conclusions: In Fontan patients there is moderate correlation between strain/SR and measures of ventricular size and ejection. Annular dysfunction suggested by correlation of low basal GCS/GCSR with grade of atrioventricular valvular regurgitation, and basal BLWMD.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Sunday, March 19, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Redefining the “F” Word
- Abstract Category: 9. Congenital Heart Disease: Adult
- Presentation Number: 1270-016
THE EVOLUTION OF ATRIOVENTRICULAR VALVE FUNCTION IN PATIENTS WITH HETEROTAXY SYNDROME: A LONGITUDINAL ASSESSMENT FROM FETUS TO LATE AFTER FONTAN OPERATION
Masaki Nii, Keisuke Sato, Jun Yoshimoto, Sung-Hae Kim, Norie Mitsushita and Yasuhiko Tanaka
vol. 69 no. 11 Supplement 659
DOI:
https://doi.org/10.1016/S0735-1097(17)34048-2
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Masaki Nii,
- Keisuke Sato,
- Jun Yoshimoto,
- Sung-Hae Kim,
- Norie Mitsushita and
- Yasuhiko Tanaka
- Shizuoka Children’s Hospital, Shizuoka, Japan
Background: The atrioventricular valve function is one of the most important determinants of mortality in patients with heterotaxy syndrome (HS). Though there are many reports to show the impact of atrioventricular valve regurgitation (AVVR) on the outcome of patients with HS, there are paucity of data analyzing the AVV function longitudinally from fetus to late after Fontan. The aims of this study are: 1) to elucidate the longitudinal change of AVVR from fetus to late after Fontan; 2) to assess the impact of AVVR on mortality on each stage.
Methods: The medical charts of patients with HS who visited Shizuoka Children’s Hospital postnatally between 1986 and 2015, and the records of fetal echocadiography between 1998 and 2015 were reviewed. The grade of AVVR was classified into 0 to 3.
Results: There were 227 postnatal patients with HS and 45 fetuses with HS on medical records. Among them, only patients with single ventricle and common AVV were analyzed. 1): postnatal patients: 198 (right atrial isomerism (RAI): 159; left atrial isomerism (LAI): 83; age at 1st visit: 15 days (0 day – 13 years) (median (range)); and 2): 40 fetuses (RAI: 31; LAI: 9; gestational week at 1st visit: 30 (18 – 37) weeks). The grade of AVVR increased from 2nd to 3rd trimester and it increased significantly after birth (AVVR: fetus in 3rd trimester: 1 (0 – 3); after birth: 2 (0 – 3) (p<0.05)). The grade of AVVR after birth increased continuously until Glenn operation and it decreased after Glenn and decreased further after Fontan, however it increased again late after Fontan. The mortality of fetuses with more than moderate AVVR was 75%, which was significantly worse than that of fetuses with less than mild AVVR (p<0.05). The grade of AVVR during fetal and neonatal period showed significant impact on mortality (p<0.05), whereas, the grade of AVVR in later stages showed no impact on survival. Sixty two patients had AVV plasty, 21 patients had multiple AVV plasties, and 8 patients had AVV replacement. The number of AVV platy showed no impact on survival.
Conclusions: The grade of AVVR increased continuously from 2nd trimester of pregnancy to before Glenn operation. The grade of AVVR during perinatal period showed significant impact on survival.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Sunday, March 19, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Congenital Heart Disease: Novel Insights in Pediatric Cardiology
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1271-018
CLINICAL YIELD OF FETAL ECHOCARDIOGRAPHY FOR SUBOPTIMAL CARDIAC VISUALIZATION ON OBSTETRIC ULTRASOUND
Rick Vavolizza, Pe’er Dar, Barrie Suskin, Robert Moore and Kenan Stern
vol. 69 no. 11 Supplement 660
DOI:
https://doi.org/10.1016/S0735-1097(17)34049-4
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 30, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Rick Vavolizza,
- Pe’er Dar,
- Barrie Suskin,
- Robert Moore and
- Kenan Stern
- Department of Pediatrics, Division of Cardiology, Children’s Hospital at Montefiore, Bronx, NY, USA
Background: Suboptimal cardiac imaging on obstetric ultrasound is a frequent referral indication for fetal echocardiography, even in the absence of typical risk factors for fetal cardiac disease. The clinical profile of patients and yield of examinations performed for such an indication are not well defined. Given the increased cost, time and resource utilization of fetal echocardiography, we sought to determine the clinical yield of such referrals.
Methods: Single-center retrospective review of referrals from January 2010 – June 2016 for fetal echocardiography for suboptimal views of fetal cardiac anatomy on obstetric ultrasound. Patients with commonly accepted indications for fetal echocardiography were excluded. Demographic variables and echocardiogram findings were collected. Clinical yield was classified as (1) ‘normal,’ if no structural or functional abnormalities were noted; (2) ‘indeterminate,’ if minor pathology couldn’t confidently be excluded (though significant pathology was not suspected); (3) ‘abnormal,’ if there was pathology.
Results: In total, 583 gestations were included (median gestational age 23.3 weeks, range 19.0 – 38.4). The median BMI was 34.6 kg/m2 (range 17.2 – 66.3). The majority of women were obese (BMI > 30 kg/m2 in 74.6% and > 40 kg/m2in 30.1%). The largest proportion of referral indications referenced maternal body habitus (47.2%). Difficult imaging was noted in 66% of the fetal echocardiogram reports. Fetal echocardiograms were repeated at least once in 76/562 patients (13.5%). Overall, 540 of 583 examinations (92.6%) were normal. Definitive pathology was noted in 10 patients (1.7%), three of who had confirmed critical congenital heart defects. In the remaining 33 (5.7%), no anomalies were noted but possible minor abnormalities could not be confidently excluded.
Conclusions: We found a cardiac anomaly rate of 1.7% in women referred for limited cardiac imaging on obstetric scan. Albeit low, this rate is higher than background rates of neonatal congenital heart disease. Fetal echocardiography for this indication may therefore be reasonable; however, improved cardiac screening procedures could result in a lower referral rate and higher clinical yield.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Sunday, March 19, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Congenital Heart Disease: Novel Insights in Pediatric Cardiology
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1271-020
LONG-TERM TRANSPLANT-FREE SURVIVAL FOR ARTERIAL SWITCH VERSUS ATRIAL SWITCH IN TREATMENT OF TRANSPOSITION OF THE GREAT ARTERIES: A STUDY FROM THE PEDIATRIC CARDIAC CARE CONSORTIUM
Alex Kiener, Mike Kelleman, Lazaros Kochilas and Matthew Oster
vol. 69 no. 11 Supplement 661
DOI:
https://doi.org/10.1016/S0735-1097(17)34050-0
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- aEmory University School of Medicine, Atlanta, GA, USA
- bChildren’s Healthcare of Atlanta, Atlanta, GA, USA
Background: In the 1980’s the preferred surgery for d-transposition of the great arteries (TGA) shifted from the atrial switch operation to the arterial switch operation (ASO). However, the long-term survival from ASO is unclear. Our objective was to compare transplant-free survival in patients with ASO vs. atrial switch.
Methods: We performed a retrospective cohort study of patients with TGA repair in the Pediatric Cardiac Care Consortium registry from 1982-1991 whose outcomes had been linked with the National Death Index and United Network for Organ Sharing. Kaplan Meier transplant-free survival curves and hazard of mortality/transplant were calculated for each group.
Results: Among the 342 patients with atrial switch and 235 patients with ASO, 20-year transplant-free survival was significantly greater in the ASO group (log-rank p=0.019, Figure), with the atrial switch cohort having a hazard of mortality/transplant of 1.58 compared to the ASO cohort (95% CI: 1.07-2.34, p=0.021). Presence of a ventricular septal defect was associated with a significantly increased hazard of mortality/transplant in the atrial switch group (2.04; 95% CI: 1.27-3.29, p=0.003) but not in the ASO group (1.54; 95% CI: 0.80-3.00, p=0.199). There was no significantly increased risk in patients with genetic defects in either group.
Conclusions: Long-term transplant-free survival for patients with TGA is superior with ASO compared to atrial switch. In-depth analysis is underway to determine causes of death in these patients.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Sunday, March 19, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Congenital Heart Disease Surgery: Updates and Innovations
- Abstract Category: 11. Congenital Heart Disease: Therapy
- Presentation Number: 1272-021
ANATOMIC REPAIR OF CONGENITALLY CORRECTED TRANSPOSITION RESULTS IN EXCELLENT SURVIVAL AND FUNCTIONAL STATUS AT INTERMEDIATE TERM FOLLOW-UP
James S. Tweddell, Shagun Sachdeva, Ronald Woods, Michael Mitchell, Joseph Cava, Nancy Ghanayem, Peter Bartzand Peter Frommelt
vol. 69 no. 11 Supplement 662
DOI:
https://doi.org/10.1016/S0735-1097(17)34051-2
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 29, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- James S. Tweddella,b,
- Shagun Sachdevaa,b,
- Ronald Woodsa,b,
- Michael Mitchella,b,
- Joseph Cavaa,b,
- Nancy Ghanayema,b,
- Peter Bartza,b and
- Peter Frommelta,b
- aChildren’s Hospital of Wisconsin, Milwaukee, WI, USA
- bCincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA
Background: Congenitally corrected transposition of the great arteries (CCTGA) is a rare cardiac malformation resulting from abnormal looping of the embryonic cardiac tube that results in atrioventricular and ventriculoarterial discordance. Surgical options include a physiologic repair (PR) or anatomic repair (AR). PR involves correction of the associated cardiac defects, leaving the morphologic right ventricle (RV) as the systemic ventricle and is associated with poor late survival. AR consists of an atrial switch operation combined with an arterial switch or Rastelli procedure and returns the morphologic left ventricle to the systemic position. Our aim was to review our outcomes with AR.
Methods: Retrospective analysis of 15 patients who underwent AR for CCTGA from 2001-2015.
Results: Two patients were lost to follow-up. Median duration of follow up was 4.5 years (0.05 −14 yrs). There have been no early or late deaths. No patients had heart failure symptoms. 12/13 patients (92%) had normal biventricular systolic function and 1 patient (7.6%) had mildly diminished left ventricular function.
Conclusions: AR repair can be applied to patients with CCTGA with excellent survival and functional status but reoperations are common. Bidirectional Glenn shunt is indicated for morphologic RV hypoplasia but should not be part of routine AR.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Sunday, March 19, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Congenital Heart Disease Surgery: Updates and Innovations
- Abstract Category: 11. Congenital Heart Disease: Therapy
- Presentation Number: 1272-022
TARGETED INCREASE IN PULMONARY BLOOD FLOW IN A BIDIRECTIONAL GLENN CIRCULATION
Samuel Casella, James Lock, Aditya Kaza, Pedro del Nido and Audrey Marshall
vol. 69 no. 11 Supplement 663
DOI:
https://doi.org/10.1016/S0735-1097(17)34052-4
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online November 30, 2017.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Samuel Casella,
- James Lock,
- Aditya Kaza,
- Pedro del Nido and
- Audrey Marshall
- Boston Children’s Hospital, Boston, MA, USA
Background: Additional pulmonary blood flow (PBF) into a Glenn shunt improves oxygenation at the risk of veno-venous collaterals, effusions, and Superior Vena Cava (SVC) hypertension. In select patients with unilateral pulmonary vascular abnormalities, targeted supplemental PBF may improve antegrade flow and permit eventual Fontan completion. We have attempted this by inserting a relatively small shunt into the affected pulmonary artery (PA) and banding the connection to the SVC-supplied lung, in an approach referred to as a “Super Glenn.”
Methods: We reviewed the charts and primary catheterization data for all patients who received a Super Glenn from 2000-2015. Comparisons of non-parametric variables were performed with the Wilcoxon sign rank test.
Results: We identified 20 patients with a median age and weight of 12.3mo and 7.9kg at intervention. Median follow up was 26mo. Vascular pathology included unilateral PA (n=8) or venous (n=5) obstruction, combined disease (n=4), or superabundant aortopulmonary collaterals (n=3). Nine patients had exclusively retrograde flow to the affected lung. There were 3 deaths: 45 days, 6mo and 8yrs postoperatively. Ten survivors had serious complications: pleural effusions (n=4), shunt thrombosis (n=3), SVC hypertension (n=2), reperfusion injury (n=1), hemidiaphragm paresis (n=1). 16 of 20 patients had initial qualitative improvement of their pulmonary vascular abnormality and all 9 patients with retrograde flow had restoration of antegrade PBF. There was no significant difference in systemic or SVC O2 saturation, or SVC pressure. There was a small increase in the shunted PA O2 saturation and pressure of 4% and 6mmHg, respectively. Presently, 8 patients have achieved a definitive palliation: 7 Fontans, 1 biventricular repair. Three patients had no improvement due to pulmonary vein atresia. A fourth patient was palliated as a Fontan with the shunt in place. Five patients are stable and awaiting further palliation.
Conclusions: The use of targeted additional PBF may be useful for the palliation of single ventricle patients with severely abnormal pulmonary vasculature. However, morbidity and mortality are common in this inherently high risk population.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Sunday, March 19, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Congenital Heart Disease Surgery: Updates and Innovations
- Abstract Category: 11. Congenital Heart Disease: Therapy
- Presentation Number: 1272-023
LONG TERM OUTCOMES AFTER THE FONTAN PROCEDURE IN PATIENTS WITH SINGLE VENTRICLE: A META-ANALYSIS
Ilana Schwartz, Courtney McCracken, Christopher Petit and Ritu Sachdeva
vol. 69 no. 11 Supplement 622
DOI:
https://doi.org/10.1016/S0735-1097(17)34011-1
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online February 28, 2018.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Ilana Schwartz,
- Courtney McCracken,
- Christopher Petit and
- Ritu Sachdeva
- Emory University School of Medicine, Atlanta, GA, USA
Background: Though there are numerous single center reports of Fontan outcomes, there is lack of comprehensive survival data. The purpose of this meta-analysis was to evaluate the long-term outcomes following Fontan operation and to assess risk factors for mortality.
Methods: PubMed, Embase and Web of Science were queried to retrieve studies published since 2000 in English language with > 20 patients, that reported survival after Fontan procedure with ≥ 5 years of followup. A random effects model was used to calculate pooled survival estimates at 5, 10 and 15 yrs, and rates of death, transplant and complications. Meta-regression was used to assess the association between study characteristics and survival.
Results: Of the 630 articles retrieved, 19 with a total of 5,859 patients (mean follow-up 8.88 ± 3.35 yrs) met the inclusion criteria. Pooled survival estimates at 5, 10 and 15 yrs were 91.1%, 87.6% and 87.5% respectively. Event rates for death, transplant, complications and meta-regression for total deaths is shown in the Table. Arrhythmias and pacemaker implantation were the most common long-term complications. Significantly increased rates of death were associated with earliest surgical year, atriopulmonary connection, and older age at Fontan, but not with systemic right ventricle.
Conclusions: Though long-term survival after Fontan has improved with time, many have complications. The survival is influenced by Fontan type and age of patients, but not by the systemic ventricular morphology.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Congenital Heart Disease: Innovations in Single Ventricle Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1182-012
RHYTHM ABNORMALITIES IN CHILDREN AND YOUNG ADULTS WITH MARFAN SYNDROME
Douglas Mah, Lynn Sleeper, Jane Crosson, Richard Czosek, David Gamboa, Barry Love, Brian McCrindle, Laura Muino Mosquero, Aaron Olson, Maully Shah, Stephanie Wechsler, Luciana Young and Ronald Lacro
vol. 69 no. 11 Supplement 658
DOI:
https://doi.org/10.1016/S0735-1097(17)34047-0
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online February 27, 2018.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Douglas Mah,
- Lynn Sleeper,
- Jane Crosson,
- Richard Czosek,
- David Gamboa,
- Barry Love,
- Brian McCrindle,
- Laura Muino Mosquero,
- Aaron Olson,
- Maully Shah,
- Stephanie Wechsler,
- Luciana Young and
- Ronald Lacro
- Pediatric Heart Network, Bethesda, MD, USA
Background: Individuals with Marfan syndrome (MFS) are at risk for sudden death. The contribution of arrhythmias is unclear. Our aim was to determine the prevalence of arrhythmias in MFS subjects, and their relationship to clinical and echocardiographic factors.
Methods: Data from the Pediatric Heart Network (PHN) prospective multicenter randomized trial of atenolol vs. losartan in subjects with MFS were analyzed. The 608 randomized subjects were 6 months-25 years old with aortic root diameter z-score (ARz) >3, and no prior AR surgery or dissection. Baseline 24-hour Holter monitors were performed prior to study drug initiation. Significant ventricular ectopy (VE) and supraventricular ectopy (SVE) were defined as ≥10 VE or SVE/hour, or the presence of high-grade ectopy: couplets, triplets, non-sustained ventricular (VT) or supraventricular tachycardia (SVT). The clinical outcome analyzed was the composite of death, aortic dissection, or AR replacement. Age-adjusted multivariable analysis was performed.
Results: There were 274 analyzable Holters from 11 PHN centers. Mean±SD age was 11±6 years, similar to the 334 subjects with unavailable Holters. 20 subjects (7%) had significant VE, 13 (5%) had significant SVE, 2 (1%) had both. None had sustained VT or SVT. VE was independently associated with increasing number of major Ghent criteria (odds ratio [OR] 2.1 per each additional criterion met, p=0.03) and greater left ventricular end-diastolic dimension z-score (OR=1.5, p=0.01). SVE was independently associated with greater aortic sinotubular junction diameter z-score (OR=1.6, p=0.03). Palpitations were more common when SVE was present vs absent (46% vs. 14%, p=0.006) but not VE (p=0.7). Syncope was not associated with either. Over 3 years, there were no deaths, 2 AR dissections with surgeries, and 13 with AR surgery only. These events were not related to VE or SVE (p≥0.3).
Conclusions: This is the largest study evaluating the prevalence of arrhythmia in children and young adults with MFS. Overall, VE and SVE were rare, with none having VT or SVT. VE is related to larger BSA-adjusted left ventricular size and a greater number of major Ghent criteria. Routine Holters are useful only in select MFS patients.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Sunday, March 19, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Congenital Heart Disease: Novel Insights in Pediatric Cardiology
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1271-017
DO PEDIATRIC CARDIOLOGISTS FOLLOW THE SPORTS RESTRICTION RECOMMENDATIONS FOR CHILDREN WITH A BICUSPID AORTIC VALVE?
Melissa Yamauchi, Michael Puchalski, Nelangi Pinto, Susan Etheridge, Hsin-Yi Weng, Angela Presson, L. LuAnn Minichand Richard Williams
vol. 69 no. 11 Supplement 630
DOI:
https://doi.org/10.1016/S0735-1097(17)34019-6
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online February 20, 2018.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Melissa Yamauchia,b,
- Michael Puchalskia,b,
- Nelangi Pintoa,b,
- Susan Etheridgea,b,
- Hsin-Yi Wenga,b,
- Angela Pressona,b,
- L. LuAnn Minicha,b and
- Richard Williamsa,b
- aUniversity of Utah, Salt Lake City, UT, USA
- bPrimary Children’s Hospital, Salt Lake City, UT, USA
Background: The AHA/ACC Task Force 7 recommends competitive sport restrictions (CSR) for patients with an isolated bicuspid aortic valve (BAV) and dilated aorta (z-score >2). We analyzed practice variation in CSR for children with BAV and factors influencing recommendations.
Methods: This retrospective single-center cohort study included children (<18 years) with an isolated BAV diagnosed from 01/05 to 12/14. CSR, follow-up interval, aortic stenosis (AS) and aortic regurgitation (AR) severity, aortic root and ascending aorta z-scores and outcomes were collected. Descriptive statistics and multi-variable mixed-effect logistic regression models were performed with providers and subjects as random effects. Adjusted odds ratio (OR) and 95% confidence interval (CI) were reported. Percent provider variation was estimated using the intra-class correlation coefficient.
Results: In 1,300 encounters (423 children; 28 providers), no CSR were documented in 25%, including 24% of encounters with a dilated (z-score >2) aortic root and 18% of encounters with a dilated ascending aorta, while 38% of encounters with a dilated aortic root and 40% of encounters with a dilated ascending aorta had high-static or high-dynamic CSR. There were no ≤ moderate static or dynamic CSR. Provider contributed 36% of observed CSR practice variation (p<0.001). CSR were independently associated with older age (OR 1.3, 95% CI 1.2-1.4), higher ascending aorta z-score (OR 1.5, 95% CI 1.2-1.8), and shorter follow-up interval (OR 0.5, 95% CI 0.4-0.7). CSR were not associated with aortic root z-score, AS or AR severity. There were no aortic dissections or deaths, and 1 cardiac intervention (BAV repair and aortic root replacement).
Conclusions: Physicians frequently fail to document CSR for children with BAV and when documented, vary from guidelines. A significant proportion of the variation in exercise restrictions is directly attributable to the provider rather than disease severity. Despite the variation in CSR, few adverse outcomes occurred in this cohort. Further study to understand deviation from recommended guidelines and the effect of CSR on BAV outcomes may lead to evidence based guidelines that are more widely accepted.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Saturday, March 18, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Congenital Heart Disease: Innovations in Single Ventricle Heart Disease
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 1182-020
PROMOTING PULMONARY ARTERIAL GROWTH VIA RIGHT VENTRICULAR TO PULMONARY ARTERY CONDUIT PLACEMENT IN CHILDREN WITH PULMONARY ATRESIA AND HYPOPLASTIC PULMONARY ARTERIES
Edon Rabinowitz, David Meyer and Shilpi Epstein
vol. 69 no. 11 Supplement 664
DOI:
https://doi.org/10.1016/S0735-1097(17)34053-6
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online February 20, 2018.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Edon Rabinowitz,
- David Meyer and
- Shilpi Epstein
- Steven & Alexandra Cohen Children’s Medical Center, New Hyde, Park, NY, USA
Background: Pulmonary atresia or severe pulmonary stenosis (PS) with hypoplasia of the native pulmonary arteries (PAs) is seen in a subset of patients with tetralogy of Fallot (TOF). Major aortopulmonary collateral arteries (MAPCAs) may contribute to pulmonary blood flow. Outcome depends on construction of an adequate sized pulmonary arterial tree incorporating or eliminating MAPCAs as needed. We report our results with a previously described management strategy which employs an initial intervention of right ventricle to native pulmonary artery (RV-PA) conduit to promote PA growth and ultimately allow for ventricular septation with low right ventricular pressure (RVp).
Methods: We retrospectively reviewed clinical and procedural data for all patients (n=8) with TOF, pulmonary atresia or severe PS, diminutive native PAs and MAPCAs in our center from October 2008 to August 2016. Preoperative and postoperative angiography was used to determine the pulmonary arterial vessel size over time to calculate the Nakata indices.
Results: Six patients had pulmonary atresia and 2 patients had severe PS; MAPCAs were present in 2 patients. There were no deaths or serious morbidity; 1 conduit required revision prior to complete repair. At time of conduit placement median age and weight were 7.5days and 3.1kg. Complete repair with ventricular septation was achieved in all patients at a median age of 262days. Postoperative RVp was less than half systemic in all patients. Nakata index in the neonatal period was 75±43mm2/m2 and at the time of full repair 200±146 mm2/m2 (p=0.015). The rate of increase in Nakata index from birth to full repair was 17+/-16mm2/m2/mo. The RPA and LPA growth ratio was similar at 0.38±0.31mm/mo and 0.42±0.33mm/mo respectively. The 8 patients underwent 24 catheterizations with 12 interventions prior to full repair; all but 1 patient had at least 1 intervention.
Conclusions: Early palliative RV-PA conduit promotes PA growth and facilitates eventual full repair with VSD closure with low RVp and operative risk.
Footnotes
- Poster Contributions
- Poster Hall, Hall C
- Sunday, March 19, 2017, 9:45 a.m.-10:30 a.m.
- Session Title: Congenital Heart Disease Surgery: Updates and Innovations
- Abstract Category: 11. Congenital Heart Disease: Therapy
- Presentation Number: 1272-024
TRANSCATHETER DUCTAL STENTING VERSUS SURGICAL SYSTEMIC-TO-PULMONARY ARTERY SHUNTS: ALTERING DOGMA AT A HIGH-VOLUME INSTITUTION
Allen Ligon, Christopher Petit, Mike Kelleman, Nikhil Chanani, Robert Vincent and Dennis Kim
vol. 69 no. 11 Supplement 555
DOI:
https://doi.org/10.1016/S0735-1097(17)33944-X
Published By:
Journal of the American College of Cardiology
Print ISSN:
Online ISSN:
History:
- Published online February 26, 2018.
Copyright & Usage:
2017 American College of Cardiology Foundation
Author Information
- Allen Ligona,b,
- Christopher Petita,b,
- Mike Kellemana,b,
- Nikhil Chanania,b,
- Robert Vincenta,b and
- Dennis Kima,b
- aChildren’s Healthcare of Atlanta, Atlanta, GA, USA
- bEmory University School of Medicine, Department of Pediatrics, Atlanta, GA, USA
Background: Stenting of the ductus arteriosus is an effective alternative in establishing stable pulmonary blood flow (PBF) in infants with cyanotic congenital heart disease. We performed a retrospective comparison between surgical shunts (SS) and ductal stents (DS) at our institution.
Methods: We reviewed all SS or DS patients from June 2012 to May 2016 who were considered equivalent candidates for either palliation. Patients who received a SS due to additional anatomic issues were not included. We compared baseline patient characteristics, re-intervention rates and post-operative outcomes including feeding patterns on discharge, somatic growth velocity after discharge and effects on the subsequent surgical intervention.
Results: Of 107 total patients (66 SS and 41 DS), there were no baseline differences between the groups prior to intervention or with respect to single vs dual source PBF lesions. In the DS group there were fewer mechanical ventilator days post-procedure (median 1 vs 4; p<0.01), inotrope utilization days (0 vs 3; p<0.01), diuretic usage days (8 vs 12; p<0.01), and ICU days (2 vs 8; p<0.01). The SS had a higher incidence of need for ECMO (18.2% vs 2.4%; p=0.02). The DS group had more patients discharged solely on oral feeds (43.9% vs 3.0%; p<0.01) and with fewer patients on strict nasogastric feeds (22% vs 53%; p<0.01). The DS cohort experienced a greater somatic growth velocity in the interval until the subsequent surgical palliation (21.9 vs 19.6 grams/day; p<0.01). The rate of catheterizations without intervention were higher in the SS (p=0.031). There was no difference between the groups in regards to catheterizations with interventions (p=0.63), overall length of stay (p=0.45), readmission within 30 days (p=0.13), pulmonary arterial augmentation (p=0.39) or age (p=0.92) at subsequent surgery.
Conclusions: At our institution, the introduction of a ductal stenting has been associated with reduced morbidity and improved post-procedural outcomes. These benefits continue to the time of next surgical intervention. Evaluation of these outcomes has resulted in a “cultural shift” in strategy for many patients who otherwise would have received a surgical shunt a priori.
Footnotes
- Oral Contributions
- Room 146 C
- Sunday, March 19, 2017, 8:25 a.m.-8:35 a.m.
- Session Title: Highlighted Original Research: Congenital Heart Disease and the Year in Review
- Abstract Category: 10. Congenital Heart Disease: Pediatric
- Presentation Number: 908-06