Abstract 18725: Current Era Survival and Prevalence of Pulmonary Hypertension-Specific Therapy in Adult Patients With Eisenmenger Syndrome
Hideo Matama, Shigefumi Fukui, Takeshi Ogo, Jin Ueda, Akihiro Tsuji, Teruo Noguchi, Kengo Kusano, Toshihisa Anzai, Satoshi Yasuda
American Heart Association 2016
Background: We have previously reported that patients with Eisenmenger syndrome (ES) without diagnosis until adulthood had a poor prognosis. Those patients were enrolled before 1998, when any pulmonary hypertension (PH)-specific therapies were unavailable in Japan. Thereafter, several PH-specific therapies have been markedly developing. However, it remains to be elucidated whether or not increasing use of modern PH treatment leads to improved prognosis in ES patients in the current era, compared with the previous era. This study aimed to investigate (1) the prevalence of modern PH treatment and (2) long-term prognosis in adult patients with ES in the current era.
Methods: We retrospectively studied 38 consecutive adult patients (42±16 years; 25 women) with ES who underwent diagnostic catheterization between January 2001 and January 2016 in our center. The prevalence of modern PH treatment; a long-acting oral prostacyclin analogue, an endothelin receptor antagonist, a phosphodiesterase type-5 inhibitor, and intravenous epoprostenol and its impact on hemodynamics and long-term prognosis were studied and compared with our previous report including 106 adult patients with ES who were treated with supportive therapy alone (historical control group).
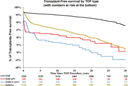
Results: Of 38 patients, 33 (87%) were treated with modern PH treatment (modern group), including oral triple combination therapy in 10, while 5 were treated without modern PH treatment throughout the follow-up (non-modern group). No significant differences were found for any baseline characteristics between modern and non-modern groups. During a mean follow-up of 7.3±3.9 years, 7 patients died and 3 underwent lung transplantation. Kaplan-Meier analysis showed that transplantation free-survival in modern group was 100% at 1 year, 90% at 5 years, and 81% at 10 years, which was significantly higher than non-modern group (75% at 1 year, 50% at 5 years, and 25% at 10 years) (P<0.05) and eventually historical control group (98% at 1 year, 77% at 5 years, and 58% at 10 years).
Conclusions: Adult patients with ES treated with modern PH treatment had better long-term prognosis than those in non-modern and historical control groups, which may be associated with proactive use of modern PH treatment over the last decade.
Article Information
vol. 134 no. Suppl 1 A18725
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Hideo Matama;
- Shigefumi Fukui;
- Takeshi Ogo;
- Jin Ueda;
- Akihiro Tsuji;
- Teruo Noguchi;
- Kengo Kusano;
- Toshihisa Anzai;
- Satoshi Yasuda
- Cardiovascular Medicine, National Cerebral and Cardiovascular Cntr, Osaka, Japan
Abstract 18313: Predictors of Death or Extracorporeal Membrane Oxygenation Support After Surgery for Adult Congenital Heart Disease
Stephen J Dolgner, Titus Chan, Eric V Krieger, Jacob Wilkes, Susan L Bratton, Ravi R Thiagarajan, Cindy S Barrett
Circulation. 2016;134:A18313
Abstract
Introduction: Adults with congenital heart disease (ACHD) who undergo cardiac surgery are at risk for poor outcomes, including death and extracorporeal membrane oxygenation support (ECMO). Prior studies have demonstrated risk factors for mortality, but have not differentiated between death despite ECMO usage and death without ECMO support. Furthermore, risk factors for ECMO support and death without ECMO have not been described.
Hypothesis: Patients who die or require ECMO after ACHD surgery will have identifiable risk factors.
Methods: All adults (≥ 18 years) undergoing congenital heart surgery in the Pediatric Health Information System database between the years of 2003-2014 were included. Patients were classified as ECMO-free survival, requiring ECMO support or death without ECMO support. Multivariate models were constructed examining death and ECMO support as individual and composite outcomes.
Results: A total of 5724 adult patients underwent cardiac surgery with 66 patients requiring ECMO and 81 dying without ECMO support. Of the 66 ECMO patients, 42 (64%) died. Pre-operative variables including older age, longer pre-operative length of stay, higher RACHS-1 score, higher number of comorbidities, and single ventricle anatomy were associated with the composite outcome of ECMO or death. Post-operative variables including acute renal failure, stroke, liver failure, post-operative hemorrhage, cardiac arrest, GI hemorrhage, paroxysmal ventricular tachycardia (VT) and secondary pulmonary hypertension were also associated with increased risk of ECMO or death. In multinomial models, age, higher number of comorbidities and GI hemorrhage were not associated with increased risk of ECMO support but were associated with death without ECMO. In contrast, paroxysmal VT and secondary pulmonary hypertension were associated with increased risk of ECMO but not death without ECMO. All other variables remained associated with both outcomes.
Conclusions: There are similar but separate risk factors for ECMO support and death without ECMO in adults undergoing congenital heart surgery in pediatric hospitals. Both pre-operative and post-operative risk factors should be considered when counseling and caring for these patients.
Article Information
vol. 134 no. Suppl 1 A18313
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Stephen J Dolgner1;
- Titus Chan2;
- Eric V Krieger3;
- Jacob Wilkes4;
- Susan L Bratton5;
- Ravi R Thiagarajan6;
- Cindy S Barrett7
- 1Cardiology, Seattle Children’s Hosp, Seattle, WA
- 2Critical Care, Seattle Children’s Hosp, Seattle, WA
- 3Cardiology, Univ of Washington, Seattle, WA
- 4Pediatrics, Univ of Utah, Salt Lake City, UT
- 5Pediatric Critical Care, Univ of Utah, Salt Lake City, UT
- 6Cardiology, Boston Children’s Hosp, Boston, MA
- 7Cardiology, Children’s Hosp Colorado, Aurora, CO
Abstract 18398: Long-Term Incidence of Pulmonary Hypertension in Adults With Congenital Heart Disease Compared to the General Population: A Nationwide Cohort Study
Morten Olsen, Nicolas Madsen, Sara S Schwartz
Circulation. 2016;134:A18398
Abstract
Background: The population of adults with congenital heart disease (CHD) is growing and ageing. One potential complication of CHD is pulmonary hypertension (PH), a severe condition that results in limited functional capacity and increased mortality. Few data exist on the incidence of adult onset PH in the CHD population. This study estimates the incidence of PH in the adult CHD-population compared to the general population.
Methods: In two Danish nationwide registries, we identified all individuals diagnosed with CHD in the years 1963-1974 and 1977-2012. Individuals were matched 1:10 by birth year and gender with individuals from the general population. Adults over 18 years were followed during January 1st 1977 to January 1st 2013 for PH-diagnosis, using data from the Danish National Registry of Patients (DNRP), a nationwide hospital discharge registry covering all Danish hospitals. Study subjects with PH-related hospitalization occurring before age 18, or before the CHD diagnosis (if this was made after 18 years of age), were excluded. A unique personal identifier assigned at birth enabled complete follow-up until PH, death, emigration or end of study. We computed incidence rates and cumulative incidences of PH.
Results: We identified 15,263 adult CHD survivors. By 70 years of age the cumulative incidence of PH was 7.8 % in all individuals with CHD, 8.3 % in individuals with systemic-to-pulmonary shunt lesions and 7 % in other heart defects, compared to 0.5 % in the general population comparison cohort. The PH incidence rate was 85 per 100,000 person years in the CHD population aged 18-50 years and it was 441 in the CHD population aged >50 years.
Conclusion: Adult onset PH is a common long-term complication of CHD. The risk is not exclusive to those with a history of systemic-to-pulmonary shunt lesions. The PH incidence rate in the adult CHD population increases with age.
Abstract 18079: Albuminuria in Adults With Congenital Heart Disease: Results From the Boston Adult Congenital Heart Biobank
Saurabh Rajpal, Laith Alshawabkeh, Justin Owumi, Robin Bradley, Elizabeth I Landzberg, Michael N Singh, Michelle Gurvitz, Finnian R McCausland, Sushrut S Waikar, Michael J Landzberg, Alexander R Opotowsky
Circulation. 2016;134:A18079
Abstract
Introduction: Albuminuria is present in ~5-10% of the population with a higher prevalence among those with diabetes mellitus or hypertension. Its presence reflects microvascular dysfunction and is associated with adverse outcomes. We assessed the prevalence of and risk factors for albuminuria in adults with congenital heart disease (CHD).
Methods: We enrolled outpatients with CHD ≥18 years old between 2012 and 2015 at Boston Children’s and Brigham and Women’s Hospitals. Urine creatinine and albumin were measured. Albuminuria was defined as an albumin to creatinine ratio (ACR) >30 mg/g; ACR >30-300 mg/g was classified as moderately increased albuminuria while values >300 mg/g were classified as severely increased albuminuria.
Results: A total of 575 patients with data on urine protein and creatinine were included. The most common types of CHD were left sided obstructive lesions (22.3%), tetralogy of Fallot (20.0%), single ventricle Fontan (16.8%), simple shunt lesions (16.6%) and transposition of the great arteries with a systemic right ventricle (9.6%). Albuminuria was present in 169 (29.4%), moderately increased in 141 (24.5%) and severely increased in 28 (4.9%). This was not attributable to the presence of diabetes mellitus or systemic hypertension. Albuminuria was associated with older age, BMI<30kg/m2, and worse functional class (Table). While albuminuria was most common among patients with cyanosis or a single ventricle Fontan circulation, it was still present in 23% of patients without either of these characteristics. Use of diuretics or beta-blockers was more common in those with albuminuria, but there was no difference in the use of angiotensin converting enzyme inhibitors or receptor blockers.
Conclusions: Adults with CHD have a high prevalence of albuminuria with the highest prevalence seen in patients with either cyanosis or a Fontan circulation. The mechanisms and clinical implications of this observation remain to be defined.
Article Information
vol. 134 no. Suppl 1 A18079
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Saurabh Rajpal1;
- Laith Alshawabkeh1;
- Justin Owumi1;
- Robin Bradley1;
- Elizabeth I Landzberg2;
- Michael N Singh1;
- Michelle Gurvitz1;
- Finnian R McCausland3;
- Sushrut S Waikar3;
- Michael J Landzberg1;
- Alexander R Opotowsky1
- 1Cardiology, Boston Children’s Hosp, Boston, MA
- 2Pediatrics, Columbia Univ Med Cntr, New York, NY
- 3Nephrology, Brigham and Women’s Hosp, Boston, MA
Abstract 17523: Pregnancy Outcomes in Women With Regurgitant Valve Lesions
Angelo Dave C Javier, Jasmine Grewal, Nadia Gabarin, Jack M Colman, Marla C Kiess, Rachel D Wald, Jennifer Mason, Matthew Sermer, Samuel C Siu, Candice K Silversides
Circulation. 2016;134:A17523
Abstract
Introduction: Pregnancy outcomes in women with significant regurgitant valve lesions have not been well defined. The primary objective of this study is to determine the frequency of maternal adverse cardiac events in pregnant women with significant regurgitant valve lesions. We also aim to describe obstetric and fetal/neonatal adverse outcomes in this population.
Methods: Women with heart disease enrolled in a prospective study on pregnancy outcomes (Toronto and Vancouver, Canada) with moderate or greater regurgitant valve lesion were included. Women with coexisting significant stenotic lesions were excluded. Multivalve disease was defined as more than one regurgitant valve lesion. Adverse maternal cardiac events included: pulmonary edema or right heart failure requiring treatment, sustained or symptomatic tachyarrhythmia requiring treatment, cardiac arrest, or cardiac death.
Results: There were 462 completed pregnancies in women with moderate or greater valvular regurgitation (mean maternal age 29.6 ± 5.7 years); 73% (337/462) of women had congenital heart disease and 13% (59/462) had rheumatic heart disease. Pregnancies were classified according to the most significant regurgitant valve lesions: systemic atrioventricular (AV) valve regurgitation (n=149), subpulmonary AV valve regurgitation (n=91), aortic valve regurgitation (n=44), pulmonary valve regurgitation (n=104), and multivalve regurgitation (n=74). Adverse cardiac events complicated 13% (61/462) of pregnancies. Among pregnancies in women with isolated regurgitant valve lesions, adverse maternal cardiac events occurred in 15% of women with systemic AV valve regurgitation, 13% with subpulmonary AV valve regurgitation, 5% with aortic regurgitation and 4% with pulmonary regurgitation. Adverse cardiac events were highest in women with multivalve disease (27%). Adverse fetal/neonatal and obstetric complications occurred in 22% and 9% of pregnancies, respectively.
Conclusions: Women with moderate or greater AV valve regurgitation are at risk for cardiac complications during pregnancy. Pregnancies in women with aortic and pulmonary valve regurgitation are usually well tolerated. Women with more than one regurgitant valve lesion are at highest risk for complications.
Article Information
vol. 134 no. Suppl 1 A17523
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Angelo Dave C Javier1;
- Jasmine Grewal2;
- Nadia Gabarin3;
- Jack M Colman4;
- Marla C Kiess2;
- Rachel D Wald4;
- Jennifer Mason5;
- Matthew Sermer6;
- Samuel C Siu7;
- Candice K Silversides4
- 1Toronto Congenital Cardiac Cntr for Adults, Peter Munk Cardiac Cntr, Univ Health Network, Univ of Toronto, Toronto, Canada
- 2Cardiac Obstetrics Clinic and Pacific Adult Congenital Heart Disease Clinic, St. Paul’s Hosp, Univ of British Columbia, Vancouver, Canada
- 3Sch of Medicine, Queen’s Univ, Kingston, Canada
- 4Toronto Congenital Cardiac Cntr for Adults, Peter Munk Cardiac Cntr, Univ Health Network, Univ of Toronto and Mount Sinai Hosp, Toronto, Canada
- 5Univ of Toronto Program in Pregnancy and Heart Disease, Obstetric Medicine Program, Univ Health Network, Univ of Toronto and Mount Sinai Hosp, Toronto, Canada
- 6Dept of Obstetrics, Mount Sinai Hosp, Toronto, Canada
- 7Div of Cardiology, Univ of Western Ontario, London, Canada
Abstract 12738: Elevated Sympathetic Activity, Impaired Endothelial Function, and Late Hypertension After Repair of Coarctation of the Aorta
Melissa G Lee, Jonathan P Mynard, Elisabeth Lambert, Michael M Cheung, Gavin Lambert, Yves d’Udekem
Circulation. 2016;134:A12738
Abstract
Introduction: There is a high prevalence of hypertension late after repair of coarctation of the aorta but its exact mechanism is unknown. Elevated sympathetic tone may contribute to the development of late hypertension. This study aims to investigate the neural profile of coarctation patients including the use of muscle sympathetic nerve activity (MSNA) testing, a direct method of measuring sympathetic activity.
Methods: Twenty-three patients aged ≥18 years with a coarctation repair underwent transthoracic echocardiography (TTE) and measurements of resting and 24-hour ambulatory blood pressures (BP), MSNA, sympathetic and cardiac baroreflex functions, digital endothelial function, and pulse wave velocity (PWV). Median age at repair was 1.2 months (interquartile range: 0-9 months). Patients were compared to 18 healthy controls matched for age, gender, weight, and waist/hip circumference ratio.
Results: After a follow-up of 26 ± 5 years, 6% (1/18) and 44% (8/18) had clinic resting hypertension and prehypertension, respectively. On 24-hour BP monitoring, 15% (3/20) and 20% (4/20) had hypertension and prehypertension, respectively. Left ventricular hypertrophy on TTE was present in 43% (6/14), and was more prevalent in patients with prehypertension/hypertension on 24-hour BP monitoring compared to those with normal 24-hour BP (75% [3/4] vs. 30% [3/10], p=0.2). Coarctation patients had elevated MSNA compared with controls (50 ± 25 vs. 29 ± 14 bursts/100 heartbeats, p=0.01), decreased sympathetic baroreflex function (-2.2 ± 2.1 vs. -7.0 ± 5.6 bursts/100 heartbeats·mmHg-1, p=0.007), normal cardiac baroreflex function (41.9 ± 30.4 vs. 35.7 ± 21.1 ms·mmHg-1, p=0.6), decreased endothelial function (pulse amplitude tonometry ratio: 0.4 ± 0.3 vs. 0.8 ± 0.5, p=0.004), and normal PWV (5.8 ± 1.1 vs. 5.5 ± 0.4 m/s, p=0.7).
Conclusions: After coarctation repair patients have increased MSNA, impaired sympathetic baroreflex response, and impaired endothelial function, all of which may contribute to the development of late hypertension. Agents targeting sympathetic activity and endothelial function may be the ideal antihypertensive therapies after coarctation repair. Regular monitoring for late hypertension after coarctation repair is warranted.
Abstract 12795: Impact of Right Ventricular Outflow Tract Obstruction on Right Ventricular Remodeling and Exercise Capacity in Patients With Severe Pulmonary Regurgitation After Repair of Tetralogy of Fallot
Qiuming Chen, Shoujun Li, Keming Yang, Xiangbin Pan, Zhongdong Hua, Hao Zhang, Minjie Lu, Xingguo Sun, Kai Ma, Sen Zhang, Lei Qi
Circulation. 2016;134:A12795
Abstract
Introduction: The long-term impact of right ventricular outflow tract obstruction (RVOTO) in patients with severe pulmonary regurgitation after repair of tetralogy of Fallot are controversial.
Hypothesis: We hypothesize that patients with combined PR and RVOTO have better RV remolding and exercise capacity than patients with isolated PR.
Methods: This is a retrospective cohort study of ninety-one consecutive patients with severe PR detected on echocardiography and evaluated with cardiac magnetic resonance and cardiopulmonary exercise test between 2012 and 2016. Twenty-three patients had combined PR and RVOTO (Doppler peak RVOT gradient ≥30 mmHg), while the other had isolated PR (n=68).
Results: In spite of similar PR fraction between the two groups, patients with combined PR and RVOTO had significantly smaller RV end-diastolic volume (129.1 ± 32.7 vs 163.3 ± 53.9 ml/m2, p=0.020) and RV end-systolic volume (84.9 ± 26.5 vs 110.8 ± 48.2 ml/m2, P= 0.006) than patients with isolated PR. No significant difference was detected in RV ejection fraction and left ventricle volumes and function between the two groups. Multivariable linear regression analysis identified that transannular repair and peak pressure gradient of RVOT as independent predictors for RV volume. Patients with combined PR and RVOTO had higher (24.9 ± 5.2 vs 20.1 ± 6.3 ml/kg/min, P=0.07) peak oxygen uptake than patients with isolated PR. Peak RVOT gradient was the only independent predictor of exercise capacity in patients with combined PR and RVOTO.
Conclusions: Patients with combined PR and RVOTO had less dilated RV and better exercise capacity than those with isolated PR. An acceptable residual RVOTO is more advantageous in the long-term outcome of repaired TOF.
Article Information
vol. 134 no. Suppl 1 A12795
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Qiuming Chen1;
- Shoujun Li1;
- Keming Yang1;
- Xiangbin Pan1;
- Zhongdong Hua1;
- Hao Zhang1;
- Minjie Lu2;
- Xingguo Sun3;
- Kai Ma1;
- Sen Zhang1;
- Lei Qi1
- 1Dept of Pediatric Cardiac Surgery, Fuwai Hosp, Chinese Academy of Med Sciences, Peking Union Med College, Beijing, China
- 2Dept of Magnetic Resonance Imaging, Fuwai Hosp, Chinese Academy of Med Sciences, Peking Union Med College, Beijing, China
- 3Heart-Lung Function Testing Cntr, Fuwai Hosp, Chinese Academy of Med Sciences, Peking Union Med College, Beijing, China
Abstract 23238: Pulmonary Vein Isolation Alone Is An Effective Rhythm Control Strategy In Patients With Persistent Atrial Fibrillation Those Changed To Paroxysmal Type With Antiarrhythmic Drug Therapy: A Multi-center Prospective Randomized Study
Hee Tae Yu, Jaemin Shim, Junbeom Park, In-Soo Kim, Tae-Hoon Kim, Jae-Sun Uhm, Boyoung Joung, Moon-Hyoung Lee, Young-Hoon Kim, Hui-Nam Pak
Circulation. 2016;134:A23238
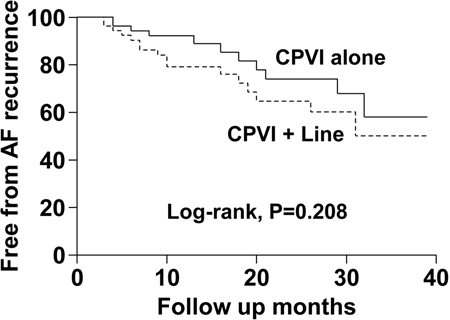
Background: Type of atrial fibrillation (AF) can change depending on the condition and time, and some of patients with initially presented persistent AF (PeAF) changed to paroxysmal AF (PAF) after anti-arrhythmic drug (AAD) medication and/or cardioversion (CV). We hypothesized that CPVI alone is an effective rhythm control strategy for radiofrequency catheter ablation (RFCA) in patients with PeAF to PAF.
Methods: We prospectively enrolled consecutive 113 patients with PeAF to PAF (male 75.2%, 60.4±10.1 years old) and randomly assigned them to either CPVI alone group (n=58) or the CPVI plus linear ablation group (posterior box + anterior line; Dallas lesion set; n=55). The primary outcome was freedom from clinical recurrence of AF after RFCA.
Results: 1. Compare to CPVI+linear ablation group, CPVI alone group required shorter procedure (185.8±57.5min vs. 212.2±63.7min, P=0.025) and ablation times (4917.7±1119.9sec vs. 6186.9±1418.7sec, P<0.001) without significant difference in procedure related major complication rate (3.4%, vs. 1.8%, P=0.590). 2. During the 18.6±11.4 months of follow-up, the clinical recurrence rates were not significantly different between CPVI alone group (19.0%) and CPVI+linear ablation group (29.1%, P=0.271). 3. AAD utility rates after RFCA were not significantly different between two groups (27.6% vs. 38.2%, P=0.316). 4. AAD free AF recurrence was not significantly different between two groups (Log-rank, P=0.208).
Conclusion: CPVI alone is an effective rhythm control strategy with shorter procedure time for PeAF who were converted as PAF with AADs after external electrical cardioversion, compared to CPVI with additional linear ablation.
Article Information
vol. 134 no. Suppl 1 A23238
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Hee Tae Yu1;
- Jaemin Shim2;
- Junbeom Park3;
- In-Soo Kim1;
- Tae-Hoon Kim1;
- Jae-Sun Uhm1;
- Boyoung Joung1;
- Moon-Hyoung Lee1;
- Young-Hoon Kim2;
- Hui-Nam Pak1
- 1Div of Cardiology, Severance Cardiovascular Hosp, Yonsei Univ College of Medicine, Seoul, Korea, Republic of
- 2Cardiology Div, Korea Univ Anam Hosp, Seoul, Korea, Republic of
- 3Cardiology Div, Ewha Womans Univ, Seoul, Korea, Republic of
Abstract 20252: Exposure to Low-Dose Ionizing Radiation From Cardiac Procedures and Risk of Malignancy in Adults With Congenital Heart Disease
Sarah Cohen, Aihua Liu, Michelle Gurvitz, Eva Goossens, Liming Guo, Judith Therrien, Ariane Marelli
Circulation. 2016;134:A20252
Abstract
Introduction: We showed that congenital heart disease (CHD) patients were exposed to increasing number of low-dose ionizing radiation (LDIR) from cardiac procedures between 1990 and 2005. We also showed an increase in prevalence of cancer among the adults with CHD (ACHD) in Quebec relative to the general population.
Hypothesis: This study aimed to measure the association between LDIR exposure and cancer incidence in ACHD patients.
Methods: We performed a nested case-control study using the Quebec CHD Database. Incident cancer cases were identified as the first cancer hospitalization from 1995 to 2010 (5-year wash-out period). Each case was matched on age, sex and calendar year with 4 controls. LDIR exposure was measured as lifetime cumulative number of LDIR cardiac procedures (cardiac catheterization, computed tomography scans of the chest, nuclear medicine and arrhythmia-related) prior to incident cancer diagnosis for each case-control pair.
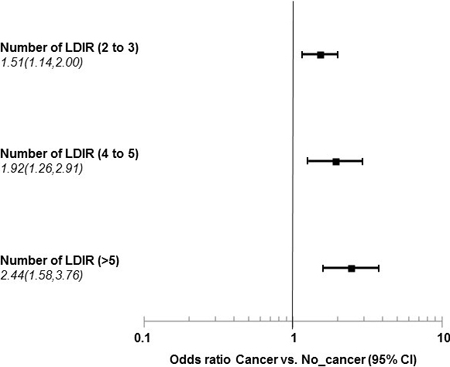
Results: A total of 2690 cancer cases were matched with 10748 controls. Genitourinary, digestive, respiratory, breast and hematological cancers were accounted for 88.2% of cancers. In a restricted population of 2052, 18-65 year olds (median age=53, IQR 43,60) with specified CHD diagnoses, each additional LDIR procedure exposure was associated with 1.1-fold (95%CI: 1.1-1.2) increase in cancer risk. The impact of LDIR exposure as a categorical variable using conditional logistic regression is shown using patients with 0 or 1 procedures as reference. A sensitivity analysis in those with hematological cancers revealed an 6.3-fold (95%CI: 1.9-21.1) increase in cancer incidence related to ≥ 6 procedures.
Conclusions: We demonstrated an association between increase in exposure to LDIR-cardiac procedures and incident cancer risk in this population-based ACHD cohort. Studies are required to further understand this possible risk and to confirm these important findings in additional data sources.
Article Information
vol. 134 no. Suppl 1 A20252
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Sarah Cohen1;
- Aihua Liu2;
- Michelle Gurvitz3;
- Eva Goossens4;
- Liming Guo2;
- Judith Therrien1;
- Ariane Marelli1
- 1McGill Adult Unit for Congenital Heart Disease Excellence, McGill Univ Health Cntr, Montréal, Canada
- 2McGill Adult Unit for Congenital Heart Disease Excellence, McGill Univ Health Cntr, Montreal, Canada
- 3Dept of Cardiology, Children’s Hosp Boston, Harvard Med Scool, Boston, MA
- 4Dept of Public Health and Primary Care, Univ of Leuven, Leuven, Belgium
Abstract 18455: Growth-Differentiation Factor 15 Predicts Adverse Cardiac Events in Adults With Congenital Heart Disease
Vivan J Baggen, Annemien E van den Bosch, Jannet A Eindhoven, Eric Boersma, Jolien W Roos-Hesselink
Circulation. 2016;134:A18455
Abstract
Introduction: Growth-differentiation factor 15 (GDF-15) is a cytokine which is strongly upregulated upon tissue injury and inflammatory states. It offers prognostic information in coronary heart disease and chronic heart failure; however, its usefulness as biomarker in adults with congenital heart disease is unknown.
Hypothesis: GDF-15 is independently associated with adverse cardiac events in adults with congenital heart disease.
Methods: We prospectively included consecutive patients who routinely visited the adult congenital cardiology outpatient clinic between April 2011 and April 2013. At the same day, patients underwent clinical examination, electrocardiography, echocardiography and venous blood sampling. Plasma GDF-15 was measured by batch analyses. The primary endpoint was a composite of ‘death or heart failure’ and the secondary endpoint was a composite of ‘death, heart failure, hospitalization, arrhythmia, thromboembolic event or cardiac re-intervention’. Cox regression was used to assess the predictive value of GDF-15, adjusted for age, sex, systemic ventricular function and NT-proBNP.
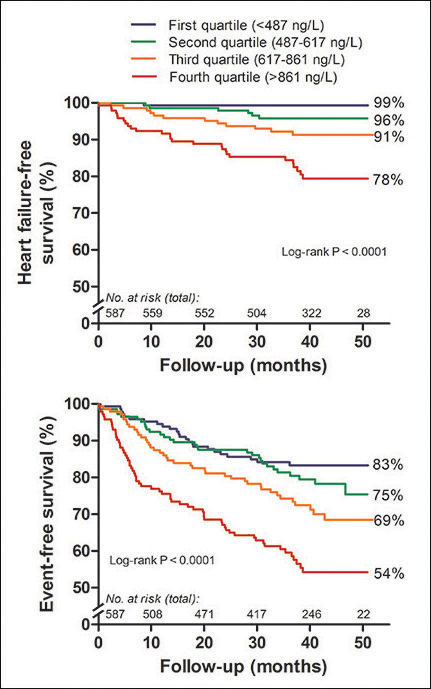
Results: In total, 587 patients were included (median age 33 [IQR 25-41] years, 58% male, 90% NYHA class I). Patients were followed for a median of 42 [IQR 37-46] months. GDF-15 was independently associated with the primary endpoint (n=48, adjusted hazard ratio per two-fold increase 1.60 [95% CI 1.13-2.26], P = 0.008) and with the secondary endpoint (n=160, adjusted hazard ratio per two-fold increase 1.34 [95% CI 1.09-1.65], P = 0.006). The discriminatory value (c-statistic) of GDF-15 for the primary and secondary endpoint was 0.79 (95% CI 0.73-0.85) and 0.64 (95% CI 0.59-0.68), respectively.
Conclusions: GDF-15 provides prognostic information, independent of age, sex, systemic ventricular function and NT-proBNP. Therefore, GDF-15 could play an important role in the monitoring and management of adults with congenital heart disease.
Article Information
vol. 134 no. Suppl 1 A18455
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Vivan J Baggen;
- Annemien E van den Bosch;
- Jannet A Eindhoven;
- Eric Boersma;
- Jolien W Roos-Hesselink
- Cardiology, Erasmus MC, Rotterdam, Netherlands
Abstract 14983: Arterial Tortuosity and Cardiovascular Outcomes in Marfan Syndrome and Loeys-Dietz Syndrome
Shaine A Morris, Nicholas A Dodd, Seitaro Oda, Kalyan Kancherla, Federico M Asch, Melissa Challman, Shelley S Andreas, William Payne, Liliana Preiss, Scott LeMaire, Richard B Devereux, Reed E Pyeritz, Kathryn W Holmes, Mary J Roman, Ronald V Lacro, Ralph V Shohet, Rajesh Krishnamurthy, Claudia Pedroza, Kim Eagle, Dianna M Milewicz
Circulation. 2016;134:A14983
Abstract
Background: Single-center research suggests that increased vertebral artery tortuosity is a biomarker of adverse cardiovascular events in young patients with Marfan and Loeys-Dietz syndromes (MFS and LDS). The objective of our study was to validate this finding in a larger, multicenter population with focus on specific cardiovascular events.
Methods: Patients were included from the National Registry of Genetically Triggered Thoracic Aortic Aneurysms and Cardiovascular Conditions (GenTAC) or our institutional Cardiovascular Genetics Clinic, with MFS or LDS (caused by TGFBR1/2 mutations) who underwent magnetic resonance or computed tomography angiography (MRA/CTA) < age 50 years that included the vertebral arteries. The vertebral artery tortuosity index (VTI) was calculated from the study including the largest proportion of the vertebral arteries. Outcomes were compared using Chi square, Wilcoxon rank sum, Poisson, and Cox regression analyses.
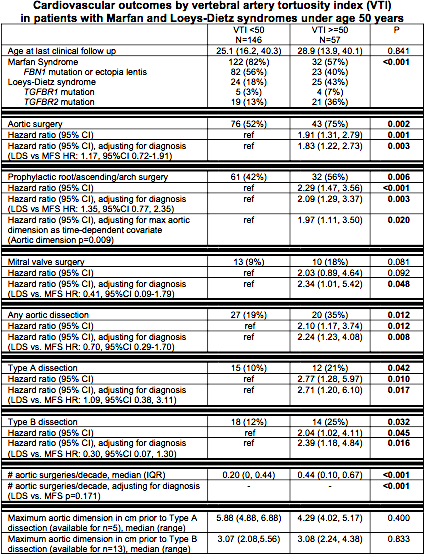
Results: A total of 203 patients were included. A VTI ≥ 50 was associated with earlier aortic surgery, earlier Type A and B aortic dissections, and more frequent aortic surgery (Table). In all multivariable models containing VTI and diagnosis, VTI retained significant association with the outcome, while the diagnosis of LDS versus MFS did not. For prophylactic aortic surgery, VTI remained significant when controlling for both diagnosis and maximum aortic dimension. Aortic dimensions were only available for 5 patients prior to Type A aortic dissection; those with VTI ≥ 50 (n=3) had a median dimension of 4.29 cm (range 4.02, 5.17) at dissection versus 5.88 cm (range 4.88,6.88) in those with VTI <50 (p=0.400).
Conclusions: In this multicenter study, VTI ≥ 50 is a marker of earlier adverse events in patients <age 50 with MFS and LDS. Further study is needed to assess whether VTI should influence treatment decisions for this population.
Article Information
vol. 134 no. Suppl 1 A14983
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Shaine A Morris1;
- Nicholas A Dodd2;
- Seitaro Oda3;
- Kalyan Kancherla4;
- Federico M Asch5;
- Melissa Challman6;
- Shelley S Andreas6;
- William Payne6;
- Liliana Preiss7;
- Scott LeMaire8;
- Richard B Devereux9;
- Reed E Pyeritz10;
- Kathryn W Holmes11;
- Mary J Roman9;
- Ronald V Lacro12;
- Ralph V Shohet13;
- Rajesh Krishnamurthy14;
- Claudia Pedroza15;
- Kim Eagle16,
- GenTAC Investigators;
- Dianna M Milewicz17
- 1Pediatric Cardiology, Baylor College of Medicine – Texas Children’s Hosp, Houston, TX
- 2Pediatric Radiology, Texas Children’s Hosp, Houston, TX
- 3Diagnostic Radiology, Kumamoto Univ, Kumamoto, Japan
- 4Cardiovascular Core Lab, Medstar Health Rsch Institute, Washington, DC
- 5Cardiovascular Core Labs, Medstar Washington Hosp Cntr, Washington, DC
- 6Cardiovascular Clinical Rsch Core, Baylor College of Medicine/Texas Children’s Hosp, Houston, TX
- 7Div of Statistics and Epidemiology, RTI International, Rockville, MD
- 8Cardiothoracic Surgery, Baylor College of Medicine/Texas Heart Institute, Houston, TX
- 9Cardiology, Weill Cornell Medicine, New York, NY
- 10Medicine (Genetics), Perelman Sch of Medicine at the Univ of Pennsylvania, Philadelphia, PA
- 11Pediatrics, Oregon Health and Science Univ, Portland, OR
- 12Cardiology, Boston CHildren’s Hosp, Boston, MA
- 13Medicine, John A. Burns Sch of Medicine/Univ of Hawaii, Honolulu, HI
- 14Pediatric Radiology, Baylor College of Medicine/Texas Children’s Hosp, Houston, TX
- 15Cntr for Clinical Rsch and Evidence-Based Medicine, McGovern Med Sch at the Univ of Texas Health Science Cntr at Houston, Houston, TX
- 16Frankel Cardiovascular Cntr, Univ of Michigan, Ann Arbor, MI
- 17Internal Medicine (Genetics), McGovern Med Sch at the Univ of Texas Health Science Cntr at Houston, Houston, TX
Abstract 12222: Patient-Reported Health and its Correlates in Adults With Congenital Heart Disease From 15 Countries
Philip Moons, Adrienne H Kovacs, Koen Luyckx, Silke Apers
Circulation. 2016;134:A12222
Abstract
Objectives: The importance of patient-reported health assessment as a critical measure of cardiovascular health has been emphasized. In adults with congenital heart disease (ConHD), geographic differences in patient-reported health are assumed, but international studies using a uniform methodology are non-existent. We sought (1) to explore patient-reported health in an international sample of adults with ConHD, and (2) to investigate the association between patient characteristics and patient-reported health.
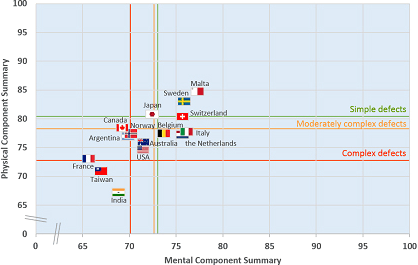
Methods: In a cross-sectional study, 4,028 patients (median age=32 y; 53% women; 26% mild, 48% moderate, 26% complex defects) from 15 countries worldwide were included. Patient-reported health was assessed using the SF-12, yielding a Physical Component Summary (PCS) and a Mental Component Summary (MCS). Patient characteristics included sex, age, marital status, educational level, employment status, ConHD complexity, and patient-reported New York Heart Association (NYHA) class. Multivariable linear regression analysis was performed.
Results: Mean PCS was 77.2 ±20.9 and mean MCS was 72.1 ±19.0, on a scale 0-100. Fig 1 shows the PCS and MCS per country (flags) and per disease complexity (lines). Malta and Sweden have the highest scores; and France, Taiwan and India have the lowest scores. Lower PCS (worse physical health) was significantly associated with female sex; older age; lack of employment; being divorced or widowed; less education; greater disease complexity; and worse NYHA class (adj. R2=0.512). Lower MCS (worse mental health) was significantly related to female sex; lack of employment; being divorced or widowed; having complex ConHD; and worse NYHA class (adj. R2=0.234).
Conclusions: International variation in patient-reported health is confirmed. The detection of both medical and sociodemographic correlates of perceived health status allow clinicians to identify patients at risk for poor health and to target resources accordingly.
Article Information
vol. 134 no. Suppl 1 A12222
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1KU Leuven Dept of Public Health and Primary Care, KU Leuven – Univ of Leuven, Leuven, Belgium
- 2OHSU Knight Cardiovascular Institute, Oregon Health & Science Univ, Portland, OR
- 3KU Leuven Sch Psychology and Child and Adolescent, KU Leuven – Univ of Leuven, Leuven, Belgium
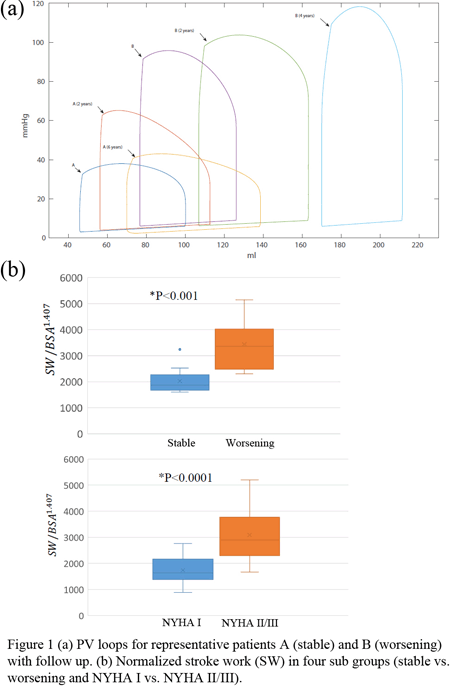
Abstract 20168: Right Ventricular Stroke Work Correlates With Outcomes in Pediatric Pulmonary Arterial Hypertension (PAH) Patients
Weiguang Yang, Alison L Marsden, Michelle T Ogawa, Keely K Phillips, Marlene Rabinovitch, Jeffrey A Feinstein
Circulation. 2016;134:A20168
Abstract
Introduction: Pulmonary arterial hypertension (PAH) is characterized by elevated pulmonary artery pressures and pulmonary vascular resistance. As no definitive treatment options exist, and lung transplant also carries significant mortality rates, optimizing treatment strategies and timing for transplant remains crucial; a quantitative measure to predict disease progression would be greatly beneficial in treatment planning.
Hypothesis: We hypothesize that right ventricular (RV) stroke work correlates with clinical worsening in PAH patients.
Methods: Pediatric patients (<18 years) with idiopathic PAH or PAH secondary to congenital heart diseases with serial, matched catheterization and magnetic resonance imaging (MRI) data were included. RV and PA hemodynamics were numerically simulated by a lumped parameter (circuit analogy) model to create patient-specific pressure-volume (PV) loops not easily replicated clinically. The model was tuned using optimization techniques to match patient-specific MRI and cath-derived RV volumes and pressures for each time point. RV stroke work was calculated from the corresponding PV loop.
Results: Eighteen patients (male: 9, average age: 9.7 years, range: 4.4-16.3 years, average follow-up: 3.9 years, range: 1.1-8.0) were enrolled. Nine patients were clinically stable during the duration of study, the remaining 9 had clinical worsening, defined by either death (n=3) or advanced disease in which IV prostacyclin was used and heart/lung transplant was indicated (n=6). Stroke work for the group with worsening symptoms/disease was significantly larger than the stable group (3430.8±930.7 vs 2029±533.9, p<0.001). Stroke work for patients in NYHA class II/III was also elevated compared to patients in class I (3087.2±963.0 vs 1739.4±566.5, p<0.0001).
Conclusion: RV stroke work correlates with symptomatic/disease worsening in pediatric PAH. Larger studies are required to validate and refine the predictive models.
Article Information
vol. 134 no. Suppl 1 A20168
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Weiguang Yang1;
- Alison L Marsden2;
- Michelle T Ogawa2;
- Keely K Phillips1;
- Marlene Rabinovitch1;
- Jeffrey A Feinstein1
- 1Pediatrics, Stanford Univ, Palo Alto, CA
- 2Pediatrics, Stanford Univ, Stanford, CA
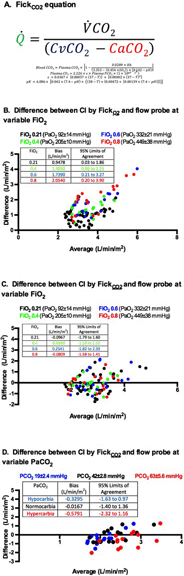
Abstract 19165: Improving Accuracy of Cardiac Output Estimates Using the Fick Principle – Oxygen versus Carbon Dioxide
Dorothy A Perry, Lindsay M Thomson, Abigail R Moore, Aditya K Kaza, John N Kheir
Circulation. 2016;134:A19165
Abstract
Introduction: The Fick principle is frequently used to estimate cardiac output (CO) in critically ill patients. These data are used to guide patient management and to estimate vascular resistance. Oxygen-based Fick (FickO2) has been shown to systematically overestimate CO. The substitution of all O2 parameters with CO2 parameters may improve the accuracy of Fick.
Objective: To compare CO as measured by (1) FickO2, (2) carbon dioxide-based Fick (FickCO2), and (3) aortic flow probe at varying O2 and CO2 tensions.
Methods: Yorkshire swine (n=8, 29-30kg) were anesthetized, intubated, and paralyzed. Instrumentation included a femoral arterial and pulmonary arterial catheters, myocardial tissue PO2 probe (Oxford Optronix), and a transit time flow probe (Transonic, Inc) placed on the aortic root via sternotomy. Indexed oxygen consumption (VO2) and carbon dioxide production (VCO2) were continuously measured (E-CAiOVX module, GE Healthcare). In separate experiments, PaO2 was varied between 100-650 mmHg, and PaCO2 between 20-80 mmHg in graded fashion. FickCO2 was calculated based on VCO2 and the veno-arterial CO2 content difference (A). Data were compared between each group to flow probe by Bland Altman analysis.
Results: FickO2 consistently overestimated cardiac index (CI) (bias 1.3 L/min/m2, SD of bias 0.75), and did so in proportion to FiO2 (B). This overestimation was explained by a correlation with both tissue PO2 and SvO2 with FiO2 (P<0.001, linear regression). FickCO2estimated CO more accurately at all PaO2 values (C) (bias -0.02 L/min/m2, SD of bias 0.84). Extremes of PaCO2 caused minimal error in FickCO2 (D) (bias -0.18 L/min/m2, SD of bias 0.82).
Conclusion: FickCO2 is more accurate than FickO2 within a range of clinically relevant ranges of PaO2 and PaCO2. FickCO2 utilizes VCO2, clinically easier variable to measure than VO2. FickCO2 may represent a translatable method for CO estimation in critically ill patients.
Article Information
vol. 134 no. Suppl 1 A19165
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Dorothy A Perry;
- Lindsay M Thomson;
- Abigail R Moore;
- Aditya K Kaza;
- John N Kheir
- Cardiology, Boston Children’s Hosp, Boston, MA
Abstract 18578: Long-term Outcome of After Percutaneous Coronary Intervension for Ischemic Heart Disease Caused by Kawasaki Disease
Yusuke Koteda, Kenji Suda, Takafumi Ueno, Shintarou Kishimoto, Yoshiyuki Kagiyama, Yushirou Yamashita
Circulation. 2016;134:A18578
Abstract
Introduction: The most important complication of Kawasaki disease (KD) is the coronary aneurysms and stenosis. Various types of percutaneous coronary intervention (PCI) have been successfully offered to alleviate ischemic coronary stenosis. However, little data is available concerning the long term outcome of these PCI.
Hypothesis: Long term outcome of PCI for KD is not great as expected and requires additional revascularization therapy.
Methods: Subjects were 22 patients (19 male and 3 female) with a history of KD who developed ischemic heart disease as a result of coronary aneurysms and were treated by PCI since 1994. Patients were evaluated regularly with CT or coronary angiography every one to five years. From medical chart, patients’ information concerning demographics, history of catheter and surgical interventions, and final outcome were collected. Based on these data, we calculated re-stenosis free rate using Kaplan-Meier’s analysis.
Results: Subject’s age at onset was 2.3 ± 2.4 years old and median observational period was 9.9 years (range 0.2-21.8 years). PCI was applied on #6 (n = 9), #1 (n = 8), #2 (n = 4), and #5 (n = 1) of coronary arteries. PCI included percutaneous transluminal coronary rotational ablation (PTCRA) (n=16), plain old balloon angioplasty (POBA) (n=3), PTCRA+coronary artery stenting (n=2), and coronary artery stenting(n=1). In the follow-up period, 10 (45%) patients showed re-stenosis. Of 10 patients, 8 patients underwent additional PTCRA (n=5), POBA (1), stent placement (1), and coronary bypass graft surgery (CABG)(1). In the remaining 2 patients that showed total occlusion of target vessel (#1), 1 patient has been scheduled for PCI and the other treated medically because of sufficient collateral communications. Re-stenosis free year was 0.1, 0.2, 0.3, 0.3, 0.6, 2.6, 2.9, 10.2, 14.6, 21.7 years, giving re-stenosis free rate of 68% at 5 years after PCI. Only 1 patient who previously underwent CABG and had stenosis on #5 died at 2nd PTCRA because of acute myocardial infarction and the remaining 21 patients survived with a median age of 24.8 years old, giving 5years survival rate of 95%.
Conclusions: Long-term outcome of PCI for KD can be acceptable, but meticulous management looking for re-stenosis soon after the procedure is mandatory.
Article Information
vol. 134 no. Suppl 1 A18578
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Yusuke Koteda1;
- Kenji Suda1;
- Takafumi Ueno2;
- Shintarou Kishimoto1;
- Yoshiyuki Kagiyama1;
- Yushirou Yamashita1
- 1Pediatrics & Child Health, Kurume Univ Sch of Medicine, Kurume, Japan
- 2Cardiology, Kurume Univ Sch of Medicine, Kurume, Japan
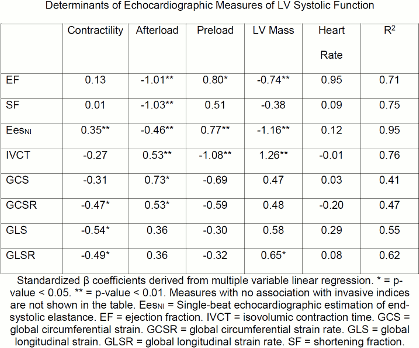
Abstract 18823: Longitudinal Measures of Deformation Are Associated With a Novel Composite Measure of Contractility Derived From Pressure-Volume Loop Analysis in Children
Shahryar M Chowdhury, Ryan Butts, Carolyn Taylor, Varsha Bandisode, Karen Chessa, Anthony Hlavacek, Arni Nutting, Girish Shirali, George H Baker
Circulation. 2016;134:A18823
Abstract
Introduction: The relationship between echocardiographic measures of left ventricular (LV) systolic function and reference-standard measures have not been assessed in children. The objective of this study was to assess the validity of echocardiographic indices of LV systolic function via direct comparison to a novel composite measure of contractility derived from pressure-volume loop (PVL) analysis.
Methods: Children with normal loading conditions undergoing routine left heart catheterization were prospectively enrolled. PVLs were obtained via conductance catheters. A novel invasive composite contractility index (ICCI) was developed using data reduction strategies to combine four measures of contractility derived from PVL analysis. Similar strategies were used to develop composites of preload and afterload. Echocardiograms were performed immediately after PVL analysis under the same anesthetic conditions. Conventional and speckle-tracking echocardiographic measures of systolic function were measured.
Results: Of 24 patients, 18 patients were heart transplant recipients, 6 patients had a small patent ductus arteriosus or small coronary fistula. Mean age was 9.1 ± 5.6 years. Upon multivariable regression, longitudinal strain was associated with ICCI (β = -0.54, p = 0.02) while controlling for indices of preload, afterload, heart rate, and LV mass under baseline conditions. Ejection fraction and shortening fraction were associated with LV mass and load indices, but not contractility. Comprehensive results can be found in the table.
Conclusion: We developed a novel measure of contractility, the ICCI, in children. Speckle-tracking derived longitudinal strain is associated ICCI in children with normal loading conditions. Longitudinal strain appears to be an accurate surrogate for LV contractility under baseline conditions in children.
Article Information
vol. 134 no. Suppl 1 A18823
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Shahryar M Chowdhury1;
- Ryan Butts1;
- Carolyn Taylor1;
- Varsha Bandisode1;
- Karen Chessa1;
- Anthony Hlavacek1;
- Arni Nutting1;
- Girish Shirali2;
- George H Baker1
- 1Pediatrics, Med Univ of South Carolina, Charleston, SC
- 2Ward Family Heart Cntr, Mercy Children’s Hosp, Kansas City, MO
Abstract 18075: Mechanical Properties of Stents and Blood Vessels to Determine a Safe Strategy to Unzip Stents Within Growing Blood Vessels
Shyam K Sathanandam, T.K. Susheel Kumar, Deepthi Hoskoppal, Saradha Subramanian, Christopher Knott-Craig, Rush Waller
Circulation. 2016;134:A18075
Abstract
Introduction: Unzipping of a stent is the technique by which a stent is fractured longitudinally using angioplasty balloons. This can allow for the stent to be further redilated and for implantation of a larger diameter stent within it. The technique may be useful in treating stenosis of infant blood vessels. The effectiveness and safety of unzipping stents depends in part on the mechanical properties of the stent and the blood vessel as well as the surrounding structures, the understanding of which is limited.
Hypothesis: Unzipping of stents can be effective and safe if the appropriate stent is implanted in the appropriate blood vessel.
Methods: 60 stents (7 stent types) were implanted in 12 neonatal piglets into different blood vessels. 3 months later, unzipping was attempted by dilating the stents till either the stent fractured or the vessel was injured. The ultimate tensile strength (UTS) of the different stent and vessel types was calculated. 6 piglets were sacrificed to determine histologic grade of vessel injury. The other 6 were survived to determine long term effects of unzipping.
Results: The mean UTS of various stent and vessel types tested is represented in Figure 1. The Genesis and Blue stents had the highest UTS, greater than any blood vessel and therefore, not suitable for unzipping. The Protégé stent had the least UTS but fractured in a disorganized fashion and did not unzip. The VeriFlex, Valeo, Express and Formula stents are perhaps best suited for unzipping as they did not result in significant vessel injury. One piglet developed a pseudoaneurysm on long term follow up. 2 distinct types of vessel injuries and 4 histologic grades of these injuries was developed from this study.
Conclusions: This study may help chose the appropriate stent to implant in an infant with a stenotic blood vessel if the intent is to unzip the stent in the future. The unzipped segment may require reinforcement with another stent implanted within it in order to prevent formation of a pseudoaneurysm.

Article Information
vol. 134 no. Suppl 1 A18075
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Shyam K Sathanandam1;
- T.K. Susheel Kumar2;
- Deepthi Hoskoppal3;
- Saradha Subramanian1;
- Christopher Knott-Craig1;
- Rush Waller1
- 1Pediatrics, Univ of Tennessee, Memphis, TN
- 2Surgery, Univ of Tennessee, Memphis, TN
- 3Pathology, Univ of Tennessee, Memphis, TN
Abstract 15978: Variability of Practice Patterns in Device Closure of Atrial Septal Defects and Patent Ductus Arteriosus: An Analysis of Data From the Impact® Registry
Michael L O’Byrne, Kevin F Kennedy, Jonathan J Rome, Andrew C Glatz
Circulation. 2016;134:A15978
Abstract
Introduction: The IMPACT® registry provides the first opportunity to measure practice variation in trans-catheter interventions for congenital heart disease, specifically device closure of atrial septal defect (ASD) and patent ductus arteriosus (PDA).
Methods: ASD and PDA cases in IMPACT® from 1/2011 to 9/2015 were included. We used hierarchical multivariable models to adjust for patient characteristics and identify variability by center, assessing the distribution of indications for closure and, in cases whose indication was right (RVVO) or left ventricular volume overload (LVVO), the factors influencing probability of a ratio of pulmonary to systemic blood flow (Qp:Qs) >1.5:1 and of a small defect (ASD <5mm or PDA<2mm).
Results: 4459 ASD and 5233 PDA cases at 77 centers were included. The indications for ASD closure were RVVO (84%) and stroke prevention (13%), and varied by region (4% stroke prevention in the Northeast and 19% in the South, p<0.001). Indications for PDA closure were LVVO (57%), endocarditis prevention (36%), and pulmonary hypertension (7%). For both procedures: region, hospital setting, and hospital-type had significant influence on the distribution of indications for closure after adjusting for patient-level factors. There was also significant variability in indications between centers for ASD and PDA closure (p<0.001). Among LV/RVVO cases, the probability of a Qp:Qs>1.5:1 increased with increasing PDA/ASD volume (p=0.04, 0.05). For ASD, the probability of a Qp:Qs>1.5:1 decreased at centers with a larger proportion of adult cases (p=0.007). In multivariable models there was no inter-center variability in closing small ASD (p=0.17). In comparison, small PDA comprised >30% of cases at 30% of centers. After adjusting for patient characteristics, there was significant inter-center variability in closure of small PDA (median rate ratio: 1.4, p<0.001). Increasing annual catheterization volume was associated with a lower proportion of small PDA closures for LVVO (p=0.02).
Conclusion: There are center-level differences in the practice of ASD and PDA device closure even after adjustment for covariates, with greater variability in PDA closure. This suggests differences in the treatment of similar patients based on center factors.
Article Information
vol. 134 no. Suppl 1 A15978
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Cardiology, Children’s National Med Cntr, Washington, DC
- 2CV Rsch, Mid America Heart Institute, Kansas City, MO
- 3Pediatrics Div of Cardiology, The Children’s Hosptial of Philadelphia, Philadelphia, PA
- 4Pediatric Div of Cardiology, The Children’s Hosp of Philadelphia, Philadelphia, PA
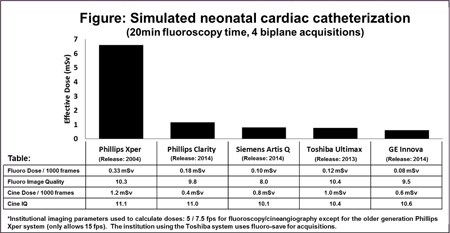
Abstract 12670: Variability in Radiation Dose and Image Quality: A Comparison Across Fluoroscopy-system Vendors and Generations of Equipment
Kevin D Hill, Michael P Carboni, Thomas P Doyle, Salim Idriss, Dana Janssen, George Nicholson, Shyam Sathanandam, Steve Mann, Gregory Fleming
Circulation. 2016;134:A12670
Abstract
Introduction: Increased recognition of the potentially harmful effects of ionizing radiation has spurred technological advances to reduce exposure during fluoroscopy. However there is currently little understanding of the dose-image quality (IQ) relationship between fluoroscopy vendors and across generations of equipment used for imaging during pediatric catheterization.
Methods: We evaluated latest generation fluoroscopy systems from Phillips, Siemens, GE and Toshiba, and an older generation Phillips system (2004 release). Fluoroscopy and cineangiography were performed on a tissue simulation anthropomorphic phantom using a standardized imaging approach. Phantom surface exposures were used for Monte Carlo simulations to calculate radiation effective dose, accounting for differences in beam parameters. We also imaged a fluoroscopy IQ phantom to assess contrast-detail and line-per-inch visualization. IQ images were scored by 3 blinded reviewers with scores averaged to produce a composite rating (scale 0-18). To assess the impact of imaging approach we then simulated a neonatal cardiac catheterization incorporating “typical” imaging protocols provided by institutions using the various systems.
Results: Effective doses and IQ scores are summarized in the table. Effective doses varied by >400% with the older generation system consistently delivering markedly higher doses. The associated figure summarizes dose and IQ for a simulated neonatal cardiac catheterization which accounts for measured doses as well as the reported institutional imaging parameters summarized in the figure legend.
Conclusion: These data demonstrate substantial technological improvements in fluoroscopy equipment and may be useful to justify institutional “upgrades”. Comparing latest generation systems across vendors and institutions, we found variability in the dose-IQ relationship that reflects both equipment and imaging approach.
Article Information
vol. 134 no. Suppl 1 A12670
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Kevin D Hill1;
- Michael P Carboni1;
- Thomas P Doyle2;
- Salim Idriss1;
- Dana Janssen3;
- George Nicholson3;
- Shyam Sathanandam4;
- Steve Mann5;
- Gregory Fleming1
- 1Pediatrics, Duke Univ Med Cntr, Durham, NC
- 2Pediatrics, Vanderbilt Univ Med Cntr, Nashville, TN
- 3Pediatrics, Vanderbilt Univ Med Cntr, Durham, NC
- 4Pediatrics, LeBonheur Children’s Hosp, Memphis, TN
- 5Radiology, Duke Univ Med Cntr, Durham, NC
Abstract 20075: Post-transplant Outcomes for Congenital Heart Disease Patients Bridged to Transplant With Ventricular Assist Deivces
Raheel Rizwan, Chet Villa, Farhan Zafar, Dennis Wells, Roosevelt Bryant, Clifford Chin, Angela Lorts, David L Morales
Circulation. 2016;134:A20075
Abstract
Introduction: Ventricular assist devices (VAD) use as a bridge-to-transplant (BTT) for children of congenital heart disease (CHD) with end-stage heart failure is challenging, yet has been increasingly described. However, its impact on post-transplant outcomes is unknown. This study describes the post-transplant outcomes of CHD patients BTT with a VAD.
Methods: United Network of Organ Sharing database from January 1, 2006 to June 30, 2015 was analyzed for all CHD patients undergoing heart transplantation. Patients were divided into two groups based on VAD use and presence of CHD; +CHD/+VAD and +CHD/-VAD. Pre transplant characteristics and post-transplant outcomes were compared between the groups. +CHD/+VAD post-transplant survival was also compared with -CHD/+VAD and -CHD/-VAD cohorts.
Results: There were 1871 heart transplant recipients who had CHD, 72% (1348) were < 18yo. Median age was 6y [IQR; 0-20y] and 41% (773) were females. One hundred and forty three (7.6%) of CHD heart transplant recipients were BTT with a VAD (+CHD/+VAD). Overtime, there has been a 3-fold increase in VAD utilization for CHD patients undergoing heart transplantation [Figure]. Pre-transplant, +CHD/+VAD compared to +CHD/-VAD had a worse functional status (p=0.004), a higher incidence of dialysis (13% vs 2.5%; p<0.001), infection (29% vs 14%; p=<0.001) and ventilator support (20% vs 13%; p=0.029). Overall, 1y (84% vs 87%) and 5y (72% vs 75%) survival are same for +CHD/+VAD and +CHD/-VAD (p>0.05). Also, 1y and 5y Kaplan-meier survival was not different when comparing +CHD/+VAD with -CHD/+VAD and -CHD/-VAD. [Table]
Conclusion: Although more ill pre-transplant, CHD patients BTT with a VAD have similar post-transplant outcomes compared to CHD patients without a VAD and to other heart transplant patients. Therefore, VAD support in CHD patients may negate certain risk factors for poor post-transplant outcomes in this challenging cohort.

Article Information
vol. 134 no. Suppl 1 A20075
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Raheel Rizwan1;
- Chet Villa1;
- Farhan Zafar1;
- Dennis Wells2;
- Roosevelt Bryant1;
- Clifford Chin1;
- Angela Lorts1;
- David L Morales1
- 1The Heart Institute, Cincinnati Children’s Hosp Med Cntr, Cincinnati, OH
- 2Cardiothoracic Surgery, Univ of Cincinnati College of Medicine, Cincinnati, OH
Abstract 20368: Congestive Heart failure in Adults With Congenital Heart Diseases: What Predicts it and How Does it Affect Mortality?
Sarah Cohen, Aihua Liu, Liming Guo, Judith Therrien, Ariane J Marelli
Circulation. 2016;134:A20368
Abstract
Introduction: Adults with congenital heart disease (ACHD) are not cured and residual disease predispose them to congestive heart failure (CHF). This study aimed to calculate the cumulative probability of CHF, identify predictors of one-year risk of CHF and assess the impact of CHF on mortality.
Methods: A retrospective cohort of 27975 was constructed consisting of patients from the Quebec Congenital heart disease (CHD) database aged 18-65 between 1995 and 2010. We calculated the cumulative probability of CHF hospitalization using the Practical Incidence Estimator macro adjusting for the competing risk of death. We conducted regression analyses to identify the predictors of one-year risk of CHF hospitalization. To assess the impact of CHF hospitalization on mortality, we used propensity score matching (age, sex, CHD lesion, hypertension, arrhythmia, diabetes, coronary artery disease, chronic kidney disease, endocarditis, and cardiac surgery) to select random controls for each CHF hospitalized patient.
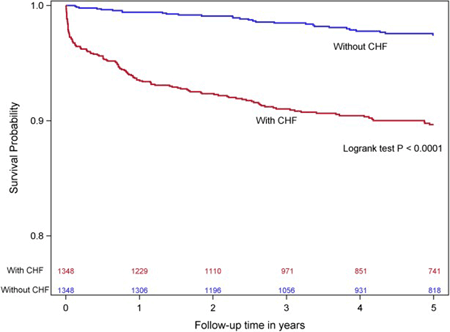
Results: The cumulative probability of CHF hospitalization by age 65 was 33.2%. Age, sex, CHD severity, CHF hospitalization history and comorbidities including arrhythmia, pulmonary hypertension, and coronary heart disease in the previous 12 months were predictive of one-year CHF hospitalization. CHF hospitality is associated with 5 fold increase in mortality risk (Hazard Ratio=5.4, 95% CI=3.5, 8.3). The impact of CHF hospitalization on the 5-year cumulative probability of survival is shown.
Conclusions: CHF hospitalization was strongly associated with death in ACHD population. ACHD patients at older age, of male sex, with severe native CHD lesion, previous CHF history, or comorbidities are at increased risk of having CHF hospitalization within a year. These data will be used to calculate a clinically useful risk score for CHF hospitalization to identify patients for accelerated referral to specialized ACHD centers.
Article Information
vol. 134 no. Suppl 1 A20368
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- McGill Adult Unit for Congenital Heart Disease Excellence, McGill Univ Health Cntr, Montréal, Canada
- McGill Adult Unit for Congenital Heart Disease Excellence, McGill Univ Health Cntr, Montreal, Canada
Abstract 17841: Heart or Heart and Lung Transplantation for Patients With Congenital Heart Disease in England: Outcomes and Future Predictions
Konstantinos Dimopoulos, Kavitha Muthiah, Rafael Alonso-Gonzalez, Stephen J Wort, Gerhard P Diller, Michael A Gatzoulis, Aleksander Kempny
Circulation. 2016;134:A17841
Abstract
Introduction: Increased longevity in patients with congenital heart disease (CHD) is associated with an increase in long-term complications, mainly heart failure, which may not be amenable to surgical or medical therapy and should trigger referral for transplantation. We assessed the current role and future prospects of heart and heart-lung transplantation in CHD patients in England.
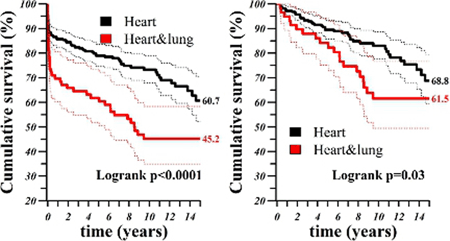
Methods and Results: We performed retrospective analysis of hospital episodes for England from 1997 to 2015, identifying CHD patients (ICD-10 “Q2x.x” codes), who underwent heart or heart and lung transplantation. In total, 469 transplants (82.2% heart and 17.8% heart-lung) were performed in 444 patients. Median age at first transplantation was 19.5 years, range 0-63.6 years, and was higher in heart-lung recipients (p<0.0001). One half of patients transplanted had CHD of less the severe (Bethesda) complexity and this number increased over time (p=0.001). Over time, the proportion of heart-lung transplants declined (p<0.0001) and the proportion of transplants performed in adults did not increase. Mortality was high during the first year (14.3% heart and 30.4% heart-lung), especially after heart-lung transplantation, but remained relatively low thereafter (21.1% heart and 38.2% heart-lung at 5 years, Figure left). Conditional survival 3 months post-transplant shown on Figure right). Older age and heart-lung transplantation were strong predictors of death. The number of transplants is predicted to increase by about a third over the next five years.
Conclusions: The current and future predicted increase in the numbers of CHD transplants in the UK does not appear to parallel the expansion of the CHD population, especially in adults. Investment should be made to establish national adult CHD transplant teams.
Article Information
vol. 134 no. Suppl 1 A17841
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Konstantinos Dimopoulos1;
- Kavitha Muthiah2;
- Rafael Alonso-Gonzalez1;
- Stephen J Wort1;
- Gerhard P Diller1;
- Michael A Gatzoulis1;
- Aleksander Kempny1
- 1Adult Congenital Heart Cntr & Cntr for Pulmonary Hypertension, Royal Brompton, London, United Kingdom
- 2Adult Congenital Heart Disease Unit, St. Bartholomew’s Hosp, London, United Kingdom
Abstract 18025: No Improvement in Outcomes for Adults With Congenital Heart Disease Listed for Heart Transplantation at the Lowest Priority Status in the United States 1986 – 2014
Laith Alshawabkeh, Knute D Carter, Heather L Bartlett, Alexander R Opotowsky
Circulation. 2016;134:A18025
Abstract
Introduction: Advances in medical therapy have improved survival for patients with chronic heart failure (HF), including those listed at low priority for heart transplantation. Adults with congenital heart disease (ACHD/CHD) are at risk of heart failure as they age but, unlike in those without CHD, there are no disease-specific evidence based medical therapies.
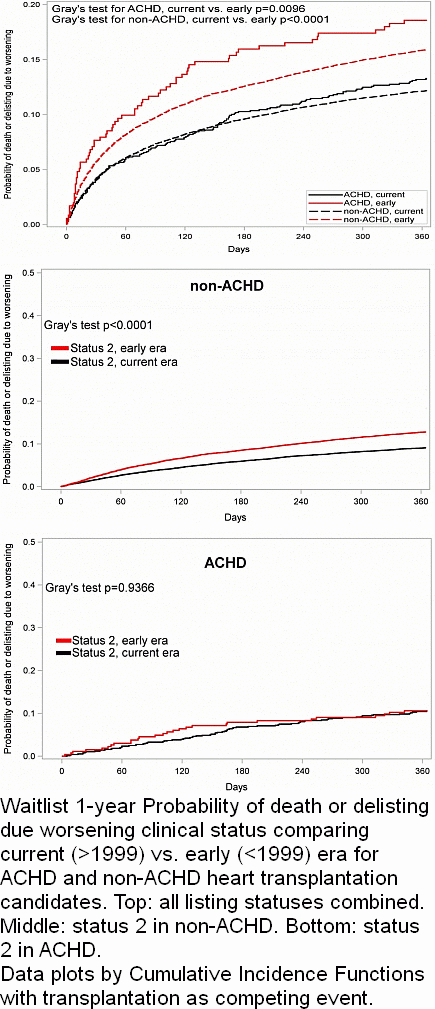
Hypothesis: The probability of adverse outcomes (death or delisting due to clinical worsening) for ACHD listed at status 2 did not improve over time, in contrast to the trend for patients without CHD.
Methods: This was a retrospective study that used the Scientific Registry for Transplant Recipients database on participants ≥ 18 years old listed for heart transplantation in the United States between 1986 and 2014. Cumulative incidence functions were used to estimate 1-year probability of death or delisting due to clinical worsening, with transplantation as a competing outcome.
Results: Among ACHD heart transplantation candidates, there were 359 and 1,290 listed before and after 1999; this figure was 22,110 and 38,557 for non-ACHD, respectively. There was improvement in the probability of the primary outcome in the current compared to the early era for both ACHD (13.2% vs. 18.6%, p=0.01) and non-ACHD (12.1% vs. 15.9%, p<0.0001) patients. However, this improvement was unevenly distributed. While there was an improvement for non-ACHD listed at status 2 in the current vs. the early era (9.0% vs. 12.8%, p=0.005), this improvement was not apparent for ACHD patients (10.4% vs. 10.6%, p=0.94), Figure.
Conclusions: Despite advances in care for patients without CHD, there has been no improvement in adverse outcomes for ACHD patients listed for heart transplantation as status 2. Absence of proven medical therapy for chronic HF in ACHD likely explains these findings. Risk stratification is challenging in the absence of data on prognostic markers in this seemingly, but perhaps misleadingly, more stable group of patients.
Article Information
vol. 134 no. Suppl 1 A18025
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Cardiology, Boston Adult Congenital Heart (BACH) Program, Boston Children’s and Brigham & Women’s Hosps, Harvard Med Sch, Boston, MA
- 2Biostatistics, Univ of Iowa, Iowa City, IA
- 3Pediatrics and Medicine, Univ of Wisconsin, Madison, WI
- 4Cardiology, Boston Children’s and Brigham & Women’s Hosps, Harvard Med Sch, Boston, MA
Abstract 17178: The Influence of Fontan-associated Protein-losing Enteropathy on Outcomes in Patients Referred for Heart Transplant: a Multicenter Study
Kurt R Schumacher, Sunkyung Yu, Ray Lowery, Ryan J Butts, Chesney Castleberry, Sharon Chen, Erik Edens, Justin Godown, Jonathan N Johnson, Mariska Kemna, Kimberly Y Lin, Kathleen Simpson, Shawn West, Ivan Wilmot, Jeffrey G Gossett
Circulation. 2016;134:A17178
Abstract
Introduction: Fontan-associated protein-losing enteropathy (PLE) is an indication for heart transplant (HTx). Timing of referral varies widely, and the influence of PLE’s severity, duration, and treatment on HTx outcomes is unknown.
Hypothesis: Long-standing PLE and PLE requiring more intensive therapy are associated with increased post-HTx mortality.
Methods: This is a 12-center, retrospective cohort study of all post-Fontan pts with PLE referred for HTx from 2003-2015. Demographic, medical, surgical, and catheterization, as well as PLE-specific data, including duration of disease, intensity and details of treatment, hospitalizations, growth, and complications, were collected. Factors associated with waitlist and post-HTx outcomes including death, rejection, infection, and PLE resolution were sought.
Results: Eighty pts (median 5/center, range 1-20) were referred for HTx evaluation. Median time from Fontan to PLE diagnosis was 4.5 yr (IQR 1.2-8.6 yr) and from diagnosis to evaluation was 1.5 yr (IQR 0.3-6.5 yr). Of 68 pts listed for HTx, 8 were removed due to deterioration, 4 died waiting, and 4 remain listed. In 52 pts undergoing HTx, median time from PLE diagnosis to HTx was 2.4 yr (IQR 1-4.6 yr). Post-HTx 1-mo survival was 92% and 1-yr was 83%. PLE-specific factors including duration of PLE prior to HTx, pre-HTx hospitalizations, need for/frequency of albumin replacement, PLE-specific therapies, and weight or height z-score had no association with post-HTx mortality. Deviation from institution standard post-HTx immunosuppressant regimen was associated with increased mortality (p=.04). Specifically, withholding MMF, azathioprine, or mTOR inhibitor occurred in 56% of deaths vs. 9% of survivors (p=.005). Rejection (53%) and infection (44%) at any time post-HTx were common, but not associated with PLE-specific factors. PLE resolved completely in all but one HTx survivor at a median of 1 mo (IQR 1-3, range 0-20 mo). Duration, severity, or prior treatment did not affect time to PLE resolution.
Conclusions: Individuals with PLE have a risk of post-HTx mortality similar to published outcomes for other Fontan pts, and PLE resolves in nearly all survivors. PLE severity, duration, and treatment do not influence post-HTx outcome.
Article Information
vol. 134 no. Suppl 1 A17178
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Kurt R Schumacher1;
- Sunkyung Yu1;
- Ray Lowery1;
- Ryan J Butts2;
- Chesney Castleberry3;
- Sharon Chen4;
- Erik Edens5;
- Justin Godown6;
- Jonathan N Johnson7;
- Mariska Kemna8;
- Kimberly Y Lin9;
- Kathleen Simpson3;
- Shawn West10;
- Ivan Wilmot11;
- Jeffrey G Gossett12
- 1Dept of Pediatrics, Div of Cardiology, Univ of Michigan, Ann Arbor, MI
- 2Dept of Pediatrics, Div of Cardiology, Med Univ of South Carolina, Charleston, SC
- 3Dept of Pediatrics, Div of Cardiology, St. Louis Children’s Hosp, St. Louis, MO
- 4Dept of Pediatrics, Div of Cardiology, Stanford Univ, Palo Alto, CA
- 5Dept of Pediatrics, Div of Cardiology, Univ of Iowa, Iowa City, MI
- 6Dept of Pediatrics, Div of Cardiology, Vanderbilt Univ, Nashville, TN
- 7Dept of Pediatrics, Div of Cardiology, Mayo Clinic, Rochester, MN
- 8Dept of Pediatrics, Div of Cardiology, Seattle Children’s Hosp, Seattle, WA
- 9Dept of Pediatrics, Div of Cardiology, Children’s Hosp of Philadelphia, Philadelphia, PA
- 10Dept of Pediatrics, Div of Cardiology, Children’s Hosp of Pittsburgh, Pittsburgh, PA
- 11Dept of Pediatrics, Div of Cardiology, Cincinnati Children’s Hosp Med Cntr, Cincinnati, OH
- 12Dept of Pediatrics, Div of Cardiology, Lurie Children’s Hosp, Chicago, IL
Abstract 20492: Long Term Outcomes After Surgical Repair of Tetralogy of Fallot (TOF): A Study From the Pediatric Cardiac Care Consortium (PCCC)
Clayton Smith, Michael Kelleman, Courtney McCracken, Andreas Kalogeropoulos, Cassandra Sung, Matthew Oster, Logan Spector, James Moller, Lazaros Kochilas
Circulation. 2016;134:A20492
Abstract
Introduction: TOF can exist either in simple (without association with other lesions) or in complex form when associated with absent pulmonary valve (TOF-APV), complete atrioventricular canal (TOF-CCAVC) or pulmonary atresia (TOF-PA). Surgical repair is feasible in all forms, but risks for long term outcomes can be different depending on the substrate of the TOF. We examined the long term vital status and risk of transplantation of patients registered in PCCC with repaired TOF.
Methods: We identified 3,841 and 1,878 patients surviving after simple and complex TOF repair between 1982 and 2003. Of these 3,302 and 1,619 respectively had direct identifiers sufficient for submission to the National Death Index (NDI) and United Network for Shared Organs (UNOS) datasets to determine vital and transplant status through 2014. Kaplan Meier (KM) transplant-free survival curves and hazard of mortality were calculated for comparisons between groups.
Results: 275 deaths (8.3%) occurred in simple TOF and 199 (19.0%) in complex TOF during a median follow-up period of 19.4 years (IQR: 14.9-24.4 years). There were 11 heart transplants in simple TOF and 11 transplants (7 heart, 3 heart-lung and 1 lung) for complex TOF. Each complex cohort had a higher hazard of mortality than simple TOF: TOF-APV 3.27 (95% CI: 2.39-4.49, p<0.001), TOF-CCAVC 4.21 (95% CI: 3.14-5.63, p<0.001) and TOF-PA 2.8 (95% CI: 2.37-3.32, p<0.001). Hazard of mortality for those with a genetic defect was 3.13 (95% CI: 2.38-4.12, p<0.001) and 1.82 (95% CI: 1.47-2.25, p<0.001) times higher than for those without identifiable genetic condition for simple and complex TOF respectively.
Conclusions: 20 year transplant-free survival for patients with repaired simple and complex TOF reaches 91.7% and 81% respectively. These results provide a conservative estimate of expected outcomes for these groups of patients. In depth analysis is underway for risk factors and specific diagnoses affecting mortality.
Article Information
vol. 134 no. Suppl 1 A20492
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Clayton Smith1;
- Michael Kelleman1;
- Courtney McCracken1;
- Andreas Kalogeropoulos2;
- Cassandra Sung3;
- Matthew Oster1;
- Logan Spector4;
- James Moller5;
- Lazaros Kochilas1
- 1Pediatrics, Emory Univ, Atlanta, GA
- 2Internal Medicine / Cardiology, Emory Univ, Atlanta, GA
- 3Pediatrics, Univ of Minnesota, Minneapolis, MN
- 4Pediatrics, Univ Of Minnesota, Minneapolis, MN
- 5Internal Medicine, Univ Of Minnesota, Minneapolis, MN
Abstract 20112: Lateral Tunnel and Extra-Cardiac Fontan Operations Have Equivalent Early and Late Outcomes in the Modern Era
Simone Bartelse, S. L Roche, William G Williams, Candice Silversides, Rachel Wald, Erwin Oechslin, Jack Colman, Michael Gritti, Eric Pham-Hung, Glen S Van Arsdell, Christopher A Caldarone, John Coles, Osami Honjo, Edward J Hickey
Circulation. 2016;134:A20112
Abstract
Introduction: Controversy continues regarding lateral tunnel (LT) versus extra-cardiac (EC) Fontan’s. Although we currently perform EC, there was a broad transition period. We aimed to compare long-term outcomes after LT or EC.
Methods
- Total surgical experience: Of 906 Fontan operations (1976-2014), 223 were LT (1987-2005) and 412 EC (1995-2014) (median f/u 8.3 years; range 0-29). Survival and re-operations (including revisions, transplants and pacemakers) were compared.
- Adults: Our ACHD program follows 102 LT and 78 EC (median 23 years post-Fontan; range 18-40). All were reviewed and risk-adjusted comparisons were made. Additional comparisons used propensity-matched pairs near-identical by diagnosis, morphology, age and era (LT=36, EC=36, parametric greedy matching, c-statistic .885).
Risk-adjustment was via parametric multivariable models and competing risks techniques, with bootstrapping.
Results
- Early peri-operative mortality after Fontan was strongly era-dependent (P<.0001). Early mortality after LT was significantly higher (13% versus 3% within 1 year, P<.0001). One year after Fontan, long-term attrition was no different between LT and EC. Once adjusted for era, long-term survival, freedom from re-operations, pacemaker or transplant was not different between LT and EC.
- Adults with LT and EC exhibit comparable risk-adjusted late outcomes (table, figure) by i) unadjusted comparisons, ii) risk-adjusted comparisons and iii) propensity-matched comparisons.
Conclusions: LT and EC in the modern era have equivalent early and late outcomes to 30 years including survival, re-operation, cardiopulmonary function, arrhythmia and Fontan failure.
Article Information
vol. 134 no. Suppl 1 A20112
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Simone Bartelse1;
- S. L Roche2;
- William G Williams1;
- Candice Silversides2;
- Rachel Wald2;
- Erwin Oechslin2;
- Jack Colman2;
- Michael Gritti1;
- Eric Pham-Hung1;
- Glen S Van Arsdell1;
- Christopher A Caldarone1;
- John Coles1;
- Osami Honjo1;
- Edward J Hickey1
- 1Cardiovascular Surgery, The Hosp for Sick Children, Toronto, Canada
- 2Cardiology, Toronto General Hosp, Toronto, Canada
Abstract 19888: Prognostic Effects of Pulmonary Valve Replacement in Repaired Tetralogy of Fallot: Results From a Large Multicenter Study
Jouke P Bokma, Barbara J Mulder, Kelsey Hickey, Sonya V Babu-Narayan, Rachel M Wald, Michael A Gatzoulis, Lynn A Sleeper, Tal Geva, Anne M Valente
Circulation. 2016;134:A19888
Abstract
Introduction: The prognostic impact and optimal timing of pulmonary valve replacement (PVR) in repaired tetralogy of Fallot (rTOF) remains a subject of debate. The objective of this study was to determine whether PVR was associated with beneficial outcome.
Methods: In this multicenter, case-controlled study, clinical, ECG, cardiac magnetic resonance (CMR) and outcome data of rTOF patients were collected. A propensity score for PVR was created to adjust for baseline differences between PVR and non-PVR patients. A frailty failure time model was used to determine the association of PVR, with matching on propensity score and adjustment for other risk factors, on time to the composite of death/sustained ventricular tachycardia (VT). In addition, differential association between impact of PVR and outcome according to predefined ‘proactive’ and ‘conservative’ (see figure) criteria was studied.
Results: A total of 440 PVR patients (age 24±13 years at baseline CMR, 58% male, RV ejection fraction (EF) 47±8%, QRS duration 148±27ms) and 537 non-PVR patients (age 29±15 years, 53% male, RV EF 51±8%, QRS duration 140±27ms) were included. During follow-up of 5.3±3.1 years, 41 events occurred (30 death, 11 sustained VT). The adjusted hazard ratio (HR) for death/sustained VT for patients with versus without PVR was 0.65 (95% CI: 0.31, 1.36, p=0.25). There was an increasing hazard of event across prespecified ordered PVR x criteria subgroups (Figure; P=0.044 for proactive, P=0.002 for conservative). There was a two-fold risk (hazard ratio=2.15, 95% CI: 1.34, 3.46) comparing each adjacent subgroup, suggesting benefit of PVR when conservative criteria were met, and lack of benefit of PVR when criteria were not met. A roughly similar pattern was seen according to proactive criteria.
Conclusions: In this multicenter, 5-year follow-up study in patients with rTOF, conservative guidelines seemed useful in selecting patients for PVR. Longer follow-up is necessary to confirm these findings.
Article Information
vol. 134 no. Suppl 1 A19888
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Jouke P Bokma1;
- Barbara J Mulder1;
- Kelsey Hickey2;
- Sonya V Babu-Narayan3;
- Rachel M Wald4;
- Michael A Gatzoulis3;
- Lynn A Sleeper5;
- Tal Geva5;
- Anne M Valente5
- 1Cardiology, Academic Med Cntr, Amsterdam, Netherlands
- 2Cardiology, Boston Children Hosp, Boston, Netherlands
- 3Cardiology, Royal Brompton, London, United Kingdom
- 4Cardiology, Toronto Congenital Cardiac Cntr for Adults, Toronto, Canada
- 5Cardiology, Boston Childrens Hosp, Boston, MA
Abstract 18443: Programmatic Approach to Management of Tetralogy of Fallot (TOF) With Major Aortopulmonary Collateral Arteries (MAPCAs): A 15-Year Experience With 458 Patients
Holly Bauser-Heaton, Alejandro Borquez, Brian Han, Lynn Peng, Stanton B Perry, Ritu Asija, Claudia Algaze, Andrew Koth, Michael Ladd, Laura Downey, Andrew Shin, Lisa Wise-Faberowski, Frank L Hanley, Doff B McElhinney
Circulation. 2016;134:A18443
Abstract
Introduction: TOF with MAPCAs is a complex and heterogeneous disease with varying degrees of severity. Since 1992, our surgical team has followed a programmatic approach to reach complete repair with the incorporation of all pulmonary vascular supply with low pulmonary artery and RV pressures. We describe and analyze our 15-year surgical experience with TOF and MAPCAs, during which time 458 patients were treated.
Methods: We performed a retrospective review of all patients undergoing surgical intervention for MAPCAs at LPCH since January of 2001. The study included only patients with TOF with pulmonary atresia or stenosis. Follow-up was conducted by a combination of medical and national death record review and contact with primary referring physicians.
Results: A total of 402 patients (87.7%) achieved complete unifocalization and repair. The median RV:AO pressure early after complete repair was 0.36 (0.31-0.43). Patients were followed for a median of 1.9 years (0.2 – 7.4 years) after the first LPCH surgery, with a total of 1798 patient-years of follow-up available. At time of follow up, 88% of all patients were alive. Survival over time was better for patients whose first LPCH surgery was complete repair (HR 0.46 [95% CI 0.26-0.81], p=0.007) than those who initially underwent palliation or revision. Patients with Alagille syndrome also had a higher risk of mortality than those without chromosomal anomalies (HR 3.9 [95% CI 1.6-9.5], p=0.003). On multivariable analysis, both initial surgery type and chromosomal abnormalities were associated with worse survival: unifocalization to shunt (HR 2.5 [95% CI 1.1-5.7], p=0.023), chromosome 22q11 deletion (2.8 [1.2-6.9], p=0.022), and Alagille syndrome or other chromosomal anomaly (6.2 [2.0-19], p=0.001). Early post-repair RV:AO pressure ratio was not associated with duration of postoperative hospitalization or ICU stay, but a RV:AO pressure ratio >0.35 was associated with worse survival over time.
Discussion: Using an approach that emphasizes early complete unifocalization and repair with incorporation of all lung segments and extensive lobar and segmental surgical reconstruction, we have achieved excellent results. Patients with chromosomal anomalies and a RV:AO ratio >0.35 experience worse outcomes.
Article Information
vol. 134 no. Suppl 1 A18443
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Holly Bauser-Heaton1;
- Alejandro Borquez1;
- Brian Han1;
- Lynn Peng1;
- Stanton B Perry1;
- Ritu Asija1;
- Claudia Algaze1;
- Andrew Koth1;
- Michael Ladd1;
- Laura Downey2;
- Andrew Shin1;
- Lisa Wise-Faberowski2;
- Frank L Hanley3;
- Doff B McElhinney1
- 1Pediatric Cardiology, Stanford Univ, Palo Alto, CA
- 2Pediatric Anesthesiology, Stanford Univ, Palo Alto, CA
- 3Cardiovascular Surgery, Stanford Univ, Palo Alto, CA
Abstract 17758: Heart-Lung Transplantation Outcomes in Adult Congenital Heart Disease
Asma M Khan, Irene D Lytrivi, Hari Rajagopal, Lisa M Nicholson, Elfriede Pahl
Circulation. 2016;134:A17758
Abstract
Introduction: Heart-lung transplantation (HLT) may be indicated in adult congenital heart disease patients (ACHD) with or without Eisenmenger syndrome (ES) with end-stage heart and lung disease. Previous studies show worse survival in pediatric HLT recipients with CHD compared to those undergoing HLT for idiopathic pulmonary arterial hypertension (IPH). Outcomes and predictors of survival post HLT in ACHD patients however have not been clearly established. We aimed to determine HLT outcomes in adult CHD patients with and without ES compared to patients who underwent HLT for IPH and to identify predictors of decreased survival.
Methods: UNOS database was queried for adult HLT recipients from 1992 to 2015. Kaplan- Meier survival analysis was performed to compare post HLT survival in patients with CHD/ES, CHD without ES and IPH. Univariate and Multivariate cox regression analyses were performed to determine donor and recipient predictors of poor survival post HLT.
Results: We identified 984 patients >18 yrs who underwent HLT; CHD/ES was the diagnosis in 218 recipients, CHD with no ES in 41 and IPH in 174 recipients; 551 recipients had other diagnoses. Kaplan-Meier analysis showed no difference in post HLT survival in ACHD patients with and without ES compared to those with IPH. On multivariate analysis, only recipient female gender (adjusted HR 2.27, 95% CI 1.35-3.73), donor age (1.02; 1.01-1.03) and treated rejection episode within one year of transplant (1.53; 1.00-2.35) were found to be predictors of decreased post HLT survival.
Conclusions: We find no difference in post HLT survival in ACHD patients with or without ES compared to patients with diagnosis of IPH. ACHD population continues to expand and diversify as outcomes of palliative CHD improve and more pediatric patients survive into adulthood. However, caution must be exercised when extrapolating pediatric data to ACHD patients.
Article Information
vol. 134 no. Suppl 1 A17758
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Pediatric Cardiology, Ann & Robert H. Lurie Children’s Hosp of Chicago, Chicago, IL
- 2Pediatric Cardiology, Mount Sinai Sch of Medicine, New York, NY
- 3Sch of Public Health, Univ of Illinois at Chicago, Chicago, IL
Abstract 18188: Reversible Pulmonary Trunk Banding. XI: Myocardial Vascular Endothelial Growth Factor Expression of Young Goats Submitted to Rapid Ventricle Retraining
Renato S Assad, Eduardo A Rocha, Tiago A Meniconi, Maria Cristina D Abduch, Luiz Felipe P Moreira, Vera D Aiello, Fabio B Jatene
Circulation. 2016;134:A18188
Abstract
Introduction: Intermittent systolic overload proved to be superior to traditional PA banding, with a more efficient ventricle hypertrophy, even with less exposure to pressure overload. There is a great interest on the adaptive mechanisms of the retrained ventricle.
Hypothesis: This study sought to assess vascular endothelial growth factor (VEGF) expression in the subpulmonary ventricle (RV) retraining of young goats submitted to continuous versus intermittent systolic overload.
Methods: Twenty one21 young goats were separated into 3 groups: sham (no systolic overload), continuous (continuous systolic overload), and intermittent (four 12-hour periods of systolic overload paired with a 12-hour resting period). During a 96-hour protocol, systolic overload was adjusted to achieve a 0.7 right ventricle/aortic pressure ratio. Hemodynamic evaluations were performed before and after systolic overload every day in the postoperative period. Echocardiograms were obtained in the preoperative period and at the end of protocol. After the study period, the animals were humanely killed for morphologic and vascular endothelial growth factor (VEGF) expression assessment.
Results: Both groups had increased right ventricular and septal masses compared with the sham group (P<0002). Echocardiography revealed a major increase in RV wall thickness in the intermittent group (+129.2%) compared with the continuous group (+58.2%; p< 0.001). There was a negligible but significant increase in water content of RV (continuous: +3.5%, intermittent: +4.6%) and septal masses (both study groups: +3.5%) compared with that in the control group (p<0.002). RV VEGF expression was greater in the RV of the intermittent group (2.89% ± 0.41%) than in the continuous (1.80% ± 0.19%) and the sham (1.43% ± 0.18%) groups (p=0.005). No changes in the VEGF expression were observed in the left ventricle (p = 0.423) and septal masses (p= 0.612).
Conclusions: Intermittent systolic overload promotes a greater neoangiogenesis signaling. The association of RV hypertrophy and increased VEGF expression has important implication on the ability of the heart to adapt to pressure overload by promoting a compensatory growth of the coronary vasculature, allowing for a more efficient hypertrophy.
Article Information
vol. 134 no. Suppl 1 A18188
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Renato S Assad1;
- Eduardo A Rocha1;
- Tiago A Meniconi1;
- Maria Cristina D Abduch1;
- Luiz Felipe P Moreira1;
- Vera D Aiello2;
- Fabio B Jatene1
- 1Div of Surgical Rsch, Heart Institute (InCor) Univ of Sao Paulo Sch of Medicine, São Paulo, SP, Brazil
- 2Div of Surgical Rsch, Heart Institute (InCor) do Hosp das Clínicas da Faculdade de Medicina da Universidade de São Paulo, São Paulo, SP, Brazil
Abstract 17490: Cerebral Near Infrared Resonance Spectroscopy Insensitively Detects Critically Low Venous Oxyhemoglobin Saturation Following Stage 1 Palliation for Hypoplastic Left Heart Syndrome
Erin Rescoe, Xiaoqi Tang, John N Kheir
Circulation. 2016;134:A17490
Abstract
Background: Venous oxyhemoglobin saturation (SvO2) is considered a gold standard in assessing the adequacy of tissue oxygen delivery (DO2); SvO2 <40% often represents compromised DO2. Regional oxygenation index (rSO2) based on near infrared resonance spectroscopy (NIRS) is frequently used to identify patients at risk for compromised DO2, though its sensitivity to detect these abnormalities in the postoperative setting is uncertain.
Hypothesis: We hypothesized that rSO2 would be <40 in at least 50% of patients with SvO2<40.
Methods: SvO2 was measured by co-oximetry (Radiometer ABL 800) from blood sampled from the superior vena cava as clinically indicated in n=88 neonates following the Norwood procedure for hypoplastic left heart syndrome. Only patients in whom the tip of the internal jugular catheter was confirmed to be in the SVC were included. A rolling average of SvO2 (assuming a constant change between each measurement) was created and matched to contemporaneously measured NIRS (ForeSight, CasMed) every 5 seconds. Then, because this device is calibrated to reflect 30% arterial oxyhemoglobin saturation (SaO2) and 70% SvO2, we corrected rSO2 for SaO2 contamination as follows: corrected rSO2 = (rSO2 – SaO2*0.3)/0.7. Groups were compared to SvO2 by linear regression and Bland Altman analysis.
Results: Among 1,792 correlations, SvO2 was <40% in 22.6%. Cerebral rSO2 correlated poorly with measured SvO2 (r2 =0.29, A). The mean bias was +10.6 (B). A low rSO2 (defined as a rSO2 <40) was only 3.9% sensitive and 98.6% specific in detecting SvO2<40%. Given the low prevalence of SvO2<40, the negative predictive value of NIRS>40 was 77.8%. Correcting rSO2 for SaO2 enhanced test performance, with corrected NIRS <40 having a sensitivity for SvO2<40 of 19% and specificity of 95% (C). This decreased positive bias to +3.4 (D).
Conclusion: Cerebral rSO2 is very insensitive in detecting critically low SvO2. Cerebral rSO2 >40 should not be reassuring for adequate DO2.
Article Information
vol. 134 no. Suppl 1 A17490
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Erin Rescoe;
- Xiaoqi Tang;
- John N Kheir
- Cardiology, Boston Children’s Hosp, Boston, MA
Abstract 16954: Staged versus Complete Repair in the Symptomatic Neonate With Tetralogy of Fallot: in Search of the Optimal Strategy
Jennifer Bailey, Laura Mercer-Rosa, Christopher Mascio, Okan Elci, Elizabeth Goldmuntz
Circulation. 2016;134:A16954
Abstract
Objective: To compare perioperative and intermediate outcomes in the symptomatic neonate with tetralogy of Fallot (TOF) undergoing complete repair versus a neonatal palliative procedure followed by a complete repair.
Methods: A retrospective cohort study of symptomatic neonates with TOF who had a complete repair (Group 1, n=111) or palliation followed by complete repair (Group 2, n= 28) from 2000 to 2013 at our center. Outcomes were compared at four points: the admission for neonatal intervention (Group 1 vs 2A), the admission for complete repair (Group 1 vs 2B), the single vs combined surgical admissions to achieve a complete repair (Group 1 vs Group 2A+2B), and cumulative events 2 years post complete repair.
Results: Demographics, surgical approach and mortality were similar between Groups. At the time of the neonatal procedure, Group 1 was exposed to cardiopulmonary bypass (CPB) and deep hypothermic circulatory arrest (DHCA) more frequently than Group 2A. As compared to Group 1, Group 2 had shorter duration of intubation, ICU care, and post-procedure length of stay during the neonatal procedure and at complete repair. The combined admissions for Group 2 showed no difference in the total duration of intubation, ICU care or total length of hospital stay as compared to Group 1. Following complete repair, the number of subjects who required re-intervention and the number of re-hospitalizations per Group were similar though Group 2 had more total number of surgeries.
Conclusions: In the largest cohort of symptomatic neonates with TOF to date, both strategies seemingly ultimately offer similar cardiac outcomes. Even though it requires one additional surgical procedure, the staged approach might offer long term neurodevelopmental advantages by minimizing exposure to CPB, DHCA and perioperative complications in the neonatal period without incurring substantially longer cumulative days of ICU or hospital care.
Article Information
vol. 134 no. Suppl 1 A16954
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Pediatrics, The Children’s Hosp of Philadelphia, Philadelphia, PA
- 2Cardiothoracic Surgery, The Children’s Hosp of Philadelphia, Philadelphia, PA
- 3Biostatistics and Data Management, The Children’s Hopsital of Philadelphia, Philadelphia, PA
Abstract 17074: Melody Valve for Surgical Mitral and Tricuspid Valve Replacement in Children With Small Annuli
Breanna L Piekarski, Francesca R Pluchinotta, David Zurakowski, James M Hammel, Oliver Kretschmar, Paul J Chai, David M McMullan, Bret A Mettler, Phillip T Burch, Lale Hakami, David B Meyer, Frederic Jacques, Alessandro Frigiola, Sitaram M Emani
Circulation. 2016;134:A17074
Abstract
Introduction: Current options for atrioventricular valve replacement are limited to mechanical valves and fixed diameter bioprostheses, with no options for annuli less than 15 mm diameter. Fixed diameter valves do not allow for expansion with somatic growth, necessitating frequent reoperation for replacement. An externally stented bovine jugular vein graft (Melody valve) has been modified for implantation in children with small annuli, with the potential for expansion as the child grows.
Methods: Pediatric patients at 11 institutions in North America and Europe who underwent surgical implantation of Melody valve in the mitral or tricuspid positions were retrospectively reviewed. Primary outcome measure was early valvular function, whereas secondary outcome measures included valve durability, mortality, and successful valve expansion.
Results: Fifty patients underwent Melody valve implantation in the mitral (n=45) or tricuspid (n=5) position. Diagnosis was congenital MS (n=26), atrioventricular canal (n=18), congenital MR (n= 4), or PA/IVS (n=2). The median age and weight at time of insertion was 1 year (Range: 1 week- 13 years) and 7.1 kilograms (Range: 3.1-52.7 kg). Median size at implantation was 14 mm (Range: 10-20 mm). Echocardiogram within 30 days of insertion demonstrated mild or less regurgitation in 48/50 patients, with a median gradient of 4 mmHg (IQR: 0-5 mmHg). There were 13 deaths, 6 early (within 30 days of implantation) and 7 late (> 30 days). Among survivors, there was clinically significant worsened valvar regurgitation (moderate-severe) at follow up in 6 patients; with median follow up of 13 months (IQR: 5.6-20.4 months). Freedom from valve replacement was 91% at 12 months excluding early deaths. Nineteen patients underwent successful catheter-based valve expansion beyond one month postoperatively for increased gradients.
Conclusions: Surgically implanted Melody valves demonstrate acceptable acute valvular function when used for atrioventricular valve replacement with annular dimensions less than 15 mm. Mortality remains high in acutely ill patients despite adequate postoperative valve function. Long term freedom from replacement is acceptable, and valve expansion is successful at preventing reoperation as a child grows.
Article Information
vol. 134 no. Suppl 1 A17074
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Breanna L Piekarski1;
- Francesca R Pluchinotta2;
- David Zurakowski3;
- James M Hammel4;
- Oliver Kretschmar5;
- Paul J Chai6;
- David M McMullan7;
- Bret A Mettler8;
- Phillip T Burch9;
- Lale Hakami10;
- David B Meyer11;
- Frederic Jacques12;
- Alessandro Frigiola2;
- Sitaram M Emani1
- 1Cardiovascular Surgery, Boston Children’s Hosp, Boston, MA
- 2Pediatric Cardiology and Adult Congenital Heart Disease, IRCCS Policlinico San Donato, Milan, Italy
- 3Anesthesia and Surgery, Boston Children’s Hosp, Boston, MA
- 4Pediatric Cardiac Surgery, Univ of Nebraska Med Cntr, Omaha, NE
- 5Pediatric Cardiology, Zurich Children’s Hosp, Zurich, Switzerland
- 6Cardiothoracic Surgery, New York-Presbyterian Morgan Stanley Children’s Hosp, New York, NY
- 7Cardiac Surgery, Seattle Children’s, Seattle, WA
- 8Pediatric Cardiac Surgery, Vanderbilt Univ Med Cntr, Nashville, TN
- 9Cardiothoracic Surgery, Primary Children’s Hosp, Salt Lake City, UT
- 10Cardiac Surgery/ Pediatric Cardiac Surgery, Univ Hosp Munich, Munich, Germany
- 11Pediatric Cardiothoracic Surgery, Cohen Children’s Med Cntr of New York, Northwell Health, New Hyde Park, NY
- 12Pediatric Cardiac Surgery, Cntr hospitalier universitaire de Québec, Quebec City, Canada
Abstract 13801: Cardiopulmonary Bypass is Protective Against Shunt Thrombosis in Patients Undergoing Placement of Modified Blalock-Taussig Shunt
Jason T Patregnani, Anthony A Sochet, Darren Klugman, Yaser Diab, John Berger, Pranav Sinha
Circulation. 2016;134:A13801
Abstract
Introduction: Enhancements in surgical technique and cardiopulmonary bypass (CPB) technology have contributed to dramatically improved outcomes of staged palliation for single ventricle patients. However, in-hospital mortality after first stage palliation procedures remains high at 16%. Systemic to pulmonary artery shunt (SPS) thrombosis is a major contributor to morbidity in these patients with an incidence reported between 5 to 37%. Cardiopulmonary bypass is known to have hypocoagulable sequelae.
Hypothesis: Hypocoagulable sequelae of CPB are protective against early thrombosis of systemic to pulmonary artery shunts.
Methods: We performed a retrospective cohort study from January 2008 through December 2014 of all children undergoing single ventricle palliation with a SPS. Early shunt thrombosis was defined as clinical hypoxemia necessitating cardiac catheterization, with angiographic evidence of a thrombosis within the shunt during the same admission. Cohorts with and without early shunt thrombosis and those with and without CPB were compared using Wilcoxon sign rank sum test, Student’s t-test and Fisher’s exact test as appropriate. Unadjusted logistic regression was used to assess independent predictors for development of shunt thrombosis.
Results: Within the study period a total of 75 neonates underwent placement of SPS (with CPB n = 25, without CPB n = 50) with an operative mortality of 11%( 8/75). In this cohort, 12% (9/75) patients developed an early shunt thrombosis during the index admission. All instances of shunt thrombosis were observed in cases performed without CPB (without CPB n = 9; with CPB n =0) (p = 0.03). Unadjusted logistic regression of CPB on early shunt thrombosis yielded an odds ratio of 0.14 (95% CI: 0.01-0.93, p = 0.04).
Conclusions: Patient’s undergoing SPS placement without CPB have an increased incidence of shunt thrombosis as compared to those with CPB. Additional studies to understand the hypocoagulable sequelae of CPB are required and may help in preventing shunt thrombosis in patients undergoing SPS.
Article Information
vol. 134 no. Suppl 1 A13801
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Dept of Critical Care/Cardiology, Children’s National Med Cntr, Washingon, DC
- 2Dept of Critical Care, Johns Hopkins All Children’s Hosp, St. Petersburg, FL
Abstract 11277: Computational Fluid Dynamics Characterization of Pulsatile Flow in Patient Specific Central and Sano Shunts: Relevance to Shear-Stress Induced, Platelet-Mediated Thrombosis
Robert Ascuitto, Nancy Ross-Ascuitto, Carey Celestin, Martin Guillot
Circulation. 2016;134:A11277
Abstract
Introduction: Central shunts (aorta) and Sano shunts (right ventricle) connected to the pulmonary arteries (PAs) are vital operations for infants with complex heart defects. However, they can become thrombosed.
Hypothesis: At sites of prominent angulation, flow augments wall shear stress (WSS), a determinate of platelet-mediated thrombosis.
Methods: We employed a patient-based computational model (Fluent) of pulsatile flow (viscosity 5 cPa-s), using a finite volume method and cardiac catheterization data, and geometric simulations (Autodesk Inventor), using angiography, to study flow behavior and WSS. Two central (4.0 and 3.5 mm) and Sano (5 and 6 mm) shunts were assessed. At the inlet to the central and Sano shunts, ascending aorta (AAo, 87/40 and 93/35 mmHg) and right ventricle (RV, 99/10 and 84/10 mmHg) pressures were used, respectively. At the outlets, measured PA pressures were used.
Results: For central shunts, Fig 1, WSS reached 245 Pa and 123 Pa, peak systole. For Sano shunts, Fig 2, WSS attained 203 Pa and 133 Pa, peak systole. At sites of angulation, we identified flow vortices augmenting WSS (>100 Pa), and downstream regions of flow stagnation and recirculation, which are conducive to platelet aggregation and thrombus formation. Shunt burden, assessed by averaging WSS over the luminal surface of the shunts and the cardiac cycle, was 73.0 Pa and 67.2 Pa for central shunts, and 34.9 Pa and 19.6 Pa for Sano shunts.
Conclusions: Our results indicate central shunts present a higher risk for thrombosis than Sano shunts. Importantly, WSS induced, platelet-mediated thrombosis is insensitive to aspirin, as the process does not involve the cyclooxygenase pathway.
Article Information
vol. 134 no. Suppl 1 A11277
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Cardiology, Louisiana State Univ, New Orleans, LA
- 2Mechanical Engineering, Univ of New Orleans, New Orleans, LA
Abstract 20302: Ventricular Arterial Coupling: A Novel Echocardiographic Risk Factor for Disease Progression in Pediatric Dilated Cardiomyopathy
Christine A Capone, Josemiguel Lorenzo, Barbara Tria, Jaqueline M Lamour, Daphne T Hsu, Joseph Mahgerefteh
Circulation. 2016;134:A20302
Abstract
Introduction: A higher (VA) coupling ratio measured non-invasively has been well described in adult heart failure patients and is associated with worse heart failure prognosis and response to treatment, largely due to increases in arterial elastance. There is no data regarding the importance of VA coupling in pediatric patients with heart failure
Hypothesis: A higher VA coupling ratio will be associated with worse outcomes in pediatric patients with dilated cardiomyopathy (DCM).
Methods: Demographic, clinical and echocardiographic (echo) data (including ventricular volumes, arterial elastance and LV elastance) were obtained in children with DCM. The association of VA coupling ratio with worse outcome (mechanical circulatory support, transplant, or death) was assessed.
Results: Echos from 29 patients with DCM (23 idiopathic, 3 Duchenne, 3 other) were reviewed. Mean age at presentation was 6±7 years, mean age at echo was 10±4 years. At the time of echo, 9 patients were hospitalized for initiation of inotropic therapy, 20 were out of hospital. Outcome events occurred in 12/29 patients (41%) at a mean of 2 ±1.7 years after echo. Patients with worse outcomes had a higher NYHA class than those without (3.5 ±0.9 vs. 1.7 ±1.3, respectively p=0.001), lower LV elastance (1.03 ± 0.64 vs. 1.95 ± 0.79, respectively p= 0.002), higher arterial elastance (3.53 ±1.57 vs. 2.74 ±1.27, respectively p= 0.001), and a higher VA coupling ratio ( 4.4 ± 2.6 vs 1.9 ± 1.8, respectively p =0.001, Figure 1). Increased VA coupling was significantly associated with worse outcome (AUC =0.858, Figure 1)
Conclusion: A higher VA coupling ratio is significantly associated with worse outcome in pediatric patients with DCM. Unlike adult data, this mechanism is driven not only by an increase in arterial elastance but also a decrease in ventricular elastance. VA coupling may provide insight into the mechanisms of heart failure in pediatric DCM and identify potential targets for therapy.
Article Information
vol. 134 no. Suppl 1 A20302
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Christine A Capone;
- Josemiguel Lorenzo;
- Barbara Tria;
- Jaqueline M Lamour;
- Daphne T Hsu;
- Joseph Mahgerefteh
- Pediatric Cardiology, The Children’s Hosp at Montefiore – Albert Einstein College of Medicine, Bronx, NY
Abstract 20391: Fluid Overload in Children Hospitalized With Heart Failure: How Common and How Much?
John C Dykes, Jenna F Kruger, Beth D Kaufman, Esther Liu, Katelin M Dennis, Alaina K Kipps, Vamsi V Yarlagadda, Sharon Chen, Seth A Hollander, David N Rosenthal, Christopher S Almond
Circulation. 2016;134:A20391
Abstract
Background: Studies suggest it is uncommon for children hospitalized with acute decompensated heart failure (ADHF) to present with overt signs of fluid overload (FO). It is unclear whether children hospitalized with HF actually have fluid overload, and if so, what the magnitude of fluid overload is. We sought to determine the prevalence and magnitude of FO in children hospitalized with heart failure.
Methods: All children age <21 years hospitalized with ADHF over an 18-month period between 2014 and 2015 were identified using a hospital database. The degree of FO was estimated by calculating the difference in body weight from admission to lowest weight.
Results: Between February 2014 and October 2015, 50 children underwent 70 hospitalizations for ADHF. The median age at admission was 13 years (IQR 2, 16), median weight 33 kg (11, 68); median BMI 19 (17, 24; including 10% with BMI>30); 50% had congenital heart disease (including 30% with single ventricle disease); ventricular function was preserved in 32%, moderately depressed in 16% and severely depressed in 51%. Overall, children lost an average of 7% (S.D ±7%) body weight between admission and their lowest weight (range 0 to 34%). The average decrease in BMI was 7% [1.5 kg/m2 (S.D ±7%)] with a range of 0 to 37% (0 to 9 kg/m2). Whereas one in 10 children (N=6) satisfied BMI criteria for obesity at presentation, one-third (N=2) no longer met criteria for obesity after diuresis.
Conclusion: Although children hospitalized with HF often do not manifest signs of fluid overload, they have significant fluid overload that is consistent in magnitude with adult patients hospitalized with HF. Because BMI may fluctuate significantly, caution should be used when interpreting BMI in the context of transplant candidacy decisions.
Article Information
vol. 134 no. Suppl 1 A20391
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- John C Dykes;
- Jenna F Kruger;
- Beth D Kaufman;
- Esther Liu;
- Katelin M Dennis;
- Alaina K Kipps;
- Vamsi V Yarlagadda;
- Sharon Chen;
- Seth A Hollander;
- David N Rosenthal;
- Christopher S Almond
- Pediatric Cardiology, Lucile Packard Children’s Hosp, Palo Alto, CA
Abstract 19945: Pathways of Myocardial Remodeling and Fibrosis in Duchenne Muscular Dystrophy: Role of Matrix Metalloproteinases and Tissue Inhibitors of Metalloproteinases
Jonathan H Soslow, Kimberly Crum, W B Burnette, Yan Ru Su, Kelsey Tomasek, Bruce M Damon, Larry W Markham
Circulation. 2016;134:A19945
Abstract
Background: Cardiomyopathy is the leading cause of death in Duchenne muscular dystrophy (DMD). Biomarkers such as troponin and brain natriuretic peptide do not reliably assess disease severity. Matrix metalloproteinases (MMPs) and tissue inhibitors of metalloproteinases (TIMPs) regulate collagen turnover in the myocardial extracellular matrix (ECM) and may serve as novel cardiac biomarkers of remodeling and fibrosis or surrogate targets for drug therapy.
Hypothesis: We hypothesized that MMPs and TIMPs would be increased in DMD compared with control and would correlate with severity of DMD cardiomyopathy.
Methods: DMD subjects (n=48) were prospectively enrolled. Cardiac MRI with contrast determined chamber size, left and right ventricular ejection fraction (LVEF and RVEF), and late gadolinium enhancement (LGE) in DMD. Control samples (n=15) were collected for comparison. Serum was analyzed for MMP1, 3, 9, and 10 and TIMP 1 and 2; samples with coefficient of variation > 25% were not included in analysis. Wilcoxon Rank Sum, Kruskal-Wallis, and Spearman correlation used for statistical analysis.
Results: DMD and control subjects had similar ages (14.3 vs 13.7, p=0.98). Mean LVEF in DMD was 54% ± 10 and 30/43 (68%) had at least one segment with LGE. Mean MMP1 and MMP3 were higher in DMD than control (5800 pg/ml ± 6300 vs 2600 pg/ml ± 1900, p=0.011 and 27500 pg/ml ± 49400 vs 4700 pg/ml ± 2800, p=0.037, respectively). DMD subjects with LVEF<55% had increased MMP1 and MMP1/TIMP1 ratio compared with DMD subjects with LVEF≥55% and controls (Fig1). MMP1 and MMP1/TIMP ratio were also higher in DMD subjects with LGE compared to both DMD subjects without LGE and controls (Fig1). MMP9 correlated inversely with indexed LV mass (r=-0.37, p=0.017).
Conclusions: MMPs and TIMPs are involved in the progression of cardiac dysfunction in patients with DMD, likely through myocardial remodeling and fibrosis. MMP1 and the MMP1/TIMP1 ratio have potential as cardiac markers of DMD cardiomyopathy.
Article Information
vol. 134 no. Suppl 1 A19945
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Jonathan H Soslow1;
- Kimberly Crum1;
- W B Burnette2;
- Yan Ru Su3;
- Kelsey Tomasek3;
- Bruce M Damon4;
- Larry W Markham1
- 1Pediatrics, Div of Pediatric Cardiology, Vanderbilt Univ Med Cntr, Nashville, TN
- 2Pediatrics, Div of Pediatric Neurology, Vanderbilt Univ Med Cntr, Nashville, TN
- 3Medicine, Div of Cardiovascular Medicine, Vanderbilt Univ Med Cntr, Nashville, TN
- 4Radiology and Radiological Sciences, Biomedical Engineering, and Molecular Ph, Vanderbilt Univ Med Cntr, Nashville, TN
Abstract 19397: Changing Risk of Rejection After Pediatric Heart Transplant Over Time
David M Peng, Victoria Ding, Tigran Khalapyan, Preston D Carter, John C Dykes, David N Rosenthal, Christopher S Almond, Seth A Hollander, Manisha Desai, Doff B McElhinney
Circulation. 2016;134:A19397
Abstract
Introduction: Due to limited and conflicting data regarding the risk of late rejection in pediatric heart recipients in the contemporary era, the practice of long-term surveillance endomyocardial biopsy (EMB) remains controversial.
Hypothesis: We assessed the hypothesis that rejection risk in pediatric patients declines steadily over time after transplant.
Methods: We retrospectively reviewed all EMBs performed at a single institution from 5/1995-9/2015. We defined significant cellular rejection as ≥2R (2004 ISHLT Grade) or ≥3A (1990 ISHLT Grade). We fit a logistic regression model with robust standard errors to characterize rejection risk over six time intervals (categorized as 0-2 years in 6-month intervals, 2-5 years, and 5+ years), accounting for demographics, CHD diagnosis, and number of prior positive EMB. We additionally estimated the unadjusted association of prior biopsies and rejection risk.
Results: A total of 5131 EMB were performed on 220 patients with a median age at transplant of 10.2 (IQR 2.2, 14.6) years. Patients underwent a median of 22 EMB (IQR 13, 31). Ninety-five (43%) patients experienced at least one rejection episode post-transplant, and among these patients, the median time to first rejection was 14 (IQR 2, 28) months. Based on our model, 75% of the EMB had a probability of rejection below 0.04. Compared to the 1.5-2yr interval, rejection risk was significantly lower in both the 2-5 and 5+ year intervals (Table). Each additional prior positive biopsy was associated with a 1.6x increase in odds of rejection (CI 1.5-1.8, P<0.001).
Conclusions: In conclusion, the risk of identifying rejection in biopsies peaks within the first two years post-transplant and declines considerably thereafter. Previous episodes of rejection are associated with significantly increased risk of future rejection. These findings may help to focus the practice of long-term surveillance biopsy on those patients at greatest risk of rejection.
Article Information
vol. 134 no. Suppl 1 A19397
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- David M Peng1;
- Victoria Ding2;
- Tigran Khalapyan3;
- Preston D Carter4;
- John C Dykes1;
- David N Rosenthal1;
- Christopher S Almond1;
- Seth A Hollander1;
- Manisha Desai2;
- Doff B McElhinney1
- 1Pediatrics (Cardiology), Stanford Univ, Palo Alto, CA
- 2Medicine, Stanford Univ, Palo Alto, CA
- 3Cardiothoracic Surgery, Stanford Univ, Palo Alto, CA
- 4Clinical Informatics, Stanford Univ, Palo Alto, CA
Abstract 17056: Validation of the Adult Hypertrophic Cardiomyopathy Sudden Death Risk Calculator in a Pediatric Population
Kathryn Armstrong, Julia Jeon, Chun-Po Steve Fan, Cedric Manlhiot, Judith Wilson, Kristen George, Elizabeth Stephenson, Seema Mital
Circulation. 2016;134:A17056
Abstract
Background: Hypertrophic Cardiomyopathy (HCM) is a frequent cause of Sudden Cardiac Death (SCD) in children; however robust SCD risk predictors are lacking. Our study evaluated the adequacy of the European Society of Cardiology HCM SCD Risk calculator developed for adult HCM to predict 5-year risk of SCD in pediatric HCM.
Methods: Retrospective single centre review of children < 18 years with HCM (1978- 2015). To validate the adult calculator in our cohort, 5-year SCD risk score was calculated, and discrimination and accuracy assessments were performed. Three risk groups (low, medium, high) were constructed using the calculated risk score. Kaplan-Meier methods with log-rank tests were used to compare freedom from SCD; competing risk models were applied to analyze aborted SCD events. C-statistic was used to quantify the discriminatory ability of the risk scoring, the discrepancy between predicted and observed risk were also assessed.
Results: 291 children were eligible for inclusion. The median (IQR) age at first presentation was 6.5 (0.2 – 13.0 yrs) (64% male). Average z-scores for maximal LV wall thickness, and LA diameter, were 2.4 (± 2.6), 0.74 (± 2.04) respectively, and maximal LV outflow gradient was 22 (± 35) mmHg. 5.7% had family history of SCD, 11.7% had non-sustained ventricular tachycardia, 5.3% had unexplained syncope. 12 (4.1%) patients died of SCD, 2 (0.7%) with aborted SCD. 34 (11.7%) had ICD insertion. 144 patients with complete data were included in risk analysis. The c-statistic for discrimination analysis was 0.728 (95% CI [0.617, 0.838], p< 0.001), suggesting the adult SCD risk scoring was capable of differentiating between pediatric patients with low, medium and high SCD risk. However, on calibration analysis, the predicted risk in children was significantly lower than the observed risk at Year 5. Predicted versus observed risk was 0.25% vs 2.6% in low-medium risk group; 0.65% vs 8.7% in high risk group (p= 0.02).
Conclusion: The adult HCM SCD risk calculator can discriminate between pediatric patients with low, medium or high 5-year SCD risk; however the predicted risk underestimates the observed risk. The calibration factor in the adult calculator requires modification and/or additional discriminating factors prior to use its use in children.
Article Information
vol. 134 no. Suppl 1 A17056
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Kathryn Armstrong1;
- Julia Jeon1;
- Chun-Po Steve Fan2;
- Cedric Manlhiot2;
- Judith Wilson1;
- Kristen George1;
- Elizabeth Stephenson1;
- Seema Mital1
- 1Pediatric Cardiology, The Hosp for Sick Children, Toronto, Canada
- 2CV Data Management Cntr, The Hosp for Sick Children, Toronto, Canada
Abstract 17197: Prevalence and Severity of Malnutrition in Children With End-Stage Heart Failure Evaluated for Heart Transplantation
Katelin M Dennis, Kelsey A Christenson, Lisa M Schultz, Alaina K Kipps, Marcy Snyder, John C Dykes, Katsuhide Maeda, Beth D Kaufman, Seth A Hollander, Kristin Jensen, Shannon Feehan, David N Rosenthal, Christopher S Almond
Circulation. 2016;134:A17197
Abstract
Background: Malnutrition is an important complication of end-stage heart failure (HF) in children. The prevalence and severity of malnutrition in pediatric advanced HF patients is unknown. We sought to determine the prevalence and severity of malnutrition in children referred for heart transplant (HT) evaluation using contemporary definitions.
Methods: All children referred for HT evaluation at Stanford from April 2015 to April 2016 were identified using a hospital database. Using criteria adapted from the American Society of Parenteral and Enteral Nutrition (ASPEN) guidelines, malnutrition was defined using the lowest z score for weight-for-age (WAZ), height-for-age (HAZ), and/or BMI-for-age (BAZ) at a time when the patient was believed to be euvolemic. Malnutrition was defined as mild for zscores of -1 to -1.99, moderate for z scores of -2 to -2.99, and severe for z scores of <-3.0.
Results: Overall, 45 children met the inclusion criteria. The median age was 8 years (IQR, 1, 13); 62% had CHD of which 86% had single ventricle lesions. Overall, the median WAZ was -1.9 (-3.0, -0.4); median HAZ was -1.5 (-2.6, -0.9), and BAZ -0.9 (-1.9, 0.9). Malnutrition was classified as not present in 22%, mild in 11%, moderate in 33%, and severe in 33%. Children with single ventricle lesions were twice as likely to have severe malnutrition compared to children with cardiomyopathy (P=0.028) and was a factor commonly cited in decisions to decline transplant (53%). Moderate to severe malnutrition was associated with a trend toward higher unadjusted mortality (P=0.056) compared to less malnutrition.
Conclusions: Severe malnutrition is common among children referred for heart transplant evaluation, especially children with single ventricle heart disease, and may be associated with high mortality. Encouraging earlier referral and finding efficient ways to nutritionally rehabilitate children with end-stage heart failure are warranted.
Article Information
vol. 134 no. Suppl 1 A17197
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Katelin M Dennis;
- Kelsey A Christenson;
- Lisa M Schultz;
- Alaina K Kipps;
- Marcy Snyder;
- John C Dykes;
- Katsuhide Maeda;
- Beth D Kaufman;
- Seth A Hollander;
- Kristin Jensen;
- Shannon Feehan;
- David N Rosenthal;
- Christopher S Almond
- Pediatric Cardiology, Lucile Packard Children’s Hosp Stanford, Palo Alto, CA
Abstract 16880: Identifying Non-invasive Tools to Distinguish Acute Myocarditis From Dilated Cardiomyopathy in Children
Divya Suthar, Debra Dodd, Justin Godown
Circulation. 2016;134:A16880
Abstract
Introduction: Children with dilated cardiomyopathy (DCM) often require orthotopic heart transplantation. In contrast, children with acute myocarditis may present with similar clinical features to DCM, but many recover completely. Endomyocardial biopsy (EMB) is the gold standard for distinguishing myocarditis from DCM in children with left ventricular dysfunction; however, it is invasive and has potential risks.
Hypothesis: We hypothesize that acute myocarditis can be distinguished from DCM non-invasively using a composite of clinical and laboratory data, which could help obviate the need for EMB.
Methods: All children (<18 years) admitted to our PICU (1996 – 2015) with symptomatic left ventricular dysfunction and a definite diagnosis of DCM or myocarditis based on EMB or explant pathology were included. This is a retrospective chart review of clinical presentation, bloodwork, chest x-ray, echocardiographic, and cardiac catheterization data.
Results: We identified 46 (79%) children with DCM and 12 (21%) with acute myocarditis. Median age was 4.4 y for DCM and 1.6 y for myocarditis. Children with myocarditis were more likely to have a fever, irregular rhythm, elevated cardiac enzymes, wall motion abnormalities, and demonstrate lower left ventricular z-scores and better ventricular function compared to the DCM group (Table).
Conclusions: There are clear differences between patients with myocarditis and DCM that can be detected non-invasively, without the need for EMB. The low number of patients in our cohort precluded a robust multivariable analysis; however, our data suggests that it may be possible to develop a predictive model to differentiate myocarditis and DCM using non-invasive measures. Further prospective study is warranted.
Article Information
vol. 134 no. Suppl 1 A16880
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Divya Suthar;
- Debra Dodd;
- Justin Godown
- Pediatric Cardiology, Vanderbilt Univ Med Cntr, Nashville, TN
Abstract 15996: Pediatric Acute Myocarditis: Predicting Hemodynamic Compromise at Presentation to Healthcare
Ashley E Wolf, Ahmad S Chaouki, Bradley S Marino, Adin-Cristian Andrei, Jeffrey G Gossett
Circulation. 2016;134:A15996
Abstract
Introduction: The spectrum of pediatric myocarditis ranges from minimal symptoms with intact hemodynamics to rapid collapse and death; appropriate triage is critical. We sought to identify vital signs, symptoms, and tests at initial presentation predicting subsequent hemodynamic compromise.
Methods: Retrospective case series of pts 1d to 18 yrs old diagnosed with myocarditis at Lurie Children’s from 2007-16. Two cohorts were defined: high-acuity (HA): all pts requiring ionotropes, CPR, ECMO, VAD, transplant, or who died; low-acuity (LA): all pts without these interventions. The first recorded set of vital signs, symptoms, laboratory values, CXR, ECG, and ECHO findings were collected if obtained within 24 hours of presentation. Univariate analysis was performed and two multivariable logistic regression (LR) models were created to discriminate between cohorts, evaluated based on the area under the receiver’s operating characteristics curve (AUC) and internally cross-validated. A “non-quaternary” model included tachycardia, tachypnea, creatinine, and cardiomegaly, and a “quaternary” model, for use when ECHO is available, added presence of a pericardial effusion.
Results: Of 74 pts, 41 were LA and 33 HA. HA pts were more likely to be younger, weigh less, be female, have shortness of breath, or GI symptoms, but less likely to have chest pain. HA pts were more likely to be tachycardic, tachypneic, hypotensive, and hypoxemic and to have wheezing, gallop, hepatomegaly, and abnormal perfusion or pulses. HA pts were more likely to have abnormal hemoglobin, albumin, ALT, pH, bicarbonate, BNP, creatinine, cardiomegaly and pulmonary edema on CXR, and bundle branch block on ECG. HA pts were more likely to have pericardial effusion, mitral regurgitation, and lower ejection and shortening fractions on ECHO. Troponin level was not different between cohorts. Non-quaternary LR model showed an AUC = 0.913. Quaternary LR model had an AUC = 0.964.
Conclusions: Factors at initial presentation with myocarditis are associated with later hemodynamic compromise. Our two internally-validated models based on initial vital signs, symptoms, and laboratory data predict the need for ICU care and can be used to appropriately disposition patients who may deteriorate rapidly.
Article Information
vol. 134 no. Suppl 1 A15996
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Pediatrics, McGaw Med Cntr of Northwestern Univ, Chicago, IL
- 2Pediatric Cardiology, Lurie Children’s Hosp, Chicago, IL
- 3Biostatistics, Northwestern Univ Feinberg Sch of Medicine, Chicago, IL
- 4Cardiology, Lurie Children’s Hosp, Chicago, IL
Abstract 14853: Left Ventricular Rotational Mechanics in Children With Dilated Cardiomyopathy
Andrea Montero, Matthew J O’Connor, Natesa G Pandian, Anirban Banerjee
Circulation. 2016;134:A14853
Abstract
Introduction: Counterclockwise rotation of LV apex and clockwise rotation of its base lead to twisting of LV in systole (“wringing” pump) and untwisting in diastole. In adult dilated cardiomyopathy (DCM), abnormal rotation of apex and base in same direction leads to the LV resembling a “roller” pump rather than a wringing pump. This phenomenon is described as rigid body rotation (RBR). Studies on rotational mechanics in children with DCM are lacking.
Hypothesis: Children with DCM may exhibit decreased rotational mechanics and may display RBR.
Methods: We analyzed 2D speckle tracking images of apex and base in 14 DCM patients (age: 0.7-18 yrs). Rotational indices and torsion-radial displacement (T-D) loops were calculated (Fig. 1A).
Results: In 6 out of 14 (43%) DCM patients, LV apex showed “reversed” rotation resulting in RBR (Fig 2). Other 8 patients showed normal apical rotation, but had decreased rotational indices (Table 1). LVEF was similar in both RBR and non-RBR groups (41.4±14.3% vs 42.5±13.1%, p>0.05). Untwisting was decreased and quite delayed (Fig. 1B).
Conclusions: Children with DCM exhibit impaired rotational mechanics. Almost half lose normal twist pattern resulting in RBR. Area of T-D loop decreases significantly in DCM. Longitudinal studies are needed to determine whether RBR and abnormal T-D loops are signals of impending deterioration of LV function in children with DCM.
Article Information
vol. 134 no. Suppl 1 A14853
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Div. of Cardiology (8NW), The Children’s Hosp of Philadelphia, Philadelphia, PA
- 2Div. of Cardiology (8NW, The Children’s Hosp of Philadelphia, Philadelphia, PA
- 3Div. of Cardiology, Tufts Med Cntr, Boston, MA
Abstract 14712: The Risk of Congestive Heart Failure in Children and Young Adults With Congenital Heart Disease in Sweden
Zacharias Mandalenakis, Thomas Gilljam, Annika Rosengren, Georgios Lappas, Peter Eriksson, Maria Fedchenko, Kristofer Skoglund, Mikael Dellborg
Circulation. 2016;134:A14712
Abstract
Introduction: Patients with congenital heart disease (CHD) have an increased life expectancy during the last decades because of the improvement in pediatric care. However, increased admission to the hospitals due to congestive heart failure (CHF) in patients with CHD has been reported recently.
Hypothesis: The aim of the present study was to estimate the risk of developing CHF in children and young adults with CHD compared to matched controls.
Methods: We used data from the Swedish Patient and Cause of Death Registers to include all patients with a CHD diagnosis who were born between 1970 and 1993. Diagnoses were coded according to the International Classification of Diseases (ICD 8th, 9th, and 10theditions). Follow-up and comorbidity data were collected until 2011. Each patient with CHD was matched by age, sex, and county with 10 controls from the Total Population Register in Sweden.
Results: Among 26,906 patients (51.3 % men) with CHD and 269,053 matched controls, 675 and 449, respectively, were hospitalized with CHF; the mean follow-up was 18.5 years. The risk to develop CHF among CHD patients was 91.1 times greater (95% [CI] 53.4-155.6, p<0.001) compared to controls. CHD patients born in 1970s had a hazard ratio (HR) of 25.1 (95% [CI] 9.5-66.0, p<0.001) to develop CHF, in 1980s the HR was 102.6 (95% [CI] 47.1-223.4, p<0.001) and for those born in the beginning of 1990s was 246.7 (95% [CI] 60.0-1015.0, p<0.001).
Conclusions: The absolute risk to develop CHF in children and young adults with CHD was low; however, the relative risk was almost 90 times higher compared to matched controls. The risk increased exponentially with subsequent birth decade, probably due to the increased chances for survival. Further studies are indicated in order to determine the underlying mechanisms of CHF and in that case possible prevention or early treatment.
Article Information
vol. 134 no. Suppl 1 A14712
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Zacharias Mandalenakis;
- Thomas Gilljam;
- Annika Rosengren;
- Georgios Lappas;
- Peter Eriksson;
- Maria Fedchenko;
- Kristofer Skoglund;
- Mikael Dellborg
- Molecular and Clinical Medicine/Cardiology, Sahlgrenska Academy, Medicine, Gothenburg, Sweden
Abstract 13220: Distinct Disease Mechanisms Drive Pediatric and Adult Dilated Cardiomyopathy
Meghna D Patel, Caralin Schneider, Geetika Bajpai, Jayham Mohan, Charles Canter, Jeffrey Towbin, Kory Lavine
Circulation. 2016;134:A13220
Abstract
Background: Numerous clinical studies have suggested that adult heart failure (HF) therapies are less effective in children with dilated cardiomyopathy (DCM). The mechanistic basis for this phenomenon is poorly defined. Collectively, adult HF therapeutics target a process termed adverse remodeling, a common pathway by which the adult heart responds to injury. We hypothesized that pediatric and adult DCM comprise distinct pathological entities in that children do not undergo adverse remodeling.
Methods: LV specimens were obtained from donor pediatric and adult controls (24), pediatric DCM (31) and adult DCM patients (33). Pathological evidence of adverse remodeling including myocardial fibrosis, cardiomyocyte hypertrophy, and gene expression was examined using immunostaining, electron microscopy and RNA sequencing.
Results: Consistent with the established pathophysiology of adult HF, adults with DCM displayed marked increases in myocardial fibrosis compared to donor controls (both p<0.01)(Figure). In contrast, pediatric DCM had minimal evidence of fibrosis compared to both aged-matched controls and adults with DCM. Examination of cardiomyocyte hypertrophy and capillary density demonstrated less extensive cardiomyocyte hypertrophy and capillary rarefaction in pediatric compared to adult DCM patients. Electron microscopy revealed similar sarcomere thickness and length between control and pediatric DCM specimens. RNA sequencing demonstrated that genes associated with adverse remodeling were not up-regulated in pediatric DCM specimens.
Conclusions: These findings demonstrate that children with DCM display minimal evidence of adverse remodeling; suggesting pediatric and adult DCM may represent different pathological entities. Collectively, these data provide a mechanistic basis to understand why adult HF therapeutics may not work in children, and suggest the possibility that distinct therapies may be needed for pediatric DCM.
Article Information
vol. 134 no. Suppl 1 A13220
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Meghna D Patel1;
- Caralin Schneider2;
- Geetika Bajpai2;
- Jayham Mohan2;
- Charles Canter1;
- Jeffrey Towbin3;
- Kory Lavine2
- 1Pediatric Cardiology, Washington Univ Sch of Medicine, St. Louis, MO
- 2Cardiology, Washington Univ Sch of Medicine, St. Louis, MO
- 3Pediatric Cardiology, Univ of Tennessee Health Science Cntr, Memphis, TN
Abstract 12162: Changes in Renal Function Following Left Ventricular Assist Device Placement in Pediatric Patients: A PediMACS Analysis
Joshua M Friedland-Little, Borah J Hong, Jeffrey G Gossett, Shriprasad R Deshpande, Sabrina Law, Kathryn A Hollifield, Ryan S Cantor, Steven J Kindel, Mark W Turrentine, Ryan R Davies
Circulation. 2016;134:A12162
Abstract
Introduction: Renal dysfunction (RD) is prevalent among pediatric patients with advanced heart failure. Data are limited regarding changes in renal function following left ventricular assist device (LVAD) placement in this population.
Hypothesis: Renal function will improve following pediatric LVAD placement, but degree and durability of improvement may vary based upon patient and device characteristics.
Methods: Pediatric LVAD recipients enrolled in the Pediatric Interagency Registry for Mechanical Circulatory Support (PediMACS) between September 19, 2012 and December 31, 2015 were included. The Schwartz equation was used to calculate eGFR and longitudinal changes in renal function were analyzed for the entire cohort as well as subgroups stratified by patient and device characteristics.
Results: Data from 218 patients from 39 centers were analyzed. Mean age at implant was 9.2 years and total follow up time was 768 patient-months. There were 117 (54%) durable continuous flow LVADs, 60 (27%) durable pulsatile flow LVADs, and 41 (19%) temporary LVADs. The underlying diagnosis was cardiomyopathy in 162 (74%) patients and congenital heart disease in 47 (22%) patients. Baseline RD (eGFR < 90 mL/min/1.73 m2) was present in 140 (64%) patients. Overall, eGFR improved post-LVAD, peaking at 1 month post-implant (Figure 1). There was an inverse relationship between baseline eGFR and the degree of improvement at 1 month (mean increase in eGFR of 45 +/- 16 for patients with baseline RD vs. mean increase of 16 +/- 58 for patients with normal eGFR pre-LVAD, p=0.001). Degree of improvement in eGFR at 1 month did not appear impacted by device type, age, or diagnosis. There was a downward trend in eGFR after 1 month, although eGFR remained over baseline for patients with pre-implant RD.
Conclusions: Renal function improves post-LVAD placement in pediatric patients regardless of age, diagnosis or device type, with improvement most pronounced in patients with baseline RD.
Article Information
vol. 134 no. Suppl 1 A12162
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Joshua M Friedland-Little1;
- Borah J Hong2;
- Jeffrey G Gossett3;
- Shriprasad R Deshpande4;
- Sabrina Law5;
- Kathryn A Hollifield6;
- Ryan S Cantor7;
- Steven J Kindel8;
- Mark W Turrentine9;
- Ryan R Davies10
- 1Pediatric Cardiology, Seattle Children’s Hosp, Univ of Washington, Seattle, WA
- 2Dept of Pediatrics, Seattle Children’s Hosp, Seattle, WA
- 3Pediatric Cardiology, Ann and Robert H. Lurie Children’s Hosp of Chicago, Chicago, IL
- 4Pediatrics, Emory Univ Children’s Healthcare of Atlanta Sibley Heart Cntr, Atlanta, GA
- 5Pediatrics, Columbia Univ Med Cntr, New York, NY
- 6Cardio Thoracic Surgery, Univ of Alabama of Birmingham, Birmingham, AL
- 7Surgery, Univ of Alabama of Birmingham, Birmingham, AL
- 8Pediatric Cardiology, Children’s Hosp of Wisconsin, Milwaukee, WI
- 9Cardiothoracic Surgery, Indiana, Indianapolis, IN
- 10Nemours Cardiac Cntr, Nemours/A.I. duPont Hosp for Children, Wilmington, DE
Abstract 19400: The Impact of Surgeon Experience on Congenital Heart Surgery Outcomes
Brett R Anderson, Amelia S Wallace, Kevin D Hill, Brian C Gulack, Roland Matsouaka, Jeffrey P Jacobs, Emile A Bacha, Sherry A Glied, Marshall L Jacobs
Circulation. 2016;134:A19400
Abstract
Introduction: Surgeon experience concerns both families of children with congenital heart disease and their medical providers. Relationships between surgeon seniority and their patients’ outcomes are often assumed, yet there is little data regarding the associations between surgeon experience and outcomes for these children.
Hypothesis: Congenital heart surgeon years of experience is associated with patient outcomes.
Methods: This retrospective national study used linked data from the American Medical Association Physician Masterfile and the Society of Thoracic Surgeons-Congenital Heart Surgery Database to examine associations between surgeon years since medical school and major morbidity or mortality for children (age <18 years) undergoing cardiac surgery. Sensitivity analyses explored different transformations of surgeon experience and adjusted for patient characteristics, institutional/surgeon volumes, and various measures of experience for each institution’s surgical team.
Results: We identified 206 congenital heart surgeons at 91 centers, performing 62,851 index operations (2010-2014). Median time from medical school was 25 years (range 9-55). A major morbidity or mortality occurred in 11.5% of cases. In multivariable analyses, the odds of major morbidity or mortality were similar for young (<15 years from medical school), mid-career (15-24 years), and senior surgeons (25-35 years). The odds of major morbidity or mortality were ~25% higher for operations performed by very senior surgeons (35-55 years from school, n=9,044 cases). In extensive sensitivity analyses, this effect remained constant.
Conclusions: In this study of >200 congenital heart surgeons, surgeon years of experience was not associated with patient outcomes for junior surgeons. Very senior surgeons, however, had significantly higher risk-adjusted odds of major morbidity or mortality. Contemporary approaches to training, referral, mentoring, surgical planning, and/or other support practices might contribute to the ability of junior congenital heart surgeons to achieve outcomes comparable to their more experienced colleagues. Understanding and disseminating these practices might benefit the medical community at large.
Article Information
vol. 134 no. Suppl 1 A19400
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Brett R Anderson1;
- Amelia S Wallace2;
- Kevin D Hill3;
- Brian C Gulack4;
- Roland Matsouaka5;
- Jeffrey P Jacobs6;
- Emile A Bacha7;
- Sherry A Glied8;
- Marshall L Jacobs9
- 1Pediatrics, Columbia Univ Med Cntr, New York, NY
- 2Biostatistics, Duke Clinical Rsch Institute, Durham, NC
- 3Pediatrics, Duke Clinical Rsch Institute, Duke Univ Med Cntr, Durham, NC
- 4Surgery, Duke Univ Med Cntr, Durham, NC
- 5Biostatistics and Bioinformatics, Duke Univ Med Cntr, Durham, NC
- 6Dept of Surgery, Johns Hopkins All Children’s Heart Institute, St. Petersburg, FL
- 7Surgery, Columbia Univ Med Cntr, New York, NY
- 8Dean, Robert F. Wagner Graduate Sch of Public Service, New York Univ, New York, NY
- 9Surgery, Johns Hopkins Sch of Medicine, Baltimore, MD
Abstract 15784: Impact of SLCO1B1 Genotype on Pediatric Simvastatin Pharmacokinetics
Jonathan Wagner, Susan Abdel-Rahman, Leon van Haandel, Andrea Gaedigk, Roger Gaedigk, Geetha Raghuveer, Ralph Kauffman, J. S Leeder
Circulation. 2016;134:A15784
Abstract
Background: Simvastatin (SV) is administered as a lactone prodrug requiring hydrolysis to its active moiety, simvastatin acid (SA), to disrupt hepatic cholesterol biosynthesis. In adults, allelic variation of SLCO1B1 encoding the liver-specific organic anion transporting polypeptide (OATP1B1) drug uptake transporter reduces statin cellular uptake. As a consequence, concentrations at the site of action are lower compromising efficacy and circulating plasma concentrations are increased, placing patients at higher risk for adverse events. Expression of OATPs in mice changes during development, raising the question of whether in humans the genotype-phenotype relationship observed in adults is relevant in the developing child.
Methods: Participants (8-21 years) with at least one allelic variant of SLCO1B1 c.521 T>C (521TC; n=12, 521CC; n=2) and wild type controls (521TT; n=12) completed a single oral dose pharmacokinetics (PK) study. SV, SA, and metabolites were quantified by liquid chromatography tandem mass spectrometry. A model-independent PK approach was used to define the peak plasma concentration (Cmax) and area under the curve (AUC) over the sampling period.
Results: At equivalent doses, SA exposure was 6- and 3-fold greater in 521CC and 521TC subjects relative to 521TT (Cmax 2.14 vs. 1.09 vs. 0.39 ng/ml; p=<0.0001 and AUC 12.09 vs. 5.15 vs. 1.86 ng/ml*h; p=<0.0001; Fig. 1). SA formation was decreased and delayed among children compared to existing adult data. Of concern, although SV and metabolites were present, SA concentrations was negligible during the sampling period in 25% of c.521TT participants.
Conclusion: The impact of the SLCO1B1 c.521 gene variants on SA PK was marked in our cohort with a decrease in the rate and extent of SA formation when compared to adults. Further investigation of the ontogeny and genetic variation of SA formation is necessary to better understand the dose-exposure relationship for SA in children beyond SLCO1B1genotype.
Article Information
vol. 134 no. Suppl 1 A15784
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Jonathan Wagner1;
- Susan Abdel-Rahman2;
- Leon van Haandel2;
- Andrea Gaedigk2;
- Roger Gaedigk2;
- Geetha Raghuveer1;
- Ralph Kauffman2;
- J. S Leeder2
- 1Pediatric Cardiology, Children’s Mercy Hosp, Kansas City, MO
- 2Clinical Pharmacology, Toxicology, and Therapeutic Innovation, Children’s Mercy Hosp, Kansas City, MO
Abstract 15299: TWIK-Related Acid-Sensitive K+ Channels Affect the Development of Aortic Root Aneurysms in Mice
Rachel D Torok, Dennis M Abraham, Clarice Gareri, Lan Mao, Howard A Rockman
Circulation. 2016;134:A15299
Abstract
Introduction: Aortic aneurysms are a significant cause of morbidity and mortality, yet the genetics underlying aortic aneurysm formation remain poorly understood. TWIK-related acid-sensitive K+ (TASK) channels are present in aortic tissue and important in neurohormonal regulation, but their function in the aorta is unknown.
Hypothesis: TASK-1 and TASK-3 channels affect aortic root morphology.
Methods: To investigate the involvement of TASK channels in thoracic aortic aneurysm development, TASK-1/3 double knockout (DKO), wild type (WT), and Marfan mice underwent serial echocardiography from 8 to 36 weeks of age to assess changes in aortic root diameter. In addition, aortic root histology was assessed in each cohort to evaluate aortic root architecture. Because TASK-1/3 DKO mice are known to have hyperaldosteronism, we tested whether aldosterone blockade with spironolactone affected aortic root diameter on serial echocardiography in TASK-1/3 DKO and WT mice.
Results: TASK-1/3 DKO mice showed significant aortic root dilation over time compared to WT on serial echocardiography (P<0.001). While Marfan mice had significant aortic root dilation at 8-12 weeks, the dilation in TASK-1/3 DKO mice occurred at 16-20 weeks of age. On histological assessment, both TASK-1/3 DKO and Marfan mice had thicker aortic root walls (P<0.05) and significant elastin fragmentation (P<0.001) compared to WT. TASK-1/3 DKO mice treated with spironolactone showed significant attenuation of the aortic root dilation, and at 28 weeks of age, aortic root diameter was similar to WT controls.
Conclusion: Loss of both TASK-1 and TASK-3 channels leads to spontaneous development of aortic root aneurysms that are associated with aortic root wall thickening and elastin disruption. Over time, aortic aneurysm formation in TASK-1/3 DKO mice closely mimics aneurysm formation in Marfan mice. Aldosterone blockade in TASK-1/3 DKO mice reduces aortic aneurysm formation, indicating a potential pathogenic role for aldosterone. These findings suggest that loss of function variants of TASK channels in humans may be important for the development of thoracic aortic aneurysms and raise the possibility of aldosterone blockade as a therapeutic option.
Article Information
vol. 134 no. Suppl 1 A15299
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Pediatrics, Duke Univ Med Cntr, Durham, NC
- 2Medicine, Duke Univ Med Cntr, Durham, NC
Abstract 13424: Prospective Trial of Adenosine on Atrioventricular Nodal Conduction in the Pediatric Transplanted Heart
Jonathan N Flyer, Warren A Zuckerman, Marc E Richmond, Brett R Anderson, Tamar G Mendelsberg, Jennie M McAllister, Leonardo Liberman, Linda J Addonizio, Eric S Silver
Circulation. 2016;134:A13424
Abstract
Introduction: Supraventricular tachycardia (SVT) is common after heart transplant. Adenosine is the standard of care for SVT treatment in children and adults, but is relatively contraindicated post-transplant due to presumed risk of prolonged atrioventricular (AV) block in denervated hearts. This is the first trial of adenosine use in pediatric and young adult heart transplant patients.
Hypothesis: Adenosine use after heart transplant does not cause prolonged asystole and is effective in blocking AV nodal conduction.
Methods: This was a single center prospective clinical trial including healthy heart transplant recipients ages 6 months – 25 years presenting for routine cardiac catheterization from July 2015 to April 2016. After catheterization, a pacing catheter was placed in the right ventricle and adenosine was given according to a stepwise protocol (12.5mcg/kg, 25mcg/kg, 50mcg/kg, 100mcg/kg and 200mcg/kg, with maximum doses of 0.8mg, 1.5mg, 3mg, 6mg and 12mg for patients ≥ 60kg) until AV block was achieved. The primary outcome was clinically significant asystole ≥ 12 seconds following adenosine that required rescue ventricular pacing. The effects of patient characteristics on adenosine dose and total adenosine effect were tested.
Results: Eighty patients completed adenosine testing. No patient (0%, 95% CI 0-3%) required rescue ventricular pacing. AV block was observed in 77 patients (96%, 95% CI 89-99%) at different doses (Figure 1). The median longest AV block was 1.9 seconds (IQR 1.4-3.2) and the mean total adenosine effect was 4.3 seconds (±2.0). No patient characteristics were significant predictors of adenosine dose and total adenosine effect. Results were similar when patients were stratified by weight ≥60kg.
Conclusion: Adenosine is a safe medical therapy for the induction of AV block in pediatric and young adult heart transplant patients when using low initial doses (25mcg/kg; 1.5mg if ≥60kg) and gradually escalating therapy.
Article Information
vol. 134 no. Suppl 1 A13424
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Jonathan N Flyer;
- Warren A Zuckerman;
- Marc E Richmond;
- Brett R Anderson;
- Tamar G Mendelsberg;
- Jennie M McAllister;
- Leonardo Liberman;
- Linda J Addonizio;
- Eric S Silver
- Pediatrics, Columbia Univ, New York, NY
Abstract 20283: Two-Dimensional Echocardiography Incorrectly Identifies Tricuspid Regurgitation Jet Location Compared to Three-Dimensional Echocardiography in Pre-Operative Assessment of Tricuspid Valve Repair in Hypoplastic Left Heart Syndrome
Kandice Mah, Billie-Jean Martin, Silvia Alvarez, Nassiba Alami Laroussi, Ivan M Rebeyka, Jeffrey Smallhorn, Nee Khoo, Timothy Colen
Circulation. 2016;134:A20283
Abstract
Background: A recent study using two-dimensional echocardiogram (2DE) reported a predominance of antero-septal commissural regurgitation in patients (70%) undergoing tricuspid valve repair (TVR) in hypoplastic left heart syndrome (HLHS). Three-dimensional echocardiography (3DE) studies on assessment of TV morphology reports a high incidence of error in the identification of TV leaflets in conventional 2DE planes. This study aims to assess the pre-operative 2DE assessment of TR jet location compared to the reference standard of 3DE color datasets in HLHS.
Methods: Twenty-five HLHS patients requiring TVR for TR between 2005 and 2015 were assessed using 2DE and 3DE to assess TR grade, 3DE vena contracta (VC) area, TV annulus diameter (indexed to body surface area, iTV) and primary TR jet location. The 2DE observer was blinded to the findings on 3DE. We compared the 2DE findings with 3DE using t-test and Pearson correlation. Surgical notes were reviewed for details of procedures performed.
Results: Indexed 2DE iTV was no different to 3DE (61mm/m2 ± 4 vs. 56mm/m2 ± 4, p=0.34). 2DE qualitative TR grade correlated with 3DE VC area (r=0.69, p<0.0001). Primary jet location on 2DE identified 20 (80%) antero-septal involvement while 5 (20%) were in other regions. 3DE showed only 2 (8%) had antero-septal TR, while 13 (52%) had central TR, 7 (28%) had central TR with extension into a commissure, and 3 (12%) had mixed commissural TR. All 25 patients underwent TV repair with primary surgical procedure of 17 (65%) having posterior annuloplasty, 5 (19%) cleft closure, 2 (8%) commissuroplasty and 2 (8%) leaflet repair.
Conclusions: 2DE was accurate in the assessment of the degree of TR and TV annular size, but in most patients incorrectly identified the primary regurgitation location in the antero-septal region instead of other location. This may have implications for planning of the primary surgical procedure in HLHS TV repair based on 2DE findings.
Article Information
vol. 134 no. Suppl 1 A20283
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Kandice Mah1;
- Billie-Jean Martin2;
- Silvia Alvarez1;
- Nassiba Alami Laroussi1;
- Ivan M Rebeyka2;
- Jeffrey Smallhorn1;
- Nee Khoo1;
- Timothy Colen1
- 1Div of Pediatric Cardiology, Stollery Childrens Hosp, Edmonton, Canada
- 2Dept of Surgery, Univ of Alberta, Edmonton, Canada
Abstract 19670: Association Between Myocardial T1-Mapping and Left Ventricular Mechanics in Patients With Repaired Tetralogy of Fallot
Christopher M Haggerty, Abba Mejia-Spiegeler, Jonathan D Suever, Gregory J Wehner, Esther Kim, Brandon K Fornwalt, Mark A Fogel
Circulation. 2016;134:A19670
Abstract
Introduction: Patients with repaired tetralogy of Fallot (TOF) have progressive, adverse ventricular remodeling, leading to abnormal contractile mechanics. Defining the mechanisms underlying this dysfunction, such as diffuse fibrosis, may provide insights into poor long-term outcomes.
Hypothesis: Left ventricular (LV) diffuse fibrosis is related to impaired LV mechanics (strain/strain rate).
Methods: Forty-three patients with TOF were evaluated with cardiovascular magnetic resonance (CMR) utilizing T1-mapping with a modified Look-Locker sequence at 3 short axis levels and spiral cine Displacement Encoding (DENSE) at the same positions to assess strain & strain rate. Native and post-contrast T1, partition coefficient, and extracellular volume fraction (ECV; using a bloodpool T1-derived hematocrit) were computed for the LV. Linear correlations were computed using Spearman’s rho. Significance was p<0.05.
Results: Four patients were excluded due to image quality or movement. 39 patients (26±10 years, 56% male) were included. Compared to normal values, seven patients had elevated ECV (>0.285), while 12 had impaired circumferential strain (<14.4%); only one patient had both. Fibrosis and mechanics data are reported in the Table. Linear associations between fibrosis and mechanics included partition coefficient with apical radial strain (R = -0.45, p = 0.006) and post-contrast T1 with basal diastolic strain rate (Figure).
Conclusions: After TOF repair, diffuse fibrosis and impaired mechanics develop in the LV. The greater prevalence of impaired mechanics and weakness of their associations suggest mechanical dysfunction may be independent of diffuse fibrosis in TOF.
Article Information
vol. 134 no. Suppl 1 A19670
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Christopher M Haggerty1;
- Abba Mejia-Spiegeler1;
- Jonathan D Suever1;
- Gregory J Wehner2;
- Esther Kim3;
- Brandon K Fornwalt1;
- Mark A Fogel4
- 1Institute for Advanced Application, Geisinger Clinic, Danville, PA
- 2Dept of Biomedical Engineering, Univ of Kentucky, Lexington, KY
- 3Div of Cardiology, Children’s Hosp of Philadelphia, Philadelphia, PA
- 4Div of Cardiology, Children’s Hosp of Philadelphia, Phildelphia, PA
Abstract 19899: Cardiac MR Stress Perfusion With Regadenoson or Dobutamine in Children Single Center Experience in Repaired & Unrepaired Congenital & Acquired Heart Disease
Cory V Noel, Ramkumar Krishnamurthy, Silvana Molossi, Brady Moffett, Rajesh Krishnamurthy
Circulation. 2016;134:A19899
Abstract
Introduction: Myocardial perfusion assessment in children is a growing need given improved survival of congenital heart disease and increasing acquired coronary disease. Pharmacologic stress cardiac MRI (CMR) is routinely utilized in adults, but rarely in children. Regadenoson has a favorable side effect profile, but has not been reported in pediatrics. We aimed to observe the safety and feasibility of regadenoson and dobutamine as pharmacologic stressors (PS) for CMR in a cohort of pediatric patients with increased risk of myocardial ischemia, compared to nuclear stress perfusion (NSP) or cardiac catheterization (CC), when available.
Methods: We reviewed our experience with regadenoson and dobutamine CMR. All CMR exams due to clinical concern for ischemia. PS achieved by either 400 mcg of regadenoson prior to perfusion assessment or dobutamine escalation to 40 mcg/kg/min. Rest/stress myocardial perfusion and viability assessed. Ventricular wall motion assessed with cine SSFP imaging. CMR perfusion and viability images jointly assessed by a pediatric cardiologist and radiologist. NSP images assessed by a radiologist blinded to CMR results.
Results: Total of 73 subjects (age 15.4 +/- 4.7 yrs, range of 10-22 yrs) included with most common diagnoses being anomalous origin of coronary (27), D-transposition of the great arteries (14), Kawasaki disease (12), Ross procedure (7) and myocardial bridge (4). All exams completed without serious adverse events, 36 by regadenoson. NSP also performed in 32 and 20 had CC with angiography and/or fractional flow reserve with PS. Discrepancy of identification or reversibility of perfusion defect between CMR and NSP tests seen in 14, 10 of whom had CC following CMR. CC confirmed CMR findings in all 10 cases, 5 demonstrated reversibility on CMR and CC, while NSP demonstrated fixed defect. Three patients with normal CMR and abnormal NSP had normal CC. Two patients had reversibility by NSP, but CMR and CC revealed scar with no reversibility.
Conclusion: Regadenoson and dobutamine CMR appears to be a safe and feasible method of PS testing in the pediatric population with an increased risk of coronary ischemia and may be a more accurate measure of provocative testing than NSP.
Article Information
vol. 134 no. Suppl 1 A19899
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Cardiology, Baylor College of Medicine – Pediatrics, Houston, TX
- 2Radiology, Texas Children’s Hosp, Houston, TX
- 3Pharmacology, Texas Children’s Hosp, Houston, TX
Abstract 19070: Three-Dimensional Speckle Tracking-Derived Left Ventricular Myocardial Deformation in Children With End-Stage Renal Disease
Daisuke Kobayashi, Sanjeev Aggarwal
Circulation. 2016;134:A19070
Abstract
Introduction: Detrimental effect of chronic renal replacement therapy on cardiac function is important in the management of children with end-stage renal disease (ESRD). Three-dimensional (3D) speckle tracking echocardiography (STE) is an emerging method to assess myocardial deformation and possibly more sensitive to detect subclinical myocardial dysfunction.
Hypothesis: We hypothesized that children with ESRD have reduced left ventricular (LV) myocardial deformation, assessed by 3D STE.
Methods: LV 3D volume data were prospectively collected in children with ESRD and on chronic renal replacement therapy (before / after hemodialysis and peritoneal dialysis) and in normal controls. LV 3D volume data were analyzed off-line by the Philips QLAB 10 and the TomTec 4D LV-Function software. The 3D LV volume, ejection fraction and global longitudinal strain (GLS) were compared between the groups. The data were compared by either independent sample t-test or paired t-test.
Results: The mean age of 27 children on dialysis (hemodialysis 14 and peritoneal dialysis 13) was 13.6 ± 3.8 years compared to 11.2 ± 3.6 years in 57 normal controls (p < 0.005), whereas there was no difference in weight and height between 2 groups. Whereas the 3D LV ejection fraction was comparable between the groups, LV end-diastolic volume index (ml/m2) was higher in dialysis group (p = 0.001). GLS was reduced in dialysis group compared to normal (-18.6 ± 2.2 vs. -15.4 ± 3.2%, p = 0.001). In the subgroup analysis, GLS significantly decreased following hemodialysis session (-16.3 ± 2.7 to -12.1 ± 2.7%, p < 0.001), though 3D ejection fraction did not change. GLS in peritoneal dialysis group (-14.6 ± 3.5%) was significantly lower than pre-hemodialysis but higher than post-hemodialysis group.
Conclusions: Children with ESRD had significantly reduced 3D STE-derived LV myocardial deformation. Acute fluid status change associated with hemodialysis had a detrimental effect on myocardial mechanics.
Article Information
vol. 134 no. Suppl 1 A19070
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Daisuke Kobayashi;
- Sanjeev Aggarwal
- Div of Cardiology, Carman and Ann Adams Dept of Pediatrics, Children’s Hosp of Michigan, Wayne State Univ Sch of Medicine, Detroit, MI
Abstract 17881: Indexed Ventricular End Diastolic Volume, Ejection Fraction, and QRS Duration Can Be Predictive of Future Cardiac Events and Associated With Interventricular Dyssynchrony in the Fontan Patients With Biventricular Heart
Tatsunori Takahashi, Yumi Shiina, Kei Inai, Michinobu Nagao, Kenji Fukushima, Hiroki Mori, Gen Harada, Eriko Shimada, Seiji Asagai, Mikiko Shimizu, Tetsuko Ishii, Tokuko Shinohara, Hisashi Sugiyama, Hirofumi Tomimatsu, In-Sam Park
Circulation. 2016;134:A17881
Abstract
Introduction: The prognostic factors in patients with biventricular heart who underwent Fontan operation remain unclear.
Hypothesis: We assessed the hypothesis that ventricular dilatation, ventricular dysfunction, and prolonged QRS duration can be predictive of future cardiac events in Fontan patients with biventricular heart.
Methods: We prospectively enrolled consecutive patients with biventricular Fontan circulation from 2003 to 2016, and performed protocolized cardiac MRI. To assess the interventricular dyssynchrony, we determined the stroke volume ratio (SVR) by using the following formula: [stroke volume (SV) of two whole ventricles] / (SV of right ventricle + SV of left ventricle), by tracing cine MRI data. If interventricular dyssynchrony existed, the blood flowed and returned to each ventricle through the VSD; therefore, the SVR should be less than 1.0. Moreover, we investigated QRS duration on medical records.
Results: A total of 40 patients were enrolled. During the follow-up period (median, 49.5 months), 9 cardiovascular events occurred (5 cases of acute exacerbation of heart failure, 3 cases of supraventricular tachycardia, one case of exacerbation of protein-losing enteropathy). Univariate analysis showed four clinical predictors: SVR less than 0.95 (RR: 8.0, 95% CI: 1.1-58.2), indexed end diastolic volume (EDVi) of the whole ventricle more than 120 mL/m2 (RR: 3.8, 95% CI: 1.2-11.3), EF less than 0.45 (RR: 4.7, 95% CI: 1.1-20.0), and QRS duration more than 110 msec (RR: 2.1, 95% CI: 0.7-6.4). The clinical cut-off points were determined from the ROC curve. Combining the three former easy available clinically parameters, we categorized the patients as “low-risk group” (with no predictors, n=17), “intermediate-risk group” (with one or two predictors, n=21) and “high-risk group” (with all three predictors, n=2). The incidence rate of a cardiac event in each group was 0% (0/17), 33% (7/21), and 100% (2/2), respectively (p < 0.01). Moreover, median SVR was 0.99 [0.90-1.0], 0.92 [0.81-1.0] and 0.87 [0.86-0.89], respectively (p < 0.01).
Conclusions: The combination of EDVi, EF, and QRS duration can be predictive of the future cardiac events and is associated with interventricular dyssynchrony in Fontan patients with biventricular heart.
Article Information
vol. 134 no. Suppl 1 A17881
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Tatsunori Takahashi1;
- Yumi Shiina1;
- Kei Inai2;
- Michinobu Nagao3;
- Kenji Fukushima1;
- Hiroki Mori1;
- Gen Harada1;
- Eriko Shimada1;
- Seiji Asagai1;
- Mikiko Shimizu1;
- Tetsuko Ishii1;
- Tokuko Shinohara1;
- Hisashi Sugiyama1;
- Hirofumi Tomimatsu1;
- In-Sam Park1
- 1Pediatric Cardiology, Tokyo Women’s Med Univ, Tokyo, Japan
- 2Clinical research for ACHD, Tokyo Women’s Med Univ, Tokyo, Japan
- 3Diagnostic imaging & Nuclear Medicine, Tokyo Women’s Med Univ, Tokyo, Japan
Abstract 16691: Reduced Aortic Elasticity in Children With Connective Tissue Disorders Regardless of Aortic Dilatation
Yohei Akazawa, Noriko Motoki, Akira Hachiya, Daisuke Akagawa
Circulation. 2016;134:A16691
Abstract
Introduction: Previous studies have demonstrated that reduced aortic elasticity in connective tissue disorders (CTDs) and the aortic stiffness could be an independent predictor of the progressive aortic dilatation. However, the evidence for aortic elasticity is less clear in children with CTDs, especially those who with non-dilated aortic root (AoR). The purpose of this study is to assess the aortic elasticity in children with CTDs who have dilated and non-dilated AoR.
Methods: A total of 31 children (age: 12±7 years) with CTDs including Marfan syndrome, Loeys-Dietz syndrome and aneurysms-osteoarthritis syndrome and 15 healthy age- and sex-matched children were studied. Aortic elasticity indexes including aortic distensibility, aortic strain were derived from echocardiography at the AoR and ascending aorta (AA). CTDs children with dilated AoR (z score ≧2.5, n=17), non-dilated AoR (z score <2.5, n=14) and controls were compared.
Results: Aortic distensibility and aortic strain at the AoR were decreased in both dilated and non-dilated groups compared to controls(aortic distensibility: 0.5±0.3х10-3 vs. 1.5±0.9х10-3vs. 2.4±1.1х10-3, p<0.05, respectively. aortic strain: 2.5±1.8vs. 5.1±2.6vs. 10.4±3.8, p<0.001, respectively). Aortic strain at AA was also decreased in both CTDs groups compared to controls(6.0±4.6vs. 11.6±7.3vs. 21.5±12.4%, p<0.05, respectively). Z scores of AoR was significantly correlated with aortic distensibility(r=-0.63, p< 0.001), and aortic strain(r=-0.54, p=0.002) in CTDs group. Multivariate analysis revealed that aortic distensibility, aortic strain and the type of CTDs were independently relevant to AoR dilatation in CTDs group (p<0.05, respectively).
Conclusions: Aortic elasticity is impaired in children with CTDs. Moreover, CTDs children with non-dilated AoR showed impairment of aortic elastic properties. Measuring aortic elasticity may help to identify children with CTDs at greater risk for aortic complications.
Article Information
vol. 134 no. Suppl 1 A16691
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Yohei Akazawa;
- Noriko Motoki;
- Akira Hachiya;
- Daisuke Akagawa
- Dept of Pediatrics, Shinshu Univ, Nagano, Japan
Abstract 15798: Yield of Echocardiograms Using Appropriate Use Criteria in an Outpatient Pediatric Cardiology Clinic at an Urban Community Hospital
Ramya Deepthi Billa, Lida Zeinali, Susan Szpunar, Premchand Anne
Circulation. 2016;134:A15798
Abstract
Introduction: Appropriate Use Criteria (AUC) were published in 2014 to help clinicians determine the need for echocardiograms in an outpatient setting. One hundred thirteen indications were identified based on common clinical scenarios. A separate, independent rating panel evaluated each indication using a scoring scale of 1 to 9, thereby designating each indication as “Appropriate” (A, median score 7 to 9), “May Be Appropriate” (M, median score 4 to 6), or “Rarely Appropriate” (R, median score 1 to 3). Fifty-three indications were identified as Appropriate, 28 as May Be Appropriate, and 32 as Rarely Appropriate.
Objectives: 1. To determine the yield of echo for indications that meet three different sets of criteria, before the publication of AUC; 2. To identify the predictors and reasons of an abnormal echo among the patients falling into 3 different criteria (A, M, R).
Methods: This was a descriptive chart review of 581 patients who had their first echocardiogram for various indications during the years 2011-2014. Results were analyzed by Pearson’s chi-square test.
Results: The overall yield was 10%. Female gender (23.1%) had the higher overall yield compared to male (8.8%) (p=0.002). Yield for the A criteria was 15.4%, for M criteria was 8.5%, and for R criteria was 5.4% (p=0.001). Patients ages zero-3 months (67.6%) and 4-11 months (66.7%) had the highest yields in the A criteria group with a yield of 1.5% in the 12-18 years age group (p<0.0001). Murmur had highest yield of 47.5% in the A group. Chest pain, cyanosis and hypertension had 0% yield. In the M criteria group, 0-3 months (100%) had the highest yield among all the age groups; murmur (33.3%) had the highest yield among all the symptoms. In the R criteria group, 0-3 months age group (17.8%) and murmur (8.3%) had the highest yields.
Conclusions: Yield was higher in patients with indications meeting appropriate criteria per AUC, especially among the younger age groups. AUC use in the future, when ordering echocardiograms by pediatric cardiologists, may contribute to a higher yield in the outpatient setting.
Article Information
vol. 134 no. Suppl 1 A15798
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Ramya Deepthi Billa;
- Lida Zeinali;
- Susan Szpunar;
- Premchand Anne
- Pediatrics, St. John Hosp and Med Cntr, Grosse Pointe, MI
Abstract 15804: Utility of Multi-modal Imaging in the Diagnosis of Pulmonary Valve Endocarditis
Jennifer S Li, Kevin D Hill, Christoph P Hornik, Richard A Krasuski, Piers C Barker, Robert D Jaquiss, Michael J Campbell
Circulation. 2016;134:A15804
Abstract
Introduction: Definitive echocardiographic evidence is a major criterion for the diagnosis of infective endocarditis by modified Duke Criteria. Pulmonary valve infectious endocarditis (PVIE), however, can be challenging to identify by echo. We sought to evaluate the added utility of multimodal imaging in PVIE.
Methods: We retrospectively analyzed demographic, laboratory, imaging, clinical, and surgical data from patients diagnosed with PVIE (2008-2015). All patients had undergone TEE as well as cardiac MRI or PET/CT and had Duke major and minor criteria evaluated.
Results: A total of 17 patients were identified with definite PVIE (76 % male and ages 4-70 years). Fourteen patients had congenital heart disease with RV to PA conduits; 3 with subsequent transcatheter pulmonary valve implant. Overall, 15/17 (88%) had positive blood cultures: strep spp 6, staph spp 5, HACEK spp 3, enterococcus 1. Only 9/ 17 demonstrated TEE evidence of PVIE. In 8 cases, TEE was negative but showed new PV obstruction and evidence of PVIE was subsequently seen by PET/CT (n=5; see figure, arrow denotes area of abnormality) or cardiac MRI (n=3). Multimodal imaging was significantly better than TEE alone for detection of PVIE (17/17 versus 9/17, p=0.001). PVIE was confirmed by surgery in 14 cases.
Conclusion: The ability to detect endocardial involvement in PVIE by echocardiography is poor, but echo is helpful in identifying new obstruction. Multimodal imaging improves the ability to preoperatively identify endocardial involvement in PVIE. Consideration should be given for PVIE to revise Duke criteria to include new obstruction and endocardial involvement by multimodal imaging.
Article Information
vol. 134 no. Suppl 1 A15804
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Jennifer S Li1;
- Kevin D Hill1;
- Christoph P Hornik1;
- Richard A Krasuski2;
- Piers C Barker1;
- Robert D Jaquiss3;
- Michael J Campbell1
- 1Pediatrics, Duke Univ Med Ctr, Durham, NC
- 2Medicine, Duke Univ Med Ctr, Durham, NC
- 3Surgery, Duke Univ Med Ctr, Durham, NC
Abstract 13848: Anatomic and Hemodynamic Changes in Single Ventricle Patients 3-9 Months After Fontan to the Teenage Years: Insights From Cardiac Magnetic Resonance and Computational Fluid Dyanmics
Mark A Fogel, Esther Kim, Matthew Harris, Kevin Whitehead, Marc keller, Thomas Spray, J William Gaynor, Stephanie Fuller, Christopher Mascio, Susan Nicolson, Lisa Montenegro, Laura Diaz-Berenstein, phillip Trusty, Alan Wei, Michael Tree, Ajit Yoganathan
Circulation. 2016;134:A13848
Abstract
Introduction: Little is known of baseline cardiac magnetic resonance (CMR) data in single ventricle (SV) pts immediately after Fontan. In addition, total cavopulmonary connection (TCPC) changes from this point to the teen years may shed some light regarding how to optimize clinical outcome.
Hypothesis: Anatomic, hemodynamic and computational fluid dynamic (CFD) parameters are significantly altered as pts age.
Methods: SV pts 3-9 months after Fontan and teens were studied with CMR. Anatomy, flows and CFD modeling were performed. Significance = P<0.05.
Results: 22 were 3-9 months after Fontan (age 3±1.1 yrs, 0.6±0.3 yrs after Fontan) & 25 were teens (age 16±1.8 yrs, 14.1±2.2 yrs after Fontan). Although a higher indexed powerloss (iPL) in teens almost reached significance, Reynold’s number & particle resident time (time a red blood cell remains in the TCPC) were greater in teens than younger pts (table). Superior vena cava (SVC) pulsatility index (PI) was greater in younger pts while inferior vena cava (IVC) PI was greater in teens, owing to the primary caval return changing from SVC to IVC as pts age (table). Both cardiac index & caval return decreased in teens while hepatic flow distribution (HFD) became more evenly distributed in teens (table). The % TCPC stenosis at its narrowest point was greater in teens (42.8 %) than younger pts (20.9%), P=0.009. In teens, iPL (R=0.39) and % TCPC stenosis (R=0.62) correlated with time from Fontan (P<0.39 for both).
Conclusion: In teens, iPL correlated with time from Fontan. Significant increase in particle resident time & Reynold’s number occur as SV pts age, with increased narrowing of the TCPC while HFD became more even. SVC PI is higher in younger pts while IVC PI is higher in teens. Cardiac index & caval return both decrease as pts age. These data serve as baseline information in the immediate post-operative state and may be used to aid in designing improved Fontan reconstruction to optimize clinical outcome.
Article Information
vol. 134 no. Suppl 1 A13848
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Mark A Fogel1;
- Esther Kim1;
- Matthew Harris1;
- Kevin Whitehead1;
- Marc keller2;
- Thomas Spray3;
- J William Gaynor3;
- Stephanie Fuller3;
- Christopher Mascio3;
- Susan Nicolson1;
- Lisa Montenegro4;
- Laura Diaz-Berenstein4;
- phillip Trusty5;
- Alan Wei6;
- Michael Tree6;
- Ajit Yoganathan5
- 1PEDIATRIC CARDIOLOGY, Childrens Hosp Philadelphia, Philadelphia, PA
- 2radiology, Childrens Hosp Philadelphia, Philadelphia, PA
- 3surgery, Childrens Hosp Philadelphia, Philadelphia, PA
- 4anesthesia, Childrens Hosp Philadelphia, Philadelphia, PA
- 5Bioengineering, GA Institute of Technology, Atlanta, GA
- 6Bioengineering, GA Tech, Atlanta, GA
Abstract 11198: Heritability of Vascular Structure and Function: A Parent-child Study
Justin R Ryder, Nathan D Pankratz, Donald R Dengel, James S Pankow, David R Jacobs, Alan R Sinaiko, Vasu Gooty, Julia Steinberger
Circulation. 2016;134:A11198
Abstract
Introduction: Vascular structure and function can be measured non-invasively in both children and adults. Understanding the heritability of these measures may aid in risk stratification and atherosclerosis prevention efforts. Data on the heritable contribution from parent to offspring for vascular measures are limited.
Hypothesis: We hypothesized that measures of vascular structure and function would be modestly heritable in this large parent-child study.
Methods: High-resolution ultrasound scans of the brachial and carotid arteries were obtained in parents (n=558; mean age=39.2±2.1) and their offspring (n=369; mean age 12.4±4.6). In the brachial artery, flow-mediated dilation (FMD) and lumen diameter (bLD) were measured. In the carotid artery, intima-media thickness (cIMT), lumen diameter (cLD), incremental elastic modulus (cIEM), diameter distensibility (cDD), and cross-sectional distensibility were measured (cCSD). Carotid-radial pulse wave velocity (PWV) was also obtained. Heritability analysis (h2, expressed as %) was performed using SOLAR on the entire cohort and adjusted for age, gender, race, body-mass index, smoking, and systolic blood pressure. Data are presented as mean (SE).
Results: Measures of bLD (h2= 25.2(8.6), p<0.001), cLD (h2= 55.4(8.8), p<0.001), cIMT (h2= 28.1(12.6), p=0.014), cDD (h2= 28.2(7.1), p<0.001), cCSD (h2= 27.1(6.9), p<0.001), and PWV (h2= 26.3(8.9), p<0.001) were significantly heritable. Only FMD (h2= 1.6(8.4), p=0.44), and cIEM (h2= 12.7(9.3), p=0.081) were not significantly heritable.
Conclusions: These data suggest that the majority of non-invasive measures of vascular structure and function are modestly heritable from parent to child. Early interventions targeted at youth with elevated vascular risk and/or a high familial cardiovascular risk profile may be able to modify vascular structure and function to prevent further dysfunction as these children transition into adulthood.
Article Information
vol. 134 no. Suppl 1 A11198
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Justin R Ryder1;
- Nathan D Pankratz2;
- Donald R Dengel3;
- James S Pankow4;
- David R Jacobs4;
- Alan R Sinaiko1;
- Vasu Gooty1;
- Julia Steinberger1
- 1Pediatrics, Univ of Minnesota, Minneapolis, MN
- 2Laboratory Medicine, Univ of Minnesota, Minneapolis, MN
- 3Kinesiology, Univ of Minnesota, Minneapolis, MN
- 4Public Health, Univ of Minnesota, Minneapolis, MN
Abstract 20794: Prenatal Predictors of Urgent Postnatal Balloon Atrial Septostomy in Transposition of Great Arteries
Nita Ray Chaudhuri, Prasad Ravi, Lisa K Hornberger, Shanthi Sivanandam
Circulation. 2016;134:A20794
Abstract
Nita Ray Chaudhuri, MD1, Prasad Ravi, MD2, Lisa K Hornberger, MD3, Shanthi Sivanandam, MD4
Background: Prenatal risk factors for poor outcomes in neonates with transposition of the great arteries are restrictive fossa ovalis (FO) and thickened atrial septum. There is limited data to assess size of fossa ovalis which makes it restrictive prenatally.
Aim: To determine urgent postnatal balloon atrial septostomy (BAS) based on effective orifice of fossa ovalis prenatally.
Materials and Methods: Prenatal echocardiograms of 50 fetuses with transposition of great arteries were reviewed retrospectively from University of Alberta (n=39) and University of Minnesota (n=11) from 2003 to 2016.
Results: Mean GA at diagnosis 33 weeks. 13 of 50 (26%) required urgent BAS within 2 hours after birth, in addition 18 of 50 (36%) required BAS > 2 hours after birth. In total, 31 (62%) required BAS within first day of life. 19 of 50 (38%) did not require BAS. 13 that required urgent BAS had restrictive fossa ovalis measuring <= 6mm. 18 that required BAS > 2 hours after birth and had fossa ovalis measuring 6-7 mm. 19 that did not require BAS had nonrestrictive fossa ovalis measuring >7 mm. A restrictive fossa ovalis of <=6 mm predicted urgent need for BAS within 2 hours after birth (sensitivity 0.60, specificity 0.84, positive predictive value 0.86). Ratio of fossa ovalis size to interatrial septum of <=0.3 predicted urgent need for BAS within 2 hours after birth (sensitivity 0.47, specificity 0.95, positive predictive value 0.93). 22 of 31 (71%) that required BAS had thick atrial septum. 19 (100%) that did not require BAS had thin atrial septum.
Conclusion: Effective orifice of fossa ovalis and ratio of fossa ovalis to interatrial septum are predictors for the need for urgent BAS postnatally. Increased thickness of atrial septum causes restriction of effective orifice of the fossa ovalis necessitating urgent BAS postnatally. Diagram: Fossa Ovalis (FO) Sagittal view. LA; left atrium, RA; right atrium
Article Information
vol. 134 no. Suppl 1 A20794
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Div of Pediatric Cardiology, Univ of Minnesota Masonic Children’s Hosp, Minneapolis, MN
- 2Div of Pediatric Cardiology, Stollery Children’s Hosp, Edmonton, Canada
Abstract 18926: Late Gestation Predictors of Biventricular Outcome After Fetal Aortic Valvuloplasty
Kevin G Friedman, Monika Drogosz, Louise Wilkins-Haug, Carol Benson, Wayne Tworetzky, Audrey C Marshall
Circulation. 2016;134:A18926
Abstract
Background: Fetal aortic valvuloplasty (FAV) has shown promise in averting progression of mid-gestation aortic stenosis to hypoplastic left heart syndrome at birth. Late gestation predictors of biventricular circulation (BiV) after FAV are not known.
Methods: Between 2000 and August 2015, 122 fetuses underwent FAV. We evaluate late gestation fetal factors associated with BiV circulation in cases who returned for 3rd trimester imaging (n=81).
Results: Of the 81 patients included, 70 (86%) had a technical successful FAV at median gestational age of 23.7 weeks (range 20.2-31.0). Median age at late gestation echo was 35.4 weeks (29.7 -38.7) and duration between FAV and last echo was 2.3 months (1.0 to 3.9). BiV outcome occurred in 34 (42%) patients. Prior to FAV, all fetuses had retrograde flow in the transverse aortic arch and the majority (75%) had exclusively right to left PFO flow with the remainder having bidirectional flow (16%) or intact atrial septum (9%). At late gestation imaging, 49 % had anterograde aortic arch flow (p<0.001 compared to pre-FAV) and PFO flow direction was bidirectional in 30 % and entirely right to left in 64% (p=NS compared to pre-FAV).
Late gestation physiological factors associated with BiV outcome after FAV were higher LV pressure (median of 72 mm Hg in BiV vs. 37 mm Hg in single ventricle, p=0.002), anterograde flow through the aortic arch (90% of BiV vs. 30% of univentricular had anterograde flow, p< 0.001), bidirectional PFO flow (44% vs. 20%, p=0.04), and higher LV ejection fraction (43% vs. 26%, p=0.008). Anatomic factors associated with BiV outcome were higher z-scores for aortic valve (-2.8 vs. -3.9, p<0.001), ascending aorta (0.6 vs. -1.2, p<0.001), mitral valve (-2.3 vs -3.4, p<0.001), LV end-diastolic volume (-0.6 vs. -3.0, p=0.004) and LV long axis dimension (-0.9 vs. -2.6, p<0.001).
In multivariate analysis, anterograde flow in transverse aortic arch (HR = 60.7 [6.9-99.9] p=0.007), higher LV pressure (HR =1.48 [1.0-2.2], p=0.05), and higher LV long axis z-score (HR =3.1 [1.4-7.1], p=0.006) were independently associated with BiV outcome.
Conclusion: BiV outcome after FAV is associated with better LV performance in late gestation evidenced by higher LV pressure and anterograde through aortic arch as well as a longer LV.
Article Information
vol. 134 no. Suppl 1 A18926
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Kevin G Friedman1;
- Monika Drogosz1;
- Louise Wilkins-Haug2;
- Carol Benson3;
- Wayne Tworetzky1;
- Audrey C Marshall1
- 1Pediatric Cardiology, Children’s Hosp Boston, Boston, MA
- 2Maternal Fetal Medicine, Brigham and Women’s Hosp, Boston, MA
- 3Radiology, Brigham and Women’s Hosp, Boston, MA
Abstract 18382: Left Ventricular Septal Mechanics in Fetal Ebstein’s Anomaly
Luke G Eckersley, Lisa Howley, Timothy Colen, Paul Brooks, Nee Khoo, Lisa K Hornberger
Circulation. 2016;134:A18382
Abstract
Introduction: Fetal Ebstein’s anomaly and tricuspid valve dysplasia (EA/TVD) are associated with high perinatal mortality. Qualitative left ventricular (LV) dysfunction and abnormal ventriculo-ventricular interactions have been implicated in poor EA/TVD outcomes. We sought to examine global and segmental LV function in fetal EA/TVD. We hypothesize dyssynchrony importantly contributes to LV dysfunction in affected fetuses.
Methods: This was a retrospective case-control study of EA/TVD diagnosed in two fetal cardiology programs. LV six segment function was analysed from a four chamber view using Vector Velocity Imaging in EA/TVD and compared to findings in healthy fetuses. Global (GLS) and segmental longitudinal strain, strain rate and inward and outward radial displacement were measured. We compared standard deviation of time to peak (T2PSD) to a novel index of global dyssynchrony (DI) (Figure 1).
Results: We analysed 32 EA/TVD and 10 similar gestation control fetuses. GLS was reduced in EA/TVD compared with control (EA/TVD -11.4+/-5.1, Ctrl -13.7+/-1.6, p=0.039). Segmental strain, GLS T2PSD and global and segmental strain rate were similar in EA/TVD and controls. The GLS DI was increased in EA/TVD (EA/TVD 18±22, Ctrl 6±7, p=0.033). Increased basal septal radial outwards displacement and inward radial displacement T2PSD were associated with increased radial DI (Table 1).
Conclusion: Fetal EA/TVD have normal LV segmental strain but reduced GLS secondary to significant mechanical dyssynchrony. Correlation of the DI with outcome in a larger cohort may lead to better prediction of intrauterine and neonatal risk in order to guide management strategies.
Article Information
vol. 134 no. Suppl 1 A18382
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Div of Pediatric Cardiology, Univ of Alberta, Edmonton, Canada
- 2Div of Pediatric Cardiology, Denver Children’s Hosp, Denver, CO
Abstract 18401: Echocardiographic Prediction of Outcomes in Fetal Pulmonary Atresia With Intact Ventricular Septum
Claudia Renaud, Bridget Zoeller, Stephanie Levasseur, Tiscar Cavalle, Marie-Josée Raboisson, Lisa Hornberger, Edgar Jaeggi
Circulation. 2016;134:A18401
Abstract
Background: Critical pulmonary stenosis (CPS) and pulmonary atresia with an intact ventricular septum (PA-IVS) represent a spectrum of pathology that ranges from good-sized to severely hypoplastic and dysplastic right ventricle (RV), pulmonary valve and tricuspid valve. These conditions are rarely associated with chromosomal or extracardiac anomalies, so parental decision regarding continuation of the pregnancy is strongly influenced by the cardiologist’s prediction of a univentricular or biventricular circulation in midgestation. Currently the prediction of outcome is mainly based on the results of five studies, each proposing a different predictive score based on small patient populations.
Hypothesis: We hypothesized that the previously published echocardiographic scores have limited capacities at predicting the outcome in patient with CPS or PA-IVS when using a larger patient population. Therefore, we aimed to create an improved predictive scoring system based on the published measurements.
Method: We conducted a multicentre retrospective study of all cases of PA-IVS or CPS diagnosed prior to 32 weeks of gestation using a single blinded observer.
Results: A total of 99 pregnancies were included. The termination rate was 36 %. Of 59 live-born patients with intention to treat, 25 had non-biventricular outcome and 32 had biventricular circulation. The survival at 1 year was 100% for biventricular repair, compared with 85% for non-biventricular outcome. The presence of sinusoids was a significant risk factor for mortality but screening was not performed systematically. All scoring systems had significantly lower sensitivities and specifities than previously reported. A small tricuspid valve annulus, a low right ventricle-to-left ventricle lenght ratio and low tricuspid-to-mitral valve ratio, as well as the presence of sinusoids are the most reliable predictors of a non-biventricular outcome.
Conclusions: The outcome of PA-IVS remains difficult to predict. A new scoring system combining the best predicting measurements of each scores is underway. Coronary sinusoids, when present, are associated with a single ventricle outcome with high mortality and should be screened systematically using optimal echocardiographic settings.
Article Information
vol. 134 no. Suppl 1 A18401
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Claudia Renaud1;
- Bridget Zoeller2;
- Stephanie Levasseur3;
- Tiscar Cavalle4;
- Marie-Josée Raboisson5;
- Lisa Hornberger6;
- Edgar Jaeggi2
- 1Fetal Cardiology, Montreal Children’s Hosp, McGill Univ, Montreal, Canada
- 2Fetal Cardiology, SickKids Hosp, Toronto, Toronto, Canada
- 3Fetal Cardiology, NewYork-Presbyterian Morgan Stanley Children’s Hosp, New York, NY
- 4Fetal Cardiology, Montreal Children’s Hosp, Montreal, Canada
- 5Fetal Cardiology, Ste-Justine Hosp, Montreal, Canada
- 6Fetal Cardiology, Stollery Children’s Hosp, Edmonton, Canada
Abstract 18081: Impaired Cerebral Autoregulation is Associated With Brain Abnormalities in Neonatal Congenital Heart Disease: Initial Experience
Jodie K Votava-Smith, Nhu Tran, Justin Abbott, Sadaf Soleymani, Hollie A Lai, Sylvia Del Castillo, Vincent Lee, Cecilia W Lo, Stefan Bluml, Lisa B Paquette, Ashok Panigrahy
Circulation. 2016;134:A18081
Abstract
Introduction: Congenital heart disease (CHD) is associated with abnormalities of brain maturation as well as brain injury, which may be related to impaired cerebral autoregulation (CA). Using serial magnetic resonance imaging (MRI), we sought to test the hypothesis that pre-operative (op) hemodynamics including impaired CA may drive: (1) brain dysmaturation and (2) post-op brain injury.
Methods: Full-term neonates with complex CHD prospectively underwent pre and post-op brain 3T MRI to assess cortical/subcortical abnormalities & injury, and short echo single voxel spectroscopy of parietal white matter (WM) to assess metabolic brain maturation. Pre-op hemodynamic monitoring included continuous mean arterial pressure (MAP), oxygen saturation (SaO2), and INVOS cerebral near infrared spectroscopy (CrSO2). Data were divided into 20 minute epochs for analysis, with significant low frequency coherence between MAP and CrSO2 waveforms defining impaired CA. Pressure passivity index (PPI) was calculated as percentage of epochs with abnormal CA per subject. Cerebral fractional tissue oxygen extraction FTOE = (SaO2 – CrSO2)/ SaO2, was calculated, as was time with significant low frequency coherence between MAP and FTOE (FTOE-PPI). Multivariate mixed-effect modeling was used with corrections for age, pre/post-op status, and number of epochs.
Results: We evaluated 22 neonates with both brain MRI (32 scans) and hemodynamics (62 ± 34 epochs per subject). Mean PPI = 14 ± 13%, range 0-52%; mean FTOE-PPI =13 ± 8%, range 0-29%. PPI correlated with concurrent brain dysmaturation including structural abnormalities of the hippocampus (p=0.02) and lower glutamate/glutamine (p=0.02), but not cortical maturation. FTOE-PPI correlated with lower concurrent glutamate/glutamine (p=0.02) and post-op WM injury (p=0.003). Higher pre-op MAP predicted post-op brain hemorrhage (p=0.016). Pre-op SaO2, CrSO2, and FTOE showed no association with MRI findings.
Conclusions: Impaired pre-op CA in CHD neonates is associated with concurrent brain dysmaturation, including hippocampal abnormalities and alterations in glutaminergic WM cellular substrate. In addition, our data suggest that susceptibility to post-op brain injury may be related to pre-op hemodynamics.
Article Information
vol. 134 no. Suppl 1 A18081
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Jodie K Votava-Smith1;
- Nhu Tran2;
- Justin Abbott3;
- Sadaf Soleymani4;
- Hollie A Lai5;
- Sylvia Del Castillo6;
- Vincent Lee7;
- Cecilia W Lo8;
- Stefan Bluml5;
- Lisa B Paquette9;
- Ashok Panigrahy10
- 1Div of Cardiology, Children’s Hosp Los Angeles, Los Angeles, CA
- 2Cardiothoracic Surgery, Children’s Hosp Los Angeles and UCLA Sch of Nursing, Los Angeles, CA
- 3Viterbi Sch of Engineering, Univ of Southern California, Los Angeles, CA
- 4Div of Neonatology, Children’s Hosp Los Angeles, Los Angeles, CA
- 5Radiology, Children’s Hosp Los Angeles, Los Angeles, CA
- 6Div of Critical Care Medicine, Children’s Hosp Los Angeles, Los Angeles, CA
- 7Dept of Radiology, Children’s Hosp of Pittsburgh of UPMC, Pittsburgh, PA
- 8Deveopmental Biology, Univ of Pittsburgh Sch of Medicine, Pittsburgh, PA
- 9Pediatrics, Div of Neonatology, Children’s Hosp Los Angeles, Los Angeles, CA
- 10Radiology, Children’s Hosp of Pittsburgh of UPMC, Pittsburgh, PA
Abstract 17713: Fetal Brain Volume as a Predictor of Postnatal Brain Injury in Neonates With Critical Congenital Heart Disease
Shabnam Peyvandi, Joanne Lau, Theodore Kingdom, Duan Xu, Anita Moon-Grady, Mike Seed, Steven Miller, Hosung Kim, Patrick McQuillen
Circulation. 2016;134:A17713
Abstract
Objective: Pre-operative brain injury is reported in 30% of neonates with critical congenital heart disease (CHD), appearing in the form of white matter injury (WMI) or stroke. Compared to controls, fetuses with CHD have a smaller total brain volume (TBV) measurable in the third trimester. The relationship between fetal onset of delayed brain development and the risk of pre-operative brain injury is unknown. We hypothesize that a lower fetal TBV predicts the presence and severity of pre-operative brain injury.
Methods: Longitudinal fetal and pre-operative neonatal brain magnetic resonance imaging (MRI) studies were evaluated in term newborns with CHD. Fetal MRI was performed in the third trimester and TBV was calculated by manual segmentation and excluded extra-axial and ventricular volumes. Neonatal MRI was assessed for the presence and severity of pre-operative brain injury (WMI and stroke). TBV was compared between those with (n= 5) and without brain injury (n= 7) and stratified based on brain injury severity (BIS) score. Analysis included descriptive statistics, Student t test and non-parametric test for trends.
Results: 25 subjects had both fetal and neonatal imaging performed, of which 12 were processed and analyzed. Fetal imaging was performed at a median gestational age of 32.3 weeks (IQR 31.3-33.4) with no difference between those with neonatal pre-operative brain injury (32 wks, IQR 32-33) and those without (32.7 wks, IQR 31.7-34). Subjects with brain injury had a lower mean fetal TBV (187.8 cm3, 95%CI: 156.9-218.7) compared to those without injury (225.2 cm3, 95%CI: 189.8-260.6, p= 0.08), Figure 1. Patients with the most severe brain injury (BIS 3) had the lowest mean TBV (176.4 cm3, SD 26.6) with a trend towards lower TBV with increasing severity of brain injury (p= 0.06).
Conclusions: Fetal TBV in the third trimester may be a predictor of risk for postnatal pre-operative brain injury in those with CHD. Further analysis with a larger sample size will be performed.
Article Information
vol. 134 no. Suppl 1 A17713
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Shabnam Peyvandi1;
- Joanne Lau2;
- Theodore Kingdom3;
- Duan Xu2;
- Anita Moon-Grady1;
- Mike Seed4;
- Steven Miller5;
- Hosung Kim2;
- Patrick McQuillen6
- 1Pediatric Cardiology, Univ of California San Francisco, San Francisco, CA
- 2Biomedical Imaging, Univ of California San Francisco, San Francisco, CA
- 3Pediatric Cardiology and Radiology, Univ of Toronto, Toronto, Canada
- 4Pediatric Cardiology and Radiology, Univ of Toronto, Hosp for Sick Children, Toronto, Canada
- 5Neurology, Univ of Toronto, Hosp for Sick Children, Toronto, Canada
- 6Pediatric Critical Care, Univ of California San Francisco, San Francisco, CA
Abstract 17097: A Novel Brain Injury Biomarker Correlates With Cyanosis in Infants With Congenital Heart Disease
Lindsey McPhillips, Kaie Ojamaa, Cristina Sison, Dorota Gruber, Dipak Kholwadwala
Circulation. 2016;134:A17097
Abstract
Introduction: Cyanotic heart lesions are a complex subset of congenital heart disease (CHD) in which patients are persistently desaturated until surgical repair/palliation.
Hypothesis: We hypothesized there will be a direct relationship between degree of preoperative desaturation and presence of systemic inflammation, as well as evidence of brain injury in children less than one year of age. We further hypothesized that preoperative desaturation with augmented systemic inflammation will predict a more complex postoperative course.
Methods: Fifty patients with CHD were enrolled in this study and classified as cyanotic (O2≤90%) or acyanotic (O2>90%) based on SpO2. Serum was obtained within 2 weeks of the cardiac surgery and the following inflammatory mediators were analyzed using commercially available ELISA kits: macrophage migration inhibitory factor, IL-6, IL-8, TNF-α, IL-12p70, IL-10, IL-1β, and INF-γ; and a novel biomarker of axonal injury, phosphorylated high-molecular weight neurofilament (pNF-H). Postoperative variables included inotrope score, duration of mechanical ventilation and length of stay.
Results: A total of 22 cyanotic and 28 acyanotic patients were enrolled with a median age of 9.5 days (range 2-303 days) and 99.5 days (range 1-274 days), respectively; and a mean ± SD SpO2 of 78 ± 18% and 97 ± 3% (p<0.001), respectively. Compared to acyanotic patients, cyanotic patients had significantly elevated IL-6 (6.6 ± 7.6 vs 2.9 ± 2.9 pg/ml, p=0.019) and pNF-H (222 ± 637 vs 57 ± 121 pg/ml, p=0.046) preoperatively, and both biomarkers were associated with the degree of desaturation (Spearman correlation ρ=-0.30, p=0.037 and ρ=-0.29, p=0.049, respectively). Cyanotic patients had higher inotrope scores at 24 and 48 hours (p=0.022 and p=0.047, respectively) and the preoperative oxygen saturation was inversely related to duration of mechanical ventilation postoperatively (ρ=-0.4, p=0.02).
Conclusions: Cyanotic patients with CHD were exposed to higher serum concentrations of inflammatory mediators in the preoperative period compared to acyanotic patients, and showed evidence of brain injury. The severity of preoperative desaturation was a significant predictor of greater postoperative medical intervention.
Article Information
vol. 134 no. Suppl 1 A17097
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Pediatric Cardiology, Cohen Children’s Med Cntr, Northwell Health, New Hyde Park, NY
- 2Molecular CardioVascular Rsch, The Feinstein Institute for Med Rsch, Manhasset, NY
- 3Biostatistics Unit, Feinstein Institute for Med Rsch, Manhasset, NY
Abstract 16238: Inter-Tester Reproducibility of Fetal Doppler Indices of Cardiac Function
Catherine C Allen, Regina Keller, Krystle C Barnard, Zhiqian Gao, Eileen C King, Erik C Michelfelder
Circulation. 2016;134:A16238
Abstract
Introduction: Doppler echocardiography is emerging as a method to identify cardiovascular dysfunction in fetuses with suspected cardiac abnormalities and inform decisions for fetal or perinatal interventions. It is clinically important to understand the reproducibility of these measures, particularly between testers. While studies have reported intra- and inter-observer variability, little is known about inter-tester variability for these measures.
Hypothesis: We hypothesized that despite being a high volume fetal echocardiography laboratory, fetal Doppler measurements will demonstrate higher inter-tester variability compared with inter- and intra-observer variability of the same measurements.
Methods: Prospective study of uncomplicated, singleton pregnancies to evaluate various fetal Doppler measures of cardiovascular function. One sonographer obtained pre-defined Doppler variables and then a second sonographer obtained the same pre-defined variables 15 minutes after the first sonographer. Separate measurements were obtained by the two sonographers to evaluate intra- and inter-observer variability (on first acquisition) as well as inter-test variability (between both acquisitions).
Results: Twenty-nine fetuses between 17-36 weeks gestation were enrolled. A significant number of variables had excellent or good inter-tester intraclass correlation coefficient (ICC), comparable to the intra- and inter-observer ICC. However, a similar percent of variables had fair or poor inter-tester ICC which contrasted with excellent or good intra- and inter-observer ICC (Table 1).
Conclusions: In conclusion, within a laboratory highly experienced in Doppler fetal echocardiography, intra- and inter-observer reproducibility is good for most fetal Doppler parameters. However, inter-tester reproducibility is fair or poor for several Doppler variables, notably time-based variables (e.g. Tei index) and venous Doppler flow indices.
Article Information
vol. 134 no. Suppl 1 A16238
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Catherine C Allen1;
- Regina Keller1;
- Krystle C Barnard1;
- Zhiqian Gao2;
- Eileen C King3;
- Erik C Michelfelder4
- 1The Heart Institute, Cincinnati Children’s Hosp Med Cntr, Cincinnati, OH
- 2Heart Institute Rsch Core, Cincinnati Children’s Hosp Med Cntr, Cincinnati, OH
- 3Biostatistics and Epidemiology, Cincinnati Children’s Hosp Med Cntr, Cincinnati, OH
- 4Sibley Heart Cntr Cardiology, Children’s Healthcare of Atlanta, Emory Univ Sch of Medicine, Atlanta, GA
Abstract 13097: Flow and Cardiac Output Redistribution in the Fetus With {S,D,D} Transposition of the Great Arteries and Intact Ventricular Septum: Insights Into the Pathophysiology
Max E Godfrey, Kevin G Friedman, Monika Drogosz, Abraham M Rudolph, Wayne Tworetzky
Circulation. 2016;134:A13097
Abstract
Introduction: Although the postnatal physiology of {S,D,D} transposition of the great arteries with intact ventricular septum (TGA) is well established, little is known about fetal TGA. In the normal fetus, the pulmonary valve (PV) is larger than the aortic valve (AoV), there is exclusive right to left flow at the foramen ovale (FO) and ductus arteriosus (DA), and the left ventricle (LV) ejects 40% of combined cardiac output (CCO) through the aorta, primarily to the brain. In TGA, the LV ejects O2-rich blood to the pulmonary artery, theoretically leading to pulmonary vasodilation, increased branch pulmonary arterial flow and resultant reduced DA flow. We tested the hypothesis that TGA anatomy results in altered distribution of CCO, FO and DA flow, and valve size.
Methods: We analyzed valve size, color flow and pulse Doppler on echocardiograms of 74 fetuses with TGA (2003-2015). Findings were compared with our institutional normal fetal data, n=222.
Results: The LV component of CCO was higher in TGA than in controls (50.7% vs 40.2%, p<0.001) with no difference in total CCO. Flow was bidirectional at the FO in 56 (75.7%) fetuses and at the DA in 24 (32.4%). Only 21.6% had normal exclusive right to left flow at both shunts. Bidirectional shunting was more common in the 3rd trimester than the 2nd(p<0.03). In contrast to normal, TGA AoV and PV sizes were nearly identical, hence the AoV z-score was higher than the PV z-score (1.13 vs -0.65, p<0.001).
Conclusion: In TGA there is loss of normal right sided dominance, as each ventricle provides half of the CCO. The AoV is relatively large as it carries 50% of CCO rather than the normal 40%. The PV is relatively small as it carries 50% rather than the normal 60% of CCO. There is increased LV component of CCO (to the pulmonary arteries) and frequently bidirectional FO and DA flow. This may support the theory that high pulmonary arterial O2content lowers pulmonary vascular resistance, thereby increasing branch pulmonary arterial flow and venous return, increasing LV preload and output. Pulmonary sensitivity to O2 is thought to increase later in gestation, which may explain the increased bidirectional shunting. Consequences of these flow alterations include increased aortic and likely brain flow, perhaps compensating for substrate deficiency in TGA.
Article Information
vol. 134 no. Suppl 1 A13097
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Cardiology, Boston Children’s Hosp, Boston, MA
- 2Cardiovascular Rsch Institute, Univ of California – San Francisco, San Francisco, CA
Abstract 12569: Relationship Between Neurodevelopmental Outcomes at 2 Years and 4 Years in Children With Congenital Heart Disease After Surgical Palliation
Cheryl L Brosig, Laurel Bear, Sydney Allen, Raymond G Hoffmann, Amy Pan, Michele Frommelt, Kathleen A Mussatto
Circulation. 2016;134:A12569
Abstract
Introduction: Children with congenital heart disease (CHD) are at risk for neurodevelopmental (ND) delays. The American Heart Association (AHA) recommends serial ND evaluation for children with CHD. This study compares the ND testing results of children with CHD at 2 and 4 years of age.
Methods: Children with CHD meeting the AHA high-risk criteria for ND delay were seen for longitudinal developmental evaluation. Testing included the Bayley Scales of Infant Development – III (BSID-III) at 2 years (±3 months) of age, and standardized neuropsychological measures at 4 years. Scores were compared to test norms and were classified as: average (within one SD of test mean); at risk (1-2 SDs from the test mean); and impaired (>2SD from test mean). Spearman correlations and McNemar’s exact tests were performed to determine the relationship between test scores at the two times of assessment.
Results: Of the 102 patients evaluated at 4 years of age, 73% (n=75) had a previous evaluation using the BSID-III; 48 (47%) completed the BSID-III at 24±3 months of age. Median age at first cardiac operation was 13 days. Patients had the following characteristics: single ventricle anatomy 33%; male 63%; prenatal diagnosis 53%; premature 18%; non-white/Hispanic race 13%; and comorbidities: medical 25%, genetic 17%. BSID-III cognitive, language, and motor scores were correlated with preschool IQ, language, and motor scores, r = 0.49 to 0.75, all p<0.01. Of the patients who had average or above BSID-III cognitive scores at age 2, 29.7% scored in the at risk or delayed range on the preschool IQ test.
Conclusion: BSID-III scores at 2 years are significantly associated with ND outcomes at 4 years. However, even though scores were related, many patients who scored in the average range at age 2 showed some deficits at age 4. Therefore, longitudinal ND assessment is recommended.
Article Information
vol. 134 no. Suppl 1 A12569
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Cheryl L Brosig1;
- Laurel Bear1;
- Sydney Allen1;
- Raymond G Hoffmann1;
- Amy Pan1;
- Michele Frommelt1;
- Kathleen A Mussatto2
- 1Pediatrics, Med College of Wisconsin, Milwaukee, WI
- 2Herma Heart Cntr, Children’s Hosp of Wisconsin, Milwaukee, WI
Abstract 11245: Normal Findings in Late Gestation Fetal Echocardiography
Lauren Tague, Mary T Donofrio, Amanda Fulgium, Robert McCarter, Catherine Limperopoulos, David Schidlow
Circulation. 2016;134:A11245
Abstract
Introduction: Fetal echocardiography (FE) provides detailed information about cardiac structure and function in-utero. Limited information is available regarding normal findings late in pregnancy. We sought to identify and describe common FE findings in late gestation.
Methods: Fetuses with structurally normal hearts at mid-gestation were identified within a subset of pregnant women in a prospective study. Atrioventricular (AV) valves, right and left atrium (RA/LA), aortic isthmus (AoI) and ductal arch (DA) diameters and flow abnormalities, septum primum aneurysm (SPA), and presence/grade of tricuspid regurgitation (TR) were assessed. Linear and logistic regression analyses were used to characterize change in quantitative and qualitative FE parameters.
Results: 40 fetuses were studied. Each had a FE completed before and after 34 weeks gestation. Studies were compared. RA/LA and tricuspid/mitral valve (TV/MV) ratios increased with GA (p<0.001). Increased AoI and DA diastolic flow, and trivial/mild TR were more frequently identified after 34 weeks gestation. Increased AoI diastolic flow, DA narrowing, DA diastolic flow, TR, and SPA increased linearly with GA (p<0.001).
Conclusion: Mild RA/LA and AV valve disproportion, trivial/mild TR, isolated AoI diastolic flow, mild DA narrowing, and SPA are frequently seen after 34 weeks GA. This suggests these FE findings in isolation are likely normal as physiologic changes occur in late gestation. Figure 1: RA/LA disproportion and AV disproportion increase with gestational age. P<0.001.
Article Information
vol. 134 no. Suppl 1 A11245
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Lauren Tague;
- Mary T Donofrio;
- Amanda Fulgium;
- Robert McCarter;
- Catherine Limperopoulos;
- David Schidlow
- Cardiology, Children’s National Med Cntr, Washington, DC
Abstract 20924: Liver Fibrosis Increases Inferior Vena Caval Flow and Power Output of the Heart in Single Ventricle Patients After Fontan
Phillip M Trusty, Zhenglun Wei, Pierre A Russo, Lea F Surrey, David Goldberg, Jack Rychik, Mark A Fogel, Ajit P Yoganathan
Circulation. 2016;134:A20924
Abstract
Introduction: The staged Fontan procedure has shown promising short term outcomes in single ventricle patients. However, Fontan-associated liver disease is a marked problem seen in this population as patients age. In this study, we investigate the relationship between hemodynamics and liver fibrosis in Fontan patients.
Hypothesis: The extent of liver fibrosis in Fontan patients is associated with poor total cavopulmonary connection hemodynamics.
Methods: Thirty-three Fontan patients with liver fibrosis were included in this study. Cardiac magnetic resonance (CMR) and phase-contrast CMR data, as well as catheterization measurements and liver biopsies were obtained for each patient. Computational fluid dynamic simulations were performed to quantify TCPC hemodynamics using patient specific anatomies and blood flow waveforms reconstructed from CMR data. Collagen deposition (as a measure of liver fibrosis) was quantified by digital image analysis of Sirius Red stained slides. Statistical analyses were performed to investigate potential relationships between liver fibrosis and Fontan hemodynamics.
Results: Patient clinical data is shown in Figure 1A. Indexed IVC flow showed a significant, positive correlation with liver fibrosis (r=0.563, p=0.001, Figure 1B). Upper and lower Sirius Red tertile comparisons showed a significant difference in indexed IVC flow (p=0.006, Figure 1D). Liver fibrosis was found to be more related to global metrics (IVC flow, ventricle power output) than local TCPC hemodynamics (Figure 1C).
Conclusions: Significant increases in IVC flow consistent with fibrosis induced arterialization and ventricular power output suggests a burden being placed on the single ventricle from liver fibrosis. Local TCPC flow dynamics do not seem to influence the degree of fibrosis. Favorable TCPC hemodynamics may not be enough to overcome the power shortage and elevated venous pressures inherent to a Fontan patient.
Article Information
vol. 134 no. Suppl 1 A20924
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Phillip M Trusty1;
- Zhenglun Wei2;
- Pierre A Russo3;
- Lea F Surrey3;
- David Goldberg4;
- Jack Rychik4;
- Mark A Fogel4;
- Ajit P Yoganathan2
- 1Biomedical Engineering, Georgia Institute of Technology, Peachtree City, GA
- 2Biomedical Engineering, Georgia Institute of Technology, Atlanta, GA
- 3Div of Pathology and Laboratory Medicine, Children’s Hosp of Philadelphia, Philadelphia, PA
- 4Div of Cardiology, Children’s Hosp of Philadelphia, Philadelphia, PA
Abstract 19714: Growth Parameters, Bone Mineral Density and Secondary Hyperparathyroidism After Fontan Operation: Results From the Multidisciplinary Clinic at the CHOP Single Ventricle Survivorship Program
Edna E Mancilla, Benjamin Zielonka, Jill Brodsky, Jeffrey Roizen, Babette Zemel, David J Goldberg, Kathryn M Dodds, Jack Rychik
Circulation. 2016;134:A19714
Abstract
Background/Objectives: Height and lean mass deficits are reported in patients with single ventricle physiology after Fontan operation (FO). Our objective is to determine growth, areal bone mineral density (aBMD) and related outcomes in a large population of patients with single ventricle physiology after FO.
Methods: Cross sectional evaluation through chart review of patients followed in our multidisciplinary Single Ventricle Survivorship Program clinic from Jan. 2011 through Aug. 2015. Standardized evaluation includes anthropometry, biochemistry and bone densitometry (DXA).
Results: 210 patients were included in the study at mean age of 11.8 ± 4.8 yrs (90 female, 120 male); 65% had dominant right ventricle and 44% hypoplastic left heart syndrome. Median age at FO was 31 mos (7.6-135.8); 25 had current or a history of protein losing enteropathy (PLE). Mean height Z score was -0.73 ± 1.35 after excluding patients with genetic syndromes, and -0.65 ± 1.42 after excluding patients with PLE. Mean height Z score for those with PLE was -1.99 ± 1.02. Overall mean weight and BMI Z scores were -0.64 ± 1.54 and -0.14 ± 1.16 respectively. Height adjusted (HA) whole body less head (WBLH) BMD Z score was -1.18 ± 1 for those without PLE, and -2.4 ± 0.58 for those with PLE. HA Lumbar Spine (LS) BMD Z score was -0.22 ±1.02 for those without PLE and -1.29 ± 1.42 for those with PLE. Laboratory values in those without PLE were significant for mean parathyroid hormone (PTH) 55.5 ± 35.4 pg/mL (normal range = 9-52) and 25 OH Vitamin D 31.7 ± 11.7 ng/mL. Overall PTH was above normal in 47% and 13% had low Vitamin D (<20 ng/mL), with higher PTH values in those with PLE (high PTH in 84%). Serum albumin, calcium and alkaline phosphatase were markedly lower in those with PLE. Height Z scores correlated with dominant right ventricle. WBLH BMD Z scores correlated with PTH and LS BMD Z scores correlated with calcium, independent of dominant ventricle.
Conclusions: Children after FO have significant deficits in height, BMD and commonly exhibit secondary hyperparathyroidism. Greater abnormalities are observed in those with PLE. These findings are part of a myriad of increasingly recognized end-organ consequences that define a “Fontan circulatory syndrome” and require further investigation as to etiology and treatment.
Article Information
vol. 134 no. Suppl 1 A19714
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Edna E Mancilla1;
- Benjamin Zielonka2;
- Jill Brodsky3;
- Jeffrey Roizen1;
- Babette Zemel4;
- David J Goldberg5;
- Kathryn M Dodds5;
- Jack Rychik5
- 1Endocrinology, Children’s Hosp of Philadelphia, Philadelphia, PA
- 2J. Stokes Jr. Rsch Inst, Children’s Hosp of Philadelphia, Philadelphia, PA
- 3Endocrinology, The Mid-Hudson Med Group, Poughkeepsie, NY
- 4Pediatrics, Children’s Hosp of Philadelphia, Philadelphia, PA
- 5Cardiology, Children’s Hosp of Philadelphia, Philadelphia, PA
Abstract 19360: Abnormal Cerebral Circulation in Patients With Fontan Circulation
Clara Kurishima, Seiko Kuwata, Yoichi Iwamoto, Hirofumi Saiki, Hirotaka Ishido, Satoshi Masutani, Hideaki Senzaki
Circulation. 2016;134:A19360
Abstract
Background: Impairment of higher brain function often occurs in patients who have undergone Fontan surgery. Apart from the surgery being conducted immediately after birth, abnormalities of the cerebral circulation induced by reduced systemic blood flow and higher central venous pressure in the Fontan circulation may be responsible for this. We tested our hypothesis that patients with Fontal circulation have abnormal cerebral circulation.
Methods: The subjects were 43 patients who had undergone Fontan surgery (Fontan group) and, as a control group, 24 patients who had undergone surgery for tetralogy of Fallot (TOF group). The blood flows in the common carotid artery, superior vena cava (SVC) and inferior vena cava (IVC), as well as the cardiac index (CI), were measured on MRI scan. Oxygen consumption and the oxygenation balance index (OBI), reflecting the ratio between oxygen supply and demand of the upper and lower halves of the body, were calculated from the cardiac catheterization data.
Results: The blood flows in the common carotid artery and SVC correlated positively with CI in both groups (Fontan group: r = 0.89, 0.93, P < 0.00001; TOF group: r = 0.95, 0.78, P < 0.001, respectively), suggesting that low cardiac output directly affects cerebral circulation. The relationship between CI and blood flow ratio between SVC and IVC (SVC/IVC flow ratio) remained stable regardless of CI in the TOF group, but in the Fontan group, CI correlated positively with SVC/IVC flow ratio. It was therefore suggested that, in the Fontan group, cerebral blood flow is difficult to maintain when cardiac output is low. The OBI was maintained around 1 (1.1 ± 0.4) in the Fontan group, but the cases with OBI < 1 had decreased blood flows in both the common carotid artery and the SVC. In the Fontan patients, when blood flow was reduced in the upper half of the body, increases in oxygen extraction represented by ▹SatO2 = (SatO2aAo-SatO2SVC) were not sufficient to maintain cerebral oxygen consumption.
Conclusion: In the Fontan group, although cerebral oxygen consumption tends to be reduced when the blood flow distribution to the brain is decreased, compensation is not adequate. This suggests difficulty in maintaining the balance between cerebral oxygen supply and demand in Fontan circulation.
Article Information
vol. 134 no. Suppl 1 A19360
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Clara Kurishima;
- Seiko Kuwata;
- Yoichi Iwamoto;
- Hirofumi Saiki;
- Hirotaka Ishido;
- Satoshi Masutani;
- Hideaki Senzaki
- Pediatric Cardiology, Saitama Med Cntr, Saitama Med Univ, Kawagoe, Japan
Abstract 17858: Decline in Peak Oxygen Consumption on Serial Cardiopulmonary Exercise Tests Predicts Death or Transplantation in Adults With a Single Ventricle Fontan Circulation
Jonathan W Cunningham, Jonathan Rhodes, Keri M Shafer, Alexander R Opotowsky
Circulation. 2016;134:A17858
Abstract
Introduction: Peak oxygen consumption (pVO2) measured by cardiopulmonary exercise testing (CPET) predicts mortality in adults with a Fontan circulation. We investigated the additive prognostic value of change in pVO2 over time.
Hypothesis: We hypothesized that change in pVO2 between consecutive CPETs would predict time to death or transplantation in adults with a Fontan circulation.
Methods: We analyzed all adult patients with a Fontan circulation at our institution between 2003-2015 with 2 maximal (RER>1.05) CPETs separated by 6-30 months. Freedom from death or cardiac transplant was analyzed using Log Rank tests and Cox regression, with % change in pVO2 (mL/kg/min) between the 2 CPETs as the independent variable (univariate and adjusting for baseline pVO2). Change in pVO2 was also analyzed as a dichotomous variable.
Results: The study included 268 CPET pairs from 124 patients. Age averaged 26.6+/-9.5 years, 41% were female and the most common underlying diagnoses were tricuspid atresia (31.0%), double inlet left ventricle (19.8%) and hypoplastic left heart syndrome (19.0%). Average time between CPETs was 1.3+/-0.5 years. Eleven patients died and 2 underwent transplant. On average, pVO2 declined 9.8+/-14.6% between tests for patients who subsequently died or underwent transplant; in contrast, there was no change for those who did not suffer this outcome (0.0+/-13.0%). Decrease in pVO2 between tests was associated with increased risk of death or transplant in univariate analysis (per 10% decrease in pVO2, HR 1.9, 95%CI 1.2-3.0, p=0.004) (figure shows change in pVO2 as dichotomous variable). Change in pVO2 remained a significant predictor after controlling for baseline pVO2 (HR 2.5, 1.6-4.1, p<0.001).
Conclusions: A decline in pVO2 between consecutive CPETs predicts increased risk for death or transplant in adults with a Fontan circulation independent of initial pVO2. These results support the additive clinical value of serial CPET in this group of patients.
Article Information
vol. 134 no. Suppl 1 A17858
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Internal Medicine, Brigham and Women’s Hosp, Boston, MA
- 2Cardiology, Boston Children’s Hosp, Boston, MA
Abstract 17908: Changes in Gut Microbiome Early After Fontan Operation
Jyoti K Patel, Ceylan E Tanes, Kyle Bittinger, Kathryn Dodds, David J Goldberg, Frederic D Bushman, Gary D Wu, Jack Rychik
Circulation. 2016;134:A17908
Abstract
Introduction: A growing body of evidence supports the role of the gut microbiome in human health and well-being. The unique physiological conditions imposed by the Fontan operation (FO) may influence intestinal circulation and oxygen delivery thus altering the gut microbiome.
Methods: Stool samples were obtained in children just prior to FO (T1), early postop within 5-7 days after FO (T2), and late postop 3-9 months after FO (T3). At early postop T2 all subjects were taking oral feeds, had at least one well-formed bowel movement and were off all cardiovascular infusions. Shotgun metagenomic sequencing of the microbiota was performed. Community-level differences between time points were assessed by PERMANOVA tests of Bray-Curtis distance between samples. Differentially abundant taxa were identified by generalized linear mixed models. Enteric protein loss was measured by level of stool alpha-1-antitrypsin concentration and its relationship to the gut microbiota was explored.
Results: Specimens from 32 subjects with single ventricle and bidirectional Glenn undergoing FO were studied. Mean age at surgery was 39 +/- 8 months. A significant difference in species composition was noted between T1 and T2 (p=0.043) and T2 and T3 (p=0.003), but not between T1 and T3. Significant differences in specific taxa abundance were seen at T2, with increased Escherichia and decreased Eubacterium and Faecalibacterium as compared to T1 and T3. Two subjects with subclinical enteric protein loss post-operatively had a unique alteration of bacterial populations, with increased abundance of Coprobacillus and decreased abundance of Bacteroides and Ruminococcusas compared to the rest of the population.
Conclusions: The gut microbiota is acutely perturbed at the time of FO with re-establishment of the populations within a few months after surgery. Whether this change is related to the stressors of cardiac surgery in the child in general, or specific to the acute imposition of a Fontan circulation with subsequent accommodation is uncertain. Additionally, children with subclinical enteric protein loss have altered gut microbiome as compared to those without. Further study of the impact of the Fontan circulation on the gut microbiome in the older child and adult is warranted.
Article Information
vol. 134 no. Suppl 1 A17908
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Jyoti K Patel1;
- Ceylan E Tanes2;
- Kyle Bittinger2;
- Kathryn Dodds1;
- David J Goldberg1;
- Frederic D Bushman3;
- Gary D Wu4;
- Jack Rychik1
- 1Div of Cardiology/EP, 8NW, Children’s Hosp of Philadelphia, Philadelphia, PA
- 2Dept of Microbiology, Perelman Sch of Medicine, Univ of Pennsylvania, Philadelphia, PA
- 3The Dept of Microbiology, Perelman Sch of Medicine, Univ of Pennsylvania, Philadelphia, PA
- 4Div of Gastroenterology, Perelman Sch of Medicine, Univ of Pennsylvania, Philadelphia, PA
Abstract 16895: Relationship of Activity Energy Expenditure With Autonomic Balance and Liver Congestion in Patients With Fontan Circulation
Akiko Yana
Circulation. 2016;134:A16895
Abstract
Background: CVP increases with physical activity (PA) in Fontan circulation; therefore, excessive PA can be deleterious as it causes organ congestion. Contrarily, moderate exercise has beneficial effects in patients with heart failure, including improvement in autonomic nerve balance, resulting in better prognosis. However, no data are available regarding whether and how the intensity of PA affects the pathophysiology of Fontan patients. To our knowledge, this is the first study that assessed the effects of daily PA on hepatic congestion and autonomic balance in patients with Fontan circulation and determined the ideal intensity of PA for them.
Methods: Daily PA was assessed by activity energy expenditure (AEE) in 37 Fontan patients (3.8-42 years) who wore a high-accuracy accelerometer (Actical®) continuously for 2 weeks. We examined the relationship of the AEE values with γ-GTP, as an indicator of hepatic congestion, and heart rate variability (HRV), as an indicator of autonomic balance. Additionally, AEE/cardiac output (CO) was calculated as an index to assess whether the AEE and CO of the patients matched.
Results: Patients were divided into 4 groups based on the median values of γ-GTP and high-frequency power (HF) obtained through the HRV analysis. AEE was the highest in the “low HF-high γ-GTP” group, which is considered to have the worst prognosis, and was significantly higher than that of the “high HF-high γ-GTP” group (p<0.05). Furthermore, AEE/CO of the “low HF-high γ-GTP” group was significantly higher than that of the other groups, suggesting that patients with unfavorable autonomic balance and congestive liver performed excessive PA that did not match the level of CO. The group with the lowest AEE was the “low HF-low γ-GTP” group, suggesting that minimum activity was beneficial for liver function, but deleterious for autonomic balance. The AEE/CO of the “high HF-low γ-GTP” group (78.5±34.5), which is considered to have the best prognosis, was very close to the average AEE/CO values of all patients, suggesting that the PA performed by the patients in this group matched their CO.
Conclusion: Daily PA improves autonomic balance but causes hepatic congestion in Fontan patients. Customized AEE needs to be determined for each Fontan patient to improve prognosis.
Article Information
vol. 134 no. Suppl 1 A16895
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Akiko Yana
- Pediatrics, Saitama Med Cntr, Kawagoe City, Japan
Abstract 16480: Factors That Affect Activity Energy Expenditure of Fontan Patients
Akiko Yana
Circulation. 2016;134:A16480
Abstract
Background: There is a general trend favoring the recommendation of adequate exercise for Fontan patients. However, its effect on hemodynamics and safety have yet to be clarified. It is clearly very important to ascertain how the daily activity amount and activity intensity are associated with hemodynamics in Fontan patients.
Objectives: This study aimed to measure activity energy expenditure (AEE) and activity intensity in Fontan patients and examine their associations with hemodynamics.
Method: In total, 41 Fontan patients (3.5 to 42.3 years of age; mean, 9.6 years) were fitted with a high-accuracy portable accelerometer for 2 consecutive weeks and AEE was calculated and compared with the values of hemodynamics parameters obtained by cardiac catheterization.
Results: AEE in Fontan patients was 237 ± 95 kcal/day, showing a negative correlation with heart rate (HR; 84.7 ± 17.4 bpm, p<0.01) and positive correlations with cardiac output (CO; 2.9 ± 0.9 L/min, p<0.05) and stroke volume (SV; 36.0 ± 16.2 mL) (p <0.01). AEE also showed significant correlations (HR, p<0.01; SV, p = 0.01) in a multivariate analysis adjusted for age. These parameters showed stronger correlations when activity was light (1.0 to 3.0 Mets), which accounts for approximately 70% of the time in daily AEE (HR, p<0.01; SV, p<0.01). Meanwhile, AEE did not correlate with central venous pressure (CVP), pulmonary to systemic flow (Qp/Qs) ratio, pulmonary vascular resistance (Rp), or SpO2. Furthermore, as compared with CO values, the γ-GTP level, an indicator of hepatic congestion detected by blood testing, was significantly higher (63.9 ± 28.1 vs. 40.4 ± 27.6, p<0.05) in those with high AEE values than in other patients.
Conclusion: Our results suggest that the amount of daily activity in Fontan patients may be primarily affected by HR and SV. Also, high activity not corresponding to CO may lead to exacerbation of liver dysfunction.
Article Information
vol. 134 no. Suppl 1 A16480
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Akiko Yana
- Pediatrics, Saitama Med Cntr, Kawagoe city, Japan
Abstract 16230: Fenestration in the Fontan Circulation Secures Circulatory Reserve~Potential for Chronic Cardio-protective Strategy~
Hirofumi Saiki, Seiki Kuwata, Clara Kurishima, Yoichi Iwamoto, Hirotaka Ishido, Satoshi Masutani, Hideaki Senzaki
Circulation. 2016;134:A16230
Abstract
Background: Fontan patients are increasingly subjected to advanced heart failure therapies due to end organ failure, which stems from Fontan specific hemodynamics. Since fenestrated Fontan (FF) procedure accelerates recovery from operation insults and preserves exercise capacity, it may liberate patients from the factors driving circulatory compromise. We hypothesized that FF possesses hemodynamic advantages over preservation of preload.
Methods and Results: Thirty Fontan pts (age 4.0±2.0 yrs) with constructed pressure volume relationship under dobutamine infusion (DOB) and/or transient fenestration occlusion (TFO) were enrolled. In FF pts (n=19), TFO suppressed end diastolic volume, stroke volume (SV) and cardiac index (CI), with increasing heart rate (HR), afterload (Ea) and ventricular chamber stiffness β (p<.05 for all), while contractility (Ees, PRSW) remained unchanged. As compared to FF, non-FF pts had a similar but more mild cardiovascular phenotype of FF with TFO. Only HR (baseline 109±6 vs 96±16 bpm, DOB 123±12 vs 105±24 bpm, p<.05) and central venous pressure (CVP, 14±3 vs 11 ±3 mmHg) were particularly higher than FF. To delineate the impact of FF with increasing HR, response to rapid atrial pacing (+20, 40, 60 bpm to pre-TFO HR) with/without TFO was monitored (figure). Marked decline of CI by TFO at baseline was compensated by the increase of HR by 20 bpm. While the product of CI and arterial oxygen saturation (SaO2), as a surrogate of arterial oxygen content, was constant, TFO consistently raised CVP regardless of HR.
Conclusions: As compared with non-FF, CI preservation in FF was mediated by not only preload reserve, but also low afterload and relative decreased ventricular stiffness. In addition, FF pts can achieve circulatory homeostasis with lower levels of HR and CVP than non-FF pts. Since somatic growth ultimately diminishes R-L shunt related to FF, the FF procedure might be a promising strategy to avoid factors driving cardiovascular remodeling.
Article Information
vol. 134 no. Suppl 1 A16230
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Hirofumi Saiki1;
- Seiki Kuwata2;
- Clara Kurishima2;
- Yoichi Iwamoto2;
- Hirotaka Ishido2;
- Satoshi Masutani2;
- Hideaki Senzaki2
- 1Pediatric Cardiology, Saitama Med Cntr, Saitama Med Univ, Kawagoe, Japan
- 2Pediatric Cardiology, Saitama Med Cntr, Saitama Med Univ, Kawagoe, Saitama, Japan
Abstract 15661: Impairment of Thyroid Function in Patients With Fontan Circulation
Seiko Kuwata, Clara Kurishima, Akiko Yana, Yoichi Iwamoto, Hirofumi Saiki, Hirotaka Ishido, Satoshi Masutani, Hideaki Senzaki
Circulation. 2016;134:A15661
Abstract
Background: An increase in central venous pressure (CVP) and decrease in cardiac output (CI) in Fontan circulation may have adverse effects on thyroid function due to congestion and low perfusion of the thyroid gland. Because thyroid hormones play important roles in the regulation of the cardiovascular system, thyroid dysfunction may be involved in the pathophysiology of Fontan circulation. We investigated the pathophysiological relationships between Fontan hemodynamics and thyroid function.
Methods and Results: Thirty-seven consecutive patients who had undergone a Fontan operation (median year after the surgery: 4.2 years) had cardiac catheterization and blood tests for thyroid function. One patient treated with amiodarone was excluded from the analysis. Of these, 9 patients (25%) had subclinical thyroid dysfunction defined as elevated thyroid stimulating hormone (TSH) level, but normal thyroid hormone levels. The levels of TSH were significantly correlated with CVP (P<0.01, R2=0.3), and patients with subclinical hypothyroidism showed significantly elevated levels of gamma-glutamyl transferase, an indicator of liver congestion, compared to the remaining patients (125.6±12.2 vs. 67.6±4.6 IU/L, P<0.01), suggesting the importance of venous congestion as a cause of subclinical hypothyroidism. Although levels of free triiodothyronine (fT3), an effective thyroid hormone, were generally within the normal range, fT3 levels in the subclinical hypothyroidism group were significantly lower than those in the normal thyroid function group (3.1±0.1 vs. 3.5±0.1 pg/dmLl, P<0.01). Furthermore, fT3 was significantly and negatively correlated with relaxation time constant (P=0.03) and brain natriuretic hormone (P<0.01), and positively correlated with CI (P=0.04).
Conclusion: Venous congestion in Fontan patients may cause thyroid dysfunction, and impaired thyroid function can be responsible for decreased ventricular function and cardiac output in Fontan patients. These novel findings suggest that thyroid function should be routinely monitored after Fontan surgery, and that thyroid hormone replacement therapy may be an effective treatment option to improve Fontan hemodynamics.
Article Information
vol. 134 no. Suppl 1 A15661
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Seiko Kuwata;
- Clara Kurishima;
- Akiko Yana;
- Yoichi Iwamoto;
- Hirofumi Saiki;
- Hirotaka Ishido;
- Satoshi Masutani;
- Hideaki Senzaki
- Pediatric cardiology, Saitama Med Cntr, Saitama Med Univ, Saitama, Japan
Abstract 14633: Cardiopulmonary Exercise Testing as a Predictor of Liver Disease in Fontan Patients: Two Tertiary Center Experience
Anushree Agarwal, Colin Cunnington, Aarthi Sabanayagam, Lucas Zier, Charles E McCulloch, Ian S Harris, Elyse Foster, Dougal Atkinson, Angela Bryan, Petra Jenkins, Jaspal Dua, Michael J Parker, Devinda Karunaratne, John Moore, Jeffrey Meadows, Bernard Clarke, Andreas Hoschtitzky, Vaikom S Mahadevan
Circulation. 2016;134:A14633
Abstract
Introduction: Liver disease (LD) is a known long-term complication in single ventricle patients who undergo Fontan procedures. Cardiopulmonary exercise test (CPET) variables are known to be associated with increased risk of hospitalization in Fontan patients but their association with liver disease is unknown.
Methods/Results: We retrospectively reviewed medical records from 2 tertiary academic institutions (Central Manchester University Hospitals, UK and University of California San Francisco, USA) and identified 114 adult Fontan patients (>18 years). LD was defined as grade IV fibrosis or cirrhosis on either ultrasound or computed tomographic imaging. Mean age was 30.9 ± 7.4 years, age at Fontan 7.9 ± 7.9 years, 56% were females, 63% underwent total cavopulmonary connection, 66% had New York Heart Association (NYHA) I, 42% had arrhythmias, 22% had systemic right ventricle and 35% had ventricular dysfunction. Of 81 patients with liver imaging data, 33 (41%) had LD. There were no differences in the demographic or Fontan related variables between those with and without LD. Of 58 patients with CPET data, mean peak maximal oxygen uptake (VO2) was 18.6 ± 5.7 ml/kg/min, percent predicted peak VO2 was 53.9 ± 15.5%, peak O2 pulse was 9.3 ± 2.9 ml/beat and percent predicted peak O2 pulse was 82.6 ± 21.5%. For each standard deviation (SD) decrease in % predicted peak VO2 (16%) and % predicted peak O2 pulse (22%), there was 2.3 fold increase in the odds for LD after adjusting for age, NYHA class, institution and type of Fontan (Table 1a). Similarly, each SD decrease in % predicted peak VO2 and % predicted O2 pulse was associated with an estimated 5.9 years and 4.9 years early onset of LD respectively (Table 1b).
Conclusions: CPET measures for aerobic capacity and stroke volume (percent predicted peak VO2 and peak O2 pulse) help predict LD in Fontan patients. Patients with poor exercise tolerance on CPET should be considered for screening for liver disease in addition to standard investigations.
Article Information
vol. 134 no. Suppl 1 A14633
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Anushree Agarwal1;
- Colin Cunnington2;
- Aarthi Sabanayagam1;
- Lucas Zier1;
- Charles E McCulloch1;
- Ian S Harris1;
- Elyse Foster1;
- Dougal Atkinson2;
- Angela Bryan3;
- Petra Jenkins3;
- Jaspal Dua4;
- Michael J Parker3;
- Devinda Karunaratne3;
- John Moore3;
- Jeffrey Meadows1;
- Bernard Clarke3;
- Andreas Hoschtitzky3;
- Vaikom S Mahadevan1
- 1Dept of Cardiology, Univ of California San Francisco, San Francisco, CA
- 2Dept of Cardiology, Manchester Royal Infirmary, Central Manchester Univ Hosps, Manchester, United Kingdom
- 3Dept of Cardiology, Manchester Royal Infirmary, Central Manchester Univ Hospsa, Manchester, United Kingdom
- 4Dept of Cardiology, Manchester Royal Infirmary, Central Manchester Univ Hospsa, Manchester, CA
Abstract 13486: Patient and Procedural Factors Are Associated With Autonomic and Endothelial Dysfunction in Adolescent and Young Adult Fontan Survivors
Bryan H Goldstein, Bradley S Marino, Zhiqian Gao, Philip R Khoury, Michelle A Amos, Wayne A Mays, Gruschen R Veldtman, Andrew N Redington, Elaine M Urbina
Circulation. 2016;134:A13486
Abstract
Introduction: Vascular dysfunction is associated with diminished functional capacity and quality of life in adolescent and young adult Fontan survivors. Patient and procedural factors associated with diminished endothelial and autonomic function have not been established.
Methods: Cross-sectional single-institution study of Fontan survivors ages 8-25 years. Anthropometric characteristics were obtained. Endothelial function was assessed with brachial flow mediated dilation (FMD) and peripheral arterial tonometry reactive hyperemia index (lnRHI; EndoPAT). Autonomic function was assessed by heart rate variability (HRV; SphygmoCor). Records were reviewed for anatomic, hemodynamic and surgical characteristics, which served as predictor variables while vascular measures served as outcome variables. Bivariate predictors (p<0.1) were candidates for inclusion in multivariable models. Model development utilized linear regression techniques.
Results: Sixty patients (52% male, 90% Caucasian) completed the protocol with a mean age of 13.9 ± 4.1 years and duration of Fontan circulation of 9.9 ± 4.2 years. Median weight was 43.5 (IQR 31.4, 58.3) kg and BMI was 18.7 (16.1, 22.6) kg/m2. A single left ventricle was present in 65%. Mean FMD was 10.2 ± 5.5% and lnRHI was 0.236 ± 0.398. Median HRV was 41.2 (29.4, 52.0) ms. Major determinants of FMD included height, total # of surgeries and stage I palliation length of stay (LOS) (R2 0.29, p<0.001), whereas determinants of lnRHI included prior Norwood procedure, systolic blood pressure, resting heart rate and oxygen saturation (SaO2), mixed venous SaO2 and cardiac index (CI) at pre-Fontan catheterization (cath) and total # of hospitalizations (R2 0.27, p=0.01). Major determinants of HRV included total duration of surgical circulatory arrest, CI at pre-Fontan cath and Fontan completion LOS (R2 0.39, p=0.006). Traditional cardiovascular risk factors including weight and BMI were not independent determinants.
Conclusions: Multiple patient and procedural factors are associated with diminished endothelial and autonomic function in adolescent and young adult Fontan survivors. Targeted intervention of modifiable risk factors may improve long-term vascular health and functional status.
Article Information
vol. 134 no. Suppl 1 A13486
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Bryan H Goldstein1;
- Bradley S Marino2;
- Zhiqian Gao1;
- Philip R Khoury1;
- Michelle A Amos1;
- Wayne A Mays1;
- Gruschen R Veldtman1;
- Andrew N Redington1;
- Elaine M Urbina1
- 1The Heart Institute, Cincinnati Children’s Hosp Med Cntr, Cincinnati, OH
- 2Pediatrics, Northwestern Univ Feinberg Sch of Medicine and Lurie Children’s Hosp, Chicago, IL
Abstract 12757: Prevalence and Outcome of Thrombotic and Embolic Complications in Adults After Fontan Operation
Alexander Egbe, Heidi Connolly, Talha Niaz, David Driscoll
Circulation. 2016;134:A12757
Abstract
Introduction: There are limited studies of thrombotic and embolic complications (TEC) in the adult Fontan population.
Hypothesis/objectives: To determine the prevalence, risk factors, and outcomes of TECs in this population.
Method: Review of adults with a previous Fontan operation, followed at Mayo Clinic, 1994-2014. Systemic TEC was defined as intracardiac thrombus, ischemic stroke, or systemic arterial embolus. Non-systemic TEC was defined as Fontan conduit/right atrial thrombus or pulmonary embolus.
Results: We identified 387 patients; mean age 28 ±7 years and follow-up 8±2 years. An atriopulmonary connection (APC) was done for 286/387 patients. Atrial arrhythmias were present in 278/387 (72%). There were 121 TECs (systemic n=36, non-systemic n=85) in 98/387 patients (25%). Risk factors for systemic TEC were atrial arrhythmia (hazard ratio [HR], 2.28; P=.001) and APC (HR, 1.98; P=.02); non-systemic TEC also had similar risk factors.
All 98 patients received warfarin but warfarin was discontinued in 10/98 because of bleeding; and 8 of these 10 had a second TEC after discontinuing warfarin. Thrombi resolution occurred in 16/82 (20%) that continued to receive warfarin 16 (20%) and had follow-up imaging; 8 with other comorbid conditions had Fontan conversion. In total, 24/98 patients had a second TEC, most of whom had inadequate anticoagulation.
Conclusions: TEC was not uncommon; risk factors for TEC were APC and atrial arrhythmias. Most patients were treated successfully with warfarin alone. A second TEC occurred in most patients whose anticoagulation was discontinued because of bleeding events.
Legends Kaplan-Meier Curves comparing freedom from TEC.
(A). Freedom from TECs in all patients and in patients with vs without atrial arrhythmia (AA) (P=.002).
(B). Freedom from TECs in all patients and in patients with vs without atriopulmonary connection (APC) (P=.001). “No APC” group comprise of patients with total cavopulmonary connections.
Article Information
vol. 134 no. Suppl 1 A12757
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Alexander Egbe;
- Heidi Connolly;
- Talha Niaz;
- David Driscoll
- Div of Cardiovascular Diseases, Mayo Clinc, Rochester, MN
Abstract 12103: Vascular Function Affects Aortic Root Dilatation in Patients After Fontan Procedure
Seiji Asagai, Kei Inai, Gen Harada, Mikiko Shimizu, Tetsuko Ishii, Tokuko Shinohara, Hisashi Sugiyama, Hifofumi Tomimatsu, In-Sam Park
Circulation. 2016;134:A12103
Abstract
Introduction: It is well known that, in patients with congenital heart disease, such as Tetralogy of Fallot, aortic root dilatation may gradually progress. Similar phenomenon also occur in patients with single ventricle circulation. However, the factors associated with aortic dilatation in these patients are still unknown.
Hypothesis: We assessed the hypothesis that vascular function associated with the aortic root dilatation after Fontan procedure.
Methods: Between July 2013 and April 2016, sixty-one patients who underwent the Fontan procedure (age, 12.8–55.8 years; median age, 23.2 years; postoperative duration, 8.2-31.3 years; median postoperative duration, 16.8 years) were enrolled. These patients were divided into 2 groups according to the presence or absence of aortic root dilatation and analyzed the relation between aortic root size and clinical profile, vascular function, hemodynamics, and neurohormonal factors. Aortic root dilatation was defined as observed/expected aortic root diameter >1.5 (aortic root dilatation, n=15, aortic root non-dilatation, n=46).
Results and Conclusions: Age at Fontan procedure was significantly higher in the dilatation group than in the non-dilatation group (10.5±7.3 vs 5.3±4.0, P<0.01). FMD was significantly lower in the dilatation group than in the non-dilatation group (5.9±1.4 vs 8.3±2.3, OR 0.49, 95%CI 0.28-0.74, P<0.0001). Pulse wave velocity (PWV) was significantly higher in the dilatation group than in the non-dilatation group (1081±277 vs 943±140, P<0.05). Although hemodynamic variables and neurohormonal factors was not associated with aortic root size, pulmonary atresia was associated with aortic root dilatation (OR 5.43, 95%CI 1.55-20.18, P<0.01). In the multivariate analysis, impaired FMD had a close association with aortic dilatation (OR 0.45, 95%CI 0.19-0.82, P<0.01). FMD showed a negative correlation between age at Fontan procedure, PWV and parameter β(age at Fontan procedure r: -0.56, p<0.0001, PWV r: -0.32, p<0.05, β r: -0.27, p<0.05). We concluded that, in patients after Fontan procedure, vascular dysfunction such as aortic stiffness occurred in the patients who underwent Fontan procedure at older age and may play a role in progressive aortic dilatation.
Article Information
vol. 134 no. Suppl 1 A12103
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Seiji Asagai;
- Kei Inai;
- Gen Harada;
- Mikiko Shimizu;
- Tetsuko Ishii;
- Tokuko Shinohara;
- Hisashi Sugiyama;
- Hifofumi Tomimatsu;
- In-Sam Park
- Pediatric Cardiology, Tokyo Women’s Med Univercity, Tokyo, Japan
Abstract 20647: Sudden Cardiac Death After Atrial Switch Repair for D-Transposition of the Great Arteries: A Systematic Review and Meta-Analysis
Prashanth Venkatesh, Anna M Maw, Arthur T Evans, Agam D Patel, Raymond A Pashun, Kana Fujikura, Irfan Minhas, Luke K Kim, Rajesh V Swaminathan, Dmitriy N Feldman, Robert M Minutello, Geoffrey Bergman, S C Wong, Emile Bacha, Harsimran S Singh
Circulation. 2016;134:A20647
Abstract
Introduction: Patients who underwent atrial switch repair with the Mustard or Senning procedure for D-transposition of the great arteries (D-TGA) in childhood are at risk of late sudden cardiac death (SCD). The existing literature in this area is heterogeneous, consisting of individual cohorts with considerable controversy as to the predictors of SCD in this population.
Methods: A systematic review and meta-analysis was performed of published and unpublished studies documenting long-term mortality of patients undergoing the Mustard or Senning procedure with a mean or median follow-up of at least 10 years. Data describing SCD was extracted. Multiple studies from the same center as well as studies describing patients with palliative atrial switch procedures were excluded.
Results: A total of 23 studies comprising 3803 patients met criteria. The median annual incidence of SCD was 0.22% (IQR 0.16-0.35), with SCD being the single most common cause of late mortality across cohorts. Using a random effects model, pooled odds ratios were calculated for risk factors thought to predispose to late SCD. A history of supraventricular tachyarrhythmia (SVT) was the only significant risk factor for SCD (OR 5.58, 95% CI 2.90-10.74, I2 0) after pooling all 11 studies that provided sufficient patient data to calculate odds ratios (Figure). Other expected risk factors, most notably right ventricular dysfunction (OR 0.69, 95% CI 0.27-1.77, I2 59%) were not predictive of SCD.
Conclusions: SCD is the most common cause of long-term mortality in D-TGA patients after atrial switch. In this meta-analysis, presence of SVT was predictive of SCD, while other risk factors including right ventricular dysfunction were not. Additional studies are required to assess whether aggressive management of SVT, including medications, ablation and even placement of implantable cardioverter-defibrillators can reduce SCD in this population.
Article Information
vol. 134 no. Suppl 1 A20647
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Prashanth Venkatesh1;
- Anna M Maw1;
- Arthur T Evans1;
- Agam D Patel1;
- Raymond A Pashun1;
- Kana Fujikura2;
- Irfan Minhas1;
- Luke K Kim3;
- Rajesh V Swaminathan3;
- Dmitriy N Feldman3;
- Robert M Minutello1;
- Geoffrey Bergman1;
- S C Wong1;
- Emile Bacha4;
- Harsimran S Singh3
- 1Internal Medicine, New York Presbyterian Hosp/ Weill Cornell, New York, NY
- 2Cardiology, Montefiore Med Cntr, New York, NY
- 3Cardiology, New York Presbyterian Hosp/ Weill Cornell, New York, NY
- 4Cardiothoracic Surgery, New York Presbyterian Hosp/ Weill Cornell, New York, NY
Abstract 20508: Out-of-Pocket Medical Costs in Severe Congenital Heart Disease
Justin Elhoff, Kimberly McHugh, Jason Buckley, Kit Simpson, Mark Scheurer
Circulation. 2016;134:A20508
Abstract
Introduction: Families of children born with congenital heart disease (CHD) face myriad stressors. These include financial burdens, which are compounded by uncertainty regarding the amount of responsibility the family will assume for medical bills. Out-of-pocket medical costs for these families has not previously been reported. This study describes the family responsibility for healthcare bills during the first 12 months of life for commercially insured children undergoing surgical repair for transposition of the great arteries, tetralogy of Fallot, and truncus arteriosus.
Methods: The MarketScan database was used to identify commercially insured infants carrying an ICD-9 diagnosis code for one of three forms of severe CHD as well as the corresponding procedure code for corrective operation from 2010-2012. Data extraction determined inpatient, outpatient, and pharmaceutical payment responsibilities of the patients’ families in the form of copayments, deductibles, and co-insurance during their first year of life.
Results: 481 infants with severe CHD undergoing surgical repair were identified (Table 1). The average family responsibility for medical bills was approximately $3000, and some families faced as much as $11,000 in medical bills for which they were responsible. Index hospitalization accounted for 28-37% of out-of-pocket costs, compared to 12-17% for follow-up hospitalization(s), 7-15% for prescriptions, and 38-45% for outpatient visits.
Conclusions: Families of commercially insured children with severe CHD requiring corrective surgery face an average of approximately $3,000 in out-of-pocket costs for healthcare bills over the first 12 months of their child’s life. While these families face enormous additional emotional and financial burdens, this information may provide a framework to alleviate some of the uncertainty surrounding healthcare financial responsibilities.
Article Information
vol. 134 no. Suppl 1 A20508
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Pediatrics, Baylor College of Medicine, Houston, TX
- 2Pediatrics, Med Univ of South Carolina, Charleston, SC
- 3Dept of Healthcare Leadership & Management, Med Univ of South Carolina, Charleston, SC
Abstract 19214: Does Melody Pulmonary Valve Replacement Improve Exercise Tolerance Over a Five-Year Period?
Bryant Priromprintr, Michael J Silka, Jonathan Rhodes, Anjan S Batra
Circulation. 2016;134:A19214
Abstract
Introduction: Percutaneous Melody valve implant is an alternative to surgical valve replacement for right ventricular outflow tract (RVOT) conduit obstruction or insufficiency. However, the long-term benefits of Melody valve implant on exercise capacity remain undefined.
Hypothesis: Melody valve implant results in improvement of objective measures of exercise capacity.
Methods: As part of the phase I Melody valve clinical trial, 136 patients with congenital heart disease underwent serial cardiopulmonary exercise testing (CPET) prior to, 6 months after, and annually for 5 years at implanting centers. CPET was performed on a mechanically braked cycle ergometer. Assessment was performed with baseline pulmonary function testing and ventilation ratios measured at ventilatory anaerobic threshold (VAT).
Results: Mean age at Melody valve implantation was 22.4±0.9 yrs, range 7-53 yrs. There were sustained improvements in predicted maximum workload from 62% pre-implant to a peak of 72% 4 yrs post-implant (p=0.005). Improvements were demonstrated in the ventilatory equivalents for CO2 (VE/VCO2; p=0.01) and O2 (VE/VO2; p<0.001) at VAT. Maximal oxygen consumption (peak VO2) and peak heart rate were not significantly changed (p>0.05). There were significant improvements in forced vital capacity (75% pre-implant vs peak 81% at 4 yrs, p=0.02) and first second forced expiratory volume (73% pre-implant vs peak 78% at 4 yrs, p=0.01), with some decline in the spirometric values noted at 5 yrs. Observed improvements in measures of exercise capacity occurred primarily in the first 6 months post-implant.
Conclusions: Melody valve implant is associated with initial improvements in exercise tolerance and ventilation-perfusion matching at 6 months that were sustained throughout follow-up. Observed changes indicate improvement in restrictive lung physiology, which may be related to RV dilation prior to implant.
Article Information
vol. 134 no. Suppl 1 A19214
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Pediatric, Children’s Hosp of Los Angeles, San Mateo, CA
- 2Pediatric, Children’s Hosp of Los Angeles, Los Angeles, CA
- 3Pediatric, Children’s Hosp of Boston, Boston, MA
- 4Pediatric, Univ of California Irvine, Orange, CA
Abstract 18280: Mucociliary Clearance Deficit and Reduced Pulmonary Function in Congenital Heart Disease Infants Undergoing Surgery With Cardiopulmonary Bypass
Phillip S Adams, Timothy E Corcoran, Daniel J Weiner, Maliha Zahid, Al Saville, Stephen A Walczak, Omar Khalifa, Michael S Czachowski, Yuliya Domnina, Mahesh S Sharma, Brian Blasiole, Patrick M Callahan, Ivy Lin, Joan Sanchez-de-Toledo, Cecilia W Lo
Circulation. 2016;134:A18280
Abstract
Introduction: Postoperative pulmonary complications are common after congenital cardiac surgery requiring cardiopulmonary bypass (CPB). Given our previous finding of a high prevalence of airway ciliary dysfunction (CD) in congenital heart disease (CHD) patients, we hypothesized CHD patients with CD may exhibit a greater reduction in post-CPB pulmonary function.
Methods: We recruited 14 CHD infants (<2 years) requiring cardiac surgery with CPB. Nasal scrapes were obtained to assess respiratory ciliary motion by videomicroscopy. Either pre- or postop mucociliary clearance (MCC) scans were conducted at the bedside using technetium sulfur colloid with a portable gamma camera. Spirometry was assessed using a forced deflation (FD) technique.
Results: MCC scans were conducted on 14 CHD infants (3 pre- and 11 postop, most within 48 hours of surgery). MCC scans postop showed significantly less airway clearance than preop scans (2.8% ±4.2 vs. 21.3% ±7.5; p=<0.0001) (Figure 1). This difference did not correlate with CD. Respiratory compliance was significantly less postop as compared to preop (0.9 ml/cmH2O/kg ±0.47 [n=6] vs. 2.16 ml/cmH2O/kg ±0.53 [n=7]; p=0.001). Infants with CD had lower pulmonary compliance (0.76 ml/cmH2O/kg ±0.41 vs. 1.97 ml/cmH2O/kg ±0.63, p=0.012) and trended toward higher resistance (81.63 cmH2O/L/sec ±11.34 vs. 58.38 cmH2O/L/sec ±20.24, p=0.094). Consistent with this, the degree of CD and respiratory compliance showed a negative correlation (r= -0.52, p=0.082).
Discussion: This is the first study to assess MCC and spirometry in CHD infants undergoing cardiac surgery with CPB. The finding of significantly depressed MCC in the immediate postop period indicates postop outcomes may be improved with pulmonary therapies to enhance infant MCC. The lower pulmonary compliance seen in CHD infants with CD would suggest further studies are needed to investigate the effects of CD on postsurgical pulmonary outcomes in CHD patients.
Article Information
vol. 134 no. Suppl 1 A18280
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Phillip S Adams1;
- Timothy E Corcoran2;
- Daniel J Weiner3;
- Maliha Zahid4;
- Al Saville5;
- Stephen A Walczak6;
- Omar Khalifa4;
- Michael S Czachowski7;
- Yuliya Domnina8;
- Mahesh S Sharma9;
- Brian Blasiole1;
- Patrick M Callahan1;
- Ivy Lin8;
- Joan Sanchez-de-Toledo8;
- Cecilia W Lo4
- 1Anesthesiology, Univ of Pittsburgh Sch of Medicine, Pittsburgh, PA
- 2Medicine, Univ of Pittsburgh Sch of Medicine, Pittsburgh, PA
- 3Pediatric Pulmonology, Univ of Pittsburgh Sch of Medicine, Pittsburgh, PA
- 4Developmental Biology, Univ of Pittsburgh Sch of Medicine, Pittsburgh, PA
- 5Critical Care Medicine, Children’s Hosp of Pittsburgh of UPMC, Pittsburgh, PA
- 6Pediatric Pulmonology, Children’s Hosp of Pittsburgh of UPMC, Pittsburgh, PA
- 7Radiology, Children’s Hosp of Pittsburgh of UPMC, Pittsburgh, PA
- 8Critical Care Medicine, Univ of Pittsburgh Sch of Medicine, Pittsburgh, PA
- 9Cardiothoracic Surgery, Univ of Pittsburgh Sch of Medicine, Pittsburgh, PA
Abstract 17866: Long-Term Outcome Following Percutaneous Closure of Isolated Secundum Atrial Septal Defects in Children: A French Nationwide Series of 1000 Consecutive Patients
Zakaria Jalal, Lucia Mauri, Claire Dauphin, Celine Gronier, Sebastien Hascoet, Bruno Lefort, Mathias Lachaud, Jerome Petit, Caroline Ovaert, Jean-Rene Lusson, Alain Fraisse, Xavier Pillois, Jean-Benoit Thambo, Alban-Elouen Baruteau
Circulation. 2016;134:A17866
Abstract
Introduction: Transcatheter closure has become the preferred treatment strategy in most cases of isolated, secundum atrial septal defect (ASD). Although widely used, data on long-term outcomes in the pediatric population are scarce.
Hypothesis: ASD closure in children provides favourable long term outcome.
Methods: A 1998-2014 retrospective multicentre study was performed at 8 French tertiary institutions, including all patients <18 yo who attempted a percutaneous ASD closure with an Amplatzer Septal Occluder.
Results: 1000 children [38% males, median age: 9 yrs (0.7-18.0), median weight: 27 kg (6-92)] were referred for transcatheter ASD closure. They all had a significant left-to-right shunting assessed by right ventricular dilation and/or a 1.5:1 Qp/Qs ratio; Median ASD size was 15 mm in transthoracic echography (TTE). ASD closure was guided by fluoroscopy and transoesophageal echocardiography in 627 cases (62.7%) or TTE in 373 cases (37.3%). Procedural success rate was 94% with a median occluder size of 19-mm (4 – 40). Device placement was unsuccessful in 60 patients (6%) due to unfavourable anatomy in 38, early device embolization in 12 and other causes in 10 patients. Follow-up (FU) data were available for 829 patients. After a mean FU of 53 ± 31 months (range, 5-204), all patients were alive and 96% were asymptomatic. Long-term complications included supraventricular arrhythmias (n=6) and pulmonary hypertension (n=2). No cardiac erosion, late ASO dislodgement or stroke occurred. Seventy-one women had pregnancy during FU without any associated complication. From an electrical standpoint, supraventricular arrhythmias occurred in 6 patients, no late atrioventricular block was observed and there was no significant difference between preprocedural and last follow-up ECG.
Conclusions: Our large-scale pediatric cohort confirms that transcatheter closure of isolated secundum ASDs is a safe procedure in children, with a favourable long-term outcome and no life-threatening delayed complication.
Article Information
vol. 134 no. Suppl 1 A17866
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Zakaria Jalal1;
- Lucia Mauri2;
- Claire Dauphin3;
- Celine Gronier4;
- Sebastien Hascoet5;
- Bruno Lefort6;
- Mathias Lachaud7;
- Jerome Petit8;
- Caroline Ovaert9;
- Jean-Rene Lusson3;
- Alain Fraisse2;
- Xavier Pillois1;
- Jean-Benoit Thambo1;
- Alban-Elouen Baruteau10
- 1Pedaitric and congenital cardiology, Univ Hosp of Bordeaux, Bordeaux, France
- 2Pedaitric and congenital cardiology, Univ Hosp of Marseille, Marseille, France
- 3Pedaitric and congenital cardiology, Univ Hosp of Clermont-Ferrand, Clermont Ferrand, France
- 4Pedaitric and congenital cardiology, Univ Hosp of Strasbourg, Strasbourg, France
- 5Pedaitric and congenital cardiology, Univ Hosp of Toulouse, Toulouse, France
- 6Pedaitric and congenital cardiology, Univ Hosp of Tours, Tours, France
- 7Pedaitric and congenital cardiology, Univ Hosp of Nantes, Nantes, France
- 8Pedaitric and congenital cardiology, Cntr Chirurgical Marie Lannelongue, Le Plessis Robinson, France
- 9Pedaitric and congenital cardiology, Univ Hosp of Marseille, Marselle, France
- 10Pedaitric and congenital cardiology, Univ Hosp of Bordeaux, London, United Kingdom
Abstract 17363: Has Survival of Patients With Heterotaxy Syndrome Improved in the Current Era?
Puja Banka, Barbara Schaetzle, Adi Adar, Lynn Sleeper, Tal Geva
Circulation. 2016;134:A17363
Abstract
Introduction: Most reports on outcomes in heterotaxy syndrome (HS) have focused on early mortality with little information on long-term survival. Some reports suggest improved survival in more recent years, but others have failed to show similar results.
Hypothesis: Mid- to long-term outcomes for HS have improved over time.
Methods: Patients with HS born between 1985 and 2007 were included. Kaplan-Meier analysis and log-rank test were used to estimate and compare the survival distributions of three birth cohorts (E1=1985-1991, E2=1992-1998, E3=1999-2007). Risk factors for mortality were identified using Cox proportional hazards regression and a stepwise multivariable model constructed.
Results: The 160 patients were 53% female, 53% diagnosed prenatally, 89% with ≥1 cardiac surgery; 80 (50%) died. Anatomic diagnoses, age at first surgery, and rates of single versus biventricular circulation were similar across cohorts. Estimated 15-year survival was 56%, with no birth era difference (E1=51%, E2=58%, E3=60%, p=0.3). Rates of prenatal diagnosis were higher in E3 (E1=36%, E2=51%, E3=77%, p<0.001) but prenatal diagnosis was not associated with mortality (p=0.3). Among those who underwent surgery (n=140), independent risk factors for mortality (all p<0.001) were: totally anomalous pulmonary venous connection (TAPVC; HR=3.2, 95% CI 1.9-5.5), single ventricle palliation (HR=2.3, 95% CI 1.1-4.8) or other non-biventricular surgeries (HR=8.1, 95% CI 2.7-24.6), and ≥mild atrioventricular valve regurgitation (AVVR) at presentation (HR=2.2, 95% CI 1.3-3.7). We found no risk factors that depended on birth era.
Conclusions: Patients with HS have poor long-term survival with no significant improvement in mortality rates over time. Prenatal diagnosis is not associated with lower mortality. TAPVC, single ventricle or other non-biventricular surgery, and ≥mild AVVR at presentation are independently associated with poor outcomes.
Article Information
vol. 134 no. Suppl 1 A17363
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Puja Banka;
- Barbara Schaetzle;
- Adi Adar;
- Lynn Sleeper;
- Tal Geva
- Cardiology, Boston Children’s Hosp, Boston, MA
Abstract 16939: Tube-assisted Feeding is Associated With Worse Longitudinal Growth in Children With Single Ventricle Cardiac Disease
Arene Butto, Laura Mercer-Rosa, Carrie Daymont, Jonathan Edelson, Erika Mejia, Meryl S Cohen
Circulation. 2016;134:A16939
Abstract
Introduction: Children with single ventricle cardiac disease (SVCD) have poor growth in early life. Tube-assisted feeding (TF) has increasingly been used to improve weight gain in SVCD patients, but little is known about its long-term effects on growth. We sought to compare the longitudinal growth of SVCD patients receiving TF at the time of hospital discharge after initial cardiac surgery with those fed entirely by mouth.
Methods: We conducted a retrospective cohort study of patients who underwent initial surgical palliation for SVCD from 1999 to 2009, excluding premature infants (<37 weeks) and patients with non-cardiac chronic conditions, including known genetic syndromes. TF was defined as nasogastric, gastrostomy, or jejunostomy tube feeds for primary or supplementary nutrition. We used non-parametric analysis to compare median weight, height, and BMI for age z-scores at each year of life between those receiving TF and those fed exclusively by mouth upon hospital discharge. A secondary analysis examined the effect of anatomy on growth between those with hypoplastic left heart syndrome (HLHS) compared to other SVCD. Mixed effects linear regression was used to assess rate of growth in the two groups.
Results: A total of 135 patients met inclusion criteria; 64% were male and 50% had HLHS. There were 44 patients (33%) in the TF group. Median weight z-score was significantly lower in the TF group at each year of life from ages 2 to 6 years (p<0.05) compared to those fed by mouth (Figure 1A). Similar findings were seen for height and BMI z-scores (Figures 1B and 1C). Growth z-scores were not associated with anatomic subtype. There was no significant difference in the rate of change in growth parameter z-scores between the two groups.
Conclusions: Long-term growth of children with SVCD who require TF at hospital discharge is diminished compared to that of peers who are fed entirely by mouth. TF patients with SVCD do not experience catch-up growth during early childhood.
Article Information
vol. 134 no. Suppl 1 A16939
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Div of Cardiology, Children’s Hosp of Philadelphia, Philadelphia, PA
- 2Dept of Pediatrics and Child Health, Univ of Manitoba, Winnipeg, Canada
- 3Dept of Pediatrics, Children’s Hosp of Philadelphia, Philadelphia, PA
Abstract 16964: National Experience of Ebstein Anomaly Births: Demographics, Treatment, and Mortality
Kimberly Holst, Kristine Hanson, Elizabeth Habermann, Patrick O’Leary, Joseph Dearani
Circulation. 2016;134:A16964
Abstract
Introduction: Neonatal Ebstein anomaly (EA) is a rare and variable congenital heart lesion with a paucity of large series data. The objectives were to describe the characteristics, concomitant diagnoses, and mortality of neonatal EA in a national cohort.
Methods: Kids’ Inpatient Database (KID) and National Inpatient Sample (NIS) were used to analyze birth hospitalizations of neonates with EA from 1998 to 2013. Univariate logistic regression identified variables associated with mortality.
Results: 1088 neonates diagnosed with EA were identified through NIS and KID; estimated incidence was 4.8 per 100,000 in-hospital live births. Associated lesions, other than atrial septal defect, included patent ductus arteriosus in 320 (29%), pulmonary atresia/stenosis in 170 (16%), ventricular septal defect in 96 (9%), transposition of great arteries in 31 (3%) and coarctation/aortic stenosis in 25 (2%). Approximately one third (322/1088) of patients were transferred to another hospital; mortality was analyzed in the remaining 766 patients. Overall mortality was 13% (103/766). Treatments were medical only in 88% (674/766), cardiac surgery alone in 7% (50/766), catheter based only in 2% (19/766), and hybrid catheterization and surgical in 3% (23/766). Mortality without interventions was 12% (78/674) and was 11% (2/19) with catheter based treatment only. Neonates with cardiac surgery had increased mortality: 28% (14/50, OR 2.97 vs no intervention, 95% CI 1.54-5.76, p=0.001) after cardiac surgery alone and 39% (9/23, OR 4.91, 95% CI 2.06-11.73, p<0.001) after hybrid. Cardiac lesions associated with increased mortality included pulmonary atresia/stenosis (OR 4.68, 95% CI 2.92-7.49, p<0.001) and coarctation/aortic stenosis (OR 3.33, 95% CI 1.12-9.95, p=0.03).
Conclusions: This large series of neonatal EA provides new insight to this rare disease. The majority of patients did not undergo surgery or catheterization during the birth hospitalization. Mortality risk was increased by concomitant right or left sided outflow obstructions and in those requiring surgical and/or catheter based procedures prior to neonatal discharge. To further investigate this rare lesion, multi-institutional collaboration is required to assess the clinical intricacies of EA.
Article Information
vol. 134 no. Suppl 1 A16964
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Surgery, Mayo Clinic, Rochester, MN
- 2Robert D. and Patricia E. Kern Cntr for the Science of Health Care Delivery, Mayo Clinic, Rochester, MN
- 3Pediatrics, Mayo Clinic, Rochester, MN
- 4Cardiovascular Surgery, Mayo Clinic, Rochester, MN
Abstract 16994: Investigating Predictors of Rapid Aortic Root Dilation and Referral for Aortic Surgery in Marfan Syndrome
Arvind Hoskoppal, Shaji Menon, Felicia Trachtenberg, Jami C Levine, Elif Seda Selamet Tierney, Kristin M Burns, Julie De Backer, Bruce D Gelb, Marie Gleason, Jeanne James, Wyman W Lai, Aimee Liou, Lynn Mahony, Aaron K Olson, Reed E Pyeritz, Angela M Sharkey, Mario Stylianou, Stephanie B Wechsler, Luciana Young, Ronald V Lacro, Timothy J Bradley
Circulation. 2016;134:A16994
Abstract
Background: Few data exist regarding predictors of rapid aortic root dilation and referral for aortic surgery in Marfan syndrome (MFS).
Objectives: To identify independent predictors of the rate of aortic root (AoR) dilation and referral for aortic surgery, we investigated the data from the Pediatric Heart Network randomized trial of atenolol vs. losartan in young MFS.
Methods: The study enrolled 608 subjects (6 mo – 25 yr) who met original Ghent criteria and had a body-surface area adjusted maximum aortic root diameter z score (AoRz) > 3. Data from core lab echocardiograms at 0, 12, 24 & 36 months were included in this analysis. Repeated measures linear and logistic regression was used to determine multivariable predictors of AoR dilation. ROC curves were used to determine cut-points in AoR dilation predicting referral for aortic surgery.
Results: Of 24 subjects who underwent aortic surgery, median preoperative change in AoRz/yr was 0.36 vs. -0.10 in 555 subjects without surgery and in aortic root diameter (AoRd)/yr was 0.22 cm vs. 0.08 cm. Some statistically significant clinical and echocardiographic predictors of rate of AoR dilation were found, but appeared to explain little of the overall variation in AoRz and AoRd (see Table). Generalized dilatation of the aortic root, sinotubular junction and ascending aortic dimensions predicted referral for aortic surgery (see Table). A yearly change in AoRz/yr of 0.72 (sensitivity 42%, specificity 92%) and in AoRd/yr of 0.34 cm (sensitivity 38%, specificity 95%) predicted referral for aortic surgery.
Conclusions: In this cohort of young MFS, no robust predictors of more rapid AoR dilation were identified; however, age, gender, race and increased sinotubular junction appear contributory. Generalized proximal aortic dilatation predicted timing of referral for aortic surgery. Rate of AoR dilation cut-points had high specificity, but low sensitivity for predicting referral for aortic surgery, limiting their clinical use.
Article Information
vol. 134 no. Suppl 1 A16994
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Arvind Hoskoppal1;
- Shaji Menon1;
- Felicia Trachtenberg2;
- Jami C Levine3;
- Elif Seda Selamet Tierney3;
- Kristin M Burns4;
- Julie De Backer5;
- Bruce D Gelb6;
- Marie Gleason7;
- Jeanne James8;
- Wyman W Lai9;
- Aimee Liou10;
- Lynn Mahony11;
- Aaron K Olson12;
- Reed E Pyeritz13;
- Angela M Sharkey14;
- Mario Stylianou4;
- Stephanie B Wechsler15;
- Luciana Young16;
- Ronald V Lacro3;
- Timothy J Bradley17,
- Pediatric Heart Network Investigators
- 1Pediatric Cardiology, Univ of Utah, Salt Lake City, UT
- 2Cardiology, New England Rsch Institutes, Watertown, MA
- 3Pediatric Cardiology, Harvard Med Sch, Boston, MA
- 4Pediatric Cardiology, National Heart, Lung, and Blood Institute, Bethesda, MD
- 5Pediatric Cardiology, Ghent Universtiy, Ghent, Belgium
- 6Pediatric Cardiology, Icahn Sch of Medicine at Mount Sinai, New York, NY
- 7Pediatric Cardiology, Children’s Hosp of Philadelphia, Philadelphia, PA
- 8Pediatric Cardiology, Univ of Cincinnati, Cincinnati, OH
- 9Pediatric Cardiology, Columbia Univ, New York, NY
- 10Pediatric Cardiology, Baylor College of Medicine, Houston, TX
- 11Pediatric Cardiology, Univ of Texas, Houston, Texas, TX
- 12Pediatric Cardiology, Univ of Washington, Seattle, WA
- 13Pediatric Cardiology, Univ of Pennsylvania, Philadelphia, PA
- 14Pediatric Cardiology, Washington Univ, St Louis, MO
- 15Pediatric Cardiology, Duke Univ, Durham, NC
- 16Pediatric Cardiology, Ann and Robert H. Lurie Children’s Hosp of Chicago, Chicago, IL
- 17Pediatric Cardiology, Univ of Toronto, Toronto, Canada
Abstract 14450: Standardized Clinical Assessment and Management Plan (SCAMP) on Growth in Infants With Congenital Heart Disease
Russell Gongwer, Kimberlee Gauvreau, Susanna Huh, Kevin Sztam, Kathy Jenkins
Circulation. 2016;134:A14450
Abstract
Introduction: Growth failure is prevalent among infants with congenital heart disease (CHD). A Standardized Clinical Assessment and Management Plan (SCAMP) was introduced at Boston Children’s Hospital cardiac medical ward to identify patients with growth failure, evaluate relevant contributing conditions, and recommend a management plan including collaboration with nutrition physicians. Our aim was to determine whether SCAMP-enrolled patients had improved growth compared to historical controls.
Methods: SCAMP patients were enrolled July 2013 – June 2014. Historical controls were selected from patients admitted to the same ward June 2010 – June 2011 who would have met eligibility criteria for SCAMP enrollment. Eligible patients: <1 year, diagnosed with CHD, and had growth failure defined by a WHO weight-for-age z-score (WAZ) < -2 or failure to sustain adequate weight gain. Exclusion criteria: contraindication to enteral feeding, diagnosis to explain growth failure, genetic syndrome, awaiting heart transplant, planned intervention within 7 days, age < 14 days. SCAMP-enrolled patients received a nutrition consult and feeding team evaluation, and ORL consult for patients with relevant conditions or symptoms. Nutrition physicians collaborated regularly with cardiologists to guide management of SCAMP patients during hospitalization. Outcome: Change in WAZ from enrollment to most recent weight measurement among patients with at least 6 months of follow-up.
Results: 29 SCAMP patients (62% male, 49% univentricular, 31% unrepaired) and 42 controls (60% male, 26% univentricular, 38% unrepaired); control patients were older at baseline admission weight (146 vs. 117 days, p=0.18), had a higher WAZ (-2.87 ± 0.74 vs. -3.69 ± 1.70, p=0.02), and had longer follow-up time (1312 vs. 579 days, p<0.01). SCAMP patients were more likely to have had catheterizations (p=0.04) before enrollment, and had greater WAZ gain (2.70 ± 1.84 vs. 1.83 ± 1.20, p=0.03) at most recent follow up.
Conclusions: Patients enrolled in a nutrition-focused SCAMP had a greater improvement in WAZ than historical controls. Identification of growth failure and collaboration with nutrition physician experts appeared to improve weight gain among CHD patients experiencing growth failure.
Article Information
vol. 134 no. Suppl 1 A14450
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Cardiology, Boston Children’s Hosp, Boston, MA
- 2Gastroenterology/Nutrition, Boston Children’s Hosp, Boston, MA
Abstract 14641: Sleep Disturbance is Associated With Lower Quality of Life and Greater Depressive Symptoms in Adults With Congenital Heart Defects
Nancy McCabe, Wendy Book, Carolyn Reilly, Sandra Dunbar
Circulation. 2016;134:A14641
Abstract
Introduction: Poor sleep quality is common in cardiac populations and known to increase adverse physical and psychological outcomes, but little is known about sleep quality or its association with outcomes in adults with congenital heart defects (ACHD).
Hypothesis: Greater sleep disturbance will be associated with greater depressive symptoms and lower quality of life (QOL) in persons with ACHD.
Methods: A secondary analysis of an observational, self-care study in patients with moderate or severe ACHD (n=125) was conducted. Patients were recruited from a single ACHD center and demographic (age, gender, race, education, employment status, marital status) and clinical data (defect severity, NYHA Class, BMI, Obstructive Sleep Apnea (OSA)), depressive symptoms (PHQ-9), sleep disturbance (PROMIS-Sleep) and overall QOL (VAS scale) were collected by chart review and self-report. Analyses included bivariate correlations and logistic and linear regression.
Results: Patients were mean age 35 years (range 20-68), 56% female, 82% Caucasian, 53% severe ACHD, 26% NYHA Class III/IV, 3% OSA. Sixty-eight (54%) patients reported sleep disturbance (PROMIS t score >50), including low sleep quality, difficulties falling asleep, general sleep problems, and poor sleep refreshment. Persons with sleep disturbance were more likely to be functional NYHA Class III/IV vs I/II (p<.001), have ≤ high school education (p=.02), and be unemployed (p=.02). In univariate analysis, persons with NYHA Class III/IV and lower education were 6.4 and 2.4 times more likely to have sleep disturbance, respectively (OR 6.4, [95% CI 2.2, 18.3]; OR 2.4, [95% CI 1.1, 5.4]). Greater sleep disturbance was related to increased depressive symptoms (β=.65, p<.001) and lower QOL (β=-2.23, p<.001). After adjusting for sociodemographic and clinical variables, sleep disturbance remained independently associated with depressive symptoms (β=.55, p<.001), and QOL (β=-2.25, p=.01).
Conclusions: Sleep disturbance was independently associated with greater depressive symptoms and lower QOL in persons with ACHD. Improving sleep quality may represent an important target for improving psychological and QOL outcomes in ACHD.
Article Information
vol. 134 no. Suppl 1 A14641
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Nursing, Emory Univ, Atlanta, GA
- 2Cardiology, Emory Univ, Atlanta, GA
Abstract 20144: Increasing Preload Permits Maintenance of Cardiac Output During Rapid Atrial Pacing in Infant Piglets but is Associated With Possible Right Heart Diastolic Impairment in Neonatal Piglets
Etienne Fortin-Pellerin, Lisa K Hornberger, James Y Coe, Lindsay Mills, Jesus Serrano-Lomelin, Po-Yin Cheung, Nee S Khoo
Circulation. 2016;134:A20144
Abstract
Introduction: Rapid LV maturation in the neonatal period influences response to hemodynamic challenges. We recently demonstrated in a piglet model, that the neonatal heart tolerates atrial tachycardia (AT) while the infant heart fails to maintain left ventricular output (LVO). We hypothesized that augmented preload would improve LVO during AT in both the young infant (YP) and neonatal (NP) piglet.
Methods: Under anesthesia, 7 NP (1-3 days) and 7 YP (14-15 days) had a Millar high-fidelity catheter placed in the LV and pacing wire placed in the right atrium. CVP was monitored. Piglets had 60ml/kg of normal saline infused over 20 minutes. After stabilization, heart rate was increased by 10bpm increments to 300bpm. LVO was measured by echocardiography (Doppler technique). Response to preload and AT was compared from baseline for each piglet by repeated measure ANOVA, paired t-tests or Wilcoxon signed-rank test. We also compared NP and YP response to AT with normovolemic piglets from our initial study.
Results: For both NP and YP, baseline LVO increased with volume load in the hypervolemia groups (NP 271 ± 11 to 334 ± 23, p=0.007; YP 231 ± 17 to 263 ± 21 ml/kg/min, p=0.025). Even with augmented preload, YP and NP demonstrated an appropriate decrease in LVEDP and CVP with pacing. Volume loaded YP maintained LVO during AT better than euvolemic YPs (p = 0.002). Although volume-loaded NPs also maintained their LVO similarly to euvolemic NP, 4 of 7 had significant desaturation at 300bpm (baseline 99.7% vs. 300bpm 87.9%, p = 0.04), associated with a right to left shunt at the patent foramen ovale. Immediate recovery of desaturation was observed on cessation of pacing in these latter NPs.
Conclusions: Increasing intravascular volume in YPs improved tolerance to AT. Although NPs also maintained LVO, the finding of desaturation and right to left atrial shunting suggested RV intolerance to volume load during AT. These findings may be relevant to the management of neonates and young infants with AT.
Article Information
vol. 134 no. Suppl 1 A20144
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Etienne Fortin-Pellerin1;
- Lisa K Hornberger2;
- James Y Coe2;
- Lindsay Mills2;
- Jesus Serrano-Lomelin3;
- Po-Yin Cheung4;
- Nee S Khoo2
- 1Neonatology, Sherbrooke Univ Hosp, Sherbrooke, Canada
- 2Pediatric Cardiology, Stollery Children’s Hosp, Edmonton, Canada
- 3Sch of Public Health, Univ of Alberta, Edmonton, Canada
- 4Neonatology, Stollery Children’s Hosp, Edmonton, Canada
Abstract 18924: Porcine Model of Aortic Coarctation: Treatment With Novel Biodegradable Stent Up to 12mm Diameter
Surendranath R Veeram Reddy, Tre R Welch, Jian Wang, Matthew Riegel, James Richardson, Joseph M Forbess, Alan W Nugent
Circulation. 2016;134:A18924
Abstract
Introduction: A novel double opposing helical (DH) biodegradable stent (BDS) made of poly-l-lactic-acid can be fabricated to larger diameters needed for use in congenital heart disease. Study aims were: 1. Create a model of coarctation of aorta (CoA) in minipigs. 2. Evaluate feasibility of stent implantation (DH BDS and metal) and assess mid-term results and inflammatory profile.
Hypothesis: DH BDS will maintain structural integrity to treat porcine CoA.
Methods: Via left lateral thoracotomy, CoA was created in 7 Yucatan minipigs (7-9 kg) by resecting a portion of the aortic wall. Stents were implanted 6-8 weeks later. Assessment included: angiography, intravascular ultrasound and histopathology.
Results: All 7 animals survived the CoA creation surgery and underwent successful stent implantation (4 DH BDS and 3 metal) via carotid (5) and femoral (2) access. 1 planned non-survival animal underwent a 10-mm metal stent implantation that successfully relieved the CoA. The remaining 6 minipigs underwent successful DH BDS (4) or metal stent (2) implantations with CoA relief. 2/6 died within 24 hours due to anesthesia and vascular access complications. The 4 survivors recovered well. At 6 months follow up, 1 animal post 12 mm DH BDS implantation, showed good apposition with vessel luminal patency and mild-moderate inflammatory response. The other 3 survivors with 10mm diameter stents (2 DH BDS and 1 metal) are well with planned evaluation at 12 months.
Conclusion: A resection CoA model was successfully performed. Feasibility to treat the CoA with a DH BDS at diameters 10-12mm is established. Long term follow-up and miniaturization to decrease the DH BDS crossing profile is needed.
Article Information
vol. 134 no. Suppl 1 A18924
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Surendranath R Veeram Reddy1;
- Tre R Welch2;
- Jian Wang2;
- Matthew Riegel3;
- James Richardson4;
- Joseph M Forbess2;
- Alan W Nugent1
- 1Pediatrics, UT Southwestern Med Cntr, Dallas, TX
- 2Cardiovascular Thoracic Surgery, UT Southwestern Med Cntr, Dallas, TX
- 3Animal Resource Cntr, UT Southwestern Med Cntr, Dallas, TX
- 4Pathology and Molecular Biology, UT Southwestern Med Cntr, Dallas, TX
Abstract 17138: Emergence of a Unique Biomarker Signature in Pediatric Patients With Developing Chemotherapy Cardiotoxicity
Olga H Toro-Salazar, Eileen Gillan, Michael O’Loughlin, Joanna Ferranti, Kia N Zellars, Paige E Perreault, Kathryn Mason, Bruce Liang, Shailendra Upadyay, Wojciech Mazur, Subba Raman, Kan Hor, Francis G Spinale
Circulation. 2016;134:A17138
Abstract
Background: A class of chemotherapeutics commonly used in pediatric cancer is the anthrycylines (ACs), but often is associated with left ventricular dysfunction: i.e. chemotherapy induced cardiotoxicity (CIC). The goal of this project was to examine whether a specific set of plasma biomarkers could be identified in pediatric patients undergoing initial AC treatment and at risk for CIC as well as examined in relationship to referent normal pediatric patients.
Methods and Results: AC treated pediatric patients (n=17, diagnosed with cancer (most commonly Hodgkin’s Lymphoma) with set dosing intervals and maximal AC doses of 325 mg/m2)) underwent cardiac MRI 24-48 hours after AC therapy for LV ejection fraction (LVEF) and plasma obtained at baseline (initial AC treatment) and with repeat studies (up to 12 mos). Plasma was also collected from referent normal pediatric subjects (n=66). Multiplex arrays quantified signatures from the inflammatory (8 unique cytokines) and matrix remodeling (13 unique matrix metalloproteinases (MMPs) and tissue inhibitors of MMPs (TIMPs)) domains. LVEF fell from baseline with continued AC treatment (63±2 vs 57±1%, p<0.05), consistent with CIC onset. A differential inflammatory/matrix signature emerged in AC patients compared to normal (Table), including increased interleukin-8 and MMP levels. With longer periods of AC dosing, MMP-7, a marker of macrophage proteolytic activation, increased by 165±54% whereas interleukin-10, an anti-inflammatory marker, fell by 75±13% (both p<0.05).
Summary: The unique findings from this study were 2-fold. First, a differential biomarker signature containing both inflammatory and matrix domains occurs early in AC treatment. Secondly, dynamic changes in these domains occur as a function of time and progression to CIC. These findings provide potential prognostic and mechanistic insight into the natural history of pediatric chemotherapy cardiotoxicity.
Article Information
vol. 134 no. Suppl 1 A17138
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Olga H Toro-Salazar1;
- Eileen Gillan2;
- Michael O’Loughlin3;
- Joanna Ferranti1;
- Kia N Zellars4;
- Paige E Perreault4;
- Kathryn Mason4;
- Bruce Liang5;
- Shailendra Upadyay6;
- Wojciech Mazur7;
- Subba Raman8;
- Kan Hor9;
- Francis G Spinale4
- 1Pediatric Cardiology, Connecticut Children’s Med Cntr, Hartford, CT
- 2Pediatric Oncology, Connecticut Children’s Med Cntr, Hartford, CT
- 3Radiology, Hartford Hosp, Hartford, CT
- 4Cardiovascular Translational Rsch Cntr, Univ of South Carolina Sch of Medicine, Columbia, SC
- 5Pat and Jim Calhoun Cardiology Cntr, Univ of Connecticut Health Cntr, Farmington, CT
- 6Pediatric Cardiology, Connecticut Children’s Med Ctr, Hartford, CT
- 7The Christ Hosp, Ohio Heart and Vascular Cntr, Cincinnati, OH
- 8Cardiology, Ohio State Univ Med Cntr, Columbus, OH
- 9Cardiology, Nationwide Children’s Hosp, Columbus, OH
Abstract 14425: Exome Sequencing Reveals a Low Frequency Variant in BMPER in a Pedigree With Recurrence of Left Ventricular Outflow Tract Obstruction Defects
Emmi Helle, Tiina Ojala, Markus Perola, Euan Ashley, James R Priest
Circulation. 2016;134:A14425
Abstract
Introduction: Bicuspid aortic valve (BAV) is the most common congenital heart defect affecting 1-2% of the population and is etiologically related to more severe left ventricular outflow tract (LVOTO) defects such as congenital AS, COA or HLHS. Family and population studies suggest that LVOTO defects are associated with significant heritability, yet only few genes have been associated with LVOTO in humans and explain only a minority of cases.
Methods: In a Finnish population of 120 patients with LVOTO and their family members (total n=248) we sought to discover novel genes and variants associated with disease using exome sequencing. Exome sequencing was performed at Personalis Inc. and UW-CMG. Variant calling was performed with the Realtime Genomic Package (RTG version 3.4) in reference to the UCSC reference sequence (hg19).
Results: In a family with two affected members, a biologically plausible heterozygous missense snp (rs144030074) was identified in BMPER, a BMP-pathway inhibitor. The proband has BAV and COA, and his maternal grandmother has BAV and AS. The mother and three siblings of the proband have the same variant with a normal phenotype, The variant has a MAF of 0.0007 in the ethnically matched Finnish Sequencing Initiative Suomi population (N= 10,474). Among the other sequenced patients with LVOTO (N=49) the identical variant was found in one unrelated individual with HLHS (p=0.03, Exact Binomial test).
BMPER is present in the developing mouse aortic valve at E9.5-E11.5. BMP proteins are essential for early heart development and variants in genes interacting with this pathway (ACVR1, NOTCH1, SMAD6) are associated with LVOTO defects in mammals. The variant N74D is located in the first cysteine rich repeat of the protein, a site that binds to BMP proteins. An in vitro transfection experiment in HUVEC cells comparing wild type and the mutant suggests altered activation of 6 of 56 tested BMP signaling targets (BMP4, COL1A2, FST, ID1, SMAD7, TGFB2, cutoff p=0.001, phyper test p=8.80e-06) when cells are exposed to flow conditions.
Conclusion: We have identified a low frequency BMPER-variant likely causal with LVOTO defects. Confirmation of the findings with an allele specific BMPER N74D knockin mouse-model and confirmation in large sequenced cohorts is ongoing.
Article Information
vol. 134 no. Suppl 1 A14425
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Cardiovascular Institute, Stanford Univ Sch of Medicine, Stanford, CA
- 2Pediatric Cardiology, Children’s Hosp, Univ of Helsinki, Helsinki, Finland
- 3Diabetes and Obesity Rsch Program, National Institute for Health and Welfare, Helsinki, Finland
- 4Cardiovascular Medicine, Stanford Univ Sch of Medicine, Stanford, CA
- 5Cardiovascular Institute, Pediatric Cardiology, Stanford Univ Sch of Medicine, Stanford, CA
Abstract 14119: Fibulin-1 Plays a Role in Smooth Muscle Cell Migration and Intimal Thickening in the Ductus Arteriosus
Satoko Ito, Utako Yokoyama, Chiharu Yanai, Munetaka Masuda, Toshihide Asou, Yoshihiro Ishikawa
Circulation. 2016;134:A14119
Abstract
Introduction: Closure of the ductus arteriosus (DA) consists of two processes, i.e., vasoconstriction and intimal thickening (IT). Premature infants with patent DA (PDA), in which IT is not sufficiently formed, are often resistant to the current vasoconstriction therapies. Our previous study showed that prostaglandin E2 (PGE2)-EP4 signaling plays a critical role in IT formation via inhibition of elastic lamina formation and smooth muscle cell (SMC) migration. However, the molecular mechanisms of IT formation are not fully understood. We aimed to identify a novel molecular mechanism inducing EP4-mediated IT in the DA.
Methods: Primary culture of smooth muscle cells of the DA (DASMCs) was isolated from rat fetuses at the 21th day of gestation. SMCs were stimulated with EP4 agonist for 24 h, and extracted RNAs were subjected to microarray analysis. Expression of mRNA and protein were evaluated by quantitative RT-PCR and western blotting, respectively. Human and rat DA and aorta tissue sections were stained against anti-fibulin-1, anti-ADAMTS-1, and anti-versican fragment. Cell migration was examined by a scratch assay in DASMCs treated with fibulin-1-targeted or control siRNA in the presence or absence of EP4 agonist.
Results: Microarray analysis of DASMCs revealed that fubulin-1 was the most positively regulated gene by EP4 stimulation (28-fold, n = 4, p < 0.0005). Robust increase in fibulin-1 mRNA and protein (273-and over 20-fold, n=4, p<0.001, respectively) was confirmed, which was attenuated by protein kinase A or phospholipase C inhibitors. It has been reported that fibulin-1 binds a protease ADAMTS-1 to cleave versican, resulting in fragmented versican-mediated cell migration. In rat and human DA tissues, fibulin-1 was highly expressed in the area of IT in the DA where ADAMTS-1 and fragmented versican were also abundantly expressed. Furthermore, stimulation of EP4 induced DASMC migration (n = 6, p < 0.001), which was attenuated in DASMCs treated with fibulin-1-targeted siRNA.
Conclusions: PGE2-EP4-induced fibulin-1 was suggested to play a primary role in IT in the DA via versican fragment-mediated SMC migration. Stimulation of selective signaling pathway for fibulin-1 induction may be a new therapeutic strategy for PDA.
Article Information
vol. 134 no. Suppl 1 A14119
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Satoko Ito1;
- Utako Yokoyama1;
- Chiharu Yanai1;
- Munetaka Masuda2;
- Toshihide Asou3;
- Yoshihiro Ishikawa1
- 1Cardiovascular Rsch Institute, Yokohama City Univ, Yokohama, Japan
- 2Depertment of Cardiovascular Surgery, Yokohama City Univ, Yokohama, Japan
- 3Dept of Cardiovascular Surgery, Kanagawa Children’s Med Cntr, Yokohama, Japan
Abstract 13847: Impact of the Unzipping Technique on Pulmonary Artery Structure and Growth
Luke Lamers, Cole Nygard, Rachel Luehrs, Alejandro Roldan, Melissa Bates
Circulation. 2016;134:A13847
Abstract
Introduction: With the unzipping technique, small diameter stents are implanted to relieve pulmonary artery (PA) stenosis, subsequently dilated, fractured and re-stented with large stents dilatable to adult PA diameters. The unzipping technique is utilized in clinical practice with undefined long term results. This study assessed the impact of unzipping on PA structure and growth.
Methods: Twelve piglets with left PA (LPA) stenosis underwent the unzipping sequence at 6, 10 and 18 weeks of age and were compared to normal controls and controls with untreated LPA stenosis. 2D and 3D rotational angiography pre/post interventions and PA histology was performed on all animals.
Results: Eleven of twelve animals completed the three catheterizations. One stent (4 mm implant diameter) could not be crossed at the second procedure. Following the interventions, the diameter of the unzipped LPA was similar to the proximal LPA of normal controls (14 mm ± 1.2 vs 14.7 mm ± 1, p = 0.19). The diameter of the distal LPA was larger in normal controls, compared to interventions and controls with untreated LPA stenosis (14.6 mm ± 0.9 vs 11.6 mm ± 1.9, vs 10 mm ± 1.2, p < .01). Diameters of six 1st order LPA branches were similar between normal controls and interventions, and larger than the branch diameters in the stenosis controls. Right PA (RPA) dimensions were larger in controls with untreated stenosis, compared to normal controls and interventions (17.8 mm ± 1.2 vs 16.2 mm ± .9 vs 16 ± 1.7 mm p<0.05). RPA 1st order branching diameters were similar for normal controls and interventions. RPA 1st order branch diameters in stenosis controls were larger for 3 of 6 branches compared to normal controls and 1 of 6 compared to interventions. Histologically, the distal LPA displayed uniform fibrointimal proliferation and smooth muscle hypertrophy in pigs with both interventions and untreated stenosis. Focal RPA fibrointimal proliferation was noted in stenosis and intervention animals.
Conclusion: PA growth distal to the unzipped segment is partially compromised, yet 1storder branch diameters are normal and significantly larger, compared to untreated stenosis. Histological vascular abnormalities are noted bilaterally in stenosis animals which do not normalize following the unzipping technique.
Article Information
vol. 134 no. Suppl 1 A13847
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Pediatrics, Univ of Wisconsin, Madison, WI
- 2Physiology, Univ of Iowa, Iowa City, IA
- 3Radiology, Univ of Wisconsin, Madison, WI
Abstract 13032: Evidence of Dimensional Adaptability of in vivo Tissue-engineered Allogenic “Biotube” Vascular Grafts in a Growing Canine Model
Maya Furukoshi, Yasuhide Nakayama
Circulation. 2016;134:A13032
Abstract
Introduction: In pediatric surgery, size mismatch inducing between artificial vascular grafts and growing recipients vessels remains a serious problem to be solved. Biotubes are autologous connective tissue tubes, formed by in body tissue architecture technology (IBTA), which is a novel and practical approach of regenerative medicine based on the tissue encapsulation phenomenon. This study aimed to evaluate the growth potential of Biotubes by examining their caliber and length adaptation to growing native arteries after implantation. Allogenic implantation of Biotubes pre-prepared from adult beagles was performed to juvenile beagles.
Methods and Results: IBTA-based Biotubes (internal diameter 3 mm, length 1 cm) were prepared in adult beagles (age, 1 year; weight ca. 10 kg) by subcutaneous embedding of silicone-based molds for 2 months. The obtained allogenic collagenous Biotubes (n=8) were implanted into the common carotid artery (internal diameter, 2 mm) of juvenile beagles (n=8, age 11 weeks, weight ca. 3 kg). In all cases, there was no aneurysm or stenosis formation with perfect patency for all observation periods. Almost complete vascular remodeling occurred only at 1 month of implantation. Follow-up angiogram showed that diameter of Biotubes was gradually expanded with that of the growing host arteries almost in the same way. In 1-year after implantation, there was little gap between them by ca.1.5-times of diameter expansion in Biotube. Interestingly, macroscopic observation showed elongation of Biotubes to ca 1.3 times in maximum.
Conclusions: Even in allogenic manner, vascular reconstruction of Biotube to layered vascular tissue successfully occurred. After vascular reconstruction, Biotubes could be extended and expanded according to the growing native arteries. The growth potential of Biotubes was indicated in this animal experimental model for the first time. Biotubes have high potential usefulness in pediatric surgery.
Article Information
vol. 134 no. Suppl 1 A13032
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Maya Furukoshi;
- Yasuhide Nakayama
- Div of medical engineering and materials, National Cerebral and Cardiovascular Cntr, Osaka, Japan
Abstract 11615: Influence of Age and Gender on Marfan Phenotype: The NHLBI GenTAC Registry
Mary J Roman, Richard B Devereux, Liliana Preiss, Federico M Asch, Joseph E Bavaria, Kim A Eagle, Kathryn Holmes, Cheryl Maslen, Dianna M Milewicz, Shaine A Morris, Siddharth Prakash, Reed Pyeritz, William J Ravekes, Ralph V Shohet, Howard Song, Jonathan W Weinsaft
Circulation. 2016;134:A11615
Abstract
Background: The influence of gender and age on phenotypic features of individuals with Marfan syndrome has not been systematically examined in a large cohort of both children and adults.
Methods: We evaluated 789 Marfan patients enrolled in the NHLBI GenTAC Registry (53% male; mean age 31 [range: 1-86 years]). Females aged≥15 and males aged≥16 years were considered adults based on average age of skeletal maturity.
Results: Children (n=183) and adults (n=606) (see Table) were comparable in revised Ghent systemic score, ectopia lentis, and most phenotypic features, including prevalences of aortic root dilatation and mitral prolapse. However, adults were more likely to have spontaneous pneumothorax, scoliosis, dural ectasia and striae. Prophylactic aortic root replacement and mitral valve surgery were rare during childhood vs. adulthood (2 vs. 35% and 1 vs. 9%, respectively, both p<0.0001). There was only one childhood aortic dissection (type B in 15 year old male). Overall females were more likely than males to have arachnodactyly (54 vs. 40%), scoliosis (60 vs. 49%), and dural ectasia (16 vs. 10%), all p<0.01. Adult males were more likely to have aortic root dilatation (92 vs. 84%), aortic regurgitation (55 vs. 36%) and to have undergone prophylactic aortic root replacement (47 vs. 24%), all p<0.001. Prevalence of prior aortic dissection was higher in males than females (25 vs. 18%, p=0.06), 44% of which were type B. Mean age at dissection (35 vs. 38 years), age at prophylactic surgery (32 vs. 35 years), and need for mitral valve surgery (9.5 vs. 10.0%) were similar between men and women, respectively.
Conclusions: Pulmonary, skeletal and aortic complications, but not other phenotypic features, increase with aging in Marfan syndrome. Aortic aneurysms and prophylactic aortic surgery are more common in men. In the era of current surgical and medical treatment, aortic dissection, commonly type B, occurs in an appreciable proportion of Marfan patients, especially among men.
Article Information
vol. 134 no. Suppl 1 A11615
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Mary J Roman1;
- Richard B Devereux1;
- Liliana Preiss2;
- Federico M Asch3;
- Joseph E Bavaria4;
- Kim A Eagle5;
- Kathryn Holmes6;
- Cheryl Maslen7;
- Dianna M Milewicz8;
- Shaine A Morris9;
- Siddharth Prakash8;
- Reed Pyeritz10;
- William J Ravekes11;
- Ralph V Shohet12;
- Howard Song13;
- Jonathan W Weinsaft1
- 1Medicine, Weill Cornell Med College, New York, NY
- 2Biostatistics and Epidemiology Div, RTI International, Rockville, MD
- 3Medicine, Medstar Health Rsch Institute, Washington, DC
- 4Cardiothoracic Surgery, Perelman Sch of Medicine at the Univ of Pennsylvania, Philadelphia, PA
- 5Medicine, Univ of Michigan Health System, Ann Arbor, MI
- 6Pediatric Cardiology, Oregon Health & Science Univ, Portland, OR
- 7Knight Cardiovascular Institute, Oregon Health & Science Univ, Portland, OR
- 8Medicine, McGovern Med Sch, Houston, TX
- 9Pediatric Cardiology, Texas Children’s Hosp/Baylor College of Medicine, Houston, TX
- 10Medicine, Perelman Sch of Medicine at the Univ of Pennsylvania, Philadelphia, PA
- 11Medicine, Johns Hopkins Univ Sch of Medicine, Baltimore, MD
- 12Medicine, John A. Burns Sch of Medicine, Honolulu, HI
- 13Cardiothoracic Surgery, Oregon Health & Science Univ, Portland, OR
Abstract 11365: Bioelectrical Impedance Analysis is Useful for the Management of Heart Failure and Prediction of Cardiac Events in Adult Patients With Congenital Heart Disease
Masaki Sato, Kei Inai, Mikiko Shimizu, Daiji Takeuchi, Testuko Ishii, Keiko Toyohara, Tokuko Shinohara, Hisashi Sugiyama, Hirofumi Tomimatsu, Toshio Nakanishi, In-Sam Park
Circulation. 2016;134:A11365
Abstract
Introduction: Since decompensated heart failure generally leads to fluid volume overload, the ability to recognize and quantify fluid retention is critical for the treatment of heart failure. Bioelectrical impedance analysis (BIA) is a safe, non-invasive, and rapid assessment method, but little has been reported on the role of BIA in the management of patients with congenital heart disease (CHD).
Hypothesis: We assessed the hypothesis that BIA is useful for the management of heart failure in adult patients with congenital heart disease.
Methods: We performed a retrospective single-center study of 173 consecutive adult patients with congenital heart disease who were admitted to our institute between April 2013 and December 2015. We retrospectively reviewed the medical records of the patients to evaluate the relationship between the BIA parameters (intracellular water, extracellular water, protein, mineral, fat, edema index (EI, ratio of extracellular water to total body water)) and the laboratory values, echocardiographic parameters, and prevalence of cardiac events.
Results: The patients in functional classes 3 and 4 had a higher EI compared with the patients in functional classes 1 and 2 (0.395 vs. 0.384, p < 0.001). In the multivariate analysis, the EI was significantly related to serum albumin, BUN, and BNP. In addition, the reduction in body weight (BW) achieved during the hospitalization was significantly related to the reduction in EI; using a generally defined upper limit of EI as 0.39, we developed this model equation: Required BW reduction (kg) = 98.1(EI – 0.39) + 2.26(Protein) – 4.14(Mineral) – 0.04(BUN) – 1.86. During the median follow-up period of 36 months, the Kaplan-Meier analysis revealed that an EI of more than 0.39 was significantly associated with an increased prevalence of cardiac events. Using the Cox hazard model, we determined that the hazard ratio of cardiac events in patients with an EI ≧0.39 compared to patients with an EI <0.39 was 3.9 (95%CI 2.0-7.9). In patients who had undergone a Fontan operation, the hazard ratio was 7.0(95%CI 1.4-77.1).
Conclusions: The Edema index determined by BIA is a useful marker for the treatment of heart failure and the prediction of cardiac events in adult patients with congenital heart disease.
Article Information
vol. 134 no. Suppl 1 A11365
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Masaki Sato;
- Kei Inai;
- Mikiko Shimizu;
- Daiji Takeuchi;
- Testuko Ishii;
- Keiko Toyohara;
- Tokuko Shinohara;
- Hisashi Sugiyama;
- Hirofumi Tomimatsu;
- Toshio Nakanishi;
- In-Sam Park
- Pediatric cardiology, Tokyo Women’s Med Univ, Tokyo, Japan
Abstract 20517: Coronary Artery Disease in Eisenmenger Syndrome
Joseph T Poterucha, Nandan S Anavekar, Alexander C Egbe
Circulation. 2016;134:A20517
Abstract
Background: A long held maxim in congenital heart disease is that patients (pts) with cyanotic congenital defects do not develop coronary artery disease (CAD) due to hypothetical protective effects of hypocholesterolemia, hypoxemia, indirect hyperbilirubinemia, thrombocytopenia, and upregulation of nitric oxide. We aimed to report the first case series of adult pts with Eisenmenger syndrome (ES) who developed CAD.
Methods: Adult pts with ES were identified by searching the Mayo Clinic medical record from 1990-2016. Clinical and catheterization data were collected and analyzed from those pts with ES and CAD.
Results: Overall, 177 adult pts (58 males) with ES were identified. A total of 86 pts underwent cardiac catheterization of whom, 8 pts (9.3%; 4 males) were diagnosed with CAD at a median age of 55 (31-68) years (left main disease, n=3, two-vessel disease, n=2, one-vessel disease, n=3)(Table). Extrinsic ostial left main coronary artery compression from an enlarged main pulmonary artery was the mechanism of left main disease in 2/3 pts. Two pts suffered ST elevation myocardial infarctions. PCI and stent placement was undertaken 4 pts (bare metal stent, n = 3; drug eluting stent, n = 1). Three pts had premature CAD. One or more traditional risk factors for CAD were present in 88% of pts. All pts were on pulmonary vasodilator therapy. The oldest pt with ES to develop CAD was a 68 year-old male with unoperated single ventricle (double-inlet left ventricle with L-transposition).
Conclusion: In contrast to longstanding dictum, pts with ES can develop CAD. Development of CAD in ES pts may be attributed to longevity secondary to pulmonary vasodilator therapies in addition to acquired CAD risk factors. Pulmonary artery coronary compression may be an unique mechanism of left main disease and may play a role in sudden death of these pts. Assessment for CAD should not be ignored in pts with ES. More study is needed to identify risk factors for CAD in ES pts.
Article Information
vol. 134 no. Suppl 1 A20517
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Div of Pediatric Cardiology, Dept of Pediatric and Adolescent Medicine, Mayo Clinic College of Medicine, Rochester, MN
- 2Dept of Cardiology, Mayo Clinic College of Medicine, Rochester, MN
- 3Div of Adult Congenital Heart Disease, Dept of Cardiology, Mayo Clinic College of Medicine, Rochester, MN
Abstract 20040: Risk Assessment in Pregnant Women With Congenital Heart Disease
Leah A Goldberg, Lacey P Gleason, Emily S Ruckdeschel, Tanmay Bhamare, David Drajpuch, Adi Hirshberg, Sara L Partington, Rachel Rogers, Sindhu K Srinivas, Natalie Stokes, Lynda Tobin, Lisa D Levine, Yuli Y Kim
Circulation. 2016;134:A20040
Abstract
Introduction: As more women with congenital heart disease (CHD) survive into their childbearing years, clinicians are faced with assessing pregnancy risk. Published risk stratification schemes have shown variable accuracy in predicting adverse cardiac outcomes in pregnancy for women with CHD.
Hypothesis: The modified World Health Organization (WHO) criteria are superior to the CARPREG and ZAHARA risk scores in predicting pregnancy outcomes in CHD.
Methods: This is a retrospective, single center study examining women ≥ 18 years with CHD who delivered between 1998 and 2014. CARPREG and ZAHARA risk scores and modified WHO criteria were applied to each subject. Cardiac events (i.e. at least one of the following: arrhythmia, heart failure or pulmonary edema, thromboembolic complications, transient ischemic attack, stroke, endocarditis, myocardial infarction, cardiac arrest, cardiac death) were assessed up to six months post-partum. Logistic regression analyses were performed and the area under the receiver operating curve (AUC) was calculated.
Results: There were 186 pregnancies (mean maternal age 32 years) and the most common CHD lesions were congenital aortic stenosis (17%), atrial septal defect (17%), and tetralogy of Fallot (12%). There were 31 cardiac events (17%) and no deaths. CARPREG and ZAHARA overestimated risk for the highest risk pregnancies: the estimated vs. observed event rates were 75% vs. 25% (N=4 at risk, p=0.021) for CARPREG and 70% vs. 38% (N=13 at risk, p=0.013) for ZAHARA. Figure 1 demonstrates the AUC for CARPREG (0.61), ZAHARA (0.78), and modified WHO (0.67) for cardiac events.
Conclusions: CARPREG and ZAHARA scores overestimate risk for higher risk pregnancies in women with CHD. In contrast to recent studies, ZAHARA risk score emerged as the model with the best discrimination for predicting adverse cardiac events. Further research is necessary to better refine risk stratification schemes for this complex patient population.
Article Information
vol. 134 no. Suppl 1 A20040
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Leah A Goldberg1;
- Lacey P Gleason1;
- Emily S Ruckdeschel2;
- Tanmay Bhamare1;
- David Drajpuch2;
- Adi Hirshberg3;
- Sara L Partington1;
- Rachel Rogers4;
- Sindhu K Srinivas3;
- Natalie Stokes3;
- Lynda Tobin1;
- Lisa D Levine3;
- Yuli Y Kim1
- 1Philadelphia Adult Congenital Heart Cntr, Univ of Pennsylvania Health System, Philadelphia, PA
- 2Philadelphia Adult Congenital Heart Cntr, The Children’s Hosp of Philadelphia, Philadelphia, PA
- 3Dept of Obstetrics and Gynecology, Univ of Pennsylvania Health System, Philadelphia, PA
- 4Biostatistics and Data Management Core, The Children’s Hosp of Philadelphia, Philadelphia, PA
Abstract 18648: Derangements in Hepatic Structure and Renal Function are Associated With Longer Duration of Follow-up After Fontan Completion
Thomas G Wilson, Yves d’Udekem, David S Winlaw, Rachael L Cordina, David S Celermajer, Gavin R Wheaton, Andrew Bullock, Thomas L Gentles, Robert G Weintraub, Robert N Justo, Leeanne E Grigg, Dorothy J Radford, Winita Hardikar, Michael Cheung, Timothy M Cain, Padma Rao, Stephen I Alexander, Diana Zannino, Ajay J Iyengar
Circulation. 2016;134:A18648
Abstract
Introduction: In Fontan survivors, systemic venous hypertension may lead to liver and renal dysfunction. The incidence of hepatic & renal impairment, the best method of diagnosis, and their predisposing factors are unclear.
Methods: A total of 151 participants from a binational registry of 1,535 patients underwent hepatic evaluation using ultrasound, transient elastography (FibroScan), serum fibrosis score (FibroTest) and standard laboratory testing, and renal evaluation using ultrasound, 99m-Tc-DTPA measurement of glomerular filtration rate (GFR), and urine albumin:creatinine ratio (ACR). Cut-off values of 10 kPa (FibroScan) and 0.49 (FibroTest) were used to define ≥F2/4 fibrosis. Proteinuria was defined as ACR ≥2.5 in males and ≥3.5 in females.
Results: Mean age and time since Fontan were 19.6 ± 9.2 and 14.0 ± 7.5 years, respectively. Fibrosis (≥F2/4) was present on FibroScan in 117/133 (88%), on FibroTest in 54/118 (46%), and on both in 40/104 (38%). Fibrosis was observed on ultrasound in 44/108 (41%), and no patient was identified to have hepatocellular carcinoma. Renal impairment was mild (GFR 60-89) in 43/130 (33%) and moderate (GFR 30-59) in 3/130 (2%). Proteinuria was detected in 54/121 participants (45%). FibroTest score was correlated with FibroScan value (r=0.248, p=0.01) and ACR (r=0.127, p=0.004). Independent predictors of increased FibroTest score (≥F2) included male gender (OR 2.52, 95% CI: 1.21-5.40, p=0.014) and time since Fontan (per year; OR 1.05, 95% CI: 1.03-1.08, p=0.034). No significant correlation between GFR and FibroScan or FibroTest was observed. Longer duration of time since Fontan was correlated with reduced GFR (1.2mL/min/1.73m2/year if proteinuria was present), and increased FibroScan and FibroTest values (r=-0.267, p=0.002; r=0.212, p=0.014; and r=0.227, p=0.013, respectively).
Conclusions: In this cross-sectional study, abnormalities in liver structure and renal function were common, and severity were associated with longer duration of time after Fontan. Proteinuria was present in almost half of patients. Prevention of end-organ dysfunction should be the focus of future research.
Article Information
vol. 134 no. Suppl 1 A18648
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Thomas G Wilson1;
- Yves d’Udekem2;
- David S Winlaw3;
- Rachael L Cordina4;
- David S Celermajer5;
- Gavin R Wheaton6;
- Andrew Bullock7;
- Thomas L Gentles8;
- Robert G Weintraub9;
- Robert N Justo10;
- Leeanne E Grigg11;
- Dorothy J Radford12;
- Winita Hardikar13;
- Michael Cheung9;
- Timothy M Cain14;
- Padma Rao15;
- Stephen I Alexander3;
- Diana Zannino1;
- Ajay J Iyengar2,
- The Australia and New Zealand Fontan Registry
- 1Heart Rsch Group, Murdoch Children’s Rsch Institute, Melbourne, Australia
- 2Dept of Cardiac Surgery, Royal Children’s Hosp, Melbourne, Australia
- 3The Heart Cntr for Children, The Children’s Hosp at Westmead, Sydney, Australia
- 4Dept of Cardiology, Royal Prince Alfred Hosp, Sydney, Australia
- 5Dept of Cardiology,, Royal Prince Alfred Hosp, Sydney, Australia
- 6Dept of Cardiology, Women’s and Children’s Hosp, Adelaide, Australia
- 7Children’s Cardiac Cntr, Princess Margaret Hosp for Children, Perth, Australia
- 8Greenlane Paediatric and Congenital Cardiac Service, Starship Children’s Hosp, Auckland, New Zealand
- 9Dept of Cardiology, Royal Children’s Hosp, Melbourne, Australia
- 10Queensland Paediatric Cardiac Service, Lady Cilento Children’s Hosp, Brisbane, Australia
- 11Dept of Cardiology, The Royal Melbourne Hosp, Melbourne, Australia
- 12Adult Congenital Heart Unit, The Prince Charles Hosp, Brisbane, Australia
- 13Dept of Gastroenterology, Royal Children’s Hosp, Melbourne, Australia
- 14Dept of Radiology, Royal Children’s Hosp, Melbourne, Australia
- 15Dept of Med Imaging, Royal Children’s Hosp, Melbourne, Australia
Abstract 18479: Double Outlet Right Ventricle in the Adult: A Broad Spectrum of Anatomic Diagnoses and Their Association With Arrhythmia and Sudden Death
Maria Boutsikou, Alejandro Silveira-Correa, Alexander Kempny, Martin Grubler, Pawel Piatek, Rafael Alonso-Gonzalez, Lorna Swan, Anselm Uebing, Michael A Gatzoulis, Konstantinos Dimopoulos
Circulation. 2016;134:A18479
Abstract
Background: Double outlet right ventricle (DORV) includes a broad spectrum of anatomic diagnoses, most of which amenable to biventricular repair, with a resultant improvement in survival. Limited data exist on the incidence of arrhythmia and sudden cardiac death (SCD) in adults with DORV.
Methods: Adult DORV patients (pts).followed at a tertiary center (1999-2016) were included and grouped into: group 1 (subaortic VSD type), group 2 (Fallot-type), group 3 (transposition with pulmonary stenosis), group 4 (transposition without pulmonary stenosis) and group 5 (complex anatomy). The primary endpoint was the composite of all-cause mortality and appropriate Implantable Cardioverter Defibrillator (ICD) shocks. The composite endpoint of SCD and appropriate ICD shocks was the secondary endpoint.
Results: Overall, 151 pts were included: 34 (22.5%) in group 1, 23 (15.2%) in group 2, 26 (17.2%) in group 3, 16 (10.6%) in group 4 and 52 (34.4%) in group 5. Over a median follow up period of 7.5 years, supraventricular tachycardias (SVTs) were observed during follow-up in 35 pts (3.2% per person years(ppy)), the most frequent being atrial tachycardia (n=23) (2.1% ppy). At least one ventricular tachycardia (VT) was seen in 15 pts (1.3% ppy). During this period, 29 pts died (mortality rate 2.3% ppy). There were 7 cases of SCD and 3 appropriate ICD shocks. Other deaths were mainly heart failure related. QRS duration >180msec at baseline (HR 7.5, 95%CI:2.2-26.1, p=0.002), history of SVT (HR 8.8, 95%CI:2.9-26.7, p<0.001) and prior palliative operations (HR 3.7, 95%CI:1.6-8.2, p=0.002) were significant predictors of the primary endpoint. QRS duration>180ms (HR 21.2, 95%CI:5.3-85.7, p<0.001) and SVT history (HR 9.6, 95%CI:1.9-46.8, p=0.005) were significant predictors of the composite secondary endpoint.
Conclusion: Arrhythmias and SCD are not uncommon in patients with DORV. Risk stratification tools are required to identify patients at risk who should be followed closely and, if at risk of SCD, offered an ICD for primary prevention.
Article Information
vol. 134 no. Suppl 1 A18479
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Maria Boutsikou;
- Alejandro Silveira-Correa;
- Alexander Kempny;
- Martin Grubler;
- Pawel Piatek;
- Rafael Alonso-Gonzalez;
- Lorna Swan;
- Anselm Uebing;
- Michael A Gatzoulis;
- Konstantinos Dimopoulos
- 1Adult Congenital Heart Disease and Pulmonary Hypertension, Royal Brompton Hosp, London, United Kingdom
Abstract 18314: Adult Congenital Heart Failure Admissions in the United States: Trends, Resource Utilization & Mortality
Luke J Burchill, Lina Gao, Jessica Minnier, Adrienne H Kovacs, Abigail M Khan, Alexander Opotowsky, Craig S Broberg, Bryan G Maxwell
Circulation. 2016;134:A18314
Abstract
Objectives: The primary objective of this study was to characterize temporal trends, health resource utilization, and outcomes in heart failure (HF) hospitalizations among adults with congenital heart disease.
Background: Understanding HF hospitalization patterns and resource needs among adult congenital heart disease (ACHD) patients is necessary to address the future care needs of this rapidly expanding population.
Methods: The Nationwide Inpatient Sample (NIS) is a stratified sample designed to approximate a 20% sample of US community hospitals; sampling weights are used to produce a national sample. Using the NIS we compared trends in ACHD related HF hospitalizations versus non-congenital HF admissions between 1998 and 2011. Trends during the study period were evaluated using the Mann-Kendall trend test. ACHD-related HF hospitalization outcomes were assessed including mortality and high resource utilization (HRU) admissions. Multivariable logistic regression was used to examine factors influencing mortality following HF hospitalization.
Results: During the study period, ACHD-related HF hospitalizations increased from 4620 to 8809 constituting a 91% rise (p<0.0001). HF as a primary diagnosis increased 47% in ACHD patients (p=0.001) whereas HF as a primary diagnosis in non-ACHD patients was unchanged (p=0.58). The distribution of HF hospitalizations remained stable across all ACHD age groups. Whereas high volume ACHD centers accounted for 10% of adult hospitals they managed 53% of ACHD HF admissions. Hospitalization in a high volume center was associated with lower mortality (OR 0.86 CI 0.75-0.99, p = 0.03). ACHD HF patients had longer inpatient stays with criteria for HRU being met in 21% of ACHD-related HF hospitalizations vs. 10% of others (p<0.001).
Conclusions: We report a stark rise in hospitalizations and costs associated with ACHD-related HF over the last decade. The lower mortality during HF hospitalizations in high volume ACHD centers suggests that the availability of ACHD HF expertise may improve HF outcomes.
Article Information
vol. 134 no. Suppl 1 A18314
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Luke J Burchill1;
- Lina Gao2;
- Jessica Minnier3;
- Adrienne H Kovacs1;
- Abigail M Khan1;
- Alexander Opotowsky4;
- Craig S Broberg1;
- Bryan G Maxwell5
- 1Knight Cardiovascular Institute Adult Congenital Heart Program,, Oregon Health Science Univ, Portland, OR
- 2Knight Cancer Institute, Oregon Health Science Univ, Portland, OR
- 3Knight Cardiovascular Institute, Oregon Health Science Univ, Portland, OR
- 4Boston Adult Congenital Heart Service Cardiovascular Program, Harvard Med Sch, Boston, MA
- 5Anesthesiology, Legacy Emanuel Med Cntr, Portland, OR
Abstract 17988: Red Cell Distribution Width in Adults With Congenital Heart Disease: Results From the Boston Adult Congenital Heart Biobank
Laith Alshawabkeh, Nureddin Almaddah, Brittani Loukas, Michael J Landzberg, Saurabh Rajpal, Hannah Stonebreaker, Annelieke C Van Riel, Anne Marie Valente, Georges Ephrem, Fred Wu, Keri Shafer, Alexander R Opotowsky
Circulation. 2016;134:A17988
Abstract
Introduction: There are few validated subclinical predictors of adverse clinical and surrogate outcomes in adults with congenital heart disease (CHD). Red cell distribution width (RDW) is a strong predictor of structural and functional outcomes in the non-CHD population.
Hypothesis: RDW is associated with New York Heart Association Functional Class (NYHA FC), peak oxygen consumption and minute ventilation relative to CO2 production independent of underlying congenital diagnosis and other relevant variables.
Methods: We conducted a cross-sectional study to investigate the correlation between RDW and measures of cardiometabolic status and functional capacity in adults with CHD enrolled in the Boston Adult CHD Biobank between 2012 and 2015.
Results: Among 588 adults with CHD, age averaged 38.6±13.4 years and 50.9% were female. Most common diagnoses were left sided obstructive lesions (21.6%), tetralogy of Fallot or double outlet right ventricle (20.7%), single ventricle/Fontan circulation (17.1%). Median RDW was 13.7% (interquartile range 13.3 – 14.3%). RDW correlated modestly with age (Pearson r = 0.20), hemoglobin concentration (r = -0.12), mean corpuscular volume (r = -0.44), creatinine (r = 0.28), and log C-reactive protein (r = 0.20), all p<0.01. RDW>15% (12.9% of participants) was present in only 7.5% of patients in NYHA FC I, while this figure was 23.3% for NYHA FC II and 46.4% for NYHA FC III/IV, Fisher’s exact p<0.0001. RDW was a significant predictor of peak oxygen consumption, minute ventilation relative to CO2production and oxygen saturation, even after adjustment for demographic and clinical covariates (Table).
Conclusion: Elevated RDW is associated with impaired cardiometabolic status and functional capacity in adults with CHD. Future research should explore the biological pathways behind these observations along with their possible applications to clinical outcomes.
Article Information
vol. 134 no. Suppl 1 A17988
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Laith Alshawabkeh1;
- Nureddin Almaddah2;
- Brittani Loukas3;
- Michael J Landzberg1;
- Saurabh Rajpal3;
- Hannah Stonebreaker3;
- Annelieke C Van Riel4;
- Anne Marie Valente3;
- Georges Ephrem5;
- Fred Wu3;
- Keri Shafer3;
- Alexander R Opotowsky1
- 1Cardiology, Boston Children’s and Brigham & Women’s Hosps, Harvard Med Sch, Boston, MA
- 2Medicine, North Shore Med Cntr, Salem, MA
- 3Cardiology, Boston Children’s Hosp, Boston, MA
- 4Cardiology, Academic Med Cntr in Amsterdam, Amsterdam-Zuidoost, Netherlands
- 5Cardiovascular Medicine, Oakland Univ-William Beaumont Sch of Medicine at Beaumont Health System, Royal Oak, MI
Abstract 17578: Pregnancy is Associated With Stable Right Ventricular Function but a High Burden of Arrhythmias in Women With Transposition of the Great Arteries After Atrial Switch
Alan H Baik, Aarthi Sabanayagam, Anushree Agarwal, Ian Harris, Elyse Foster
Circulation. 2016;134:A17578
Abstract
Introduction: Most adult patients with d-transposition of the great arteries (d-TGA) have undergone an atrial switch operation. Insufficient data exists regarding the effects of pregnancy on adverse outcomes, including RV failure, tricuspid regurgitation (TR), and atrial arrhythmias, in these patients.
Hypothesis: We hypothesized that pregnancy in patients with TGA following atrial switch is associated with worsening RV systolic function and a high burden of arrhythmias.
Methods: Longitudinal observational cohort study of adult women with TGA following atrial switch in a tertiary care adult congenital cardiology clinic. Serial echocardiogram, Holter, and EKG reports were reviewed. Ordinal variables were represented as percentages and medians.
Results: A total of 20 patients were included. Of the 85% of patients with at least one pregnancy, 47% had 1 pregnancy, with a total of 29 pregnancies in the cohort. The most recent follow-up echo was done at a median of 54 months (30, 126 months) after last pregnancy. On most recent echo, patients had trace-mild TR (87.5%), mild pulmonary regurgitation (93.8%), moderate RV hypertrophy (60%), and mildly decreased RV systolic function (46%). Compared to echos prior to first pregnancy, there was no change in TR in 67% of patients, and 11% of patients had worsening TR from mild to moderate. Pulmonary valve regurgitation was unchanged in all patients. RV systolic function was stable except for one patient who had worsening from moderate to severe RV function. Arrhythmias were documented in 62.5% of patients, including atrial flutter (18.75%), atrial fibrillation (12.5%), accelerated junctional rhythm (6.25%), sick sinus syndrome (18.75%), SVT (6.25%), and Torsades (6.25%). 43.75% of arrhythmias were detected post-pregnancy. There were no deaths or hospitalizations for heart failure in the peripartum period.
Conclusions: In conclusion, this study found that in women with TGA after atrial switch, pregnancy is not significantly associated with worsening RV systolic function, TR, and pulmonary valve regurgitation. Most patients developed arrhythmias at an incidence that was higher than seen in prior reports. Future work will assess if change of peak RV systolic strain predicts the development of arrhythmias.
Article Information
vol. 134 no. Suppl 1 A17578
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Cardiology, UCSF Dept of Medicine, San Francisco, CA
- 2Cardiology, UCSF, San Francisco, CA
- 3Cardiology, UCSF Div of Cardiology, San Francisco, CA
Abstract 16853: Prognostic Value of Plasma Parathyroid Hormone Levels in Adult Congenital Heart Disease
Takeshi Shimizu, Kei Inai, Seiji Asagai, Eriko Shimada, Tokuko Shinohara, In S Park, Toshio Nakanishi
Circulation. 2016;134:A16853
Abstract
Introduction: Plasma parathyroid hormone (PTH) level predicts cardiovascular morbidity and mortality in patients with chronic heart failure. In the previous study, we showed that Vitamin D deficiency and secondary hyperparathyroidism are common in adult patients with congenital heart disease (CHD). However, the prognostic predictive value of plasma PTH level in adult patients with CHD remains unclear.
Hypothesis: We have hypothesized that plasma PTH level can predict cardiovascular morbidity and mortality in adult patients with CHD.
Method: This study was a single-center, prospective study, and consisted of 86 consecutive patients. An intact PTH laboratory test was ordered for each of the 86 patients. All of the patients underwent follow-up surveys for morbidity (hospitalization for heart failure) and mortality over 3 years. The enrolled patients were divided into two groups based on the levels (the upper limit of the normal range: 65 pg/ml) of PTH.
Results and Conclusions: According to the classification of the Working Group on research in adult congenital heart disease: National Heart, Lung, and Blood Institute, the 86 patients were classified as follows: 19 simple CHDs, 14 moderate severity CHDs, and 53 CHDs of great complexity. Intact-PTH values (median 60.5 pg/ml, interquartile range 45.8-82.3) were elevated in this cohort, and 41 (48 %) patients had intact-PTH values above the upper limit of the normal range. Between the two groups, the high-PTH group (PTH≧65 pg/ml) had significantly higher levels of brain natriuretic peptide (p = 0.011) and functional class (p = <0.001), and lower levels of estimated glomerular filtration ratio (p = 0.04), 25-hydroxyvitamin D (p < 0.001), cardiac index (p = 0.024) and 6-minute walking distance (p = 0.008). During a follow-up period (mean: 48 months), 8 patients died and 12 patients were hospitalized for heart failure. Kaplan-Meier survival curves demonstrate that patients with higher levels of intact PTH had higher mortality (Log-lank p = 0.029) and morbidity (Log-lank p = 0.034). Plasma PTH levels may have a prognostic value for mortality and morbidity in adult patients with CHD.
Article Information
vol. 134 no. Suppl 1 A16853
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Takeshi Shimizu;
- Kei Inai;
- Seiji Asagai;
- Eriko Shimada;
- Tokuko Shinohara;
- In S Park;
- Toshio Nakanishi
- Pediatric Cardiology, Heart Institute, Tokyo Women’s Med Univ, Tokyo, Japan
Abstract 15230: Development and Validation of a Natural Language Processing System for Identifying and Classifying Severe Congenital Heart Defects: The PORTAL CHD Study
Keane K Lee, Jingrong Yang, Alison K Meadows, Kristi Reynolds, David Magid, Sue Hee Sung, Alan S Go
Circulation. 2016;134:A15230
Abstract
Introduction: The number of adults with congenital heart defects (CHD) is increasing nationally with recognition of the need to improve surveillance and care across the lifespan. Yet, accurately identifying patients with severe CHD, from electronic medical records (EMR) is challenging.
Methods: Within 3 integrated healthcare delivery systems (Kaiser Permanente in Northern California (KPNC), Southern California (KPSC), and Colorado (KPCO)) serving >8.5 million members, we identified 66,775 adults with a CHD diagnostic code during 2008-2013; 1652 had ≥1 severe CHD diagnosis code (atrioventricular canal defect [AVCD], Eisenmenger syndrome, single ventricle physiology, Tetralogy of Fallot [TOF], or transposition of the great arteries [TGA]). We developed a natural language processing (NLP) system using Linguamatics i2E and split-sample validation in KPNC based on medical records review by a CHD specialist. Positive predictive value (PPV) and negative predictive value (NPV) were calculated for each severe CHD condition. Accuracy of the refined NLP system was also evaluated among 216 KPCO patients and 373 KPSC patients with severe CHD diagnosis codes.
Results: The KPNC NLP system had high PPV and NPV across all severe CHD diagnoses and improved after refinement (range 96-100%, Table). Validation results in KPCO showed lower PPVs and NPVs, especially the NPV for TGA and single ventricle (Table). The results of the same NLP system in KPSC were better, with PPVs and NPVs that were approximately 90% except TGA (0% NPV) because the NLP identified one diagnosis out of 44 as not being TGA, when all the ICD-9 diagnoses were accurate.
Conclusion: We developed and validated an NLP system for accurate identification persons with severe CHD from unstructured EMR data that can facilitate population-based opportunities for quality improvement and future research.
Article Information
vol. 134 no. Suppl 1 A15230
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Keane K Lee1;
- Jingrong Yang2;
- Alison K Meadows3;
- Kristi Reynolds4;
- David Magid5;
- Sue Hee Sung2;
- Alan S Go2,
- Kaiser Permanente&Strategic Partners Patient Outcomes Rsch to Advance Learning (PORTAL) Network
- 1Dept of Cardiology, Kaiser Permanente Santa Clara Med Cntr, Santa Clara, CA
- 2Div of Rsch, Kaiser Permanente Northern California, Oakland, CA
- 3Dept of Cardiology, Kaiser Permanente San Francisco Med Cntr, San Francisco, CA
- 4Div of Rsch & Evaluation, Kaiser Permanente Southern California, Pasadena, CA
- 5Dept of Emergency Medicine, Univ of Colorado, Denver, CO
Abstract 14544: Ramipril Efficacy on Left Ventricular Systolic and Diastolic Function in Stable Patients With Pulmonary Regurgitation After Repair of Tetralogy of Fallot
Sylvia Krupickova, Michael A. Gatzoulis, Mun Hong Cheang, Michael Rigby, Alain Fraisse, Anselm Uebing, Konstantinos Dimopoulos, Lorna Swan, Rafa Alonso-Gonzales, Wei Li, Sonya V. Babu-Narayan
Circulation. 2016;134:A14544
Abstract
Introduction: We reported previously complex results of the APPROPRIATE (ACE inhibitors for Potential PRevention Of the deleterious effects of Pulmonary Regurgitation In Adults with repaired TEtralogy of Fallot) randomised double-blinded placebo controlled trial of ramipril therapy. More recently it has become evident that measures of left ventricular (LV) systolic and diastolic function are major predictors for mortality.
Hypothesis: The aim of this study was to provide retrospective echocardiographic analysis of patients entered into the APPROPRIATE study to further characterise degree and mechanism of LV remodeling with therapy.
Methods: Echocardiographic analysis of LV function of baseline and follow-up scans was retrospectively performed in 64 patients; 32 in the ramipril and 32 in the placebo group.
Results: There was significant difference in change in long axis shortening (1.9±4.2 mm vs -0.2±3.7 mm; p = 0.030), peak lateral systolic velocity – S’ lateral (1.0±2.0 cm/s vs -0.3±2.2 cm/s; p = 0.025), peak lateral early diastolic velocity – E’ lateral (0.57±2.4 cm/s vs -3.3±3.9 cm/s; p<0.001) and transmitral to lateral mitral annular early diastolic velocity ratio – E/E’ lateral (-0.7±1.9 vs 1.5±1.9; p<0.001) between baseline and follow-up when compared Ramipril to placebo group. LV long axis shortening (15.2±4.2 mm vs 17.0±3.1 mm; p = 0.008) improved in the Ramipril group. There was also significant worsening of the LV long axis shortening (15.1±2.8 mm vs 14.8±3.8 mm; p<0.05), E’ lateral (16.0±4.2 cm/s vs 13.0±3.0 cm/s; p = 0.001) and E/E’ lateral (5.5±1.4 vs 6.9±1.9; p = 0.003) in the placebo group. In addition, a subgroup of patients with restrictive physiology showed significant improvement in active left atrial emptying fraction (37.0±11.8 % vs 48.0±8.6 %; p = 0.043) in Ramipril arm and improvement in peak late diastolic velocity (A) (5.9±13.5 cm/s vs -5.8±12.5 cm/s; p = 0.041) and early to late diastolic transmitral velocity ratio – E/A (-0.18±0.42 vs 0.23±0.48; p = 0.037) between baseline and follow-up when Ramipril was compared to the placebo.
Conclusion: This study demonstrates that 6 months’ treatment with ramipril improves both systolic and diastolic LV function in patients with pulmonary regurgitation late after Tetralogy of Fallot repair.
Article Information
vol. 134 no. Suppl 1 A14544
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Sylvia Krupickova1;
- Michael A. Gatzoulis2;
- Mun Hong Cheang3;
- Michael Rigby1;
- Alain Fraisse1;
- Anselm Uebing2;
- Konstantinos Dimopoulos2;
- Lorna Swan2;
- Rafa Alonso-Gonzales2;
- Wei Li2;
- Sonya V. Babu-Narayan2
- 1Paediatric Cardiology, Royal Brompton Hosp, London, United Kingdom
- 2Adult CongenitalHeart Disease, Royal Brompton Hosp, London, United Kingdom
- 3UCL Institute of Cardiovascular Science, Univ College London, London, United Kingdom
Abstract 14607: Pregnancy and Long-Term Heart Failure Risk in Women With Congenital Heart Disease
Andreas P Kalogeropoulos, Anita Saraf, Trenton Hoffman, Cheryl Raskind-Hood, Fred H Rodriguez, Carol J Hogue, Wendy M Book
Circulation. 2016;134:A14607
Abstract
Introduction: There are limited data on long-term risk for heart failure (HF) after pregnancy in women with congenital heart disease (CHD).
Hypothesis: We hypothesized that type of CHD would be associated with long-term risk for HF in pregnant women with CHD.
Methods: We extracted 20-year (1996-2016) data for women who received CHD services (based on ICD9-CM codes 745-747) in our institution between 2008 and 2014 (cohort inception ). Pregnancy was identified through ICD9-CM codes 630-679, V22-24, V27-28, and V91. The earliest occurrence of a pregnancy-associated service was considered as baseline. We defined HF as ICD9-CM codes 428, 402.X1, 404.X1, and 404.X3 (Medicare definition). Incident HF was defined as new HF-associated services after baseline. We followed a modified Marelli classification for CHD severity.
Results: We identified 667 women with CHD who received pregnancy-associated services. Of these, 118 (17.9%) received HF-associated services before receiving any pregnancy-associated service and were deemed to have HF at baseline. Among the 549 women without HF at baseline, followup data were available in 534 (97.3%). Table 1 summarizes their characteristics. Of these, 108 received new HF-related services over a median of 4.9 (2.2-8.2) years. Risk for HF decelerated after 1 year but remained elevated (Fig. 1). By 5 years, 18.4% of women received HF-related services. Women with severe CHD were at highest risk (5-year risk 45.6%), followed by valvular (28.2%), shunts (27.5%), and other (21.4%) abnormalities.
Conclusions: Approximately 1 out of 5 of women with CHD will develop HF within 5 years after a 1st pregnancy. Risk is highest in the 1st year but remains elevated afterwards.
Article Information
vol. 134 no. Suppl 1 A14607
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Andreas P Kalogeropoulos1;
- Anita Saraf1;
- Trenton Hoffman2;
- Cheryl Raskind-Hood2;
- Fred H Rodriguez3;
- Carol J Hogue2;
- Wendy M Book1
- 1Medicine/Cardiology, Emory Univ, Atlanta, GA
- 2Rollins Sch of Public Health, Emory Univ, Atlanta, GA
- 3Pediatrics and Internal Medicine, Emory Univ, Atlanta, GA
Abstract 13080: Transition Readiness in Adolescents With Heart Disease as Perceived by Their Parents: Do Parents and Teens Agree?
Karen Uzark, Sunkyung Yu, Ray Lowery, Katherine Afton, Angela Yetman, Jonathan W Cramer, Nancy Rudd, Scott Cohen, Russell Gongwer, Michelle Gurvitz
Circulation. 2016;134:A13080
Abstract
Introduction: Transition is defined as “the process by which adolescents and young adults with chronic childhood illnesses are prepared to take charge of their lives and their health in adulthood”. Knowledge deficits and lack of transition readiness (TR) in 13-25 year olds with congenital or acquired heart disease have been previously reported. The aim of this multicenter study was to examine agreement between parental perceptions of their adolescent’s TR (knowledge, self-efficacy, self-management behaviors) and adolescent self-reported TR.
Methods: Adolescents (n=175), age 13-18 yrs, and their parents completed the TR Assessment utilizing an e-tablet, web-based format at a routine clinic visit. Parent responses to the survey were compared to the teens’ self-reported responses and items of greatest disagreement identified.
Results: Median patient age was 15.7 yrs. Parents perceived knowledge deficit scores (% of items with no reported knowledge) were significantly higher than self-reported by teens, 29.2% vs 25.9% p=.01. On a 100-point scale (higher = better), the mean score for self-efficacy was significantly lower as perceived by parents than by teens, 58.6 ± 21.1 vs 68.2 ± 18.3 (p<.0001), but parent and teen reports of self-management were not significantly different, 39.5 ± 15.2 vs 41.0 ± 15.8 (p=.27). For specific knowledge deficits, overall agreement ranged from poor to fair (kappa 0.07-0.41), highest for name of heart condition/surgery (0.41), poor for exercise/sports allowed (0.10) and follow-up needs (0.10). In patients on medications (n=94), agreement was moderate for medication purpose (0.42) and refill (0.46), but poor for name (0.17). For self-efficacy and self-management, agreement also ranged from poor to fair (kappa =0.16-0.29); parents more often perceived that their teen understood what the doctor said, but overestimated how difficult it was for the teen to talk to the doctor/nurse. Teens tended to request information more often than their parents (79% vs 65%, p=.06) and information requested varied (pregnancy/contraception, communication, insurance).
Conclusion: Parents and teens differ in their perceptions regarding TR. Routine TR assessment is important to identify transition needs for both patients and their parents.
Article Information
vol. 134 no. Suppl 1 A13080
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Karen Uzark1;
- Sunkyung Yu1;
- Ray Lowery1;
- Katherine Afton1;
- Angela Yetman2;
- Jonathan W Cramer2;
- Nancy Rudd3;
- Scott Cohen3;
- Russell Gongwer4;
- Michelle Gurvitz5
- 1Pediatrics, Univ of Michigan Congenital Heart Cntr, Ann Arbor, MI
- 2Pediatrics, Univ of Nebraska Med Cntr, Omaha, NE
- 3Pediatrics, Children’s Hosp of Wisconsin, Milwaukee, WI
- 4Pediatrics, Boston Children’s Hosp, Boston, MA
- 5Cardiology, Boston Children’s Hosp, Boston, MA
Abstract 11854: Nationwide In-hospital Outcomes of Pregnancy in Women With Single Ventricle Congenital Heart Disease
Ronnie T Collins, Adam Sandlin, Di Chang, Anthony Goudie, James M Robbins
Circulation. 2016;134:A11854
Abstract
Introduction: Most patients with single ventricle (SV) congenital heart disease (CHD) are expected to survive to adulthood. Women with SV are often counseled against pregnancy; however, data on pregnancies in these women are lacking. We sought to evaluate in-hospital outcomes of pregnancy in women with SV.
Methods: We used nationally representative data from 1998 to 2012 Nationwide Inpatient Sample database to identify patients ≥ 18 years of age admitted to the hospital with International Classification of Diseases-9th Revision codes for an intrauterine pregnancy and a diagnosis of either hypoplastic left heart syndrome, tricuspid atresia or common ventricle. A matched comparison group without a diagnosis of CHD or pulmonary hypertension was identified from the database. National estimates of hospitalizations were calculated. Length of stay (LOS), total hospital charges, and cardiovascular complications were analyzed and compared between groups. Charge data were adjusted to 2012 dollars.
Results: There were 310 admissions of pregnant women with SV (63% with deliveries) and 1547 admissions in the control group (91% with deliveries). There was no change in the annual number of SV pregnancies during the study period. Vaginal delivery was more common in SV (74% vs 72%, p<0.001). LOS (4.6 [0.98] days vs 2.5 [0.07], p<0.001) and charges ($38,627 [11,918] vs $13,880 [631], p<0.0001) were higher in SV. SV deliveries occurred more commonly in teaching hospitals (78% vs 51%, p<0.001). Complications occurred in nearly all SV admissions and were more common in SV compared to controls. (Table) There were no deaths in either group.
Conclusions: Pregnancies in women with SV are associated with increased hospital resource utilization and cardiovascular complications, though in-hospital pregnancy related death is rare. Vaginal delivery is common in these patients. These data suggest that pregnancy and vaginal delivery are well tolerated in women with SV.
Article Information
vol. 134 no. Suppl 1 A11854
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Pediatrics, Univ of Arkansas for Med Sciences, Little Rock, AR
- 2Obstetrics and Gynecology, Univ of Arkansas for Med Sciences, Little Rock, AR
Abstract 20210: Optical Coherence Tomography Provides Insight Into Early Coronary Changes Related to Cardiac Allograft Vasculopathy in Pediatric Transplant Recipients
Kevin C Harris, Stephan Schubert, Enrique Balbacid, Christine Voss, Nolan Lee, Martin C Hosking
Circulation. 2016;134:A20210
Abstract
Introduction: Cardiac allograft vasculopathy (CAV) is a common cause of graft failure and mortality in pediatric heart transplant (Tx) recipients. CAV is diagnosed with coronary angiography which is unable to detect early coronary vascular changes that do not cause luminal narrowing.
Hypothesis: 1) Optical coherence tomography (OCT) can detect angiographically-silent coronary changes; 2) children with new CAV have more severe intimal thickening than those without CAV.
Methods: The International Pediatric OCT Registry includes 75 Tx recipients (age at Tx 4.6±4.3yrs) from centers in Canada and Europe. Patients underwent ≥1 assessment of ≥1 coronary artery using OCT (St Jude Medical) at cardiac catherization. We included cases with data from ≥10 cross-sectional images ≥1mm apart; we identified the maximal intimal thickness. CAV was classified by angiography according to the ISHLT criteria with investigators blinded to OCT findings. We used multi-level regression to assess between-group differences.
Results: We included 93 cases (age 11.8±4.0yrs at OCT; posttransplant time 7.6±4.6yrs; 54% male). In newly diagnosed CAV (all grade 1), maximal intimal thickness was significantly greater (median 0.31mm; IQR 0.22-0.56) compared to those without CAV (0.18mm; 0.12-0.23; p<0.001). In 12 cases, a change in medical management was made, typically related to immuno-suppressant therapy (e.g. 3 started sirolimus, 7 started steroid therapy). Of these cases, 10 were angiographically silent. Intimal thickness was greater in cases where medical management was changed compared with those where it was not changed (0.29mm; 0.18-0.38 vs. 0.18mm; 0.12-0.22; p<0.001). Serial assessments were done in 17 patients (time between OCT assessments 1.6±0.6yrs). Intimal thickness did not change significantly over time in those with or without CAV. One patient was diagnosed with CAV at the second OCT and had angiographically-silent severe intimal thickening at first OCT (0.43mm).
Conclusions: OCT can detect changes in intimal thickness that are angiographically silent. Children with a new diagnosis of CAV have more pronounced intimal thickening than those without CAV. These findings suggest that OCT findings may be useful in evaluating for CAV after heart transplantation.
Article Information
vol. 134 no. Suppl 1 A20210
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Kevin C Harris1;
- Stephan Schubert2;
- Enrique Balbacid3;
- Christine Voss1;
- Nolan Lee1;
- Martin C Hosking1
- 1Pediatrics, Univ of British Columbia, Vancouver, Canada
- 2Pediatrics, Deutsches Herzzentrum Berlin, Berlin, Germany
- 3Pediatrics, Hosp Universitario La Paz, Madrid, Spain
Abstract 17576: Right Atrial and Right Ventricular Deformation Are Reflections of Right Ventricular Afterload in Predicting Outcomes in Pediatric Pulmonary Hypertension
Pei-Ni Jone, Ling Li, Matthew J Mulvahill, Mary Craft, D. Dunbar Ivy, Shelby Kutty
Circulation. 2016;134:A17576
Abstract
Background: Pulmonary hypertension (PH) results in right ventricular (RV) dysfunction. Elevated right atrial (RA) pressure is prognostic of adverse outcomes in PH. Strain imaging provides quantitative assessment of cardiac deformation and our previous study demonstrated that RA reservoir and conduit functions are decreased in pediatric PH compared to controls. In this study, we compared RA and RV deformation to invasive hemodynamics and assessed outcomes in pediatric PH.
Methods: Sixty-six PH patients (mean age 8.9 ±5.6 years) with 146 echocardiograms and 105 catheterizations were retrospectively evaluated. RA and RV deformation indices were obtained in the apical 4 chamber view using 2D speckle tracking (2DCPA, TomTec). RA strain, strain rates, emptying fraction, and RV global longitudinal strain (GLS) were measured. Tricuspid regurgitation (TR) velocity, end-systolic RV/LV ratio, TAPSE, and fractional area change (FAC) were measured. Systolic and mean pulmonary artery pressure (sPAP, mPAP), mean RA pressure (mRAP), pulmonary vascular resistance index (PVRi), and cardiac index were obtained. PH patients with and without clinical events were compared. Logistic regression was used to test the association of invasive indices and with adverse events defined as: initiation of intravenous prostacyclin, atrial septostomy, death, or transplant.
Results: PH patient with 22 adverse events had worse TR velocity, FAC, peak RA strain (ɛS), higher RV/LV ratio, sPAP, mPAP, and PVRi compared to patients with no clinical events (all p<0.01). There was significant association between early strain (ɛE), atrial EDV, and ESV with mRAP (estimate -o.o6, p<0.02; 2.13, p<0.001; 1.59, p<0.004 respectively). RVGLS was significantly associated with mPAP (estimate 0.08, p<0.004). ɛS, ɛE, early negative SR, RVGLS, and RV/LV ratio were found to be predictors of survival (HR 0.95, p<0.01; 0.95, p<0.04; 2.03, p<0.001; 1.18, p<0.001; 14.27, p<0.001).
Conclusions: High afterload results in RV dysfunction which results in impaired RA reservoir and conduit functions in pediatric PH patients. RA pump function remains preserved in pediatric PH. Reservoir, conduit function, RV strain, and RV/LV ratio (reflection of RV afterload) emerged as outcome predictors in pediatric PH.
Article Information
vol. 134 no. Suppl 1 A17576
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Pediatric Cardiology, Univ of Colorado Children’s Hosp Colorado, Aurora, CO
- 2Pediatric Cardiology, Univ of Nebraska Med Cntr, Omaha, NE
- 3Dept of Pediatrics, Univ of Colorado Sch of Medicine, Aurora, CO
Abstract 17065: Utilization of Magnetic Resonance Lymphangiography to Determine the Etiology of Chylothorax and Predict the Outcome of Lymphatic Embolization in Patients With Congenital Heart Disease
Jill Savla, Maxim Itkin, Joseph W Rossano, Yoav Dori
Circulation. 2016;134:A17065
Abstract
Introduction: Postoperative chylothorax in patients with congenital heart disease (CHD) is a challenging problem with high morbidity and mortality. Dynamic contrast-enhanced MR lymphangiography (DCMRL) is a novel technique to visualize the lymphatic system.
Methods: This study is a retrospective review of 18 patients with CHD and postoperative chylothorax, who presented for lymphatic intervention at our institution between July 2012 and May 2016.
Results: All 18 patients had T2-weighted MR imaging and 17 patients had both DCMRL and intranodal lymphangiography performed prior to intervention. We identified three groups: 2 patients (11%) with traumatic leak from a branch of the thoracic duct (TD), 9 patients (50%) with abnormal pulmonary lymphatic flow, and 7 patients (39%) with a central lymphatic flow disorder (CLFD). We define CLFD as lymphatic effusions in multiple compartments and retrograde central lymphatic flow by imaging. The patients with traumatic leak and abnormal pulmonary lymphatic flow were combined into a group of 11 patients without CLFD, of which 10 (91%) had an intact central TD. All 11 patients underwent lymphatic intervention, including selective or complete TD embolization. The median chest tube drainage decreased significantly from 7 days before (21 ml/kg/day, IQR 15-34) to 7 days after intervention (14 ml/kg/day, IQR 5-22) (p = 0.021). All 11 patients had resolution of chylothorax, with a median of 18 days (IQR 6-47) from intervention to discharge. Of the 7 patients with CLFD, 4 (57%) had an intact TD and 7 (100%) had ascites. Six patients underwent lymphatic intervention and there was no difference in the median chest tube drainage from 7 days before (31 ml/kg/day, IQR 27-61) to 7 days after intervention (38 ml/kg/day, IQR 16-111) (p = 0.735). All 7 patients died, with a median of 79 days (IQR 33-187) from intervention to death.
Conclusions: The majority of patients in this study had non-traumatic chylothorax and DCMRL was essential to determine the etiology. Percutaneous lymphatic embolization was successful in patients with traumatic leak and abnormal pulmonary lymphatic flow, and thus should be considered as first-line treatment. Interventions in patients with CLFD were not successful and alternate approaches need to be developed.
Article Information
vol. 134 no. Suppl 1 A17065
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Div of Cardiology, Children’s Hosp of Philadelphia, Philadelphia, PA
- 2CHOP/HUP Cntr for Lymphatic Imaging and Interventions, Hosp of the Univ of Pennsylvania, Philadelphia, PA
- 3CHOP/HUP Cntr for Lymphatic Imaging and Interventions, Children’s Hosp of Philadelphia, Philadelphia, PA
Abstract 14855: Altered Flow Hemodynamic Metrics in Descending Aorta Correlate With N-terminal Prohormone of Brain Natriuretic Peptide (NT-proBNP) in Youth With Type 1 Diabetes
Michal Schafer, Petter Bjornstad, Mason McClatchey, Kendall S Hunter, Melanie Cree-Green, Amy Baumgartner, Alex J Barker, Uyen Truong, Kristen J Nadeau
Circulation. 2016;134:A14855
Abstract
Introduction: Cardiovascular disease (CVD) remains the leading cause of mortality in T1D. Early non-invasive characterization of CVD in youth with T1D is thus of great importance. Therefore we aimed to: 1) characterize sensitive wall shear stress (WSS) parameters in youth with T1D, known to promote vascular remodeling in the descending aorta (DA); 2) examine the relationship between WSS and NT-proBNP, a known marker of ventricular dysfunction.
Hypothesis: NT-proBNP will correlate with WSS in youth with T1D.
Methods: Youth with T1D (n=37, mean age 16±2 years, 46 % female) and control youth (n=23, mean age 15±2, % female) underwent phase-contrast cardiac MRI evaluation of flow hemodynamic shear stress in the DA, 10 cm below the aortic isthmus. Collected indices included peak and time-averaged WSS (dyne/cm2), and vascular strain (%). Additionally, youth with T1D underwent a fasting blood sample for NT-proBNP (median: 41 [26-53] pg/mL). Generalized linear regression models were used to examine the relationships between NT-proBNP, WSS peak and WSS time averaged, adjusted for age and sex. NT-proBNP was positively skewed and thus natural log-transformed (ln).
Results: T1D youth had greater time-averaged WSS (4.2 vs. 2.7 (dyne/cm2), p < 0.0001) and peak systolic WSS (15.5 vs. 10.7 (dyne/cm2), p < 0.0001) vs. controls. Strain in the DA also decreased in participants with T1D (22 vs. 26 (%), p = 0.048). Ln(NT-proBNP) was associated with time averaged WSS (β±SE: 1.06 ± 0.27, p = 0.0005) and peak WSS (β±SE: 2.75 ± 1.13, p = 0.02).
Conclusion: Flow hemodynamic shear was significantly increased in the DA in T1D youth, and was associated with NT-proBNP concentrations. Vascular stiffness promoting shear forces may play an important role in the development of CVD in youth with T1D, and NT-proBNP may be a potential clinical marker for early vascular dysfunction in this population.
Article Information
vol. 134 no. Suppl 1 A14855
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Michal Schafer1;
- Petter Bjornstad2;
- Mason McClatchey3;
- Kendall S Hunter1;
- Melanie Cree-Green2;
- Amy Baumgartner2;
- Alex J Barker4;
- Uyen Truong5;
- Kristen J Nadeau2
- 1Bioengineering, Cardiology, Univ of Colorado; Children’s Hosp Colorado, Aurora, CO
- 2Endocrinology, Children’s Hosp Colorado, Aurora, CO
- 3Bioengineering, Univ of Colorado, Aurora, CO
- 4Radiology, Northwestern Univ, Chicago, IL
- 5Cardiology, Children’s Hosp Colorado, Aurora, CO
Abstract 13741: Neurologic Injury and Cerebral Blood Flow In Single Ventricles Throughout Staged Surgical Reconstruction
Mark A Fogel, Tom Pawlowski, Christine Li, Peter Schwab, Felice Wilson, Susan Nicolson, Lisa Montenegro, Laura Diaz-Berenstein, Thomas Spray, J William Gaynor, Stephanie Fuller, Christopher Mascio, Marc keller, Matthew Harris, Kevin K Whitehead, Okan Elci, James Bethel, Daniel Licht, Arastoo Vossough
Circulation. 2016;134:A13741
Abstract
Introduction: Single ventricle pts experience a high rate of brain injury and adverse neurodevelopmental outcome.
Hypothesis: The incidence of brain abnormalities is different at various surgical stages and is linked with cerebral blood flow (CBF), oxygen delivery and carbon dioxide reactivity.
Methods: Single ventricle pts were studied with MRI scans immediately prior to bidirectional Glenn (pre-BDG), prior to Fontan and then 3-9 months after Fontan reconstruction.
Results: 168 consecutive subjects recruited into the project underwent 235 scans: 63 pre-BDG (4.8±1.7 months), 118 BDG (2.9±1.4 years) and 54 after Fontan (3.4±1.1 years). Non-acute ischemic white matter changes on T2 weighted imaging, focal tissue loss, punctate microbleeds and ventriculomegaly were all more commonly detected in BDG and Fontans compared to pre-BDG (see figure); punctate microbleeds were also more common in Fontan than pre-BDG (P<0.05). CBF was higher in BDG than Fontan and almost reached statistical significance versus pre-BDG (see graph). The odds of discovering brain injury adjusting for surgical stage as well as 2 or more co-existing lesions within a patient all decreased (63-97% and 44% respectively) with increasing amount of CBF (P<0.05). In general, there was no association of oxygen delivery or carbon dioxide reactivity with neurological injury.
Conclusion: Significant brain abnormalities are commonly present in single ventricle pts and detection of these lesions increase as children progress through staged surgical reconstruction with multiple co-existing lesions more common earlier than later. Cumulative exposures to surgery may account for increased incidence, though changes in brain maturation may increase detection of white matter injury. In addition, an inverse association of various indices of CBF with these brain lesions is present (CBF highest in BDG stage), however, CO2 reactivity, oxygen delivery were not associated with brain lesion development.
Article Information
vol. 134 no. Suppl 1 A13741
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Mark A Fogel1;
- Tom Pawlowski1;
- Christine Li1;
- Peter Schwab1;
- Felice Wilson1;
- Susan Nicolson1;
- Lisa Montenegro1;
- Laura Diaz-Berenstein1;
- Thomas Spray1;
- J William Gaynor1;
- Stephanie Fuller1;
- Christopher Mascio1;
- Marc keller1;
- Matthew Harris1;
- Kevin K Whitehead1;
- Okan Elci2;
- James Bethel2;
- Daniel Licht1;
- Arastoo Vossough1
- 1PEDIATRIC CARDIOLOGY, Childrens Hosp Philadelphia, Philadelphia, PA
- 2Statistics, Westat, Rockville, MD
Abstract 13145: Ventriculoarterial Coupling Ratio is Associated With Adverse Outcomes in Repaired Tetralogy of Fallot
Max E Godfrey, Tal Geva, Lynn A Sleeper, Minmin Lu, Anne Marie Valente, Ashwin Prakash
Circulation. 2016;134:A13145
Abstract
Introduction: Patients with repaired tetralogy of Fallot (TOF) are at risk of premature death and ventricular arrhythmias. The ventriculoarterial coupling (VAC) ratio, the ratio of arterial elastance (Ea) and ventricular end-systolic elastance (Ees), is a measure of cardiac efficiency. Little is known about the VAC ratio in this population. We used a previously described cardiac magnetic resonance (CMR) method to measure right and left VAC ratios in patients with repaired TOF, and assessed the hypothesis that this is related to outcomes.
Methods and Results: We measured VAC from CMR data at a single institution on 593 TOF patients (age 21.5 ± 14.4 years) and 58 controls (age 13.2 ± 4.0 years). Frequency matching based on age and gender yielded 326 TOF patients to compare with controls. VAC ratio was calculated for both right (RV) and left (LV) ventricles as Ea/Ees = end-systolic volume/stroke volume. TOF patients had higher RV and LV VAC ratios (p<0.001) (RV results, figure A). Within the TOF cohort, RV VAC ratio correlated positively with LV VAC (r=0.43, p<0.001), but not with pulmonary regurgitation fraction. After a median follow-up of 5.0 (IQR 2.4-8.5) years, 26 patients (4.4%) reached a composite endpoint of death (n=16), aborted sudden cardiac death (n=5), or sustained ventricular tachycardia (VT, n=5). An RV VAC ratio in the highest tertile (T3) was associated with higher risk of the outcome (p<0.001, figure B). Controlling for known risk factors (RV mass-to-volume ratio, atrial arrhythmia and non-sustained VT), an RV VAC ratio ≥1.11 (highest tertile) was independently associated with the composite outcome (hazard ratio 7.3, 95% CI 2.7-19.9, p<0.001).
Conclusion: In this cohort, TOF patients demonstrated inefficient VAC as compared with controls. A higher RV VAC ratio was independently associated with the composite outcome of death, aborted sudden cardiac death, or sustained VT. Further investigation of the significance of VAC in this population is warranted.
Article Information
vol. 134 no. Suppl 1 A13145
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Max E Godfrey;
- Tal Geva;
- Lynn A Sleeper;
- Minmin Lu;
- Anne Marie Valente;
- Ashwin Prakash
- Cardiology, Boston Children’s Hosp, Boston, MA
Abstract 20308: Impact of Standardized Clinical Assessment and Management Plans on Resource Utilization in Children With Aortic Regurgitation
Rahul H Rathod, Brittney Jurgen, Lynn A Sleeper, Minmin Lu, Kevin G Friedman, James E Lock, Steven D Colan
Circulation. 2016;134:A20308
Abstract
Introduction: Standardized Clinical Assessment and Management Plans (SCAMPs) are a quality improvement initiative designed to reduce unnecessary utilization, decrease practice variation and improve patient (pt) outcomes. The Aortic Regurgitation (AR) SCAMP algorithms focused on the outpatient management of patients with isolated AR. Using multiple longitudinal encounters, we sought to assess the impact of the AR SCAMP on total costs compared to a historical control cohort.
Methods: All AR SCAMP pts (enrollment dates 9/09-7/15) were compared to a historical control group (1/01-8/09). Pts ≥ 2 yrs old were included in the analysis. A SCAMP managed episode of care (SMEOC) was defined as 3 years in length. Utilization during a SMEOC included all cardiology visits, diagnostic tests, and procedures. Standardized costs were applied to each unit of utilization.
Results: There were 88 SCAMP and 80 historical pts. There was no significant difference in the frequency of pts with ≥ moderate AR (p=0.09). Resource utilization by cohort is shown in the table. SCAMPs reduced average outpatient clinic visits by 34%, chest radiographs by 57%, and echocardiograms by 32%. Similar savings were realized in outpatient clinic visits and echocardiograms when dichotomized by patients with ≥ moderate AR. There was no difference in number of deaths or surgeries between the historical and SCAMP cohorts. Including all expenditures, the AR SCAMP reduced utilization by 34% and saved $338,865 during the first 6 years of the SCAMP.
Conclusions: SCAMPs can reduce resource utilization and costs in pts with AR without affecting outcomes.
Article Information
vol. 134 no. Suppl 1 A20308
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Rahul H Rathod;
- Brittney Jurgen;
- Lynn A Sleeper;
- Minmin Lu;
- Kevin G Friedman;
- James E Lock;
- Steven D Colan
- Dept of Cardiology, Boston Children’s Hosp, Boston, MA
Abstract 18605: Long-Term Cardiac Follow-up of Patients With Severe Congenital Heart Disease: Are Care Gaps Associaed With an Increased Probability of Mortality
Eva Goossens, Aihua Liu, Liming Guo, Sarah Cohen, Judith Therrien, Philip Moons, Ariane Marelli
Circulation. 2016;134:A18605
Abstract
Introduction: The ACC/AHA 2008 guidelines for adults with congenital heart disease (CHD) recommend follow-up in patients with severe CHD at specialized centers every 6-12 months. Care gaps, however, are prevalent in adolescents transitioning to adulthood. Studies investigating CHD surveillance in adults are currently lacking. Furthermore, an assessment of the impact of care gaps on mortality is lacking. We investigated CHD outpatient visit rates in patients with severe CHD aged 12-65y. The probability of mortality was assessed in 3 groups (i.e., lost to follow-up, care gaps, surveillance at least yearly) stratified by age. We hypothesized that care gaps are most prevalent in adolescents and that patients with no or discontinued care, have an increased probability of mortality.
Methods: A cohort study was performed on the Québec CHD database. Patients with severe CHD, 12-65y between 2001-2010, were selected (n=4,713). The mean number of CHD outpatient visits was calculated. Based on this number, patients were subdivided in 3 groups stratified by age. Group1 represented patients without outpatient CHD visits (i.e., lost to follow-up). Group2 comprised patients who had CHD visits less than annually (i.e., care gaps). Finally, patients who had cardiac surveillance visits at least yearly were in line with recommendations.
Results: The proportion of patients lost to follow-up increased significantly with age (χ2=50.769; p<0.001). Care gaps were most prevalent in patients aged 25-40y. Mortality risks for group 1,2 and 3 were 0.33%, 0.74% and 0.68% in patients aged 12-24y; 0.90%, 0.53% and 1.65% for 25-40y; and 3.59%; 0.56%, 3.17% for 41-65y. The mortality risk did not differ significantly across groups.
Conclusions: Care gaps were most prevalent in adults (25-40y). Increased probability of mortality in patients with discontinued care was not demonstrated. Additional analyses are required to investigate if groups differ in service seeking behaviors and comorbidities.
Article Information
vol. 134 no. Suppl 1 A18605
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Eva Goossens1;
- Aihua Liu2;
- Liming Guo2;
- Sarah Cohen2;
- Judith Therrien2;
- Philip Moons1;
- Ariane Marelli2
- 1Dept of Public Health and Primary Care, KU Leuven- Univ of Leuven, Leuven, Belgium
- 2Dept of Medicine, Div of Cardiology, McGill Univ Health Cntr, Montréal, Canada
Abstract 18856: Patients With Mild Congenital Heart Disease Lesions Are at High Risk of Infective Endocarditis: A UK Tertiary Centre Experience
Athanasios Koutsoukis, Rhian Lakhani, Natali Chung, Yaso Emmanuel, Christoph Kiesewetter, Cathy Head, Bernard Prendergast, John Chambers, David Anderson, Conal Austin, Alessandra Frigiola
Circulation. 2016;134:A18856
Abstract
Introduction: Infective Endocarditis (IE) is a serious complication in patients with congenital heart disease (CHD). This study reviews the characteristics of patients with IE and CHD presenting to a UK tertiary centre, from 2008 when the new NICE guidelines on antibiotic prophylaxis were applied
Methods: All cases of IE in patients with CHD presented at St Thomas’ and Evelina Hospital between 2008 and 2015 were retrieved. Using the NICOR database and our electronic record, we reviewed: type of CHD, site of IE, presence of prosthetic material, recent dental procedure or other interventions, antibiotic prophylaxis, microbiology, echocardiographic features, treatment and outcome
Results: 65 cases of Ιε were identified (mean age 17 years, range 1 month -52 years, 46 male). Patients with complex cyanotic CHD were the most affected (35%) followed by patients with unrepaired ventricular septal defect (22%), and bicuspid aortic valve (12%). Fifty patients had signs of endocarditis on echocardiography. Native valves were most commonly affected (n=40) with the aortic valve/root in 45% of patients, followed by tricuspid valve (30%), mitral valve (30%) and pulmonary valve (5%); 4 patients had more than one valve involved. In patients with prosthetic material (n=20), RV-PA conduit was mostly affected (58.5%), followed by aortic stent/graft for aortic coarctation (21%), prosthetic aortic valve 10.5%, BT shunt 5% and PDA stent (5%). 10 patients had a dental procedure within 3 months prior to the IE, whereas 16 patients had other type of invasive procedures. Streptococcus species was the most frequent organism (n=29, 45%) followed by Staphylococcus in 13 cases (20%). Surgery was required in 66% of cases during the same admission. In-hospital mortality was 6.1%.
Conclusions: IE in patients with CHD is associated with high hospital mortality and often requires surgery during the same hospital admission. Patients with complex cyanotic CHD are known to be at high risk of developing IE and this is confirmed by our study; however patients with “mild” CHD lesions are also at high risk. These results would suggest the need to review the current NICE guidelines which should further consider the effect of flow dynamics in the pathogenesis of IE.
Article Information
vol. 134 no. Suppl 1 A18856
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Athanasios Koutsoukis1;
- Rhian Lakhani1;
- Natali Chung1;
- Yaso Emmanuel1;
- Christoph Kiesewetter1;
- Cathy Head2;
- Bernard Prendergast2;
- John Chambers1;
- David Anderson2;
- Conal Austin2;
- Alessandra Frigiola2
- 1Dept of Cardiology, Guy’s and St Thomas’ Hosp ,NHS Foundation Trust, London, United Kingdom
- 2Cardiovascular Dept, Guy’s and St Thomas’ Hosp ,NHS Foundation Trust, London, United Kingdom
Abstract 15203: Long Term Survival After Surgical or Transcatheter Interventions for Congenital Heart Disease (CHD): A Study From the Pediatric Cardiac Care Consortium (PCCC)
Lazaros Kochilas, Jeremiah Menk, Jeffrey M Vinocur, Brian Harvey, Matthew Oster, James St Louis, Logan Spector
Circulation. 2016;134:A15203
Abstract
Introduction: We aim to study long term survival in the cohort registered in the PCCC after surviving interventions for CHD between 1982 and 2003. The PCCC is the longest standing registry of outcomes for pediatric cardiac interventions in the world containing data from surgical and trans-catheter procedures from 48 centers in 27 U.S. states.
Methods: We linked the PCCC dataset with the National Death Index (NDI) using direct identifiers to determine long term vital status of individuals with repaired or palliated CHD. The identifiers included first name (when available), middle name (when available), last name, birth date, state of last residence, and sex. A total of 54,667 subjects (47.6% female) were registered prior to April 15, 2003 (date of implementation of stricter HIPAA rules) in the PCCC as survivors after undergoing an intervention for CHD and were submitted for linkage with the NDI. The standardized mortality ratio and one-sample log-rank test were computed by matching age, sex, and year to mortality tables from the Centers for Disease Control and Prevention (CDC WONDER data). A Kaplan Meier (KM) plot was created for the PCCC cohort along with survival curves for the standard population.
Results: A total of 4,690 deaths (8.6%) were identified after the last PCCC contact (median follow-up: 17.0 years [range: 1 day – 33.0 years]) vs 736 expected (1.3%). The standardized mortality ratio was 6.37 (95% CI: 6.17-6.59, p<0.001) (Figure A). Females had a higher mortality ratio compared to the general population, 6.78 (95% CI: 6.44-7.13) versus 6.12 for males (95% CI: 5.86-6.39) (Figure B).
Conclusions: Survivors with repaired or palliated congenital heart disease have a significantly higher mortality ratio than the general population. Additional in depth analysis of risk factors for long term outcomes and causes of death by group of conditions and specific diagnoses is underway.
Article Information
vol. 134 no. Suppl 1 A15203
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Lazaros Kochilas1;
- Jeremiah Menk2;
- Jeffrey M Vinocur4;
- Brian Harvey5;
- Matthew Oster1;
- James St Louis6;
- Logan Spector5
- 1Pediatrics, Emory Univ, Atlanta, GA
- 2Biostatistical Design and Analysis Cntr (BDAC), Univ of Minnesota, Minneapolis, MN
- 3Bdac, Univ of Minnesota, Minneapolis, MN
- 4Pediatrics, Univ of Rochester, Rochester, NY
- 5Pediatrics, Univ of Minnesota, Minneapolis, MN
- 6Surgery, Univ of Missouri-Kansas City Sch of Medicine, Kansas City, MO
Abstract 15137: Association of Congenital Heart Defects With Childhood Cancer in Privately Insured US Children: A Rapid Claims Analysis
Matthew Oster, April Dawson, Cynthia Wetmore, Scott Grosse
Circulation. 2016;134:A15137
Abstract
Background: As treatment for congenital heart defects (CHDs) has improved, understanding the long-term outcomes of survivors has become important. Recent studies have focused on the risk of adult-onset cancer in CHD survivors, but little is known about the incidence of childhood cancer in this population. Our objective was to determine the association of CHDs with childhood cancer using a nationwide administrative healthcare database of more than 100 million Americans.
Methods: Using the Treatment Pathways online analytic interface to access the Truven Health MarketScan® research databases, we examined the presence of ICD-9 diagnosis codes for neoplasm during 2009-2015 among 6.1 million children <18 years of age not coded for Down syndrome, continuously enrolled in employer-sponsored plans during 2014. To avoid overestimating the risk of cancer in CHD survivors, only those children with ≥1 CHD code during 2009-2014 ≥30 days prior to the first neoplasm code were considered to be CHD survivors with cancer. We calculated risk ratios and 95% confidence intervals using Taylor series variance approximation. Findings were confirmed with a sensitivity analysis limited to children with ≥2 outpatient CHD codes or ≥1 inpatient CHD code.
Results: There were 346 neoplasms identified among 88,493 children with CHDs (3.91/1000) and 4793 neoplasms among 6,040,429 children without CHDs (0.79/1000). Compared to those without CHDs, the risk ratio for the development of any neoplasm in those with CHDs was 4.9 (95% confidence interval [CI] 4.4-5.5) in the primary analysis and 6.4 (95% CI 5.7-7.2) in the sensitivity analysis. The risk was greatest for the development of bone tumors and neuroblastoma. (Figure)
Conclusions: Children with CHDs are at increased risk of developing neoplasms during childhood. Further investigations are needed to determine whether this association may be related to inherent factors (such as common biologic predisposition) or environmental factors.
Article Information
vol. 134 no. Suppl 1 A15137
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Sibley Heart Cntr Cardiology, Children’s Healthcare of Atlanta, Atlanta, GA
- 2National Cntr on Birth Defects and Developmental Disabilities, US Cntrs for Disease Control and Prevention, Atlanta, GA
- 3Aflac Cancer and Blood Disorders Cntr, Children’s Healthcare of Atlanta, Atlanta, GA
Abstract 14498: Variability in Practice Patterns and Consistency With Published Guidelines for Aortic and Pulmonary Balloon Valvuloplasty: An Analysis of Data From the IMPACT Registry
Andrew C Glatz, Michael L O’Byrne, Kevin F Kennedy, Jonathan J Rome
Circulation. 2016;134:A14498
Abstract
Introduction: Potential measures of quality in practice are its variability and consistency with published guidelines. We sought to assess, for the first time, these measures in congenital cardiac catheterization for aortic (AV) and pulmonary valvuloplasty (PV) procedures using the IMPACT Registry.
Methods: All procedures for isolated AV and PV between 1/11 and 9/15 were obtained from the IMPACT Registry. Hierarchical regression modeling was used to assess center-level differences in intervention indications, adjusted for patient- and procedure-level factors. Further, for cases >30 days of age with “high resting gradient” as the indication, consistency with the 2011 AHA Scientific Statement (pre-intervention gradient ≥40 mmHg and, for AS, pre-intervention aortic insufficiency <4+) was assessed, again adjusted for patient and procedure-level factors.
Results: The cohort consisted of 1071 AV procedures from 60 centers and 2207 PV procedures from 75 centers. For AV, indication was “high resting gradient” in 82%, “LV dysfunction” in 11%, “symptoms” in 5%, and “abnormal stress test/EKG” in 2%. For PV, indication was “high resting gradient” in 82%, “RV dysfunction” in 9%, “right to left shunting” in 6%, and “symptoms” in 5%. There were no center-level differences in the adjusted distribution of indications for either procedure. 86% of AV (IQR 78-100% per center) and 66% of PV (IQR 50-82% per center) done for “gradient” were consistent with guidelines. For AV, there were significant adjusted differences in consistency based on geographic region, with equivalent consistency in the Northeast and South, both significantly more consistent than the Midwest and West (overall p=0.005). For PV, there were significant adjusted individual center differences in consistency [median rate ratio=1.42 (95% CI 1.2 – 1.6), p<0.001], with pre-intervention gradient <40 mmHg in >50% of cases at 22% of centers.
Conclusions: Overall, there is more consistency with published guidelines for the practice of AV than for PV. For AV, consistency varies significantly across geographic regions. For PV, consistency varies significantly between centers. This suggests that similar patients are treated differently based on center factors and may have implications for quality of care.
Article Information
vol. 134 no. Suppl 1 A14498
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Div of Cardiology, The Children’s Hosp of Philadelphia, Philadelphia, PA
- 2Cardiology, Children’s National Med Cntr, Washington, DC
- 3CV Rsch, Mid America Heart Institute, Kansas City, MO
Abstract 13990: Early Clinical Experience of Trans-Catheter Closure of Patent Ductus Arteriosus in Extremely Premature Neonates
Ranjit Philip, Kaitlin Balduf, Kristin Washington, Sandeep Chilakala, Alejandro Arevalo, Thomas Fagan, B. Rush Waller, Shyam Sathanandam
Circulation. 2016;134:A13990
Abstract
Introduction: Children born prematurely often have a patent ductus arteriosus (PDA). Surgical ligation of the PDA is standard when pharmacologic therapy fails. Trans-catheter closure of PDA (TCCPDA) in premature neonates is a relatively new technique.
Hypothesis: To describe our early clinical experience of TCCPDA in premature neonates who require positive pressure ventilation (PPV) and to identify risk factors for poor respiratory outcomes.
Methods: A retrospective review was performed. A respiratory severity score (RSS) was calculated for all patients. The change in the RSS post-procedure and the time taken for return to pre-procedure RSS were used as outcome variables. Patients with pulmonary artery systolic pressure >50% of the systolic blood pressure were considered to have pulmonary hypertension (PHT).
Results: Thirty premature neonates (25.7±2.8 weeks’ gestation, birth weight=756±284 g) that were PPV dependent with or without PHT were referred for TCCPDA at 55.5±32.2 days of age, weighing 1.67±0.54 Kg. Procedures were performed using only femoral venous access under echo and fluoroscopic guidance. The device used for closure included the 4mm Amplatzer Vascular Plug-II (AVP-II) in 10, 6 mm AVP-II in 10, 8mm AVP-II in 3, 4mm AVP-4 in 1 and MVP-5Q device in 6 patients. The procedure and fluoroscopic times were 83.7±56.8 and 12.8±11.6 minutes respectively. The radiation and contrast doses were 52.8±34.2 mGy and 2.8±1.5 mL/Kg respectively. The baseline RSS and QP:QS ratio were 3.9±3.3 and 2.2±0.8 respectively. The presence of PHT was the only predictor for a longer time to return to pre-procedure RSS (18 vs. 87 hours; OR=5.4, 95% CI:2.2-9.4, P<0.001) with a 68.8±32.6% increase in RSS (P<0.01). There was one procedure-related mortality. One patient, weighing1.06 Kg, developed left pulmonary artery stenosis following device closure. The device embolized in another patient 6 hours post-procedure. Both these devices were snared and retrieved. No other complications were noted during the procedure or on follow-up (mean 1.8 ± 0.8 years). No patients had residual PDA on follow-up echocardiogram.
Conclusions: It is feasible to perform trans-catheter closure of PDAs in premature neonates. Presence of PHT prolongs the need for PPV after PDA closure.
Article Information
vol. 134 no. Suppl 1 A13990
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Ranjit Philip1;
- Kaitlin Balduf1;
- Kristin Washington2;
- Sandeep Chilakala1;
- Alejandro Arevalo1;
- Thomas Fagan1;
- B. Rush Waller1;
- Shyam Sathanandam1
- 1Pediatric Cardiology, Univ of Tennessee, Memphis, TN
- 2Pediatric Cardiology, Le Bonheur Children’s Hosp, Memphis, TN
Abstract 18175: Predicting Low-grade Rejection After Heart Transplantation In Children Using Whole Genome Sequencing
William Y Shi, Annie Xin, Gordon K Smyth, Yifang Hu, Slavica Praporski, Anne Shipp, Robert G Weintraub, Igor E Konstantinov
Circulation. 2016;134:A18175
Abstract
Introduction: Endomyocardial biopsy (EMB) remains the gold standard for detecting rejection after heart transplantation. EMB is costly, invasive and, particularly, burdensome in children. We aimed to predict low-grade rejection by whole genome sequencing (WGS) in blood sample.
Hypothesis: WGS can predict low-grade rejection in children after heart transplantation.
Methods: A total of 106 blood samples with corresponding EMB from 18 children who underwent heart transplantation from 2011 to 2014 were analysed. There were 18 baseline preoperative samples and 88 samples taken at the time of each EMB. Grade of rejection corresponding to each blood sample was determined (no rejection, n=34, 1R, n=45, and 2R, n=9). An input of 200 ng of total RNA per sample was prepared and indexed separately for Illumina sequencing using the TruSeq RNA Library Prep Kit v2 (Illumina, San Diego, CA). Next generation WGS was performed. Differential expression (DE) analysis was performed using the limma package. A k-nearest neighbor prediction method was used.
Results: The mean age at transplantation was 10.3 years (median 12 years, range: 4 months -17.5 years). Preoperative interpersonal variances in gene expression were negated by post-transplantation immunosuppression. Using the top 3 DE genes (ATP1A1, CD8B, MKS1) in low-grade rejection (0 vs 1R), 68 correct predictions of 79 samples were determined. A scatterplot with the log2-counts-per-million expression values for these 3 genes is shown in Figure 1. Drop-one-out cross validation determined a correct prediction rate of 88% (30/34) for no rejection (Grade 0) and 84% (38/45) for the rejection (Grade 1R). Prediction of grade 2R was not feasible due to small number of samples.
Conclusions: Early grade of allograft rejection after heart transplantation in children can be predicted in blood using genomic approach despite wide age range.
Article Information
vol. 134 no. Suppl 1 A18175
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- William Y Shi1;
- Annie Xin1;
- Gordon K Smyth2;
- Yifang Hu2;
- Slavica Praporski1;
- Anne Shipp1;
- Robert G Weintraub3;
- Igor E Konstantinov1
- 1Cardiac Surgery, Royal Children’s Hosp, Parkville, Australia
- 2Bioinformatics, WEHI, Parkville, Australia
- 3Cardiology, Royal Children’s Hosp, Parkville, Australia
Abstract 17362: New-onset Diabetes After Pediatric Heart Transplantation
Joshua D Sparks, Elizabeth P Pruitt, James K Kirklin, Tricia Brown, Michael P Carboni, William J Dreyer, Steven Kindel, Thomas D Ryan, Robert Morrow
Circulation. 2016;134:A17362
Abstract
Introduction: New-onset Diabetes after Transplantation (NDT) is a well defined complication after solid organ transplantation. Little has been published describing the incidence, risk factors, and effect on outcome after pediatric heart transplantation.
Hypothesis: Herein, we aim to describe the incidence and risk factors for the development of NDT.
Methods: We performed a retrospective cohort analysis of patients ≤ 18 years of age alive at 1 year post transplant from the Pediatric Heart Transplant Study event driven database from 2004 to 2014. Continuous variables were compared using Wilcoxon rank-sum and Chi squared analysis was were used for categorical variables. Kaplan-Meier method was used to assess survival and Log-rank method to compare curves. Logistic regression was used to identify independent risk factors.
Results: Of the 2163 recipients, 1767 were alive and followed at 1 year. The freedom from NDT was 98.32% (95CI 97.98% – 98.60%), 94.73% (95CI 94.04% – 95.35%), and 86.07% (95CI 83.21% – 88.52%) at 1, 5, and 10 years, respectively. Patients with NDT were more likely to be older at time of transplant (6.35 ± 6.04 vs. 12.32 ± 4.51, p<0.0001) with 60% over the age of 12, to be of non-white race (28.6% vs. 54.8%, p=0.0002), and to have an increased BMI at time of transplant (17.41 ± 4.60 vs. 21.65 ± 6.25, p<0.0001) with 32% having a BMI ≥ 25. On multivariable analysis, risk factors for NDT at one-year post transplant were black race [HR 2.36 (1.25 – 4.47), p=0.009], older age at transplant [HR 1.16 (1.09 – 1.24), p<0.0001], and BMI ≥ 25 at transplant [HR 2.5 (1.18 – 5.29, p=0.02].
Conclusion: Though uncommon, NDT occurs with a continuous hazard after pediatric heart transplant; more often in older patients at transplant, those who are of non-white race, and those with higher BMI (a potential modifiable risk factor). Therefore, targeted weight reduction in at risk populations could prevent NDT. Further data is needed to determine whether NDT alters the outcome after transplant.
Article Information
vol. 134 no. Suppl 1 A17362
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Joshua D Sparks1;
- Elizabeth P Pruitt2;
- James K Kirklin3;
- Tricia Brown1;
- Michael P Carboni4;
- William J Dreyer5;
- Steven Kindel6;
- Thomas D Ryan7;
- Robert Morrow8
- 1Pediatrics, Univ of Louisville Sch of Medicine, Louisville, KY
- 2Pediatrics, Univ of Alabama Birmingham, Birmingham, AL
- 3Surgery, Univ of Alabama Birmingham, Birmingham, AL
- 4Pediatrics Cardiology, Duke Univ Med Ctr, Durham, NC
- 5Pediatrics, Baylor College of Med, Houston, TX
- 6Pediatrics, Children’s Hosp of Winsconsin, Milwaukee, WI
- 7Pediatrics, Univ of Cincinnati, Cincinnati, OH
- 8Pediatrics, Children’s Hosp Dallas, Dallas, TX
Abstract 16712: Calcineurin Inhibitor-free Regimens in Pediatric Heart Transplant Recipients – Outcomes of Empiric Transition to Sirolimus
Adam Putschoegl, Dahl Sonja, David Driscoll, Patrick O’Leary, Carl Cramer, Richard Daly, Sudhir Kushwaha, Jonathan Johnson
Circulation. 2016;134:A16712
Abstract
Introduction: Mammalian Target of Rapamycin (mTOR) inhibitors including sirolimus have been successfully used in adult heart transplant patients (pts) to attenuate graft arterial vasculopathy (CAV) and calcineurin inhibitor (CNI) nephrotoxicity. Of interest in pediatric pts is the potential offered by mTOR inhibitors to decrease morbidity related to CAV, CNI related nephrotoxicity and PTLD. Here, we report our updated experience with transition to sirolimus in a CNI-free regimen in pediatric heart transplant pts.
Materials and Methods: We retrospectively reviewed all pediatric heart transplant pts with attempted transition from a CNI to a sirolimus regimen. Patients were also treated routinely with an anti-metabolite medication with or without steroids.
Results and Discussion: We identified 31 pts (mean age at transplant 8.3 years, 55% male) for whom transition was attempted. Transition trials occurred a mean of 30 months post-transplant. Eight pts discontinued sirolimus due to side effects (pneumonitis, aphthous ulcers, diarrhea or proteinuria). All pts with a history of Fontan and protein losing enteropathy (PLE, N = 3) developed significant proteinuria while on sirolimus, requiring discontinuation. Twenty-three of 31 pts (mean age at transplant 7.6 years, 65% male) successfully completed transition to a CNI-free protocol, over a mean of 71 days. Follow-up was available for a mean of 4.3 years post-conversion. No pts were diagnosed with CAV during this short-term follow-up. There was no significant difference between the rate of rejection while taking CNIs (prior to transition) relative to the rate when on the CNI-free regimen (p = NS). Glomerular filtration rate (mL/min/1.73m2) increased from 79 pre-transition to 89 post-transition and further to 94 at latest follow-up. However, this trend did not reach statistical significance.
Conclusion: In this cohort of pediatric heart transplant pts, a sirolimus-based, CNI-free immunosuppressive regimen was not associated with increased rejection rate. All pts with PLE before transplant developed proteinuria on sirolimus. Transition to sirolimus in a CNI-free regimen for pediatric heart transplant pts was effective in most and has the potential to improve graft and patient survival.
Article Information
vol. 134 no. Suppl 1 A16712
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Adam Putschoegl1;
- Dahl Sonja1;
- David Driscoll1;
- Patrick O’Leary1;
- Carl Cramer2;
- Richard Daly3;
- Sudhir Kushwaha4;
- Jonathan Johnson1
- 1Pediatric Cardiology, Mayo Clinic, Rochester, MN
- 2Pediatric Nephrology, Mayo Clinic, Rochester, MN
- 3Cardiovascular Surgery, Mayo Clinic, Rochester, MN
- 4Cardiovascular Diseases, Mayo Clinic, Rochester, MN
Abstract 15207: Predicting Tacrolimus Concentrations in Heart Transplant Recipients Using Population Pharmacokinetic Models
Kimberly Molina, Joseph Rower, Chris Stockmann, Catherine Sherwin
Circulation. 2016;134:A15207
Abstract
Background: Tacrolimus (TAC) promotes graft longevity in heart transplant recipients, yet is associated with large inter-patient variability that necessitates frequent drug monitoring. We hypothesized that a population pharmacokinetic (popPK) model could be used to generate accurate predictions of TAC concentrations in a population of pediatric heart transplant recipients.
Methods: Children receiving TAC during the first 6 weeks after heart transplant at Primary Children’s Hospital from 2007-2015 were studied. Demographics, dosing, and TAC concentrations were utilized to develop a one-compartment popPK model using NONMEM v7.3. Data from 1/2007-12/2013 were used for model development. Data from 1/2014-12/2015 were used for model validation.
Results: Thirty children with a median age of 5.7 yrs (range: 0.1-17.7) had 395 TAC troughs obtained (median: 12 per child). The median (range) observed TAC concentration was 12.7 (1.5-32.7) μg/L. Of the 275 samples collected at steady-state (>96 hours after 1st dose), 39% were within the target therapeutic range (12-16 μg/L), while 41% were <12 μg/L. The popPK model identified a positive correlation between age and volume of distribution (p<0.001). Individual parameter estimates were used to calculate a mean (%CV) half-life of 20.6 (63%) hours, consistent with prior PK studies in pediatric liver transplant recipients. Large inter-patient variability in the elimination rate (56%) was observed. Model validation revealed no evidence of bias (median prediction error (MPE): 0.36% [95% CI: -0.33, 1.21]) and high accuracy (median absolute prediction error (MAPE): 3.8% [95% CI: 3.2, 4.9]). Individual parameter estimates determined from ≥3 concentrations predicted future concentrations with a small positive bias (MPE: 13.8% [95% CI: 3.0, 23.7]) and acceptable accuracy (MAPE: 37.0% [95% CI: 31.7, 40.6]).
Conclusion: PopPK modeling is a valuable tool for generating reasonably unbiased and accurate predictions of TAC concentrations in pediatric heart transplant recipients. Prospective clinical validation is warranted to determine whether the use of a popPK model can effectively keep children within the target therapeutic range and reduce the need for frequent TAC monitoring.
Article Information
vol. 134 no. Suppl 1 A15207
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Pediatric Cardiology, Univ of Utah, Salt Lake City, UT
- 2Clinical pharmacology, Univ of Utah, Salt Lake City, UT
- 3Clinical Pharmacology, Univ of Utah, Salt Lake City, UT
Abstract 14552: The Impact of the PediMACS Score on Pediatric Heart Transplant Survival: A 25 Year Experience
Sarah J Wilkens, Alaa Aljiffry, Bradley S Marino, Zhi Li, Adin C Andrei, Michael C Monge, John M Costello, Elfriede Pahl
Circulation. 2016;134:A14552
Abstract
Background: The Pediatric Interagency Registry for Mechanical Circulatory Support (PediMACS) profile has not been applied to pediatric heart transplant (HTx) patients to predict post-operative outcomes. We sought to assess the predictive value of the PediMACS profile at listing on early and late post-operative morbidity and mortality in pediatric HTx patients.
Methods: This is a retrospective cohort study of 217 patients at our center who received an initial heart transplant between May 1989 and December 2014. PediMACS profiles were assigned at listing by 2 cardiologists during data collection. Data were collected at 1 month, 1 year, and 5 years post-HTx to assess early and late morbidity and mortality. Statistical modeling included Cox Regression analysis and Kaplan Meier survival curves.
Results: At listing, PediMACS profiles were as follows: 1 (n=75, 35%); 2 (n=26, 12%); 3 (n=78, 36%); and 4-6 (n=38, 17%). Heart disease etiology prior to HTx were cardiomyopathy (n=129, 59%) and congenital heart disease (n=88, 41%). The mortality rates post-HTx were 6%, 11% and 32% at 1 month, 1 year, and 5 years, respectively. The PediMACS profile at listing was associated with early mortality. Profiles 1-2, those most seriously ill, had an increased rate of mortality compared to profiles 3-6, those more stable (1-2: 9%; 3-6: 3%; p=0.04). Profiles 1-2 had higher rates of post-operative dialysis (1-2: 15%; 3-6: 4%; p=0.003). At 1 month post-HTx, profiles 1-2 were more likely to require respiratory support (1-2: 29%; 3-6: 12%; p=0.001), and sedation (1-2: 19%; 3-6= 5%; p=0.002), and were less likely to be discharged from the hospital (1-2: 49%; 3-6: 19%; p=<0.001). Long-term mortality was not influenced by the PediMACS profile at listing (Figure).
Conclusion: A lower PediMACS profile assigned at listing was associated with increased mortality and resource utilization early after HTx. However, long-term mortality was not associated with PediMACS profiles assigned prior to HTx.
Article Information
vol. 134 no. Suppl 1 A14552
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Sarah J Wilkens1;
- Alaa Aljiffry1;
- Bradley S Marino1;
- Zhi Li2;
- Adin C Andrei2;
- Michael C Monge3;
- John M Costello1;
- Elfriede Pahl1
- 1Pediatric Cardiology, Ann & Robert H. Lurie Children’s Hosp of Chicago, Chicago, IL
- 2Bluhm Cardiovascular Institute, Northwestern Univ Feinberg Sch of Medicine, Chicago, IL
- 3Cardiovascular Thoracic Surgery, Ann & Robert H. Lurie Children’s Hosp of Chicago, Chicago, IL
Abstract 13110: Pediatric Heart Transplantation in Pre-Sensitized Recipients: A Current Perspective
Bibhuti Das, Elizabeth Pruitt, Kimberly Molina, William Ravekes, Scott Auerbach, Andrew Savage, Leah Knox, James Kirklin, David Naftel, Daphne Hsu
Circulation. 2016;134:A13110
Abstract
Introduction: Anti-HLA antibodies (Ab) are increasingly prevalent in pediatric patients (pts) awaiting heart transplant (HT) and may result in a significant delay in time to HT because of the need to wait for a negative prospective donor HLA crossmatch (XM).
Methods: Data from pts in the Pediatric HT Study transplanted between 2010-2014 were analyzed to determine the association of pre-HT percent reactive anti-HLA Ab (PRA) detected by flow cytometry with retrospective donor XM results and outcomes after HT. Sensitization was defined as a PRA >20%.
Results: HT was performed in 1,596 pts, 1,459 had a PRA calculated and 1,419 had XM results available. Sensitization was present in 32% of pts; 25% were sensitized against Class I and 20% were sensitized against Class II Ab (p<0.01). Sensitization was more common in pts with congenital heart disease (CHD) compared to cardiomyopathy (CM), 28% vs. 15%, respectively, p<0.01). Sensitization was similar between pts with and without ventricular assist device support, 20% vs. 25%, respectively, p=0.07. The level of sensitization was significantly associated with a +XM (p<0.01, Table). Sensitized pts who had a +XM were at higher risk for rejection than those who had a – XM and those who were not sensitized (p<0.01, Figure). There was no difference in post-HT survival between sensitized and nonsensitized pts, p=0.11, or those with and without a +XM, p=0.06.
Conclusions: In the current era, 32% of pediatric HT pts are sensitized, with a higher incidence seen in pts with CHD compared to those with CM. Although, increasing PRA levels were associated with a higher likelihood of a positive retrospective XM, 68% of pts with a pre-HT PRA >50% had a negative XM. XM was positive in 9% of pts with a PRA between 1-20%. Sensitized pts with a positive XM had a higher incidence of rejection than all other pts. Better methods of identifying pts at risk for a positive XM are needed to refine the indications for a prospective XM in pediatric pts listed for HT.
Article Information
vol. 134 no. Suppl 1 A13110
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Bibhuti Das1;
- Elizabeth Pruitt2;
- Kimberly Molina3;
- William Ravekes4;
- Scott Auerbach5;
- Andrew Savage6;
- Leah Knox7;
- James Kirklin8;
- David Naftel9;
- Daphne Hsu10
- 1Pediatrics, Univ of Texas Southwestern Med Cntr, Dallas, TX
- 2Heart Cntr, Univ of Alabama at Brimingham, Brimingham, AL
- 3Pediatrics, Primary Children’s Hosp, Salt Lake City, UT
- 4Pediatrics, Johns Hopkin Hosps, Baltimore, MD
- 5Pediatrics, Children’s Hosp of Colorado, Aurora, CO
- 6Pediatrics, Med Univ of South Carolina, Charleston, SC
- 7Heart Cntr, Children’s Med Cntr Dallas, Dallas, TX
- 8Pediatric Surgery, Univ of Alabama at Brimingham, Brimingham, AL
- 9Heart Cntr, Univ of Alabama at Brimingham, Dallas, TX
- 10Pediatrics, The Children’s Hosp at Montefiore, Bronx, NY
Abstract 12609: Impaired Mitochondrial Respiration Precedes Clinical Heart Failure in Right Ventricular Pressure Overload
Nefthi Sandeep, Mingming Zhao, Donq-Qing Hu, Michael Coronado, Kristina B Kooiker, Giovanni Fajardo, Daniel Bernstein, Sushma Reddy
Circulation. 2016;134:A12609
Abstract
Introduction: Congenital heart disease patients with right-sided obstruction have increased stress on the right ventricle (RV) leading to right ventricular hypertrophy (RVH) and failure (RVF). The critical role of mitochondrial energetics in the development of RVH and RVF is not known. We hypothesize that mitochondrial dysfunction contributes to the chronic energy deficit and mechanical dysfunction in heart failure.
Methods: Adult, male FVB mice underwent pulmonary artery banding (PAB) to induce RVH (n=9) and RVF (n=4) and were compared to sham-operated controls (n=9). We used a high-resolution Oxygraph2K respirometer to measure oxygen consumption in tissue and in isolated mitochondria from the RV free wall. We evaluated leak respiration during substrate utilization by complex 1-NADH dehydrogenase and complex 2-succinate dehydrogenase and during maximal ATP generation by complex 5-ATP synthase. Groups were compared using ANOVA. Data is presented as mean ± SEM (*p<0.05).
Results: All mice had a PAB gradient of 30-40 mmHg by echocardiography. RVH mice had preserved systolic function while RVF mice had heart failure (ascites, tachypnea, hepatomegaly) and decreased function (Table). RVH showed preserved complex 1 mediated respiration but lower complex 2 and 5 respiration and lower respiratory control ratios (RCR) while in RVF, all complexes showed impaired respiration (Table). However, isolated mitochondria from RVF demonstrated preserved respiratory capacity when supplied with exogenous substrates and no change in complex levels.
Conclusion: Mitochondrial respiration is impaired even in stable RVH and progressively worsens in RVF in vivo. Interestingly, isolated mitochondria show normal respiration in RVF when supplied with substrates ex vivo suggesting a defect with substrate delivery rather than intrinsic mitochondrial function. Strategies to enhance substrate delivery may improve ATP generation and thereby preserve function in heart failure.
Article Information
vol. 134 no. Suppl 1 A12609
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Nefthi Sandeep;
- Mingming Zhao;
- Donq-Qing Hu;
- Michael Coronado;
- Kristina B Kooiker;
- Giovanni Fajardo;
- Daniel Bernstein;
- Sushma Reddy
- Cardiology, Lucile Packard Children’s Hosp Stanford, Palo Alto, CA
Abstract 20695: Junctional Ectopic Tachycardia in Recent Surgical Era : Clinical Epidemiology, Risk Factors & Outcomes
Sabikha Alam, Austin Kane, Kevin O Maher, Peter Fischbach, Shriprasad R Deshpande
Circulation. 2016;134:A20695
Abstract
Background: JET is common after congenital heart surgeries & has been associated with high mortality (up to 14%). We aim to report JET incidence, risk factors & outcomes in the current era.
Methods: Retrospective analysis of cardiac surgical patients less than 18 years of age over a six year period. When available, for each JET patient, two controls with similar lesions, repair type & no post operative arrhythmias were studied for pre, intra & post operative variables.
Results: We identified 104 patients with JET (incidence of 6 %). Majority of cases occurred after surgeries known as high risk for JET; VSDs including those with DORV , AVSD were the commonest lesions (35/104), followed by TOF (20/104) & TGA 11/104. Other cases occurred after surgeries that are not traditionally known to be associated with JET; TAPVC repair (3 cases with rate of 3 %), BT shunt (2 cases with rate of 1 %) & Fontan (1 case with rate of 2 %). Onset of JET was within first 24 hours after surgery in 74 % of patients, & lasted for less than 48 hours in the majority of cases. After multivariate logistic regression analysis, patient’s weight at time of surgery, less than 4 Kg [adjusted OR 3.97, 95% confidence interval (CI) 1.25-12.63], CPB duration > 100 min [adjusted OR 4.07; 95% CI 1.40-11.77], & postoperative lactic acid higher than 20 mg/dl (adjusted OR 5.64; 95% CI 1.88-16.93) were associated with an increased risk of JET. Amiodarone was the most commonly used specific therapy in JET ( 49/104), followed by procainamide in 14/104, esmolol 4/104, dexmedetomidine 14/104. Pacing (65/104) was an important adjuvant therapy. JET patients also had 3 times longer ICU stay, 3 times longer mechanical ventilation time & 1.5 times longer hospital stay therefore adding to significant healthcare cost burden. Overall, early mortality was very low (2/104) & comparable to patients without JET.
Conclusion: This is the largest cohort to date. Small patients with a long CPB time & high post-operative lactic acidosis are at high risk of developing JET with very significant morbidity & cost, but very low mortality. Future studies to assess efficacy of preventive measures in high risk patients are needed.
Article Information
vol. 134 no. Suppl 1 A20695
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Pediatrics, Emory Univ, Atlanta, GA
- 2Pediatric Cardiology, Emory Univ, Atlanta, GA
Abstract 20343: Usefulness of Echocardiography in Children and Adolescents With New Onset Supraventricular Tachycardia
Kaitlin L’Italien, Steven Conlon, Tami Ackley, Naomi Kertesz, Anna Kamp
Circulation. 2016;134:A20343
Abstract
Introduction: Supraventricular tachycardia (SVT) is the most common sustained arrhythmia in children. Patients with SVT and Wolff-Parkinson-White (WPW) are known to have 10-30% incidence of congenital heart disease (CHD). Infants without WPW who present with SVT under 1 year of age have a similar incidence of CHD. However, for children without WPW who present with SVT at older ages, the incidence of CHD is not known. This study aims to determine the incidence of CHD in older children and adolescents who present with SVT without WPW.
Methods: Children aged 5 to 18 years who presented to our institution with confirmed SVT between January 2011 and December 2015 were included in this retrospective review. Patients with any history of ventricular pre-excitation or pre-existing heart disease were excluded.
Results: There were 290 patients who met inclusion criteria. Echocardiograms were completed on 226 patients, and were included in the study. Only 3 patients had significant echocardiographic findings; 2 patients had systolic dysfunction, and 1 patient had an atrial septal defect. All 3 patients had abnormal physical exam or electrocardiogram (EKG) findings. No significant CHD was identified in any of the remaining patients. Minor anomalies were noted in 25 patients (11%), and included trivial to mild mitral valve regurgitation, mild tricuspid valve regurgitation, mild pulmonary valve regurgitation, trivial aortic insufficiency, left superior vena cava, small coronary fistula, abnormal aortic branching, borderline aortic root dilation, low normal function, and mild left ventricular hypertrophy (LVH). Follow up echocardiograms were performed for 10 of the 25 patients with minor anomalies (40%). Of those patients with additional imaging, 7 with minor anomalies had normalized, 2 remained stable, and only 1 new finding was noted (mild LVH).
Conclusions: No significant CHD was identified in this cohort of children ages 5 to 18 years with SVT without ventricular pre-excitation. All significant abnormal echocardiogram findings were also associated with abnormal physical exam or EKG findings. For older children and adolescents presenting with SVT without WPW, echocardiogram may not be a necessary part of evaluation when physical exam and EKG are normal.
Article Information
vol. 134 no. Suppl 1 A20343
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Kaitlin L’Italien;
- Steven Conlon;
- Tami Ackley;
- Naomi Kertesz;
- Anna Kamp
- Heart Cntr, Nationwide Childrens Hosp, Columbus, OH
Abstract 19763: Clinical Outcomes and Modes of Death in Timothy Syndrome in the Current Era: A Multi-Center International Study of a Rare Genetic Disorder
Keith A Dufendach, Katherine W Timothy, Benjamin Blevins, Andreas Pflaumer, Susan Etheridge, James Perry, Nico A Blom, Joel Temple, Devyani Chowdhury, Jon Skinner, Christopher Johnsrude, Andras Bratincsak, J. Martijn Bos, Michael J Ackerman, Maully Shah
Circulation. 2016;134:A19763
Abstract
Introduction: Timothy syndrome (TS) is a rare genetic disorder of the L-type cardiac channel Cav1.2 encoded by CACNA1C. The seminal report in 2004 characterized TS as a multisystem disorder, consisting of QT prolongation, congenital heart defects, syndactyly, facial dysmorphism, developmental delay, and 50% mortality by the 3rd year of life. In the last decade additional data regarding outcomes of TS have been limited. The present study aims to investigate clinical outcomes, genetic mutations, and modes of death of TS in the current era.
Methods: A cohort of 17 patients with TS from 12 international tertiary care pediatric centers was included in this retrospective study. Data included demographics, clinical characteristics, electrocardiograms, genetic results, treatment strategies, and outcomes. Patients were classified as either early era or current era based on whether they were diagnosed pre- or post-2004.
Results: Three patients (#1 – 3) were classified as early era and 14 patients (#4 – 17) as current era. Mean follow-up period was 4.9 years (range 0 – 19 years). Amongst all patients, mean maximum QTc = 640 msec (range 500 – 976 msec). The canonical G406R mutation in exon 8 or 8a of CACNA1C was present in 8 (44%) patients. All patients were treated with beta blockers, with 11/14 (78%) current-era patients being treated with an implantable cardioverter defibrillator (ICD). Eleven (61%) total patients had an episode of aborted cardiac arrest, six associated with general anesthesia and two with hypoglycemia. There were four (22%) sudden deaths with one occurring in the early era and three in the current era.
Conclusions: In contrast to previously published data from the early era, TS mortality in patients diagnosed since 2004 is 27%. While increased numbers are needed for definitive results, the data suggests that ICD implantation may increase survival in TS patients, and there is a possible association between general anesthesia and hypoglycemia and sudden cardiac death.
Article Information
vol. 134 no. Suppl 1 A19763
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Keith A Dufendach1;
- Katherine W Timothy2;
- Benjamin Blevins3;
- Andreas Pflaumer4;
- Susan Etheridge2;
- James Perry5;
- Nico A Blom6;
- Joel Temple7;
- Devyani Chowdhury8;
- Jon Skinner9;
- Christopher Johnsrude10;
- Andras Bratincsak11;
- J. Martijn Bos12;
- Michael J Ackerman13;
- Maully Shah14
- 1Cardiology, Perelman Sch of Medicine at the Univ of Pennsylvania, Philadelphia, PA
- 2Pediatric Cardiology, Univ of Utah, Salt Lake City, UT
- 3Cardiology, Naval Med Cntr, San Diego, CA
- 4Cardiology, Royal Children’sHosp, MCRI and Univ of Melbourne, Parkville, Melbourne Victoria, Australia
- 5Cardiology, Rady Children’s Hosp/UC San Diego, San Diego, CA
- 6Cardiology, Leiden Univ Med Cntr, Leiden, Netherlands
- 7Pediatric Cardiology, Nemours/Alfred I. duPont Hosp for Children, Wilmington, DE
- 8Pediatric Cardiology, Cardiology Care for Children, Lancaster, PA
- 9Pediatric Cardiology/Electrophysiology, Starship Children’s Hosp, Aukland, New Zealand
- 10Cardiology, Univ of Louisville, Louisville, KY
- 11Cardiologhy, Pediatric and Adult Congenital Cardiology Kapi’olani Med Specialists, Honolulu, HI
- 12Cardiology, Mayo Clinic, Rochester, MN
- 13Pediatric Cardiology, Mayo Clinic, Rochester, MN
- 14Pediatric Cardiology, Children’s Hosp of Philadelphia, Philadelphia, PA
Abstract 18911: Electrocardiographic Assessment of Brugada Syndrome in Children
Meena Fatah, Jason Klemensberg, Shayenthiran Sreetharan, Laura Fenwick, Myriam Lafreniere-Roula, Robert Hamilton
Circulation. 2016;134:A18911
Abstract
Background: Increasing numbers of children are being referred for assessment of Brugada syndrome (BrS) following the diagnosis of BrS in a parent. We sought to study the ECG phenotype of Brugada syndrome in children referred for assessment.
Methods: Subjects were children with a diagnosis of BrS or its mutations, and referred children of adults with a diagnosis of BrS. All standard electrocardiograms (ECGs), modified Brugada lead ECGs, signal-averaged ECGs (SAECGs), and procainamide challenge results were derived from GE Medical ECG systems (MUSE measurement matrix), and compared to a cohort of normal children aged 5 to 15 years.
Results: 41 subjects were evaluated. For standard ECG parameters, subjects referred for assessment of BrS more frequently had Q waves absent in V6 and present in AVR. R-wave amplitudes were lower across the precordial leads, and R wave duration was longer in AVR, but with no R’ wave. No differences were found in ST J-point, midpoint or endpoint levels between subjects and controls in leads V1, V2 or V3. Brugada lead ECGs, with leads V1, V2 or V3 placed one or two interspaces higher, were performed in 36 subjects and identified a higher mean J-point elevation, but control data for comparison was unavailable. SAECGs were abnormal in 20/41 subjects, providing the highest yield of abnormalities and approaching the anticipated 50% estimate of diseased patients among progeny of Brugada parents (Table 1). Procainamide challenge was performed in 8 individuals, but with poor yield.
Conclusion: Children at risk for Brugada syndrome demonstrate differing ECG patterns from normal, but rarely demonstrate ST changes of Brugada type 1 on standard ECG or with procainamide challenge. Signal averaged ECG appears to be the most sensitive test for Brugada syndrome in children, approaching the expected 50% yield anticipated among children of Brugada syndrome parents referred for evaluation.
Article Information
vol. 134 no. Suppl 1 A18911
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Meena Fatah;
- Jason Klemensberg;
- Shayenthiran Sreetharan;
- Laura Fenwick;
- Myriam Lafreniere-Roula;
- Robert Hamilton
- Paediatrics, Hosp for Sick Children, Toronto, Canada
Abstract 18351: Reentrant Atrial Tachycardia in Congenital Heart Disease Patients, Role of a Crista Leak
Aarti Dalal, Prince Kannankeril, Andrew Radbill, Frank Fish
Circulation. 2016;134:A18351
Abstract
Introduction: Atrial tachycardias (AT) occur commonly in adult patients with congenital heart disease (CHD). Common mechanisms include macroreentry utilizing the cavo-tricuspid isthmus or atriotomy scars, and focal tachycardias (FAT). Increasingly we have observed macroreentry around the crista terminalis utilizing slow, transverse conduction through the crista terminalis which we have termed “crista leak” (AF-CtL).
Methods: We performed a single center retrospective chart review of patients >18 years with postoperative CHD undergoing ablation (RFA) for AT between May 2011 to September 2015. 60 patients underwent ablation of 120 ATs in 73 procedures. Among these 13 patients displayed AF-CtL.
Results: RFA was acutely effective for 117/120 ATs (71/73 cases) and in 13/13 AF-CtL. Median age of the 13 patients with AF-CtL was 37.5 years (19.9-59.8). Congenital lesions included tetralogy of Fallot (2), congenitally corrected transposition (1), double outlet right ventricle (2, one s/p single ventricle repair), VSD/Coarctation of the aorta (1), pulmonary atresia/VSD (1), and ASD (6). 12/13 patients had additional RA scar due to atriotomy or previous ablations. 11/13 had up 4 to additional ATs (median 2), including 4 with additional FAT. Though, 3D-activation mapping suggested a focal origin, entrainment with concealed fusion was achieved along both sides of the crista terminals during AT, confirming the mechanism. In all patients, a broad, low amplitude EGM was recorded at the site of the “crista leak,” often comprising more than 30% of the tachycardia CL. AF-CtL often terminated with a single lesion (total lesions delivered were <10 in all patients, median 5). Differential pacing post-ablation confirmed elimination of conduction through the “crista leak.”
Conclusion: In this single center cohort of CHD patients with AT, macroreentry around the crista terminalis with transverse slow conduction through the crista was common and could be mistaken for FAT. Recognition of this mechanism can improve the efficacy of RFA and help avoid injury to the SA node and phrenic nerve.
Abstract 15740: Cardiac Magnetic Resonance Imaging Predictors of Ventricular Arrhythmia in Tetralogy of Fallot
Angela J Weingarten, Jonathan H Soslow, Larry W Markham
Circulation. 2016;134:A15740
Abstract
Introduction: Tetralogy of Fallot (TOF) is the most common cyanotic congenital heart defect. Surgical management has resulted in dramatic improvements in mortality; however, burden of both atrial and ventricular arrhythmia remains an important cause of morbidity and mortality. Cardiac MRI (CMR) is serially performed in this population to determine timing of pulmonary valve replacement.
Hypothesis: We hypothesized that standard volumetric and functional CMR measures are associated with ventricular arrhythmia (VA) in adults with repaired TOF.
Methods: A cohort of adult patients with repaired TOF who underwent CMR between 8/2004 and 8/2015 was identified. CMR measures were recorded and medical records were reviewed for arrhythmia diagnoses including sustained ventricular tachycardia, non-sustained ventricular tachycardia, sudden death, and aborted sudden death. VA was diagnosed by Holter monitor detection of 3 or more beats of ventricular tachycardia or documentation of clinical diagnosis in the medical record. CMR measures were tested for association with the diagnosis of VA using a Mann Whitney-U test.
Results: Of 119 adults with repaired TOF, 57 (48%) had a diagnosis of arrhythmia; 63% of the arrhythmias were ventricular. Age, left ventricular (LV) diastolic volume, LV systolic volume, and LV stroke volume by CMR were significantly associated with VA. Right ventricular volumes and performance were not significantly associated with VA. See table 1 for all parameters that were tested.
Conclusions: In conclusion, both atrial and ventricular arrhythmias are common following repair of tetralogy of Fallot. Age is the strongest predictor of arrhythmia risk. While tetralogy of Fallot is primarily a right heart lesion, LV hemodynamics play a more significant role in ventricular arrhythmia risk. CMR can potentially assist with VA risk prediction.
Article Information
vol. 134 no. Suppl 1 A15740
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Angela J Weingarten;
- Jonathan H Soslow;
- Larry W Markham
- Div of Pediatric Cardiology, Vanderbilt Univ Med Cntr, Nashville, TN
Abstract 15453: QRS Fragmentation is Associated With Right Ventricular Failure in Adults With Tetralogy of Fallot
Jouke P Bokma, Michiel M Winter, Koen C de Wilde, Hubert W Vliegen, Maarten Groenink, Barbara J Mulder, Berto J Bouma
Circulation. 2016;134:A15453
Abstract
Introduction: Limited data is available to identify tetralogy of Fallot (TOF) patients at risk for right ventricular (RV) function deterioration and subsequent heart failure. Recently, fragmentation of QRS complexes (fQRS) was related to RV fibrosis and all-cause mortality. Our objective was to determine whether fQRS was associated with RV failure.
Methods: This dual center study included all adult TOF patients with at least one cardiovascular magnetic resonance (CMR) investigation from a prospective registry. Notches in the QRS complex in ≥2 contiguous leads on a standard 12-lead electrocardiogram (ECG), not related to right bundle branch block, were defined as fQRS (figure A). Cox hazards regression was used to determine variables associated with the primary outcome heart failure (increase NYHA class requiring diuretics) or death. For patients with multiple CMR examinations, predictors of RV ejection fraction (EF) deterioration were determined with mixed linear models.
Results: A total of 276 TOF patients (age at inclusion: 33±12 years, 55% male, 8.9±3.4 years follow-up, QRS fragmentation in 45%) were included. Baseline RV EF was 49±9% and LV EF was 52±7%. A total of 23 patients had heart failure (n=18) or died from other reasons. In 206 patients with multiple CMRs (total 621), yearly change of RV EF was +0.29% and yearly change of LV EF was +0.20%. In bivariate analysis, a combination of baseline RV EF (HR: 0.90, 95%C.I.:0.85-0.95, p<0.001) and RV EF deterioration (HR: 0.83, 95%C.I.:0.73-0.94, p=0.004) was associated with heart failure/death. QRS fragmentation was the only factor associated with RV EF deterioration (β:-0.60% yearly, 95%C.I.:-1.0, -0.2, p=0.006), corrected for baseline RV EF.
Conclusions: In adult TOF patients, RV EF deterioration was independently predictive for heart failure/death. QRS fragmentation was the only factor associated with RV deterioration. These findings may improve selection of patients for therapy to prevent heart failure.
Article Information
vol. 134 no. Suppl 1 A15453
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Jouke P Bokma1;
- Michiel M Winter1;
- Koen C de Wilde1;
- Hubert W Vliegen2;
- Maarten Groenink1;
- Barbara J Mulder1;
- Berto J Bouma1
- 1Cardiology, Academic Med Cntr, Amsterdam, Netherlands
- 2Cardiology, Leiden Univ Med Cntr, Leiden, Netherlands
Abstract 15571: Analysis of Out-of-hospital Cardiac Arrest in Infants, Children, < Adolescents in Japan
Masao Yoshinaga
Circulation. 2016;134:A15571
Abstract
Background: A prospective population-based study using the Utstein style has obtained data on patients suffering OHCA since 2005 in Japan. Additional information may help determine confounders present in each case and aid in preventing OHCA in infants, children, and adolescents.
Methods and Results: A council for prevention of cardiovascular diseases in childhood of Kyushu Medical Association began obtaining data on OHCA (<20 years of age) from local fire departments and school officials in the Kyushu area in 2013. The questionnaire sought data using the Utstein style and additional data on: presence/absence of underlying diseases; location of OHCA; and activities before/surrounding OHCA, including school activities. A total of 276 cases were obtained: aged 0 (84 cases); aged 1-5 (53 cases); aged 6-12 (42 cases); and aged 13-19 (97 cases). Among 166 cases that occurred at home, 86% (136/159; seven cases unknown whether dead/alive) were fatal. In 84 infants, 65% (55 cases) occurred during sleep. Of these, 96% (51/53; two cases with unknown prognosis) were fatal. Prevalent situations/locations were during sleep (44%) in aged 1-5, water accident (35%) in aged 6-12, and suicide (25%) and exercise-related (24%) in aged 13-18, respectively. Of 28 OHCA cases with underlying cardiovascular diseases, cardiomyopathy (eight cases: HCM 7, DCM 1), arrhythmia (seven cases: CPVT 2, LQTS 1, SSS 1, VT 1, AF 1, VT/ICD implantation 1), and congenital heart diseases (six cases: aberrant origin of coronary artery 1, VSD/Eisenmenger 1, TOF (postoperative) 2, dTGA (P/O) 1, CoA (P/O) 1) were prevalent causes.
Conclusions: New strategies to prevent sudden death during sleep should be examined and implemented for infants. Cardiomyopathy/arrhythmia/postoperative chronic heart disease are still major causes of cardiovascular-related OHCA. Diagnostic criteria with high sensitivity and specificity should be determined to screen cardiomyopathy and/or arrhythmia in younger age groups. The recommendation and support not to start competitive sports activities should be infromed not only to the parents but to the young.
Article Information
vol. 134 no. Suppl 1 A15571
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Masao Yoshinaga
- Pediatrics, Kagoshima Univ Graduate Sch of Med and Dental Sciences, Kagoshima, Japan
Abstract 13416: The Days of the Holter Monitor Are Numbered: Extended Continuous Rhythm Monitoring Detects More Clinically Significant Arrhythmias in Adults With Congenital Heart Disease
Karen Schultz, George Lui, Doff McElhinney, Susan Fernandes, Anne Dubin, Ian Rogers, Mohan Viswanathan, Anitra Romfh, Kara Motonaga, Scott Ceresnak
Circulation. 2016;134:A13416
Abstract
Introduction: Arrhythmias are a leading cause of death in adults with congenital heart disease (ACHD). Arrhythmia detection is essential to management and risk assessment in ACHD. While 24 to 48-hour Holter monitors are often used to assess arrhythmia burden, extended continuous rhythm monitors (ECRM) can record 2 weeks of data. We hypothesized that more clinically significant arrhythmias would be detected on ECRM beyond the first 48 hrs of monitoring.
Methods: We reviewed ambulatory Zio® (iRhythm, San Francisco, CA) monitors performed in ACHD patients from June 2013 – May 2016. Atrial fibrillation/flutter (AF), ventricular tachycardia (VT), supraventricular tachycardia (SVT), sinus pause >3 sec, and 3rd or 2nddegree type II atrioventricular block (AVB) were considered significant. Number and type of arrhythmias detected within the first 48 hrs were compared to those identified beyond 48 hrs.
Results: A total of 387 monitors were performed in 306 patients (34 ± 12.5 yrs, 40% male). The most common diagnoses were Tetralogy of Fallot, transposition of the great arteries, and single ventricle after Fontan. Average wear time was 9.4 ± 4.2 d. Overall, 51% of ECRM showed a significant arrhythmia, fewer than half of which were noted during the first 48 hrs (25% overall). VT was detected by ECRM in 17%, only 30% of which were within 48 hrs. SVT was detected by ECRM in 40%, 48% of which were within 48 hrs. Kaplan-Meier estimates of freedom from arrhythmia are shown in the table and figure.
Conclusion: ECRM was more likely to detect a significant arrhythmia beyond the standard 48-hour monitoring period in ACHD patients, suggesting that ECRM may be more useful than Holter monitoring in this population.
Article Information
vol. 134 no. Suppl 1 A13416
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Karen Schultz1;
- George Lui2;
- Doff McElhinney1;
- Susan Fernandes2;
- Anne Dubin1;
- Ian Rogers2;
- Mohan Viswanathan2;
- Anitra Romfh2;
- Kara Motonaga1;
- Scott Ceresnak1
- 1Pediatric Cardiology, Stanford Univ, Palo Alto, CA
- 2Adult Congenital Heart Disease, Stanford Univ, Palo Alto, CA
Abstract 11413: Appearance of QRS Fragmentation Late After Atrial Switch Repair for d-Transposition of the Great Arteries is Associated With Adverse Clinical Outcome
Frederik Helsen, Bert Vandenberk, Pieter De Meester, Alexander Van De Bruaene, Charlien Gabriels, Els Troost, Marc Gewillig, Bart Meyns, Rik Willems, Werner Budts
Circulation. 2016;134:A11413
Abstract
Introduction: The extent of myocardial fibrosis on magnetic resonance imaging (MRI) in the systemic right ventricle (RV) of adults after atrial switch repair for d-transposition of the great arteries (d-TGA) correlates with outcome. However, MRI is costly and access is limited. Fragmented QRS (fQRS) on a 12-lead electrocardiogram (ECG) reflects inhomogeneous ventricular activation. It is considered to be a surrogate for fibrosis and related with outcome in ischemic cardiomyopathy.
Hypothesis: Appearance of fQRS during follow-up is a predictor for adverse events in adults after atrial switch repair for d-TGA.
Methods: Records of adults with atrial switch repair for d-TGA were retrospectively reviewed in the database of a tertiary care hospital. Exclusion criteria were systemic RV assist device or heart transplantation (HTx) before the age of 16 years, or fQRS already present at transfer from the pediatric department. One blinded reader analyzed all available ECGs to detect fQRS. fQRS, severe tricuspid regurgitation (TR), severe RV dysfunction and severe RV dilatation were modeled as time-dependent covariates. Cox regression was performed to assess the relationship between covariates and (1) the composite endpoint of cardiovascular mortality, HTx or systemic RV assist device, and (2) worsening RV function.
Results: Records of 89 patients (34% female, 42% Mustard repair) were analyzed. Patients underwent atrial switch repair between Oct 1969 and Nov 1992. At latest follow-up, fQRS was noted in 26 patients (29%), most frequently inferior (92%). Over a median follow-up of 16.9 (IQR 12.6-22.9) years, the composite endpoint occurred in 9 patients (10%). In multivariate Cox analysis, appearance of fQRS (HR 14.11; 95% CI 1.42-140.12) and development of severe RV dysfunction (HR 11.36; 95% CI 2.08-62.17) were significantly associated with the composite endpoint. Moreover, appearance of fQRS was significantly associated with worsening RV function (HR 2.66; 95% CI 1.18-6.01), independently of development of severe TR.
Conclusions: Appearance of fQRS is associated with adverse clinical outcome and worsening RV function in adults after atrial switch repair for d-TGA. It might become an easily implementable tool to identify patients at risk for adverse events.
Article Information
vol. 134 no. Suppl 1 A11413
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Frederik Helsen1;
- Bert Vandenberk1;
- Pieter De Meester1;
- Alexander Van De Bruaene1;
- Charlien Gabriels1;
- Els Troost1;
- Marc Gewillig2;
- Bart Meyns3;
- Rik Willems1;
- Werner Budts1
- 1Cardiology, Univ Hosps Leuven, Leuven, Belgium
- 2Pediatrics, Univ Hosps Leuven, Leuven, Belgium
- 3Cardiac Surgery, Univ Hosps Leuven, Leuven, Belgium
Abstract 20437: Predictors of Prosthesis Durability After Mitral Valve Replacement in Children
Patrick A Upchurch, Sitaram Emani
Circulation. 2016;134:A20437
Abstract
Introduction: Limits of successful mitral valve replacement (MVR) in children include patient size, left ventricular (LV) geometry, and lack of small prosthetic valves. Due to its non-fixed diameter, the Melody valve is suited to address these concerns.
Methods: A single institution retrospective review of children aged less than 18 years undergoing MVR between 1992 and 2016. Primary outcomes include freedom from structural valve deterioration (SVD) and freedom from re-replacement, which were examined as a function of prosthesis type, patient age, diagnosis of LV hypoplasia, and markers of prosthesis-patient mismatch. A conditional recurrent event Cox proportional hazards regression model assessed association between outcome and predictors.
Results: A total of 154 children underwent 213 MVRs: 134 (62.9%) mechanical, 37 (17.4%) porcine, 12 (5.6%) pericardial, and 30 (14.1%) Melody. Median age in years at initial replacement: 8.6 for pericardial valves, 6.0 for mechanical, 3.0 for porcine, and 0.8 for Melody. There were 93 SVD events and 61 re-replacements. Four year freedom from SVD: 66% for mechanical valves, 75% for Melody, 16% for porcine, and undefined for pericardial. Younger patient age, diagnosis of LV hypoplasia, prosthesis type, smaller prosthesis size, and larger prosthesis size: patient weight ratio were univariately associated with hazard of SVD and re-replacement (p<.05). In multivariable modeling, valve type remained a predictor after adjustment for valve size and diagnosis (p=0.002) and after adjustment for age (p<.001). Melody valves were limited to patients aged less than 3.2 years. Secondary analysis examined this age-restricted cohort. Median times to SVD were 4.03, 0.71, and 0.38 years for mechanical, porcine, and pericardial valves. For Melody valves, the SVD rate did not reach 50%. Median times to re-replacement were 7.68, 4.13, 1.47, and 0.77 years for mechanical, Melody, porcine, and pericardial valves.
Conclusions: Melody and mechanical valves are at lower covariate-adjusted risk of SVD and re-replacement than porcine and pericardial valves, and are thus more durable. Given adjustable Melody valve diameter and lack of small mechanical prostheses, the Melody valve should be considered for MVR in neonates and infants.
Article Information
vol. 134 no. Suppl 1 A20437
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Patrick A Upchurch;
- Sitaram Emani
- Cardiac Surgery, Boston Children’s Hosp, Boston, MA
Abstract 18300: Cardiac Arrest in the Pediatric Post-Operative Cardiac Population: An Opportunity to Further Enhance PALS Guidelines
Kristen Nelson McMillan, Jordan Duval-Arnould, Kristen Brown, Leann McNamara, Diane Alejo, Mayuri Machado Alvarez, Narutoshi Hibino, Luca A Vricella, Donald H Shaffner, Elizabeth A Hunt
Circulation. 2016;134:A18300
Abstract
Introduction: Despite cardiopulmonary arrest (CPA) occurring 10 times more frequently in children admitted to pediatric intensive care units with cardiac disease than other diagnoses, there is a paucity of data regarding patient and procedure-specific parameters or use of real-time feedback during CPA.
Hypothesis: Using our pediatric CPA database, we describe patient, procedure and resuscitative variables related to CPA following congenital heart disease (CHD) surgery.
Methods: Children < 21 years requiring cardiopulmonary bypass (CPB) were reviewed and those experiencing CPA in the post-operative period were identified. Parameters from pre, intra and post-arrest resuscitation periods were analyzed.
Results: Of 461 consecutive CPB, 28/461 (6%) had a CPA within 30 days of the procedure in 27 patients. Six patients had >1 event, for a total of 34 CPA events. CPA occurred < 24 hours post-CPB in 15/28 (54%) with 10/15 (67%) of procedures being STAT 4 or 5 category (90% of which involved placement of shunts or conduits during the corresponding operative event). The sternum remained open at the time of CPA in 10/34 (29%), with 75% open following STAT 4 or 5 procedures. Arterial line was in place at time of CPA for 26/34 (76%) events. Weight at time of CPA was <5 kg for 17/28 (61%). Mean duration of CPA was 14 minutes. In 94% of CPA events (32/34) return of circulation was achieved, with 5/32 (16%) requiring ECPR to do so. Survival to hospital discharge was achieved in 18/27 patients (67%), with 5/8 (63%) surviving following STAT 5 procedures. Post-op CPA occurred equally in males and females, but 7/9 (78%) of those who died before hospital discharge were male. Of those surviving to hospital discharge, 17/18 (94%) had return to neurologic baseline at time of discharge.
Conclusions: Rate of CPA in the postoperative CHD child is high but outcomes can be good. The majority of post-CPB CPAs occurred within 24 hours of surgery and the majority of those had STAT 4 or 5 procedures. Goal directed CPR utilizing arterial lines is not covered in current guidelines but offers the chance to optimize outcomes, particularly in the patient with an open sternum. Important data is available regarding patient, procedure and resuscitation factors that deserve further analysis to inform future guidelines.
Article Information
vol. 134 no. Suppl 1 A18300
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Kristen Nelson McMillan1;
- Jordan Duval-Arnould1;
- Kristen Brown1;
- Leann McNamara2;
- Diane Alejo3;
- Mayuri Machado Alvarez3;
- Narutoshi Hibino4;
- Luca A Vricella4;
- Donald H Shaffner1;
- Elizabeth A Hunt1
- 1Anesthesia and Critical Care Medicine, Johns Hopkins Sch Med, Baltimore, MD
- 2Pharmacy, Johns Hopkins Hosp, Baltimore, MD
- 3Surgery, Johns Hopkins Hosp, Baltimore, MD
- 4Surgery, Johns Hopkins Sch Med, Baltimore, MD
Abstract 18380: Physiological Augmentation of Pulmonary Arterial Growth in Patients With Single Ventricle Physiology With Interim Selective Systemic to Pulmonary Arterial Shunt
Cameron Seaman, Yves d’Udekem, Bryn Jones, Christian Brizard, Michael M Cheung
Circulation. 2016;134:A18380
Abstract
Introduction: Stenosis or diffuse hypoplasia of central pulmonary arteries (PA) is common in patients with single ventricle physiology, often requiring surgical patching. Such repairs are prone to failure, particularly with low pressure venous flow (BCPC or Fontan). We describe our experience of disconnection of central pulmonary arteries and selective systemic-PA shunt to the hypoplastic vessel.
Methods: Single ventricle patients (n=12) with a diffuse LPA hypoplasia underwent PA disconnection (ligation clip) and selective arterial shunt to the LPA. Patients were considered, if there was ≤ mild AV valve regurgitation, and no more than mild systolic dysfunction on echo. Following systemic-LPA shunt, patients were re-assessed by cardiac catheterisation prior to further surgery, with follow-up catheterisation later performed.
Results: Increased volume loading was well tolerated with no increase in AV valve regurgitation and preserved systolic function. Selective arterial shunting increased the caliber of the LPA (baseline median 4.1mm (1.2-5.6); post shunt 6.5 (1.7-11.9)) and this increase was preserved post-Fontan (median 6.7mm (1.3-8.0)). As expected ventricular EDP was increased with arterial shunting but resolved after takedown of the shunt and Fontan completion. Post-Fontan hospital length of stay was not prolonged (median 11 days (7-14)).
Conclusion: In univentricular hearts and PA hypoplasia, selective systemic-PA shunting physiologically increases the caliber of the distal vessels. In selected patients this can be done safely with maintenance of PA growth and resolution of the elevated EDP with Fontan completion.
Article Information
vol. 134 no. Suppl 1 A18380
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Cardiology, The Royal Children’s Hosp, Melbourne, Australia
- 2Cardiac Surgery, The Royal Children’s Hosp, Melbourne, Australia
Abstract 18124: Delayed Staged Palliation Does Not Affect Clinical Outcomes for Children With Hypoplastic Left Heart Syndrome and Variants
Devin Chetan, Christoph Haller, Steven M Schwartz, Christopher A Caldarone, Glen S Van Arsdell, Osami Honjo
Circulation. 2016;134:A18124
Abstract
Introduction: Impact of delayed stage II and/or Fontan palliation on survival and Fontan physiology is not well understood.
Hypothesis: Delayed staged palliation results in lower survival and worse Fontan outcomes.
Methods: All 232 patients with HLHS undergoing stage I palliation from 2000-2011 were reviewed (Figure). The clinical course for patients who had delayed stage II (>7 months) or Fontan (>3.5 years) was documented. Patients were classified as having either minor or significant reasons for delayed palliation. Rates of on-time and overall Fontan completion, survival, transplant, and post-Fontan failure were compared between patients who did not meet (G1; n=28) and met (G2; n=125) conventional stage II palliation timelines. Rates of post-Fontan failure were also compared for patients who did not meet (G3; n=44) and met (G4; n=74) conventional Fontan completion timelines.
Results: Delayed stage II palliation resulted in equivalent rates of on-time (G1: 15 [53.6%] vs G2: 59 [47.2%]; p=0.54) and delayed (G1: 10 [35.7%] vs G2: 34 [27.2%]; p=0.37) Fontan completion, with no difference noted between rates of delay because of minor or significant reasons (p<0.10). There was a trend toward greater overall Fontan completion (G1: 25 [89.3%] vs G2: 93 [74.4%]; p=0.09) in the delayed stage II group. The rates of interstage death (G1: 2 [7.1%] vs G2: 17 [13.6%]; p=0.53) and transplant (G1: 1 [3.6%] vs G2: 6 [4.8%]; p=1.00) were similar between groups. The rates of Fontan failure were comparable (G1: 1 [3.6%] vs G2: 3 [2.4%]; p=0.56). For patients having delayed Fontan, the rate of Fontan failure was comparable (G3: 1 (2.3%) vs G4: 3 (4.1%); p=1.00).
Conclusions: Delayed timing of stage II and Fontan palliation did not impact survival or Fontan failure. While close followup and sensible rehabilitation strategy are likely contributors to equivalent outcomes, this result may partly be due to patients who never reached subsequent palliation because of inter-stage death or transplant.
Article Information
vol. 134 no. Suppl 1 A18124
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Devin Chetan;
- Christoph Haller;
- Steven M Schwartz;
- Christopher A Caldarone;
- Glen S Van Arsdell;
- Osami Honjo
- Cardiovascular Surgery, The Hosp for Sick Children, Toronto, Canada
Abstract 16506: A Defect of the Aortic Wall Regenerated by a Novel Warp Knitting Fabric Comprising a Combination of Biodegradable and Non-biodegradable Yarn
Shintaro Nemoto, Hayato Konishi, Ryo Shimada, Hideaki Yamada, Jun Sakurai, Atsuko Onishi, Kazuteru Kohno, Masaya Ito
Circulation. 2016;134:A16506
Abstract
Introduction: Vascular wall regeneration has been attempted using various types of biodegradable materials and stem cells, but the results have been disappointing.
Hypothesis: Aortic wall regeneration can be promoted by use of an elaborately designed synthetic cardiovascular patch (OFT patch).
Methods: The OFT patch is made from an extensible warp-knitted fabric that is a combination of biodegradable (poly-L-lactic acid: PLLA) and non-biodegradable (polyethylene terephthalate: PET) yarn. The fabric was coated with gelatin crosslinked with glutaraldehyde to provide water resistance. The in vitro mechanical properties of the OFT patch were compared with those of currently used surgical patches. Part of the wall of the canine descending aorta was replaced with an OFT patch. The patch was explanted three months later for histological examination.
Results: The OFT patch had excellent tensile strength, suture retention strength, and bending resistance that were equivalent to those of current patches. The aortic lumen of the explanted OFT patch was covered with smooth intimal tissue. Microscopic examination revealed ideal tissue regeneration characterized by layered smooth muscle cells and collagen fibers with tissue connection across the OFT patch with neo-arterioles in the early stage after implantation. There was little inflammatory reaction and no calcium deposition on the patch yarn, and no aneurysmal or stenotic changes in patch-implanted regions.
Conclusions: Since the non-biodegradable yarn of the patch is program-designed to expand to quadruple its initial size, the regenerated vascular wall can grow in size as the biodegradable PLLA portion is absorbed. Our results suggest that the OFT patch is suitable for use as a surgical patch in pediatric cardiac surgery.
Article Information
vol. 134 no. Suppl 1 A16506
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Shintaro Nemoto1;
- Hayato Konishi1;
- Ryo Shimada1;
- Hideaki Yamada2;
- Jun Sakurai2;
- Atsuko Onishi3;
- Kazuteru Kohno3;
- Masaya Ito3
- 1Thoracic and Cardiovascular Surgery, Osaka Med College, Osaka, Japan
- 2Production Development, Fukui Warp Knitting Co., Ltd., Fukui, Japan
- 3Healthcare Business Development, Teijin Limited, Hino, Tokyo, Japan
Abstract 16723: Rates of Interventions Post Coarctation Repair in Neonates Versus Infants: Does Age Matter?
Rinske IJsselhof, Hua Liu, Frank Pigula, John Mayer, Pedro del Nido, Meena Nathan
Circulation. 2016;134:A16723
Abstract
Introduction: Conflicting reports exist about the timing of coarctation (CoA) repair and rate of subsequent interventions on the CoA site and other left sided structures (LSS).
Hypothesis: There will be no difference in post-discharge interventions (post-DCI) between neonates and infants following isolated CoA repair.
Methods: Retrospective review of neonates (≤30 days) and infants (1-6 months) with isolated CoA undergoing repair (via thoracotomy) between 2000 and 2016. Clinical and echocardiographic data including preoperative Z scores of aortic valve, arch and isthmus were reviewed. Postoperative length of stay (intensive care [PICULOS]; hospital [PHLOS]), and post-DCI on CoA and LSS (mitral valve/LVOT/aortic valve) were compared between groups. Linear/Cox regression was used to determine predictors of post-DCI and LOS for the entire cohort.
Results: There were 213 (71.5%) neonates and 85 (28.5%) infants. Mean follow up was 3 (IQR 0.2, 9) years. There was no difference in post-DCI on CoA (10.3% vs. 4.7%; p=0.1) or LSS (9.9% vs. 9.4%; p=0.9); figure. Median PICULOS (3.01 vs. 2.28 days, p<0.001) and PHLOS (6.23 vs. 4.85 days, p<0.001) was higher in neonates versus infants. On multivariable modeling preoperative left sided catheter intervention, left sided obstructive lesions, and hypoplastic aortic arch predicted post-DCI on CoA or LSS. Age and genetic abnormality predicted prolonged PICULOS and PHLOS (table). On comparing preoperative aortic valve, transverse arch and isthmus Z scores between those with and without post-DCI, preoperative aortic valve Z score was associated with post-DCI on LSS [-2.05(-2.88, -1.28) vs. -1.56 (-2.19, -0.72); p=0.001).
Conclusions: Coarctation repairs can be safely performed in infants and neonates with acceptable post-DC intervention on CoA and other LSS. Weight and age should not be considered a contraindication to early repair. Preoperative aortic valve Z score may be an important discriminator for interventions on LSS.
Article Information
vol. 134 no. Suppl 1 A16723
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Cardiac Surgery, Univ Med Cntr Utrecht, Utrecht, Netherlands
- 2Cardiac Surgery, Boston Children’s Hosp, Boston, MA
- 3Cardiovascular and Thoracic Surgery, Univ of Louisville Physicians, Inc., Louisville, KY
Abstract 14490: Outcome of Symptomatic Partial Atrioventricular Septal Defect Requiring Repair During Infancy. Multicentric Study.
Sylvia Krupickova, Gareth Morgan, Mun Hong Cheang, Olivier Ghez, Michael Rigby, Andrea Battista, Ariana Spanaki, Rodney Franklin, Jan Marek, Alain Fraisse
Circulation. 2016;134:A14490
Abstract
Introduction: Patients with symptomatic partial atrioventricular septal defect (pAVSD) requiring early surgical repair are thought to be at greater risk. However, the outcome and risk profile of this cohort of patients is currently poorly defined.
Hypothesis: The aim of this study was to investigate the outcome of symptomatic pAVSD infants requiring early repair and to identify risk factors which may predict mortality and left atrioventricular valve (LAVV) reoperation.
Methods: This multicenter study recruited 51 patients (24 female) in 3 tertiary centres. The inclusion criteria were: i) pAVSD (including cases with negligible ventricular component), ii) heart failure unresponsive to treatment, iii) biventricular repair during the first year of life. Medical notes and operative notes were retrospectively analysed for demographic, perioperative and echocardiographic data.
Results: The median age at the corrective surgery was 179 (range 0-357) days. Sixteen patients (31%) had unfavorable anatomy of the LAVV: dysplastic(N=7), double orifice(N=3), severely deficient valve leaflets (N=1), hypoplastic LAVV annulus and/or mural leaflet (N=3), short/poorly defined chords (N=2). Four patients (7.8%) died at median interval of 52 days (range 0-187 days) after primary repair. Eleven patients (22%) were re-operated at a median interval of 40 days following primary repair (4 days – 5.1 years) for severe LAVV regurgitation. Two patients required mechanical LAVV replacement. In multivariate analysis, the anatomy of the LAVV was the only risk factor associated with LAVV reoperation.
Conclusions: Patients with pAVSD requiring repair during infancy experience significant morbidity and mortality. Surgical repair is successful in the majority of the cases. The re-operation rate of the LAVV is high and the presence of unfavourable LAVV anatomy is an independent predictor of an adverse outcome.
Article Information
vol. 134 no. Suppl 1 A14490
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Sylvia Krupickova1;
- Gareth Morgan2;
- Mun Hong Cheang3;
- Olivier Ghez4;
- Michael Rigby1;
- Andrea Battista5;
- Ariana Spanaki2;
- Rodney Franklin1;
- Jan Marek5;
- Alain Fraisse1
- 1Paediatric Cardiology, Royal Brompton Hosp, London, United Kingdom
- 2Paediatric Cardiology, Evelina London Children’s Hosp, London, United Kingdom
- 3UCL Institute of Cardiovascular Science, Univ College London, London, United Kingdom
- 4Paediatric Cardiothoracic Surgery, Royal Brompton Hosp, London, United Kingdom
- 5Paediatric Cardiology, Great Ormond Street Hosp, London, United Kingdom
Abstract 12056: Computational Fluid Dynamics Description of Blood Flow in a Bidirectional Glenn Shunt Supplemented With a Modified Blalock-Taussig Shunt: Relevance to Thrombosis and Power Loss
Seda Aslan, Nancy Ross-Ascuitto, Martin Guillot, Robert Ascuitto
Circulation. 2016;134:A12056
Abstract
Introduction: A bidirectional Glenn shunt (BGS) has been supplemented with a modified Blalock-Taussig shunt (BTS), to enhance growth of the pulmonary arteries (PAs). However, the hemodynamics is incompletely understood.
Hypothesis: High velocity BTS flow imposed on low velocity BGS flow can create secondary currents (vortices) in the PAs conducive to clot deposition and power dissipation.
Methods: We employed a computational model (Fluent) of pulsatile flow (viscosity 5 cPa-s), using the finite volume method, and a schematic representation of a BGS with a BTS, to determine velocity field, wall shear stress (WSS) and power (W) efficiency (PE). The region studied included the internal jugular, subclavian and innominate veins, BGS (12.5 mm), BTS (4 mm) and PAs (9 mm). Vessel sizes and flow rates were derived from reported values. Flow rates were fixed at the inlet of the veins, and in the BGS was 1L/min. Aortic pressure (82/42 mmHg) was used at the inlet to the BTS, and a mean pressure (12 mmHg) at the outlets of the PAs.
Results: Fig 1 shows velocity magnitude at peak systole. The BTS jet (red) enters the LPA, where it gives rise to dissipative counter-rotating velocity fields, which augment local WSS. Fig (2) shows the velocity fields (arrows) in cross-sectional planes where the BGS and BTS connect to the PAs. The high WSS (350 Pa) is sufficient (> 100 Pa) to initiate platelet aggregation leading to thrombus formation. PE (1-Wloss /Win) for the BGS alone was 97%; whereas, with the BTS it decreased to 29%. The BTS increased BGS pressure, 12.3 to 14.0 mmHg.
Conclusion: Supplementing a BGS with a BTS can: 1) elevate BGS pressure, 2) create regions at risk for thrombus formation and 3) worsen power loss.
Article Information
vol. 134 no. Suppl 1 A12056
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Mechanical Engineering, Univ of New Orleans, New Orleans, LA
- 2Cardiology, Louisiana State Univ, New Orleans, LA
Abstract 12201: Infants With 22q11.2 Deletion Syndrome Undergoing Repair of Tetralogy of Fallot, Interrupted Aortic Arch, and Truncus Arteriosus have Longer Hospitalizations and Increased Rates of Infection
Mary K Olive, Carlos M Mery, Amelia S Wallace, Kevin D Hill, Jeffrey P Jacobs, Erle H Austin, Sara K Pasquali, Marshall L Jacobs, Jeffrey S Heinle, Daniel J Penny
Circulation. 2016;134:A12201
Abstract
Introduction: 22q11.2 deletion syndrome (22q11del) is common in patients with certain types of congenital heart disease. The prevalence of 22q11del and its impact on clinical outcomes remains unclear as only small single center studies are available and have shown conflicting data.
Methods: All infants with tetralogy of Fallot (TOF), truncus arteriosus (TA), interrupted aortic arch (IAA), or IAA+TA included in the STS Congenital Heart Surgery Database from 1/10 to 6/15 were included. Infants with single ventricle lesions, pulmonary atresia with MAPCAs, and trisomies were excluded. Perioperative mortality and STS-defined major morbidities were compared between patients with and without 22q11del. Analyses were performed using Wilcoxon rank sum or chi-square tests.
Results: A total of 5,179 patients were included. 22q11del was present in 255 (6.3%) patients with TOF, 160 (28.8%) with TA, 206 (38.4%) with IAA, and 19 (28.8%) with IAA+TA undergoing repair. For all procedural cohorts, there was no significant difference in perioperative mortality between the two groups. Infants with 22q11del had a longer hospitalization and a higher incidence of postoperative infections (Table). Within the TOF cohort only, infants with 22q11del had a higher incidence of the STS-defined composite major morbidity measure (12.5% vs. 6.1%, p<0.01), largely driven by an increased incidence of unplanned re-interventions (9.9% vs. 4.3%, p<0.01) and phrenic nerve injuries (2.5% vs. 0.8%, p=0.01).
Conclusions: 22q11del is common in infants undergoing repair of TOF, TA, IAA, and IAA+TA. While operative mortality for the diagnostic groups was not impacted by 22q11del, patients with 22q11del did have longer hospitalizations and a higher incidence of infectious complications. Families should be counseled appropriately and further strategies should be developed to limit the morbidity in patients with 22q11del undergoing congenital heart surgery.
Article Information
vol. 134 no. Suppl 1 A12201
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Mary K Olive1;
- Carlos M Mery2;
- Amelia S Wallace3;
- Kevin D Hill4;
- Jeffrey P Jacobs5;
- Erle H Austin6;
- Sara K Pasquali1;
- Marshall L Jacobs7;
- Jeffrey S Heinle2;
- Daniel J Penny8
- 1Dept of Pediatrics, Univ of Michigan C. S. Mott Children’s Hosp, Ann Arbor, MI
- 2Dept of Surgery, Div of Congenital Heart Surgery, Baylor College of Medicine, Houston, TX
- 3Pediatrics, Duke Clinical Rsch Institute, Durham, NC
- 4Div of Pediatric Cardiology, Duke Univ, Durham, NC
- 5Dept of Surgery, Div of Cardiothoracic Surgery, John’s Hopkins All Children’s Heart Institute, Saint Petersburg, FL
- 6Dept of Cardiovascular and Thoracic Surgery, Univ of Louisville Hosp, Louisville, KY
- 7Dept of Surgery, Johns Hopkins Sch of Medicine, Baltimore, MD
- 8Dept of Pediatrics, Baylor College of Medicine, Houston, TX
Abstract 12477: Association of Age and Outcome After Bidirectional Cavopulmonary Anastomosis
Andrew M Koth, Claudia A Algaze, Shiying Hao, Andrew Y Shin
Circulation. 2016;134:A12477
Abstract
Introduction: The Glenn procedure has traditionally been performed between 4-6 months of age. Several studies have investigated the benefits of performing the procedure earlier, to shorten the inter-stage period. No studies have specifically looked the unintended consequences of early Glenn procedures (< 4 months) related to post-operative outcomes.
Hypothesis: We hypothesized that after the Glenn procedure, younger patients would have a longer post-operative length of stay.
Methods: All patients undergoing the Glenn procedure between 1/2010 and 7/2015 were included in this retrospective cohort study. Demographic data, including baseline saturations, medications, length of intubation and chest tube drainage were recorded. Mean post-operative length of stay was calculated. Standard descriptive statistics were used. A univariable analysis was conducted using the appropriate test based on data distribution. A multivariable analysis was then completed using predictors from the univariable analysis.
Results: Over the study period, 50 patients were included. Patients were separated into two cohorts[≥4 months (28) and <4 months (22)]. Other than height and weight, the two cohorts were indistinguishable in their pre-operative saturation, medications, catheterization hemodynamics, atrioventricular valve regurgitation and ventricular function. Length of intubation and chest tube drainage were not different between the cohorts. Younger age was associated with longer post-operative length of stay [mean 14.6 (±15) vs. 7.7(±5.1) days, p=0.03]. In a multivariable regression analysis, in addition to ventricular dysfunction (Bcoefficient 8.8, p=0.05), Glenn procedures performed before 4 months were independently associated with longer length of stay (B coefficient -6.9, p=0.03).
Conclusion: We found that elective Glenn procedures performed after 4 months of age had improved outcomes compared to a younger cohort. These findings suggest that balancing timing of surgery to decrease the inter-stage period should take into consideration differences in post-operative recovery with early operations.
Article Information
vol. 134 no. Suppl 1 A12477
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Andrew M Koth;
- Claudia A Algaze;
- Shiying Hao;
- Andrew Y Shin
- Pediatric Cardiology, Stanford Univ, Palo Alto, CA
Abstract 16899: Exome Sequencing for Genetic Etiology in Families With Sudden Cardiac Death or Arrest
Victoria L Vetter, Noreen P Dugan, Sawona Biswas, Mindy Li, Matthew C Dulik, Vijayakumar Jayaraman, Laura K Conlin, Basal Devkota, Edward J Romasko, Jenica Abrudan, Nancy B Spinner, Ian D Krantz
Circulation. 2016;134:A16899
Abstract
Introduction: Sudden cardiac arrest/death (SCA/D) is an uncommon, but tragic occurrence in youth. Causes include inherited structural, functional, and electrical cardiac abnormalities, with more than 100 known associated genes. A proactive family screening approach is important to provide life-saving treatment and to help identify other affected members due to the high association of genetic causes.
Hypothesis: Exome sequencing (ES) can be used to identify genetic causes of SCA/D.
Methods: Our objective was to use ES to identify definite and potential causes in families affected with SCA/D. Our study population included 41 probands with clinical symptoms or signs ± family history of SCA/D or SCA/D-associated conditions (affected), but without known molecular etiologies for SCA/D. Additional samples were obtained from 127 family members (parents/siblings/grandparents: 40 clinically affected and 87 unaffected). Samples were analyzed following exome capture and sequencing at an average read depth of 100X. Reads were mapped to human genome GRCh37 using Novoalign, and post-processing and analysis was done using Picard and GATK. A total of 103 genes (2,190 exons) related to SCA/D were used as a primary filter; 100 random variants within the targeted genes were evaluated for depth of sequencing and coverage. The majority of exons (97.6%) were captured and fully covered on average at minimum of 20x sequencing depth.
Results: Analysis of the 41 SCA/D probands revealed a definitive diagnostic answer in 11/41 (26.8%). Variants of uncertain significance (VUS), potential causes of SCA-associated cardiac conditions, were found in 15/41 (36.6%) cases, and 15/41 (36.6%) cases were negative. Of the 11 gene positive probands, 14/42 (33.3%) family members were positive for the deleterious gene. Other medically actionable pathogenic gene mutations, not related to the primary cardiac conditions, were identified in 3/41 probands (7.3%).
Conclusions: Exome sequencing is a helpful diagnostic tool for SCA/D, given its potential to successfully identify a molecular diagnosis, but clinicians should be aware of the limitations including incomplete knowledge of disease genes, uncertainty resulting from identification of VUS, and incomplete coverage of known genes.
Article Information
vol. 134 no. Suppl 1 A16899
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Victoria L Vetter;
- Noreen P Dugan;
- Sawona Biswas;
- Mindy Li;
- Matthew C Dulik;
- Vijayakumar Jayaraman;
- Laura K Conlin;
- Basal Devkota;
- Edward J Romasko;
- Jenica Abrudan;
- Nancy B Spinner;
- Ian D Krantz
- Perelman Sch of Medicine, Children’s Hosp of Philadelphia, Philadelphia, PA
Abstract 17036: Transesophageal Electrophysiology Study as a Tool to Guide Post-natal Management of Fetal Supraventricular Tachycardia
Claudia Renaud, Jeffrey M. Vinocur, Edgar Jaeggi
Circulation. 2016;134:A17036
Abstract
Background: With advancements in fetal echocardiography, the diagnosis of supraventricular tachycardia (SVT) is now often made antenatally. There is wide variability in the post-natal management and indications to initiate therapy have not been clearly defined. Esophageal recording and pacing is a useful and minimally invasive tool in the assessment and management of SVT. The proximity of the esophagus to the atria in an anatomically normal individual allows for excellent atrial signal recording as well as noninvasive-programmed stimulation to elicit or terminate reentrant SVT. Transesophageal-pacing study (TEPS) has been used to predict clinical recurrence and efficacy of various management strategies in patients with neonatal SVT, but was never used as a tool to guide post-natal management in newborns with a pre-natal diagnosis of SVT.
Hypothesis: Our primary hypothesis is that TEPS can guide post-natal management in patients with fetal SVT. Secondary objectives were to evaluate if fetal echo accurately diagnoses SVT mechanism and to assess the proportion of fetal SVT that will resolve by the time of birth.
Methods: A retrospective review of all cases of fetal SVT at the Hospital for Sick Children of Toronto from 1999 to 2015 was performed.
Results: A total of 66 patients were included. There were 6 intra-uterine demises. Of the liveborns, 41% had spontaneous SVT during the observation period. Of the 59% remaining, half had inducible SVT during the TEPS. Overall, 70% of patients with a fetal diagnosis of SVT had post-natal recurrence, either spontaneous or inducible. None of the “non-inducible patients” had long-term recurrence.
Conclusions: TEPS is a valid tool to evaluate the need for postnatal therapy in fetal SVT. Based on the results, treatment could be safely avoided in approximately a third of the patients. Futures studies should be done to evaluate long-term spontaneous recurrence of SVT in inducible patients without initiation of treatment
Article Information
vol. 134 no. Suppl 1 A17036
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Pediatric and Fetal Cardiology, Montreal Children’s Hosp, Montreal, Canada
- 2Pediatric Electrophysiology, Golisano Children’s Hosp, Rochester, NY
- 3Pediatric and Fetal Cardiology, Hosp for Sick Children’s Hosp, Toronto, Canada
Abstract 16630: Clinical Predictors of Intraatrial Reentrant Arrhythmias in Adults With Congenital Heart Disease
Pablo Ávila, José María Oliver, Pastora Gallego, Ana González-García, María José Rodríguez-Puras, José Ruíz-Cantador, Ana Campos, Rafael Peinado, Raquel Prieto, Fernando Sarnago, Raquel Yotti, Francisco Fernández-Avilés
Circulation. 2016;134:A16630
Abstract
Background: Intraatrial reentrant tachycardias (IART) are a significant source of morbidity and mortality in adults with congenital heart disease (CHD). The aim of this study was to evaluate the incidence and clinical predictors of IART in a cohort of patients with CHD.
Methods: We conducted a retrospective analysis of 3,311 adults (median age at entry 22.6 years, 50.6% males) with CHD (49% simple, 39% moderate and 12% complex) followed-up in a tertiary center for 37,607 person-years. Predictors of IART were identified by multivariate logistic regression. An external validation was performed in a second cohort of 1,432 patients. ROC curves were used to assess the discriminative ability of model obtained. Survival curves were constructed by Kaplan-Meier method.
Results: Overall, 153 (4.6%) patients presented IART. Risk factors independently related to IART are presented in the Table. The model obtained showed excellent discrimination power (area under the ROC [AUC] curve 0.807, p<0.001) (Figure, panel A) and its predictive ability was confirmed in the validation cohort (AUC 0.754, p<0.001). IART incidence was 0.3%, 3%, 9% and 20% in patients 0, 1, 2 and ≥ 3 risk factors, respectively. Cumulative IART freedom is plotted in the Figure (panel B).
Conclusion: Simple clinical parameters such as univentricular physiology, systemic right ventricle, subaortic or subpulmonary ventricular dysfunction, pulmonary or subpulmonary AV valve regurgitation, previous intracardiac repair and pre-tricuspid shunt were independent predictors of IART in adults with CHD. While IART risk was negligible in patients without any of these factors, their addition progressively increased IART burden.
Article Information
vol. 134 no. Suppl 1 A16630
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Pablo Ávila1;
- José María Oliver2;
- Pastora Gallego3;
- Ana González-García4;
- María José Rodríguez-Puras3;
- José Ruíz-Cantador4;
- Ana Campos3;
- Rafael Peinado4;
- Raquel Prieto1;
- Fernando Sarnago1;
- Raquel Yotti1;
- Francisco Fernández-Avilés5
- 1GUCH Unit, Cardiology department, Gregorio Marañón Hosp, Madrid, Spain
- 2Cardiology, Hosp Gregorio Marañón and Hosp Universitario La Paz, Madrid, Spain
- 3Intercentre Congenital Heart Disease Unit, Hosp Virgen Macarena y Virgen del Rocío, Sevilla, Spain
- 4Cardiology, Hosp Universitario La Paz, Madrid, Spain
- 5Cardiology, Gregorio Marañón Hosp, Madrid, Spain
Abstract 15720: A Prospective Assessment of Optimal Mechanical Ventilation Parameters for Pediatric Catheter Ablation
Christopher M Janson, Scott R Ceresnak, Anne M Dubin, Kara S Motonaga, Glenn E Mann, Madelyn Kahana, Ingrid Fitz-James, Lisa Wise-Faberowski, Komal Kamra, Lynn Nappo, Anthony Trela, Jaeun M Choi, Robert H Pass
Circulation. 2016;134:A15720
Abstract
Introduction: Catheter stability is an important factor in ablation success and may be affected by changes in intrathoracic pressure related to mechanical ventilation. There are few data on the effects of ventilation on catheter stability during ablation procedures in children and young adults. We prospectively characterized the effects of ventilation parameters on catheter movement, with a goal of determining the optimal mode of ventilation for pediatric ablation procedures.
Methods: Subjects < 25 years undergoing ablation for SVT or WPW at 2 centers from 3/15-6/16 were prospectively enrolled and randomized to receive mechanical ventilation with either positive end-expiratory pressure of 5 cm H20 (PEEP) or 0 cm H2O (ZEEP). The ablation catheter was moved to pre-determined standard annular positions [right posterior septal (RPS), right lateral (RL), +/- left lateral (LL)], and movement of the catheter tip was measured using 3D electroanatomic mapping systems under 2 conditions: small tidal volume (STV) (3-5 mL/kg) or large TV (LTV) (6-8 mL/kg), with rate adjusted to achieve equivalent minute ventilation. Multivariate analysis was conducted using a generalized linear mixed model to evaluate the effects of TV, PEEP, annular position, and patient BSA on catheter movement.
Results: 50 subjects [mean age 13.8 years; 24 (48%) PEEP] were enrolled for a total of 234 separate observations of catheter movement: 100 RPS, 100 RL, 34 LL. STV ventilation was associated with significantly reduced catheter movement, compared to LTV at all positions (RPS: 2.4 ± 1.4 vs. 5.0 ± 3.2 mm, p <0.001; RL: 2.4 ± 1.3 vs. 5.9 ± 3.5 mm, p < 0.001; LL: 1.8 ± 1.0 vs. 4.3 ± 1.9 mm, p < 0.001). Presence or absence of PEEP had no effect on catheter movement. In multivariate analysis, STV was associated with a 3.2 +/- 0.4 mm reduction in movement (p < 0.001), and LL location predicted a 1.4 +/- 0.8 mm decrease (p=0.002).
Conclusions: STV ventilation is associated with reduced ablation catheter movement compared to a LTV strategy, independent of PEEP and annular position. A STV strategy may be the preferred approach for mechanical ventilation during pediatric ablations.
Article Information
vol. 134 no. Suppl 1 A15720
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Christopher M Janson1;
- Scott R Ceresnak2;
- Anne M Dubin2;
- Kara S Motonaga2;
- Glenn E Mann3;
- Madelyn Kahana3;
- Ingrid Fitz-James3;
- Lisa Wise-Faberowski4;
- Komal Kamra4;
- Lynn Nappo1;
- Anthony Trela2;
- Jaeun M Choi5;
- Robert H Pass1
- 1Cardiology, Children’s Hosp at Montefiore, Bronx, NY
- 2Cardiology, Lucile Packard Children’s Hosp, Stanford Univ, Palo Alto, CA
- 3Anesthesiology, Children’s Hosp at Montefiore, Bronx, NY
- 4Anesthesiology, Lucile Packard Children’s Hosp, Stanford Univ, Palo Alto, CA
- 5Pediatrics, Children’s Hosp at Montefiore, Bronx, NY
Abstract 14696: The Risk of Atrial Fibrillation in Young Patients With Congenital Heart Disease in Sweden
Zacharias Mandalenakis, Annika Rosengren, Georgios Lappas, Peter Eriksson, Thomas Gilljam, Kristofer Skoglund, Maria Fedchenko, Per-Olof Hansson, Mikael Dellborg
Circulation. 2016;134:A14696
Abstract
Introduction: Patients with congenital heart disease (CHD) are assumed to be a vulnerable group for atrial fibrillation (AF) due to residual shunts, different vessel anatomy, progressive valvulopathy, hypertension and atrial scars from previous heart operations. However, the risk of developing AF in children and young adults with CHD compared to controls has not been established.
Hypothesis: The aim of the present study was to estimate the risk of developing AF in children and young adults with CHD compared to matched controls.
Methods: Data from the Swedish Patient and Cause of Death Registers were used in order to identify all patients with a CHD diagnosis who were born between 1970 and 1993. Diagnoses were coded according to the International Statistical Classification of Diseases (ICD 8th, 9th, and 10th editions). Each patient with CHD was matched by age, sex, and county with 10 controls from the Total Population Register in Sweden who were without any diagnosis of CHD. Follow-up and comorbidity data were collected until 2011.
Results: Among 26,906 patients (51.3 % men) with CHD and 269,053 matched controls, 675 respective 449 developed AF; mean follow-up was 18.5 years. The risk to develop AF was 5.2 times higher (95% [CI] 3.3-8.4, p<0.001) in CHD patients compared to controls. The hazard ratio (HR) for AF in women and men with CHD was 5.2 (95% [CI] 2.9-9.3, p<0.001) and 5.3 (95% [CI] 2.4-11.8, p<0.001), respectively, compared to their controls. Only patients with complex conditions i.e. tetralogy of Fallot, transposition of the great vessels, double inlet ventricle, hypoplastic left heart syndrome, common arterial trunk, and atrioventricular septal defect had a significantly elevated risk to develop AF with a HR of 35.3 (95% [CI] 12.9-96.6, p<0.001).
Conclusions: the risk of AF in children and young adults with CHD was approximately 5 times higher compared to matched controls. The patient group with the most complex congenital defects carried most of the risk and had a significantly 35 times higher risk of AF and could be considered for targeted intervention.
Article Information
vol. 134 no. Suppl 1 A14696
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Zacharias Mandalenakis;
- Annika Rosengren;
- Georgios Lappas;
- Peter Eriksson;
- Thomas Gilljam;
- Kristofer Skoglund;
- Maria Fedchenko;
- Per-Olof Hansson;
- Mikael Dellborg
- Molecular and Clinical Medicine/Cardiology, Sahlgrenska Academy, Medicine, Gothenburg, Sweden
Abstract 14270: Decline in Incidence of Sudden Cardiac Death Caused by Congenital Heart Disease After Implementation of Nationwide Prenatal Ultrasound Screening: A Nationwide Study
Thomas Hadberg Lynge, Alexander Gade Jeppesen, Bo Gregers Winkel, Lars Søndergaard, Bjarke Risgaard, Jacob Tfelt-Hansen
Circulation. 2016;134:A14270
Abstract
Introduction: Congenital heart defects (CHD) affect 8 in every 1,000 live births. CHD is one of the leading causes of sudden cardiac death (SCD) in children and the young. However, the incidence of SCD caused by CHD (SCD-CHD) in the young general population is unknown. The aims of this study were to investigate the incidence and causes of SCD-CHD, how the implementation of nationwide prenatal ultrasound screening in 2005 has changed the epidemiology of SCD-CHD in children, and to which extent CHD was diagnosed antemortem in the SCD cases.
Methods and Results: The study population consisted of all persons aged 0-35 years in Denmark in 2000-09, which equals 24.4 million person-years. All 11,451 deaths were included. By using the in depth descriptive Danish death certificates, 1,094 cases of sudden and unexpected death were identified. Through review of autopsy reports, records from hospitals and general practitioners, discharge summaries, and data from The National Patient Registry on medical history, we identified 103 cases of SCD-CHD (9.4% of all sudden deaths). Median age at time of death was 13 years. In total, only 60 (58%) were diagnosed with CHD prior to death. The annual incidence rate of SCD-CHD was 0.42 per 100,000 person-years among persons aged 0-35 years in the 10-year period. The annual incidence rate for infants (< 1 year old) born prior to implementation of nationwide prenatal ultrasound screening was higher than the incidence rate for infants born after implementation (incidence rate ratio 3.2. 95% CI, 1.4-7.2, p=0.005) (Fig. 1). The most common causes of SCD-CHD were coarctation of the aorta (n=16, 15%) and transposition of the great arteries (n=13, 13%).
Conclusion: A total of 9.4% of all sudden deaths in the young is caused by congenital heart disease. Only 58% of SCD-CHD cases were diagnosed with CHD prior to death. We observed a significant decline in incidence of SCD caused by CHD among infants after implementation of nationwide prenatal ultrasound screening.
Article Information
vol. 134 no. Suppl 1 A14270
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Thomas Hadberg Lynge;
- Alexander Gade Jeppesen;
- Bo Gregers Winkel;
- Lars Søndergaard;
- Bjarke Risgaard;
- Jacob Tfelt-Hansen
- 1The Dept of Cardiology, The Heart Cntr, Copenhagen Univ Hosp, Rigshospitalet, Copenhagen, Denmark
Abstract 12438: Intraoperative Magnesium Reduces Postoperative Arrhythmias in Congenital Heart Surgery Is the Effect Arrhythmia-Specific and Dose-Dependent?
Dingchao He, Nimisha Aggarwal, Xiangming Fan, Yao I Cheng, Charles I Berul, Robert McCarter, Richard A Jonas, Jeffrey P Moak
Circulation. 2016;134:A12438
Abstract
Introduction: Magnesium (MG) has been used to decrease the incidence of postoperative junctional ectopic tachycardia (PO JET); its efficacy on other arrhythmias (A) is less known. We tested the hypotheses that the effect of MG on PO A may be: 1) arrhythmia-specific and 2) dose-dependent.
Methods: 1871 out of a total of 2208 congenital heart surgeries (CHS), performed from 2005 to 2013, were reviewed based on selection criteria. 750 cases did not receive MG, 338 cases received 25 mg/kg MG (25 Mg) and 783 cases received 50 mg/kg MG (50 Mg) after aortic cross clamp release. All procedures were classified according to Aristotle Score (1 to 4). The incidence of 5 PO A categories was recorded: JET, accelerated junctional rhythm (AJR), atrial tachycardia (AT), ventricular tachycardia (VT) and 2°and 3° heart block (HB). Pearson chi-square test and logistic model analyses were used to evaluate the effect of MG on arrhythmia. BSA, Aristotle score, cardiopulmonary bypass, aortic cross-clamp and surgery times were controlled in logistic models.
Results: 1) PO JET was reduced with MG use (0 Mg 15.3%; Mg 7.2%; p<0.001), but without evidence of a difference by dose (25 Mg 7.1%: 50 Mg 7.3%). 2) AJR was reduced with MG use (0 Mg 4.3%: 25 Mg 2.4%: 50 Mg 2.2%, NS between doses). 3) AT was reduced with MG use (0 Mg 9.1%: 25 Mg 3.6 %: 50 Mg 4.0%, NS between doses). 4) VT was reduced in low dose (0 Mg 5.1%: 25 Mg 2.7%; p =0.02), but not at the higher dose (50 Mg 5.5%). 5) PO HB did not differ by Mg use (0 Mg 4.8 %: 25 Mg 3.3 %: 50 Mg 2.6 %). The reduction of PO JET was significantly greater with increasing surgical complexity. Effect of MG was independent of Aristotle score in other A- categories.
Conclusion: In agreement with prior clinical trial results, MG use was preventive of PO arrhythmia; however its effect appeared to be arrhythmia-specific. The occurrence of PO JET, AJR, and AT was reduced with Mg use. The effect of MG on PO VT appeared inversely dose dependent with no effect at higher dose and MG appeared to have no impact on PO HB. In general, higher doses of MG did not enhance PO arrhythmia suppression, but might be proarrhythmic (VT) in patients undergoing CHS. Our results suggest that an intraoperative MG dosage of 25 mg/kg may be optimal.
Article Information
vol. 134 no. Suppl 1 A12438
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Dingchao He1;
- Nimisha Aggarwal2;
- Xiangming Fan1;
- Yao I Cheng3;
- Charles I Berul2;
- Robert McCarter3;
- Richard A Jonas1;
- Jeffrey P Moak2
- 1Cardiac Surgery, Children’s National Med Cntr, Washington, DC
- 2Cardiology, Children’s National Med Cntr, Washington, DC
- 3Biostatistics and Study Methodology, Children’s National Med Cntr, Washington, DC
Abstract 18508: Extubation Failure is Associated With Increased Mortality Following First Stage Single Ventricle Reconstruction
Thomas Scodellaro, Jane McKenzie, Yves d’Udekem, Warwick Butt, Siva Namachivayam
Circulation. 2016;134:A18508
Abstract
Introduction: Extubation following first stage single ventricle reconstruction surgery presents a considerable challenge to the patient and clinician. We aimed to identify the incidence, risk factors and outcomes associated with extubation failure for these patients within our institution.
Methods: A retrospective cohort study was undertaken of all neonates who underwent a Norwood or Damus-Kaye-Stansel procedure between 1 January 2005 and 31 December 2014. Extubation failure was defined as endotracheal reintubation within 48 hours of first extubation attempt.
Results: Extubation failure occurred in 23 of 137 (16.8%, 95%CI 11.0-24.1%) neonates who underwent a trial of extubation. Overall, 42 (30.7%) patients were extubated to room air, 88 (64.2%) to nasal CPAP and 7 (5.1%) high-flow nasal cannulae, but there was no significant difference in extubation failure rates between the three forms of support (p=0.37). The median time to reintubation was 16.7 hours (IQR 3.2-35.2) and failure was due to cardiorespiratory impairment in 14 cases and other causes in 9 (upper airway obstruction=6, sepsis=3). Male infants failed extubation more frequently (63.2% vs 87.0%, p=0.02), whilst age, weight, cardiac diagnosis, shunt type, intraoperative perfusion times, time to extubation, postoperative fluid balance and pre-extubation blood gas results were not related to extubation outcome. Reintubation within 48 hours was significantly associated with an increased total duration of mechanical ventilation (5.7 days vs 11.4, p<0.001), intensive care length of stay (8.9 days vs 16.7, p=0.02), intensive care mortality (3.5% vs 19.4%, p=0.03) and in-hospital mortality (6.1% vs 30.4%, p<0.001). Children with a cardiorespiratory impairment causing extubation failure had a higher mortality compared to other causes (57.1% vs. 0%, p=0.007).
Conclusions: There is a high incidence of extubation failure following first stage single ventricle reconstruction and this is associated with considerably worse patient outcomes. Cardiorespiratory impairment as a cause for extubation failure is associated with high mortality.
Article Information
vol. 134 no. Suppl 1 A18508
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Paediatric Intensive Care Unit, The Royal Children’s Hosp, Parkville, Australia
- 2Dept of Cardiac Surgery, The Royal Children’s Hosp, Parkville, Australia
Abstract 18157: Mortality, Rehospitalizations and Costs of Congenital Heart Disease Managed Operatively in the First Year of Life
Claire M Lawley, Samantha J Lain, Gemma A Figtree, Gary F Sholler, David S Winlaw, Christine L Roberts
Circulation. 2016;134:A18157
Abstract
Introduction: Hospitalizations for cardiac procedures and associated readmissions are an expected part of management for many children with congenital heart disease (CHD). The full burden of these hospitalizations including readmissions and costs to the health system is unknown.
Hypothesis: Children undergoing a cardiac procedure in the first year of life experience increased mortality and rehospitalizations outside of the immediate perioperative period, quantifiable using population-based data.
Methods: A longitudinal record-linkage population-based cohort study was performed examining a twelve-year period 2001-2012, in New South Wales (NSW), Australia. Data were obtained from NSW Admitted Patient Data Collection, NSW Perinatal Data Collection and Register of Births, Deaths and Marriages. Children undergoing a cardiac procedure (surgical or catheter-based) in the first year of life were identified using procedure codes from the Australian Classification of Health Interventions.
Results: Rate of cardiac procedures in the first year of life over the study period was steady at 2.5 children per 1 000 live births, accounting for 2 722 children. Children undergoing isolated closure of a patent ductus arteriosus (n=416) were excluded from further analysis. Of the remaining 2 306 children, 50% required readmission in the first year of life, of these over 50% were unplanned. Average total cost per infant for the initial procedure admission was $67 054 AUD (95% CI $63,124 – $70,984) with a median length of stay (LOS) of 13 days (IQR 8-23). Average cost per readmission in the first year of life was $11,342 (95% CI 10,361-$12,323) with average LOS of 5.1 days. Mortality rate in the first 30 days following initial procedure was 3.1% (72/2306). Mortality rate by age 1 year was 7.1% (164/2306) and for the subgroup who had surgery in the neonatal period 13.8% (131/981).
Conclusion: The risk of mortality in operatively-managed CHD extends beyond the immediate perioperative period. Children undergoing a cardiac procedure in their first year are often readmitted to hospital for both further planned procedures and unplanned reasons such as infection. These readmissions represent the significant burden of illness and pose a substantial financial cost to the health system.
Article Information
vol. 134 no. Suppl 1 A18157
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Claire M Lawley1;
- Samantha J Lain2;
- Gemma A Figtree3;
- Gary F Sholler4;
- David S Winlaw4;
- Christine L Roberts2
- 1North Shore Heart Rsch Group and Clinical Population Perinatal Health Rsch, Univ of Sydney, Sydney, Australia
- 2Clinical Population Perinatal Health Rsch, Univ of Sydney, Sydney, Australia
- 3North Shore Heart Rsch Group, Univ of Sydney, Sydney, Australia
- 4Heart Cntr for Children, The Children’s Hosp at Westmead, Sydney, Australia
Abstract 18169: Thromboelastography Predicts Peri-Operative Bleeding Outcomes in Pediatric Patients Undergoing Cardiac Surgery
Sirisha Emani, David Zurakowski, Michelle Mulone, James DiNardo, Juan Ibla, Sitaram M Emani
Circulation. 2016;134:A18169
Abstract
Introduction: Peri-operative bleeding is the most common morbidity in pediatric patients undergoing cardiac surgery. Although thromboelastography (TEG) has been utilized in select patients, its ability to predict bleeding in this population has not been established.
Hypothesis: We hypothesize that TEG parameters predict bleeding outcomes peri-operatively in pediatric patients undergoing cardiac surgery.
Methods: TEG was performed in 450 pediatric patients undergoing complex cardiac surgery requiring cardiopulmonary bypass (CPB). TEG was performed at baseline (T0), post-protamine in the OR (T1), during the first ICU labs (T2), and 24-hours post-surgery (T3). TEG values from all time points were compared in patients with and without perioperative bleeding. Bleeding was defined by several methods – objective (transfusion requirements, need for re-exploration) or subjective (time spent controlling bleeding in OR, and caregiver assessment).
Results: Although none of the TEG parameters were significantly different between bleeding and non-bleeding patients at the T0, T2, or T3 time points, significantly higher ADP-induced platelet inhibition at T0 was observed in bleeding patients (37.6%) compared to non-bleeding patients (13.5%) (p<0.0001). At T1 time point, abnormal TEG maximum amplitude (MA) was associated with perioperative bleeding. Perioperative bleeding (objective) occurred in 39.4% of patients with abnormal TEG, compared to 27.7% of patients with normal MA (p=0.03). By multivariable regression analysis abnormal TEG MA was independently associated with perioperative bleeding. Patients with abnormal MA who were administered platelet transfusion had lower bleeding in the ICU (12.1%) compared to those without transfusion (21.4%). On the other hand, there was no difference in the bleeding rate in patients with or without platelet transfusion with normal MA.
Conclusions: Inhibition of platelet function pre-surgery may predict peri-operative bleeding. Abnormal TEG MA is associated with perioperative bleeding. Prophylactic platelet transfusion in the OR may not be useful to prevent bleeding in the ICU when patients are not bleeding and with normal MA.
Article Information
vol. 134 no. Suppl 1 A18169
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Cardiac surgery, Boston Children’s Hosp, Boston, MA
- 2Anesthesia, Boston Children’s Hosp, Boston, MA
Abstract 17115: Airway Anomalies and Respiratory Factors Significantly Impact Post-operative Intensive Care Management in Patients With Trisomy 13 and 18 Following Cardiac Surgery
Sara K Swanson, Kurt R Schumacher, Richard G Ohye, Jeff D Zampi
Circulation. 2016;134:A17115
Abstract
Introduction: Congenital heart disease is common in individuals with trisomy 13 and 18 (T13/18). While excellent survival after cardiac surgery is reported, there are limited data describing the impact of comorbidities, specifically airway anomalies, on the current intensive care (ICU) management strategies and outcomes.
Hypothesis: Airway anomalies are common and significantly impact post-operative management and outcomes in T13/18 patients following cardiac surgery when compared to an age-matched cohort.
Methods: We performed a retrospective nested case-control study of all patients with known T13/18 who underwent cardiac operations at our institution from 1994-2014. A control group of 3:1 age-matched non-T13/18 patients who underwent a similar surgery was used for comparison. Patient demographics and clinical characteristics including post-operative course and management were compared. Descriptive statistics (median, interquartile range [IQR]) and Wilcoxon unpaired rank t-tests were used to determine significant differences.
Results: Fourteen patients with T13 (14%) or T18 (86%) underwent cardiac surgery (median age: 93 days) for ventricular septal defect (VSD) (n=8), VSD with coarctation (n=2), atrioventricular septal defect (n=2) and tetralogy of Fallot (n=2). There was 1 mortality. Hospital length of stay (LOS) was longer in the T13/18 cohort (31 days [IQR: 20-40] versus 8 days [IQR: 6-15], p<0.0001), as was ICU LOS (14 days [IQR: 7-24] versus 4 days [IQR: 2-5], p<0.0001). The duration of intubation (7 versus 2 days, p < 0.0001) was longer as was the duration of non-invasive positive pressure ventilation (NIPPV) (8 versus 3 days, p < 0.0002). More T13/18 patients required NIPPV (71% vs. 42%) and 2 required a tracheostomy. Airway anomalies were found in 6 (43%) T13/18 patients, all bronchomalacia, compared to 1 control patient (2%) born prematurely with chronic lung disease.
Conclusions: The majority of T13/18 patients survive cardiac surgery, but have a prolonged hospital course compared to controls. T13/18 patients appear to have increased airway complications, including the need for tracheostomy or prolonged NIPPV. Parental guidance prior to cardiac surgery should include a discussion about post-operative airway management.
Article Information
vol. 134 no. Suppl 1 A17115
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Sara K Swanson;
- Kurt R Schumacher;
- Richard G Ohye;
- Jeff D Zampi
- Pediatric Cardiology, Univ of Michigan, Ann Arbor, MI
Abstract 16636: Patient and Hospital-level Predictors of Early Unplanned Pediatric Cardiac Intensive Care Unit Readmissions
Andrew H Smith, Vijay Anand, Mousumi Banerjee, Katherine E Bates, Marissa A Brunetti, David S Cooper, Jessica Lehrich, Kshitij P Mistry, Sara K Pasquali, Andrew Y Shin, Sarah Tabbutt, Michael G Gaies
Circulation. 2016;134:A16636
Abstract
Background: Unplanned readmissions to pediatric cardiac intensive care units (CICU) are associated with higher mortality and greater resource utilization. Patient and hospital factors leading to CICU readmission remain unknown and differences in readmission rates across hospitals have not been reported.
Methods: We examined initial CICU encounters in the Pediatric Cardiac Critical Care Consortium (PC4) registry from 10/2013 to 3/2016. The primary outcome was unplanned CICU readmission <48 hours from CICU discharge. Patient, encounter, and hospital factors were compared. Those associated with the outcome (p<0.1) were included in a multivariable logistic regression model with treating hospital as a fixed effect. Patient factors associated with readmission (p<0.05) formed a model to calculate adjusted hospital readmission rates.
Results: Of 11,673 included CICU encounters, 62% were surgical (v. medical) and 70% were planned (v. unplanned). There were 175 (1.5%) unplanned CICU readmissions within 48 hours, most commonly for respiratory (32%) or cardiac (27%) conditions. Univariate comparisons showed no association between unplanned readmission and hospital factors including nurse hours per patient day, 24/7 in-house CICU attending and use of early warning scores on ward units. In multivariable analysis, only extracardiac anomaly (OR 1.4 [95%CI 1.1-2.0]) greater surgical complexity (OR 1.8 [95%CI 1.2-2.8]), and treating hospital (p=0.01) were associated with early unplanned readmission. After adjusting for patient-level factors, we observed four-fold variation in unplanned readmission rates across hospitals (Figure).
Conclusions: Patient factors related to surgical complexity and extracardiac anomalies are associated with early unplanned CICU readmission. Future quality improvement depends on uncovering hospital practices impacting the wide variation in readmission rates we identified across hospitals.
Article Information
vol. 134 no. Suppl 1 A16636
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Andrew H Smith1;
- Vijay Anand2;
- Mousumi Banerjee3;
- Katherine E Bates4;
- Marissa A Brunetti5;
- David S Cooper6;
- Jessica Lehrich7;
- Kshitij P Mistry8;
- Sara K Pasquali4;
- Andrew Y Shin9;
- Sarah Tabbutt10;
- Michael G Gaies4
- 1Pediatrics, Monroe Carell Jr. Children’s Hosp at Vanderbilt, Vanderbilt Univ Sch of Medicine, Nashville, TN
- 2Critical Care, Stollery Children’s Hosp, Univ of Alberta, Edmonton, Canada
- 3Internal Medicine, Cntr for Healthcare Outcomes & Policy, Univ of Michigan, Ann Arbor, MI
- 4Pediatrics and Communicable Diseases, CS Mott Children’s Hosp, Univ of Michigan Med Sch, Ann Arbor, MI
- 5Anesthesiology and Critical Care Medicine, Children’s Hosp of Philadelphia and Perelman Sch of Medicine, Univ of Pennsylvania, Philadelphia, PA
- 6Pediatrics, Cincinnati Children’s Hosp Med Cntr, Univ of Cincinnati College of Medicine, Cincinnati, OH
- 7Internal Medicine, Cntr for Healthcare Outcome and Policy, Univ of Michigan, Ann Arbor, MI
- 8Pediatrics, Levine Children’s Hosp, Charlotte, NC
- 9Pediatrics, Lucille Packard Children’s Hosp Stanford, Stanford Univ Sch of Medicine, Palo Alto, CA
- 10Pediatrics, Univ of California San Francisco Benioff Children’s Hosp, San Francisco, CA
Abstract 16659: What Contributes to the Difference in Cost Between the CICU and NICU in Neonates Undergoing Congenital Heart Surgery?
Joyce T Johnson, Kirsen Sullivan, Xiaoming Sheng, Tom Greene, David Bailly, Aaron Eckhauser, LuAnn Minich, Nelangi Pinto
Circulation. 2016;134:A16659
Abstract
Introduction: The mechanisms for previously reported increased costs of care for neonatal congenital heart surgery (CHS) in a neonatal intensive care unit (NICU) compared to a cardiac (CICU) or pediatric ICU (PICU) are not known. We leveraged decomposition analysis, commonly used in labor economics, to understand determinants of differences in cost by location of care.
Methods: Patient and center data were collected on neonates (<30 days old) who had CHS from 2003-13 using the Pediatric Health Information Systems. Differences in hospital costs adjusted for region and inflation based on care location (NICU vs. CICU/PICU) were modeled with gamma regression. A decomposition analysis with bootstrapping determined characteristic (explainable by differing covariate levels) and structural effects (if covariates are held constant). Covariates included hospital volume, gender, admission age, RACHS-1 score, prematurity, payor, race, admission year, syndrome, infection, ECMO and delayed sternal closure.
Results: For 20,595 neonates (NICU 47%, CICU/PICU 53%), NICU admission was associated with $22,222±3,430 higher unadjusted cost (p<0.001) compared to CICU/PICU admission. Characteristic effects accounted for $27,015±2,285 higher cost in the NICU (p<0.001). Contributing to this effect were higher rates of infection ($12,602±862, p<0.001), prematurity ($2,485±448, p<0.001), syndromes ($1,379±187, p<0.001), lower hospital volume ($10,587±731, p<0.001) and lower admission age ($3,979±823, p<0.001) for the NICU vs. CICU/PICU. Aggregate structural effects were not associated with cost differences (p=0.1), but were significantly different for some covariates examined individually, including higher NICU costs when admission age ($5,220±1361, p<0.001) and infection rates were held constant ($3,485±1334, p=0.009).
Conclusions: While many factors increasing cost of CHS care in the NICU may not be modifiable, the infection rates which contributed most to higher costs (compared to CICU/PICU) is a modifiable target. Higher costs in the NICU vs. CICU/PICU even when infection and admission age are constant may be secondary to differing overhead cost structures that require further delineation.
Article Information
vol. 134 no. Suppl 1 A16659
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Joyce T Johnson1;
- Kirsen Sullivan2;
- Xiaoming Sheng3;
- Tom Greene4;
- David Bailly5;
- Aaron Eckhauser6;
- LuAnn Minich7;
- Nelangi Pinto7
- 1Pediatric Cardiology, Ann & Robert H. Lurie Children’s Hosp of Chicago, Chicago, IL
- 2Biostatistics, Univeristy of Utah, Salt Lake City, UT
- 3Biostatistics, Univ of Utah, Salt Lake City, UT
- 4Epidemiology, Univ of Utah, Salt Lake City, UT
- 5Pediatric Critical Care, Univ of Utah, Salt Lake City, UT
- 6Pediatric Cardiothoracic Surgery, Univ of Utah, Salt Lake City, UT
- 7Pediatric Cardiology, Univ of Utah, Salt Lake City, UT
Abstract 15355: Dysnatremia is Associated With Adverse Outcomes in Pediatric Patients After Surgery Under Cardiopulmonary Bypass for Congenital Heart Disease
Andrea Ontaneda, Javier Lasa, Ayse Akcan-Arikan, Jorge Coss-Bu, Lara Shekerdemian
Circulation. 2016;134:A15355
Abstract
Background: Sodium imbalances are one of the most common electrolyte disorders in ICU and have been associated with adverse outcomes in many patient groups. Few studies have investigated associations between dysnatremia and outcomes in children after surgery for congenital heart disease (CHD).
Methods: Retrospective chart review of children (01/12 to 01/15) after CHD surgery with cardiopulmonary bypass (CPB). Infants operated at < 37 weeks of gestation or > 18 years of age were excluded. Data collected: age, gender, weight, Risk Adjusted Congenital Heart Surgery Score (RACHS-1) classification; mechanical ventilation (MV), CPB and cross clamp (CC) times; serum sodium (Na) 24, 48 and 72 hrs after surgery; hospital length of stay (LOS), adverse neurological events (strokes or seizures) and mortality. Na level <135mmol/L was defined as hyponatremia and >145 mmol/L as hypernatremia. Comparisons between groups by logistic regression analysis.
Results: 1177 encounters (55.7% males) were included. Median (IQR) age 13.6 (3.4-67) months, weight 8.9 (4.9-18.6) kg. 180 (15.3%) patients were in RACHS-1 category 4-6. Hospital LOS 8 (5-15) days; MV time 23.5 (7.1-58) hours; CPB time 138 (92-192) min; CC time 77 (38-121) min. Post-operative dysnatremia was 46.3%; 16.14% had hyponatremia, 27.7% hypernatremia and 1.44% had both in the first 72 hours. Post-operative mortality (1.7%) was associated with hypernatremia at 24 hrs (Odds Ratio (OR) 4.9 [2.2-11], p=0.0001); 48 hrs (OR 4.8 [2.0-11], p=0.0003); 72 hrs (OR 5.3 [2.2-12.7], p=0.0002); no association between hyponatremia and mortality. In a univariate logistic regression analysis, hypernatremia, not hyponatremia, at all time points was significantly associated with adverse neurological event at 24 hrs(OR 3.9 [1.6-9.5], p=0.0028); 48 hrs (OR 3.3 [1.3-8.8], p=0.0163) and 72 hrs (OR 3.4 [1.3-9.3], p=0.0139). In a multivariable model controlling for age, LOS and CC times, prolonged CPB time was associated with post-operative hypernatremia (OR1.01 [1.00-1.01], p=0.0012).
Conclusions: Perioperative dysnatremia was a common finding in pediatric cardiac surgical patients. Hypernatremia was more prevalent than hyponatremia, and was associated with increased CPB time, adverse neurological outcome and mortality.
Article Information
vol. 134 no. Suppl 1 A15355
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Andrea Ontaneda;
- Javier Lasa;
- Ayse Akcan-Arikan;
- Jorge Coss-Bu;
- Lara Shekerdemian
- Pediatric critical care, Texas Children’s Hosp, Houston, TX
Abstract 14780: Analytical Identification of Stable Hemodynamic Conditions in Patients With Transposition of the Great Arteries
Ryo Inuzuka, Hideaki Senzaki
Circulation. 2016;134:A14780
Abstract
Introduction: Newborns with transposition of the great arteries (TGA) have systemic and pulmonary circulation in parallel; thus, mixing of both circulations is essential to maintain appropriate oxygen saturation level. However, shunt flow through a patent ductus arteriosus (PDA), ventricular septal defect (VSD), and atrial septal defect (ASD) may result in hemodynamic instability against a decrease in pulmonary arterial resistance. This tradeoff between oxygen saturation and hemodynamic stability should be fully understood for better management of patients with this unique circulation, but has never been elucidated.
Methods: We developed a lumped parameter model for TGA circulation based on the 3-element Windkessel model coupled with the time-varying elastance model of the ventricles. We examined the impacts of the shunt sizes and locations on oxygen saturation and cardiac index (CI) by combining various sizes of ASD, VSD and PDA. Contribution of each shunt to the mixing between systemic and pulmonary circulation was calculated based on the difference in oxygen saturation in each chamber.
Results: Seven combinations of the shunt sizes achieving oxygen saturation over 70% were identified and shunt through ASD had the greatest contribution to the mixing as shown in the Figure. Moreover, 50% reduction in pulmonary vascular resistance resulted in a 7% increase in oxygen saturation level and 4% increase in CI in those dependent on an ASD shunt (model A and C), and a 13% increase in oxygen saturation level and 7% decrease in CI in those dependent on a PDA shunt (model B and D). All the models dependent on a VSD shunt showed reduction in CI in response to reduction in pulmonary vascular resistance.
Conclusions: In clinician’s choice between prostaglandin infusion and atrial septostomy, the model predicted that utilizing an ASD shunt to maintain oxygen saturation level would be beneficial as it is more hemodynamically stable and more efficiently raises oxygen saturation.
Article Information
vol. 134 no. Suppl 1 A14780
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Pediatrics, Univ of Tokyo, Tokyo, Japan
- 2Pediatric Cardiology, Saitama Med Univ, Saitama, Japan
Abstract 13168: High Morbidities in Hospitalized Adolescents With Both Single and Biventricle Congenital Heart Disease
Aparna Kulkarni, Patricia Zybert, Shelby Kutty, Richard Neugebauer, Brett Anderson
Circulation. 2016;134:A13168
Abstract
Introduction: Quality of life in adolescents with single ventricle (SV) is known to be significantly impaired. In this study, we sought to quantify inpatient morbidities for single ventricle (SV) versus biventricle (BV) adolescents using data from the Pediatric Health Information System (PHIS).
Methods: The PHIS database was queried for all admissions in adolescents aged 12-18 years (1/1/2004–12/31/2013) coded for CHD. Patients were categorized as SV or BV based on their primary and secondary ICD-9 diagnostic and/or procedure codes. Patient characteristics, diagnoses, procedures, vital status and standardized costs were examined.
Results: 4,267 adolescents were admitted to 42 children’s hospitals over 10 years, accounting for 8,512 hospitalizations. Among patients, 24.6% were SV, 64.1% BV and 11.3% unclassifiable. Among hospitalizations, 29.5% were SV patients, 56.1% were BV patients, and 14.4% were unclassifiable. SV patients were more likely to have multiple hospitalizations than BV patients [51.0% vs 37.9%, p ≤ 0.001]. Mean age for adolescent admissions were similar for SV and BV hospitalizations [mean (SD) 15.0 (1.9) years vs 14.8 (1.9)]. Median lengths of stays (LOS) for BV hospitalizations were 2 days, [IQR 1-5] and 2 days [IQR 1-4] for SV hospitalizations, with a higher proportion of patients with LOS>2 days in the BV group [46.9%] than SV group [38.5%, p<0.001]. BV hospitalizations were more likely to entail ICU stays [36.6% vs 26.1%, p ≤0.001], to require mechanical ventilation [20.2% vs 8.8%, p ≤0.001] and had higher median total costs [$14,500, IQR $4140-$40,900 vs $8250, IQR $2,440-$23,300, p≤0.001]. There were no differences between SV and BV hospitalizations in use of one or more electrophysiological studies [16.4% vs 18.2%, p=0.062] or reporting of one or more tachyarrhythmias [7.5% vs 7.0%, p=0.505]. Procedure codes for pacemaker/intracardiac defibrillator were higher among SV hospitalizations [6.1% vs 4.1%, p≤0.001], as was an associated diagnosis of heart transplantation [2.3% vs 0.5%, p≤0.001].
Conclusions: Adolescents with CHD requiring hospitalizations are resource intensive irrespective of their CHD classification.
Article Information
vol. 134 no. Suppl 1 A13168
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Pediatrics, Children’s Hosp at Montefiore, Bronx, NY
- 2Statistics, Columbia Univ, New York, NY
- 3Pediatrics, Children’s Hosp and Med Cntr, Omaha, NE
- 4Mailman Sch of Public Health, Columbia Univ, New York, NY
- 5Pediatrics, Columbia Univ Med Cntr, New York, NY
Abstract 12728: Impact of Cardiac Function and Hemodynamics on Mortality in Patients After the Fontan Operation
Hideo Ohuchi, Yosuke Hayama, Jun Negishi, Kanae Noritake, Aya Miyazaki, Isao Shiraishi
Circulation. 2016;134:A12728
Abstract
Background: High central venous pressure (CVP) with low cardiac output (CO) characterizes Fontan hemodynamics. However, the association of these characteristics with prognosis remains controversial, especially in adult patients.
Purpose: To elucidate associations of Fontan hemodynamics with the mortality.
Method and Results: We evaluated cardiac function and hemodynamics in 431 consecutive Fontan survivors (≥ 6 months), including 170 adults, that included CVP (mmHg), cardiac index (CI; L/min/m2), systemic ventricular end-diastolic volume index (EDVI; ml/m2) and ejection fraction (EF; %), and arterial oxygen saturation (SpO2; %). The latest variables were compared with the 5-year all-cause mortality. During follow-up, 22 child and 15 adult patients died. In child and adult patients, higher CVP (hazard ratio [HR]:1.36 and 1.29, respectively, p < 0.01-0.0001), larger EDVI (HR: 1.01 and 1.03, respectively, p < 0.01 for both) and lower SpO2 (HR: 0.93 and 0.90, p < 0.001 for both) predicted the mortality. Lower EF predicted the mortality only in child patients (HR: 0.42, p < 0.0001). There was an opposite impact of CI on mortality (p < 0.001), i.e., lower CI in child patients (HR: 0.40, 95% confidence interval: 0.20-0.79, p < 0.01), whereas higher CI in adult patients (HR: 2.21, 95% confidence interval: 1.13-4.07, p < 0.05) predicted the mortality and the cutoff value was 2.46 and 2.90, respectively.
Conclusions: High-CO-associated CVP with preserved EF predicted mortality in adult Fontan patients. The failing pathophysiology in some long-term Fontan survivors may differ from that in child patients although both of them have high CVP in common.
Article Information
vol. 134 no. Suppl 1 A12728
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Pediatric Cardiology, National Cerebral and Cardiovascular Cntr, Osaka, Japan
- 2Pediatric Cardiology, National Cerebral and Cardiovascular Cntr, Suita, Japan
Abstract 11485: New Metrics of Postoperative Mechanical Ventilation Duration After Congenital Heart Surgery Reveal Variation Across Hospitals
Michael Gaies, David Werho, Nancy Ghanayem, Sarah Tabbutt, John Costello, Mark Scheurer, Sara K Pasquali, Janet Donohue, Wenying Zhang, Mousumi Banerjee, Steven Schwartz
Circulation. 2016;134:A11485
Abstract
Background: Pediatric cardiac surgical programs aim to limit duration of postoperative mechanical ventilation (POMV) to reduce complications and hospital stay. Measuring casemix-adjusted duration of POMV across hospitals might elucidate differential performance and identify improvement opportunities.
Methods: All surgical hospitalizations in the Pediatric Cardiac Critical Care Consortium (PC4) clinical registry from 10/2013-8/2015 were used to create a model predicting casemix-adjusted total duration of POMV using zero-inflated negative binomial regression and validated with 1000 bootstrap samples. From the model we developed metrics based on observed-to-expected POMV: early extubation success/failure, POMV reduction, and total hours of POMV saved/lost (Table 1). We ranked hospitals on each metric (1-15, 1=best) and calculated an average ranking across metrics to identify high and low performing hospitals.
Results: The cohort included 4739 hospitalizations from 15 hospitals: 53% were infants and 22% had high complexity surgery. The final model included age, weight-for-age z-score, prematurity, pre-operative MV, extracardiac anomalies, procedure complexity, and bypass time. The model was well-calibrated to predict mean duration of POMV for groups of patients. Table 1 displays the range and median of hospital rates on each of the four metrics, demonstrating variation across the group. The average ranks across these POMV duration metrics suggested two positive outlying hospitals (average rank across all 4 metrics = 1.75) and five hospitals with consistently lower performance (average 8.75-11.25).
Conclusions: We developed novel casemix-adjusted metrics of hospital performance to limit duration of POMV following pediatric cardiac surgery, and identified wide variation in relative performance across centers. These metrics may suggest opportunities for improvement when evaluated in context with other perioperative quality measures.
Article Information
vol. 134 no. Suppl 1 A11485
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Michael Gaies1;
- David Werho2;
- Nancy Ghanayem3;
- Sarah Tabbutt4;
- John Costello5;
- Mark Scheurer6;
- Sara K Pasquali1;
- Janet Donohue1;
- Wenying Zhang7;
- Mousumi Banerjee8;
- Steven Schwartz9
- 1Pediatrics and Communicable Diseases, Univ of Michigan, Ann Arbor, MI
- 2Pediatrics, Stanford Univ Sch of Medicine, Palo Alto, CA
- 3Pediatrics, Med College of Wisconsin, Milwaukee, WI
- 4Pediatrics, Univ of California-San Francisco Sch of Medicine, San Francisco, CA
- 5Pediatrics, Feinberg Sch of Medicine Northwestern Univ, Chicago, IL
- 6Pediatrics, Med Univ of South Carolina, Charleston, SC
- 7Congenital Heart Cntr, Univ of Michigan, Ann Arbor, MI
- 8Biostatistics, Univ of Michigan, Sch of Public Health, Ann Arbor, MI
- 9Critical Care Medicine and Paediatrics, Univ of Toronto Faculty of Medicine, Toronto, Canada
Abstract 19823: Predictors of Post Cardiac Surgery Rehabilitation Therapy in Congenital Heart Disease Patients
Ana Ubeda Tikkanen, Meena Nathan, Lynn A Sleeper, Marisa Flavin, Ana Lewis, Donna Nimec, John E Mayer, Pedro del Nido
Circulation. 2016;134:A19823
Abstract
Introduction: Congenital heart disease (CHD) patients are at risk of motor, cognitive, speech and feeding difficulties after cardiac surgery. Rehabilitation therapy (RT) can decrease the post-surgical functional morbidity. Our goal was to describe predictors of RT in CHD patients.
Hypothesis: Palliative surgery patients have greater RT needs.
Methods: This is a retrospective cohort study on CHD patients < 18 years repaired on cardiopulmonary bypass (CPB) at our center from 01/01/2013 to 01/31/2015. Demographic; pre, intra and postoperative; and RT (physical, occupational, speech, feeding therapy and neurodevelopment intervention) data were collected. Case complexity was determined by STS/EACTS mortality categories (STAT) and residual lesions by Technical Performance Score (TPS). Primary outcome was need for RT, primary predictor was full vs. palliative repair. Multivariable model determined the association between RT and pre and intraoperative predictors.
Results: Of 1415 subjects, 253(17.9%) had palliative repairs. Median age at surgery was 1.6(IQR 0.3, 6.1) years, 627(44.3 %) were males, 226(16%) were neonates, 116(8.2%) were premature, 292(20.6%) had a genetic syndrome. STAT category was ≥ 3 in 536(37.9%), TPS was 3 (major residua) in 136(9.6%) subjects, mean CPB time was 126.1(±65.1) minutes.
A total of 586(41%) subjects required RT after surgery, with 180/226(79.6%) neonates requiring RT, feeding therapy 130/226(57.5%) was the most common. On multivariable analysis, palliative repair, prematurity, neonates, genetic syndrome, higher STAT category, class 3 TPS and longer CPB were associated with need for RT.
Conclusions: Post CHD surgery RT needs are high, with nearly half the patients needing some form of therapy. Age, preterm birth, genetic syndrome, prolonged pre-surgical hospital stay, case complexity, type of repair, and presence of residua predict the need for RT, thus aiding decision making on resource allocation for appropriate RT.
Article Information
vol. 134 no. Suppl 1 A19823
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Ana Ubeda Tikkanen1;
- Meena Nathan2;
- Lynn A Sleeper3;
- Marisa Flavin4;
- Ana Lewis2;
- Donna Nimec1;
- John E Mayer2;
- Pedro del Nido2
- 1Pediatric Rehabilitation, Spaulding Rehabilitation Hosp, Boston, MA
- 2Cardiovascular Surgery, Boston Children’s Hosp, Boston, MA
- 3Cardiology, Boston Children’s Hosp, Boston, MA
- 4Rehabilitation, Spaulding Rehabilitation Hosp, Boston, MA
Abstract 19273: Short and Long Term Outcomes in Children With Trisomy 21 Following Interventions for Congenital Heart Disease (CHD): A Study From the Pediatric Cardiac Care Consortium (PCCC).
Jennifer K Peterson, Kirsti G Catton, Lazaros Kochilas, Shaun P Setty
Circulation. 2016;134:A19273
Abstract
Methods: Retrospective review of the PCCC for 7809 patients (4081 females) with Trisomy 21 who underwent transcatheter or surgical intervention for CHD from 1982 to 2007. Short term outcomes included in-hospital mortality, need for extracorporeal life support (ECLS), and need for permanent pacemaker. Outcomes of 30 day mortality, long term survival, and transplant status were obtained for patients with available direct identifiers up to April 2003 by linkage to the National Death Index (NDI) and the United Network for Organ Sharing.
Results: The most common surgical procedures were endocardial cushion defect repair (3197/8511, 37.6%), ventricular septal defect repair (1728/8511, 20.3%), and Tetralogy of Fallot repair (589/8511, 6.9%). In-hospital mortality was 5% (334/6694) for corrective procedures, 28.7% (72/251) for palliative procedures, and 34% (38/112) single ventricle procedures. Forty of 7057 patients required ECLS and 140 (2%) initial pacemaker implantation. Six patients underwent transplant; 5 cardiac, 1 lung. Transcatheter interventions were performed in 593 patients; the most common interventions were patent ductus arteriosus occlusion (395/833, 47.4%), pulmonary arterioplasty/stent (137/833, 16.4%), and atrial septal defect closure (133/833, 15.9%). Catheterization mortality was 27/3979 (0.7%). Late deaths occurred in 468 patients out of 4294 discharged alive and submitted to NDI (including 15 with 30 day mortality). Survival by treatment pathway is shown in the Figure. The most common causes of late mortality were cardiac (199/453, 43.9%), infection (71/453, 15.7%), and pulmonary hypertension (46/453, 10.2%).
Conclusions: Long term survival conditioned after CHD interventions in patients with Trisomy 21 approaches 92% (95% CI 91.3-92.9%) for corrective procedures, 64% (95% CI 55.9-72.9%) for palliative procedures, and 66% (95% CI 50.5-81.5%) for single ventricle procedures. Causes of late deaths are predominately cardiac.
Article Information
vol. 134 no. Suppl 1 A19273
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Heart & Vascular Institute, Long Beach Memorial/Miller Children’s & Women’s Hosp, Long Beach, CA
- 2Sibley Heart center Cardiology, Emory Univ, Atlanta, GA
Abstract 18564: Redefining the Incidence and Impact of Acute Brain Injury After Neonatal Cardiac Surgery
Charlotte Verrall, Karen Walker, Alison Loughran-Fowlds, Chris Troedson, Julian Ayer, Jonathan Egan, Robert Halliday, Yishay Orr, Gary Sholler, Gary Sholler, Nadia Badawi, David S Winlaw
Circulation. 2016;134:A18564
Abstract
Introduction: Whilst the reported incidence of acute brain injury (ABI) after paediatric cardiac surgery at all ages is around 2%, the true incidence and impact of ABI in neonatal cardiac surgery are not well defined and are the focus of this study.
Methods: Neonates undergoing cardiac surgery with cardiopulmonary bypass (CPB) between July 2011 and December 2014 were identified. 134 patients were enrolled; 29 Norwood cases (22%) and 105 non-Norwood cases (78%). Clinical data were retrospectively collected including neurodevelopmental assessments (Bayley-III Scales) at one year. All imaging abnormalities as well as seizures and abnormal EEG results were recorded. Post-operative changes were considered ABI.
Results: Preoperative neuroimaging or EEG abnormalities were evident in 6%, with an ABI rate of 17% post-operatively, totalling 23% with pre and/or post-operative neurologic abnormality. There were higher rates of abnormality in the Norwood group compared to the non-Norwood group (41% vs 18%, p=0.008). Significant predictors of ABI on multivariate regression analysis were use of ECMO (p<0.001) and cardiac arrest (p=0.01). Bayley-III assessments were complete in 50% of the cohort at 1 year of age. Those with recorded neurologic abnormalities had significantly worse developmental delay (scoring below average in two or more domains) compared to those with no abnormality (86% vs 44% respectively, p=0.005). ABI was a predictor of delay (p=0.012) on univariate analysis. The only other variable found to predict neurodevelopmental delay was length of stay (p=0.026). No other clinical or operative characteristics, including circulatory arrest, were predictive.
Conclusion: In neonates undergoing CPB, the rate of ABI is substantially higher than previously described. The incidence of ABI varies according to procedural complexity and is underestimated in the paediatric literature. Although clinical recovery after ABI in neonates is usually rapid and apparently complete, the risk of subsequent neurodevelopmental disability is significantly increased.
Article Information
vol. 134 no. Suppl 1 A18564
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Charlotte Verrall1;
- Karen Walker2;
- Alison Loughran-Fowlds2;
- Chris Troedson3;
- Julian Ayer1;
- Jonathan Egan4;
- Robert Halliday2;
- Yishay Orr1;
- Gary Sholler1;
- Gary Sholler1;
- Nadia Badawi2;
- David S Winlaw5
- 1Heart Cntr for Children, The Children’s Hosp at Westmead, Westmead, Australia
- 2Grace Cntr for Newborn Care, The Children’s Hosp at Westmead, Westmead, Australia
- 3Neurology, The Children’s Hosp at Westmead, Westmead, Australia
- 4PICU, The Children’s Hosp at Westmead, Westmead, Australia
- 5Heart Cntr for Children, The Children’s Hosp at Westmead, Sydney, Australia
Abstract 18391: Birth at 39-40 Weeks Gestation is Associated With Improved Survival in Neonates Supported With Post-Operative Extracorporeal Life Support for Congenital Heart Disease
Jane McKenzie, Thomas Scodellaro, Yves d’Udekem, Warwick Butt, Siva Namachivayam
Circulation. 2016;134:A18391
Abstract
Introduction: The neonatal population compared to other age groups with congenital heart disease (CHD) is unique because of their developmental immaturity, case complexity and consequent higher rates of extracorporeal life support (ECLS) in the post-operative period. Debate remains around whether those with single ventricle (SV) anatomy have worse outcomes after ECLS compared to biventricle (BV) anatomy.
Methods: From 2005-2014, 110 neonates (representing 9.5% of neonates undergoing cardiac surgery) required ELCS after initial cardiac surgery. Indications were failure to separate from cardiopulmonary bypass in 40 (36%), extracorporeal cardiopulmonary resuscitation (ECPR) in 48 (44%), progressive low cardiac output in 15 (14%) and other reasons in 7 (6%).
Results: Median age was 5 days (IQR 2 – 9 days), 54 (49%) underwent SV repair and median support duration was 94 hours (IQR 53 – 135). Overall survival to intensive care unit (ICU) discharge was 54.5% (95% CI 44.7 – 64.0), with 1-year survival of 43.6% (95% CI 34.2 – 53.4). There was no difference in ICU survival based on underlying anatomy [51.8% (95% CI 37.8 – 65.6) for SV vs 57.1% (95% CI 43.2 – 70.2) for BV anatomy; p=0.55], but era influenced survival [43.5% (95% CI 29 – 59) for 2005-2009 vs 62.5% (95% CI 49 – 74) for 2010-2014; p=0.048]. By multivariable analysis, gestational age was the only independent predictor of ICU mortality (when compared to being born before 37 weeks, the OR (95% CI) for 37-38 weeks was 0.3 (0.12 – 1.19), for 39-40 weeks 0.27 (0.08 – 0.84) and for ≥41 weeks 1.06 (0.07 – 14.7).
Conclusions: Mortality for neonates requiring ECLS following cardiac surgery is high but has improved in the most recent era. Gestational age 39-40 weeks appears to be the optimal time of delivery for neonates with complex congenital heart disease, as this may confer a survival advantage.
Article Information
vol. 134 no. Suppl 1 A18391
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Paediatric Intensive Care Unit, Royal Children’s Hosp, Parkville, Australia
- 2Paediatric Cardiac Surgery, Royal Children’s Hosp, Parkville, Australia
Abstract 13013: Associations Between Unplanned Cardiac Reinterventions and Early Outcomes After Pediatric Cardiac Surgery: Findings From the Society of Thoracic Surgeons Congenital Heart Surgery Database
John M Costello, Michael C Monge, Kevin D Hill, Sung Hee Kim, Sara K Pasquali, Babatunde Yerokun, Jeffrey P Jacobs, Carl L Backer, Mjaye L Mazwi, Marshall L Jacobs
Circulation. 2016;134:A13013
Abstract
Introduction: In children undergoing cardiac surgery, we sought to determine the incidence of unplanned cardiac reinterventions (surgery or therapeutic catheterization) during the same hospitalization as the index operation, identify risk factors for reinterventions, and explore associations between unplanned reinterventions and adverse outcomes.
Hypothesis: We hypothesized that younger patients undergoing more complex operations would be at greater risk for unplanned cardiac reinterventions, and that operative mortality and postoperative length of stay (LOS) would be greater in patients who undergo reintervention when compared to those who do not.
Methods: Patients ≤18 years of age in the STS Congenital Heart Surgery Database from January 2010-June 2015 were included. Multivariable logistic regression was used to evaluate risk factors for unplanned reintervention, and the impact of reintervention on outcomes including operative mortality and post-operative LOS. Covariates were included to adjust for important patient characteristics (e.g., weight, age, and comorbidities), case complexity, and center effects.
Results: Included were 84,404 patients from 117 centers, of whom 21% were neonates and 36% infants. An unplanned cardiac reintervention was performed in 5.4% of patients, including 11.8% of neonates, 5.2% of infants, and 2.8% of children. Independent risk factors for an unplanned reintervention included presence of non-cardiac anomalies and genetic syndromes, non-Caucasian race, younger age, lower weight among neonates and infants, prior cardiothoracic operations, preoperative mechanical ventilation, preoperative risk factors, and higher STAT Mortality Category (adjusted p<0.001 for all). The performance of an unplanned reintervention was an independent risk factor for operative mortality (adjusted OR, 5.34, 95% CI, 4.83-5.91, p<0.001) and longer post-operative LOS (adjusted RR=2.31, 95% CI, 2.20-2.42, p<0.001).
Conclusions: Unplanned cardiac reinterventions are not rare, particularly in neonates, and are independently associated with mortality and increased post-operative LOS. Patients at greater risk may be readily identified preoperatively, presenting opportunities for quality improvement.
Article Information
vol. 134 no. Suppl 1 A13013
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- John M Costello1;
- Michael C Monge1;
- Kevin D Hill2;
- Sung Hee Kim3;
- Sara K Pasquali4;
- Babatunde Yerokun5;
- Jeffrey P Jacobs6;
- Carl L Backer7;
- Mjaye L Mazwi1;
- Marshall L Jacobs8
- 1Cardiology, Ann & Robert H. Lurie Children’s Hosp of Chicago, Chicago, IL
- 2Cardiology, Duke Children’s Hosp & Health Cntr, Durham, NC
- 3Cardiology, Duke Clinical Rsch Institute, Durham, NC
- 4Cardiology, C.S. Mott Children’s Hosp, Ann Arbor, MI
- 5General Surgery, Duke Clinical Rsch Institute, Durham, NC
- 6Cardiovascular Surgery, John Hopkins All Children’s Hosp, St. Petersburg, FL
- 7Cardiovascular-Thoracic Surgery, Ann & Robert H. Lurie Children’s Hosp of Chicago, Chicago, IL
- 8Pediatric Cardiac Surgery, John Hopkins All Children’s Hosp, Baltimore, MD
Abstract 11322: Multi-Institutional Analysis of Noninvasive Ventilation Practice After Infant Cardiac Surgery
Ryan Romans, Steven Schwartz, John Costello, Nikhil Chanani, Parthak Prodhan, David Cooper, Jeffrey Alten, Kshitij Mistry, Andrew H Smith, Avihu Gazit, Janet Donohue, Whenying Zhang, Michael Gaies
Circulation. 2016;134:A11322
Abstract
Background: Hospitals performing infant cardiac surgery commonly use noninvasive ventilation (NIV) for postoperative respiratory support. The epidemiology of NIV use in this population remains unknown and it is unclear how practice varies across centers.
Methods: We analyzed all infant surgical encounters (<1 year) in the Pediatric Cardiac Critical Care Consortium (PC4) registry from 10/2013–12/2015. NIV included high flow nasal cannula (HFNC) or positive airway pressure (PAP) support. We described patient, operative and postoperative characteristics of patients who did and did not received NIV. To examine casemix-adjusted duration of total respiratory support and the contribution of mechanical ventilation (MV) vs. NIV we created a model incorporating age, prematurity, extracardiac anomalies, surgical complexity and MV at preoperative admission. We calculated and compared adjusted mean duration of total support (MV + NIV), MV, and NIV across hospitals using observed-to-expected duration.
Results: The cohort included 3708 encounters from 15 institutions: 2032 (55%) received NIV postoperatively, 40% were neonates, 36% were high complexity. Neonatal age group, extracardiac anomalies, single ventricle, procedure complexity, preoperative respiratory support, longer MV duration, and greater postoperative disease severity were all associated with NIV therapy vs. none (p<0.001 for all). Of those receiving NIV, 93% and 43% received HFNC and PAP, respectively. Across hospitals, NIV use ranged from 32%-65%, and adjusted mean duration ranged from 1-4 days (3 days observed mean). Differences in total adjusted respiratory support were largely driven by duration of MV (Figure 1).
Conclusions: NIV therapy is common after infant cardiac surgery, though use varies across hospitals. The analysis suggests that initiatives to reduce differences across hospitals in postoperative respiratory support time should initially focus on MV practices, not NIV.
Article Information
vol. 134 no. Suppl 1 A11322
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Ryan Romans1;
- Steven Schwartz2;
- John Costello3;
- Nikhil Chanani4;
- Parthak Prodhan5;
- David Cooper6;
- Jeffrey Alten7;
- Kshitij Mistry8;
- Andrew H Smith9;
- Avihu Gazit10;
- Janet Donohue1;
- Whenying Zhang11;
- Michael Gaies12
- 1Pediatrics and Communicable Diseases, Univ of Michigan Congenital Heart Cntr, C.S. Mott Children’s Hosp, Ann Arbor, MI
- 2Critical Care Medicine and Dept of Paediatrics, The Labatt Family Heart Cntr,The Hosp for Sick Children,Univ of Toronto Sch of Medicine, Toronto, Canada
- 3Congenital Heart Cntr, Ann & Robert H. Lurie Children’s Hosp of Chicago,Northwestern Univ Feinberg Sch of Medicine, Chicago, IL
- 4Pediatrics, Div of Pediatric Cardiology, Emory Univ Sch of Medicine/Children’s Healthcare of Atlanta, Atlanta, GA
- 5Critical Care, Pediatric Cardiology, Univ of Arkansas Med Sciences/Arkansas Children’s Hosp, Little Rock, AR
- 6Heart Institute, Cincinnati Children’s Hosp Med Cntr, Cincinnati, OH
- 7Pediatrics, Div of Critical Care, Univ of Alabama at Birmingham, Brimingham, AL
- 8Pediatric Critical Care Medicine, Levine Children’s Hosp, Charlotte, NC
- 9Pediatrics, Vanderbilt Univ Sch of Medicine, Nashville, TN
- 10Pediatrics, Washington Univ Sch of Medicine, St. Louis, MO
- 11Cntr for Healthcare Outcomes & Policy, Univ of Michigan, Ann Arbor, MI
- 12Pediatrics and Communicable Diseases, Univ of Michigan, Ann Arbor, MI
Abstract 19460: Obesity Associates With Heart Failure in Young Adults With Congenital Heart Disease
Joseph B Lerman, Ira A Parness, Rajesh U Shenoy
Circulation. 2016;134:A19460
Abstract
Introduction: Adults with Congenital Heart Disease (ACHD) are a growing segment of the population, at elevated cardiovascular risk. This risk increases with age, and is primarily attributable to congestive heart failure (CHF). Obesity is an emerging cardiovascular risk factor, associated with CHF in the healthy adult population. To date, however, the relationship between obesity and CHF in ACHD is poorly described.
Hypothesis: We hypothesized that obesity would independently associate with CHF in young ACHD.
Methods: Retrospective analysis was performed on all ACHD (identified via ICD-9 coding), ages 19 – 45 years old, seen at a Pediatric Heart Network-affiliated center in 2013. ACHD were classified as having simple or complex congenital heart disease per the Bethesda Conference Criteria. Obesity was defined as body-mass index ≥ 30 kg/m2. Statistical analysis included multivariate regression and likelihood ratio testing.
Results: 493 ACHD met inclusion criteria, with 24 identified cases of CHF. CHF patients had a higher prevalence of obesity (p=0.003), diabetes (p <0.001), and hypertension (p=0.05), as compared to patients without CHF (Table 1). Logistic regression analysis revealed that obese ACHD had greater odds of having CHF (OR 3.29, p <0.01) than non-obese ACHD, which retained significance beyond adjustment for traditional cardiovascular risk factors and complex/univentricular congenital heart disease (OR 2.66, p=0.03) (Table 2). Likelihood ratio testing revealed that obesity independently predicted the odds of having concomitant CHF (X2 4.49, p=0.03), a finding not seen in hypertension, hyperlipidemia, or diabetes mellitus.
Conclusions: Obesity was independently associated with CHF in this cohort of 493 young ACHD. In the midst of the modern obesity epidemic, these results may indicate a need for improved lifestyle counseling in congenital heart disease patients of all ages. Larger, prospective studies are needed to confirm these findings.
Article Information
vol. 134 no. Suppl 1 A19460
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Dept of Med Education, Icahn Sch of Medicine at Mount Sinai, New York, NY
- 2Div of Pediatric Cardiology, Icahn Sch of Medicine at Mount Sinai, New York, NY
Abstract 17229: First Trimester Elevated Serum Glucose Values Are Associated With Congenital Heart Disease in the Offspring
Emmi Helle, Preston S Biegley, Joshua W Knowles, Joseph B Leader, Sarah A Pendergrass, Gary Reaven, Marylyn D Ritchie, Gary M Shaw, Wei Yang, James R Priest
Circulation. 2016;134:A17229
Abstract
Introduction: Maternal diabetes mellitus (DM) during pregnancy is a well known and prevalent risk factor for congenital heart disease (CHD) in offspring. In mothers without DM, we recently observed an association between elevated serum glucose values measured in the second trimester and the risk for CHDs in offspring.
Hypothesis: As cardiac development largely occurs during weeks 4-12 of gestation, we hypothesized that measurements of glucose metabolism during early pregnancy, i.e., well before the second trimester, would be associated with risk for CHD.
Methods: We performed a multi-institutional retrospective case-control study from a population-based cohort of 19,107 pregnant women from Stanford Healthcare and Geisinger Health System comparing liveborn infants with CHD to infants without CHD (Table 1). Multivariable logistic regression analysis was used to investigate the association between 1) mother’s plasma glucose values from 4 weeks prior to conception to 15 weeks and 2) the 1hour glucose tolerance test value (OGTT) and risk for CHD the offspring. The model was adjusted for known maternal risk factors for CHD (maternal age, pregestational DM, prepregnancy BMI).
Results: Early pregnancy plasma glucose values were significantly higher in mothers who delivered offspring with any CHD relative to mothers of infants without CHD (aOR 1.08; 95% CI 1.02-1.13; Table 2). The OGTT did not reach statistical significance between these groups (aOR 1.69; 95%CI 0.9-2.91).
Conclusions: For the first time we show random first trimester plasma glucose measured during early pregnancy is associated with risk for CHD in offspring, and furthermore are more strongly correlated with risk than abnormal OGTT (which is currently used to risk-stratify patients for echocardiographic screening). Though these conclusions are limited by the sampling bias inherent in retrospective studies, they support prospective investigation of first trimester glucose metabolites in the risk for CHD.
Article Information
vol. 134 no. Suppl 1 A17229
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Emmi Helle1;
- Preston S Biegley2;
- Joshua W Knowles3;
- Joseph B Leader2;
- Sarah A Pendergrass2;
- Gary Reaven4;
- Marylyn D Ritchie2;
- Gary M Shaw5;
- Wei Yang5;
- James R Priest3
- 1Cardiovascular Medicine, Stanford Univ Sch of Medicine, Stanford, CA
- 2Biomedical and Translational Informatics, Geisinger Health System, Danville, PA
- 3Stanford Cardiovascular Institute, Stanford Univ Sch of Medicine, Stanford, CA
- 4Cardiovascular Institute, Stanford Univ Sch of Medicine, Stanford, CA
- 5Pediatrics, Stanford Univ Sch of Medicine, Stanford, CA
Abstract 16408: Objectively-Measured Physical Activity Does Not Differ by Disease Severity in Children With Congenital Heart Disease
Stephanie L Duncombe, Christine Voss, Paige H Dean, Astrid M De Souza, Ross Gardner, Kevin C Harris
Circulation. 2016;134:A16408
Abstract
Introduction: There are conflicting reports on the physical activity levels in children with congenital heart disease (CHD) according to disease severity. Few studies have objectively measured physical activity in children across the CHD spectrum.
Hypothesis: We hypothesised that physical activity would be significantly lower in children with more severe CHD compared with mild CHD.
Methods: We recruited patients with CHD, aged 9-19 yrs, from pediatric cardiology clinics throughout British Columbia, Canada. Patients were fitted with an accelerometer (GT3X+ or GT9XLink; ActiGraph LLC; 60s epoch) to be worn over the right hip for 7days. We included accelerometry files if they had ≥3days with ≥600min/day wear time. We estimated daily means for: total physical activity (axis1 counts/day), moderate-to-vigorous physical activity (MVPA; min/day), vigorous physical activity (min/day), and %sedentary time (%/day). We classified CHD as mild, moderate, severe (Bethesda), or cardiac transplant (Tx). We used multiple linear regression to assess the association between physical activity metrics, disease complexity and relevant patient characteristics.
Results: We included 82 patients (13.6±2.7yrs; 54% male), of which 21 had mild CHD, 26 moderate CHD, 26 severe CHD and 9 Tx. Overall, median daily mins of MVPA was 31 min/day (interquartile range: 18.3-43.6 min) and 17% met physical activity guidelines of 60 min of MVPA/day. There were no significant differences in any physical activity metric according to CHD disease complexity. In multiple linear regression analyses (adjusted for BMI z-score), age was positively related to sedentariness (p<0.001), and inversely related to total physical activity and MVPA (both p<0.01). Boys were less sedentary (p<0.05) and more active than girls (total and MVPA; both p<0.05). Neither age nor sex was related to vigorous physical activity.
Conclusions: In conclusion, we found no difference in physical activity patterns based on CHD disease severity. We observed age- and sex-related patterns in physical activity as expected for healthy children, suggesting that socio-cultural determinants are also at play.
Article Information
vol. 134 no. Suppl 1 A16408
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Stephanie L Duncombe;
- Christine Voss;
- Paige H Dean;
- Astrid M De Souza;
- Ross Gardner;
- Kevin C Harris
- Pediatrics, Univ of British Columbia, Vancouver, Canada
Abstract 15812: Pediatric Familial Hypercholesterolemia: Children and Adolescents Enrolled in the CAscade SCreening for Awareness and DEtection Registry
Sarah D de Ferranti, Emily C O’Brien, Iris Kindt, Sarah Clauss, Joshua W Knowles, Amy L Peterson, Irwin Benuck, Zahid S Ahmad, Lisa C Hudgins, Samuel S Gidding, Daniel J Rader, MacRae F Linton, Christie M Ballantyne, P. B Duell, Michael D Shapiro, Matthew T Roe, Peter Shrader, Katherine Wilemon, William Neal
Circulation. 2016;134:A15812
Abstract
Introduction: Familial hypercholesterolemia (FH) in US youth is not well described. CAscade SCreening for Awareness and Detection of FH (CASCADE FH) is a registry designed to address this knowledge gap.
Methods: We conducted a cross-sectional analysis of 268 children and adolescents <18 years with heterozygous FH enrolled in the CASCADE FH Registry from 9 US lipid clinics between April 2014 and February 2016.
Results: Median age at FH diagnosis was 9 yrs (interquartile range [IQR] 6,12); 50.0% were male, 70.9% White. In ~1/3rd of youth FH was diagnosed by specific criteria, e.g. MEDPED (22.8%), Simon Broome (10.8%), more than one criteria (1.9%); most were diagnosed clinically (57.8%). Only 2 (0.7%) patients had a confirmed genetic mutation. While 22.8% had a family history of premature MI, no youth experienced cardiovascular events. Some youth with FH had additional cardiovascular risk factors, with low HDL-C (29.1%) and obesity (14.9%) being relatively common, followed by hypertension (2.2%) and diabetes (0.7%); 9.0% had ≥2 additional risk factors. A majority (59.3%) of the cohort was treated with a lipid-lowering therapy (LLT), mostly commonly statins (48.9%). Children ≥10 years were more likely than younger patients to receive LLT (68.3% vs. 31.8%, p<0.0001). Median age at LLT initiation was 11 years (range 0-17). The mean reported highest untreated LDL-C level was 233 mg/dL (IQR 195,277), n=255; while the average LDL-C on treatment was 175 mg/dl (140-211). Of the FH youth on LLT, 18.9% had an LDL <130 mg/dL and 13.2% had an LDL-C ≥50% lower than their maximum untreated level; 23.9% met one or the other LDL-C goal.
Conclusions: Among youth enrolled in the CASCADE FH registry, just over half reported being on LLT, with higher rates of pharmacotherapy reported in older children. Despite this, less than a quarter of youth achieved sufficient LDL-C lowering. Opportunities exist to optimize the treatment of youth with FH to reduce their risk of cardiovascular disease.
Article Information
vol. 134 no. Suppl 1 A15812
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Sarah D de Ferranti1;
- Emily C O’Brien2;
- Iris Kindt3;
- Sarah Clauss4;
- Joshua W Knowles5;
- Amy L Peterson6;
- Irwin Benuck7;
- Zahid S Ahmad8;
- Lisa C Hudgins9;
- Samuel S Gidding10;
- Daniel J Rader11;
- MacRae F Linton12;
- Christie M Ballantyne13;
- P. B Duell14;
- Michael D Shapiro15;
- Matthew T Roe2;
- Peter Shrader2;
- Katherine Wilemon16;
- William Neal17
- 1Cardiology, Boston Children’s Hosp, Boston, MA
- 2Duke Clinical Rsch Institute, Duke Univ, Durham, NC
- 3n/a, The FH Foundation, South Pasedena, CA
- 4Medicine, Children’s National Med Cntr, Boston, MA
- 5Medicine, Stanford Univ, Stanford, CA
- 6Pediatric Cardiology, Univ of Wisconsin Sch of Medicine, Madison, MA
- 7Medicine, Ann &Robert H. Lurie Children’s Hosp of Chicago, Chicago, IL
- 8Internal Medicine, Univ of Texas Southwestern, Dallas, TX
- 9Comprehensive Lipid Control Cntr, The Rogosin Institute, New York, NY
- 10Cardiology, Nemours Cardiac Cntr, Wilmington, DE
- 11Medicine, Univ of Pennsylvania, Philadelphia, PA
- 12Medicine, Vanderbilt Univ Sch of Medicine, Nashville, TN
- 13Medicine, Baylor College of Medicine, Houston, TX
- 14Medicine, Oregon Health and Science Univ, Portland, OR
- 15Cardiology, Oregon Health and Science Univ, Portland, OR
- 16n/a, The FH Foundation, Pasadena, CA
- 17Pediatrics, West Virginia Univ, Morgantown, WV
Abstract 14394: Overweight and Obesity Across the Lifespan Among White and Black Congenital Heart Disease Survivors
Jamie L Jackson, Tondi Harrison
Circulation. 2016;134:A14394
Abstract
Introduction: Rates of obesity among adults with congenital heart disease (CHD) living in the U.S. have risen, contributing to increased morbidity and mortality. In the general population, obesity rates are higher among Black adults than Whites. However, research on health outcomes among ethnic minority survivors of CHD is lacking.
Methods: Medical chart abstraction from a both a pediatric and adult hospital identified 4852 individuals who received a diagnosis of structural CHD spanning childhood (ages 6-12; n = 1504), adolescence (ages 13-18; n = 1085), young adulthood (ages 19-39; n = 1387), and adulthood (ages ≥ 40; n = 876). The sample was 84.7% White, 9.3% Black, and 5.8% “Other” (i.e., Latino, Asian, biracial, and non-U.S. citizens). Disease severity was representative (36% simple; 50% moderate; 14% complex). BMI was calculated from the most recent hospital visit and was categorized as either normal or overweight/obese based on Center for Disease Control definitions. Underweight individuals were excluded from analyses. Observed and expected frequencies of overweight/obese were compared using chi-square tests.
Results: The following proportion of individuals with CHD was overweight/obese: 32.9% of children, 37.6% of adolescents, 59.1% of young adults, and 72.3% of adults. The frequency of overweight/obese among adolescents with CHD was higher than expected based on CDC state data for adolescents (27.4% overweight/obese; χ2 = 56.8 [1], p < 0.01). Rates of overweight/obese for adults with CHD 19+ years (62.2%) were similar to Ohio adults (65%). In comparing White and Black survivors, Black survivors had significantly higher rates of overweight/obese in adolescence (White = 37.1% vs. Black = 48.3%; χ2 = 63.8 [1], p < 0.01) and young adulthood (White = 57.7% vs. Black = 70.6%; χ2 = 22.1 [1], p < 0.01) with a trend in adulthood (White = 72.5% vs. Black = 83%; χ2 = 2.9 [1], p = 0.09).
Conclusion: Rates of overweight/obese among adolescent CHD survivors is higher than state data, which is alarming considering that precursors for atherosclerosis have been identified in children and adolescents with CHD. Furthermore, rates of obesity in both adolescence and young adulthood are higher among Black CHD survivors which may contribute to outcome disparities.
Article Information
vol. 134 no. Suppl 1 A14394
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Abstract 12767: Trajectory of Exercise Capacity in Childhood and Its Impact on Their Adult Pathophysiology in Patients After the Fontan Operation
Hideo Ohuchi, Jun Negishi, Yosuke Hayama, Kanae Noritake, Aya Miyazaki, Isao Shiraishi
Circulation. 2016;134:A12767
Abstract
Background: Preserved exercise capacity in childhood may predict better long-term outcome in patients after the Fontan operation.
Purpose: This study was to elucidate an impact of trajectory of exercise capacity in childhood on the long-term exercise capacity and non-cardiac multi-organ function.
Method and Results: Since 1990, consecutive 197 Fontan patients had undergone two serial cardiopulmonary exercise testing (CPX) at the age of 8±2 and 14±2 years and we measured the change in %-predicted peak oxygen uptake (dPVO2: %). Of these, 94 patients had performed CPX in the adulthood (24±4 years). Our patients were subdivided into 2 groups; those with positive dPVO2 (n=113, group I) and those with negative dPVO2 (n=84, group D). Early era at operation, heterotaxy, protein losing enteropathy, high PVO2 and plasma brain natriuretic peptide levels (BNP) at 1st CPX had independent negative impact on dPVO2 (p<0.05-0.0001). Group I showed significantly higher PVO2 and lower BNP in their adulthood, while 49 clinical events, including 9 deaths occurred after 2nd CPX. When compared with group I, group D had high hazard ratio of 2.1 and 6.5 for morbidity and mortality, respectively (p<0.05 for both); however, there were no differences in high prevalence of impaired glucose tolerance, liver MELD XI score, or 24-hour creatinine clearance between two groups in their adulthood.
Conclusions: The trajectory of exercise capacity in childhood is improving in current Fontan children which is associated with better prognosis, higher PVO2 and lower BNP in the adulthood. However, the non-cardiac multi-organ dysfunction may progress regardless of the trajectory.
Article Information
vol. 134 no. Suppl 1 A12767
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Hideo Ohuchi;
- Jun Negishi;
- Yosuke Hayama;
- Kanae Noritake;
- Aya Miyazaki;
- Isao Shiraishi
- Pediatric Cardiology, National Cerebral and Cardiovascular Cntr, Suita, Japan
Abstract 20393: End Stage Renal Disease After Pediatric Heart Transplantation: A 25-Year National Cohort Study
Swati Choudhry, Chesney D Castleberry, Vikas R Dharnidharka, Charles Goss, Kathleen E Simpson, Kenneth Schechtman, Charles E Canter
Circulation. 2016;134:A20393
Abstract
Background: End stage renal disease (ESRD) is a known complication after heart transplant (HTx); however risk factors associated with ESRD are not well elucidated. The objectives of this study were to determine the time course, risk factors, and outcome associated with ESRD.
Methods: Scientific Registry of Transplant Recipients data was linked to the US Renal Data System to identify patients (≤ 18 years) who underwent HTx (1989-2013). Multi-organ transplant were excluded. Associated risk factors and time course for ESRD (defined: chronic dialysis, wait listed for, and or kidney transplant [KTx]) were assessed using Cox regression analysis. Subjects that did not have an ESRD event were censored at death, lost to follow up, or December 31, 2013, whichever occurred earliest. P < 0.05 was significant.
Results: The final study cohort included 6702 HTx recipients. During a median follow up of 4.5 years ([IQR, 1.3 – 9.5], [range 0 – 24.7), 162 (2.4 %) patients developed ESRD. The actuarial risk of developing ESRD 5, 10 and 20 years post HTx were 0.3, 1.9, and 10.3% respectively (Fig. 1). Of the various risk factors analyzed only African American (AA) race was found to be significant (0.04) on univariate analysis. Age at HTx (<1, 1 – <10, 10 – 18 years) was not a risk factor for ESRD (P=0.2). Fifty patients (30.9%) with ESRD died after a median follow up of 3.8 years (IQR [2.1, 8.3]). The mortality in those who developed ESRD was 10% higher than those without ESRD (P = 0.01). Those who remained on chronic dialysis until death or end of follow had significantly higher risk of mortality compared to those who received KTx (P <0.0001), (Fig. 2).
Conclusions: ESRD is an important complication after HTx that generally begins 10 year post HTx. The risk significantly increases over next decade. AA race is the only other risk factor associated with ESRD. Post HTx ESRD strongly predicts mortality particularly in those who remain on chronic dialysis whereas KTx is protective.
Article Information
vol. 134 no. Suppl 1 A20393
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Swati Choudhry;
- Chesney D Castleberry;
- Vikas R Dharnidharka;
- Charles Goss;
- Kathleen E Simpson;
- Kenneth Schechtman;
- Charles E Canter
- Pediatrics, Washington Univ Sch of Medicine, St. Louis, MO
Abstract 14470: A Comparison Between Patent Ductus Arteriosus Stent and Modified Blalock-Taussig Shunt as Palliation for Infants With Ductal-dependent Pulmonary Blood Flow: Insights From a Multi-center Collaborative
Andrew C Glatz, Christopher J Petit, Bryan H Goldstein, Michael S Kelleman, Courtney E McCracken, Alicia McDonnell, Christopher Mascio, Subi Shashidharan, R. Allen Ligon, Jingning Ao, Wendy Whiteside, W. Jack Wellen, Christina M Metcalf, Varun Aggarwal, Hitesh Agrawal, Jeffrey S Heinle, Athar M Qureshi
Circulation. 2016;134:A14470
Abstract
Introduction: Infants with ductal dependent pulmonary blood flow (PBF) may undergo palliation with either ductus arteriosus stent (DAS) or Blalock-Taussig shunt (BTS). A balanced comparison of these two approaches has not been performed.
Methods: Consecutive infants with ductal dependent PBF and confluent pulmonary arteries palliated with either DAS or BTS from 1/08 to 11/15 were retrospectively reviewed from the 4 member centers of the Congenital Catheterization Research Collaborative. Primary outcome was defined as death or reintervention to treat cyanosis prior to any definitive repair or next staged palliation. Secondary outcomes included: intensive care unit (ICU) and hospital length of stay (LOS), diuretic use at discharge, and procedural complications. Outcomes were compared between treatment strategies using propensity score adjustment to account for baseline differences between groups.
Results: The cohort consisted of 105 DAS and 174 BTS patients. There were no differences in demographic and clinical characteristics. The groups differed in underlying anatomy (expected two-ventricle circulation in 63% of DAS v. 52% of BTS, p=0.08), and presence of antegrade PBF (65% of DAS v. 39% of BTS, p<0.001). The observed risk of the primary outcome was higher in the DAS group (48% v. 35%, p=0.04), due to a difference in risk of reintervention. There was no difference in risk of death (11.7% v. 14.1%, p=0.6). After propensity score adjustment, the risk of the primary outcome remained higher among the DAS group [OR=1.79 (95% CI: 1.01 – 3.17), p=0.045]. The DAS group had a lower adjusted ICU LOS [mean 4.5 (95% CI: 3.4 – 5.8) v. 9.4 (7.7 – 11.4) days, p<0.001] and risk of diuretic use at discharge [OR=0.34 (0.19 – 0.63), p<0.001]. There was no difference in adjusted hospital LOS. Procedural complications were lower in the DAS group (13.6% v. 26.2%, p=0.014).
Conclusions: This is the first multi-center comparison of palliative DAS and BTS for infants with ductal-dependent PBF, adjusted for patient factors to account for confounding by indication. Although there was a higher rate of reintervention to treat cyanosis, the ICU LOS was shorter, diuretic use was less, and procedural complications were lower in the DAS group, supporting DAS as a reasonable alternative to BTS.
Article Information
vol. 134 no. Suppl 1 A14470
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Andrew C Glatz1;
- Christopher J Petit2;
- Bryan H Goldstein3;
- Michael S Kelleman4;
- Courtney E McCracken4;
- Alicia McDonnell1;
- Christopher Mascio5;
- Subi Shashidharan2;
- R. Allen Ligon2;
- Jingning Ao2;
- Wendy Whiteside6;
- W. Jack Wellen6;
- Christina M Metcalf6;
- Varun Aggarwal7;
- Hitesh Agrawal7;
- Jeffrey S Heinle8;
- Athar M Qureshi9
- 1Div of Cardiology, The Children’s Hosp of Philadelphia, Philadelphia, PA
- 2Pediatrics, Emory Univ Sch of Medicine, Atlanta, GA
- 3The Heart Institute, Cincinnati Children’s Hosp Med Cntr, Cincinnati, OH
- 4Pediatrics, Emory Univ, Atlanta, GA
- 5Dept of Cardiothoracic Surgery, The Children’s Hosp of Philadelphia, Philadelphia, PA
- 6The Heart Institute, Cincinnati Children’s Hosp Med Cntr, Cincinnati, OH
- 7The Lillie Frank Abercrombie Section of Cardiology, Texas Children’s Hosp, Baylor College of Medicine, Houston, TX
- 8Congenital Heart Surgery, Texas Children’s Hosp, Baylor College of Medicine, Houston, TX
- 9The Lillie Frank Abercrombie Section of Cardiology, Texas Children’s Hosp, Baylor College of Medicine, Houston, TX
Abstract 11827: Endothelial Microparticles Modulate Vasculitis During the Acute Phase of Kawasaki Disease
Hideyuki Nakaoka, Keiichi Hirono, Mako Okabe, Nariaki Miyao, Kazuyoshi Saito, Keijiro Ibuki, Sayaka Ozawa, Kei Takahashi, Fukiko Ichida
Circulation. 2016;134:A11827
Abstract
Introduction: Kawasaki Disease (KD) is an acute inflammatory disease that takes the form of systemic vasculitis. Endothelial microparticles (EMPs) are vesicles formed by cell membranes after endothelial activation, which contain microRNAs (miRs) recognized as an important transcellular delivery system in the exchange of biological signals. The purpose of this study was to elucidate whether EMPs are involved in vasculitis in acute KD.
Methods: We enrolled 50 KD patients (aged 4 months to 14 years), 50 controls (25 non-KD febrile and 25 healthy children). KD patients were divided into two subgroups: those with coronary artery lesions (CAL, Z-socre>2.5, n=4) and those without coronary artery lesions (NCAL, Z-score≦2.5, n=46). Blood samples were collected three times; first, at the time of diagnosis before the initiation of IVIG treatment; second, immediately after the first IVIG infusion; finally, at 2-4 weeks after the onset of the disease. EMPs were measured using flow cytometry and miR expression profiling was performed using microarrays (Affymetrix®GeneChip® miRNA 4.0). We also performed miRCURY LNA™ microRNA in situ hybridization using 2 miRs in CAL patients and analyzed THP-1 monocyte stimulation using 2 miRs.
Results: The percentage of EMPs was 1.27±0.16% in all of the small vesicles in KD patients prior to treatment, which was significantly higher than in controls (0.09±0.03%: P<0.0001). Furthermore the percentage of EMPs in patients with CAL rapidly increased after the initial treatment, and was significantly higher than those without CAL (p<0.001). We identified two miRs (hsa-miR-145-5p and hsa-miR-320a) out of 2578 miRs (0.08%) specific to the patients with CAL and these two miRs are predicted to affect the monocyte system using in silicoanalysis. We also detected these two miRs in CAL patients’ endothelial cells, using in situ hybridization, and showed these two miRs suppressed gene expression of the two inflammatory cytokines (IL-6 and TNF-α).
Conclusions: EMPs could serve as a sensitive marker of the severity of endothelial dysfunction and vasculitis in acute KD. Moreover, hsa-miR-145-5p and hsa-miR-320a may contribute to regulation of gene expression of cytokines and pathogenesis of KD.
Article Information
vol. 134 no. Suppl 1 A11827
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Hideyuki Nakaoka1;
- Keiichi Hirono1;
- Mako Okabe1;
- Nariaki Miyao1;
- Kazuyoshi Saito1;
- Keijiro Ibuki1;
- Sayaka Ozawa1;
- Kei Takahashi2;
- Fukiko Ichida1
- 1Pediatrics, Medicine Univ of Toyama, Toyama, Japan
- 2Pathology, Toho Univ Med Cntr Ohashi Hosp, Tokyo, Japan
Abstract 20371: Non-Cardiomyocyte MicroRNA-34a Mediates Dysregulation of Angiogenesis in RV Failure
Sushma Reddy, Dong-Qing Hu, Mingming Zhao, Gwanghyun Jung, Edda Spiekerkoetter, Elizabeth A Barnes, Giovanni Fajardo, Daniel Bernstein
Circulation. 2016;134:A20371
Abstract
Introduction: The right ventricle (RV) is uniquely at risk in patients with complex congenital heart disease (CHD) involving right-sided obstructive lesions. In the left ventricle (LV) angiogenesis is a key adaptation to pressure overload, induced during adaptive hypertrophy via Hif-1α and VEGF, and declining with LV failure. In contrast, early capillary rarefaction occurs in RV hypertrophy (RVH), the mechanism of which is unknown. We hypothesize that microRNA (miR) 34a is responsible for the attenuated angiogenic response in RVH and RV failure (RVF).
Methods: Adult, male FVB mice were subject to pulmonary artery banding (PAB) to induce RVH and RVF and compared to sham-operated controls. In vitro miR overexpression studies using lipofectamine miR-34a and in vivo miR inhibition studies using LNA-antimiR-34a (25mg/kg IP) were performed. RNA and protein expression was evaluated from the RV free wall. Student’s t test was used for two group comparisons and Kaplan Meier for survival analysis. Data are presented as mean±SEM (*p<0.05).
Results: miR-34a is upregulated (6.5 fold) in RVH/RVF and is associated with capillary rarefaction (1.5±0.1 vs. 1.2±0.1*) and decreased VEGF signaling. miR-34a originates from fibroblasts and endothelial cells in RVH/RVF. miR-34a overexpression in endothelial cells induces cell senescence (10±1 vs. 30±4%*) by suppressing SIRT1 expression (1.8±0.5 vs. 0.8±0.1*), decreases proliferation (0.5±0.04 vs. 0.3±0.01*) and decreases tube formation by 50% via suppression of Hif-1α (0.9±0.1 vs. 0.5±0.02*), VEGF A (0.7±0.2 vs. 0.5±0.03*), VEGF B (0.4±0.1 vs. 0.1±0.01*) and VEGFR2. AntimiR-34a suppresses miR-34a in PAB, reverses the decrease in capillarity and VEGF, and improves survival half-time by 44%*. miR-34a is also increased in children with RVF (2-fold) and capillarity is decreased compared to those with RVH.
Conclusions: Capillary rarefaction is a feature of RVH/RVF in murine models of CHD and children with CHD. Capillary rarefaction is due to the uncoupling of HIF-1α and VEGF signaling which maybe mediated by non-cardiomyocyte miR-34a. Inhibition of miR-34a rescues capillarity and delays the onset of heart failure thereby raising its potential for therapeutic manipulation and translation into clinical practice.
Article Information
vol. 134 no. Suppl 1 A20371
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Sushma Reddy1;
- Dong-Qing Hu1;
- Mingming Zhao1;
- Gwanghyun Jung1;
- Edda Spiekerkoetter2;
- Elizabeth A Barnes1;
- Giovanni Fajardo1;
- Daniel Bernstein1
- 1Pediatrics, Lucile Packard Children’s Hosp, Stanford, CA
- 2Medicine, Stanford Hosp, Stanford, CA
Abstract 19517: Circulating Factors Contribute to PDE5-Mediated Pathological Myocardial Remodeling in Single Ventricle Congenital Heart Disease
Anastacia M Garcia, Stephanie J Nakano, Brian L Stauffer, Carmen C Sucharov, Shelley D Miyamoto
Circulation. 2016;134:A19517
Abstract
Introduction: Single ventricle congenital heart disease (SV) is fatal without intervention, and maladaptive myocardial remodeling and eventual heart failure (HF) is a major cause of morbidity and mortality. Our previous studies demonstrated gene expression changes indicative of pathological myocardial remodeling (e.g., up-regulated BNP and MHC isoform switching) and increased PDE5 expression and activity in the systemic right ventricle (RV) of SV patients. Sildenafil, a phosphodiesterase-5 inhibitor (PDE5i), is increasingly utilized for the treatment of SV, with the pulmonary vasculature as the intended target. However, our data suggest potential myocardial effects of PDE5i. Our objective is to determine if myocardial and circulating PDE5 have a role in the induction of pathological gene expression changes seen in SV myocardium.
Methods: Circulating PDE5 levels in non-failing (NF) and SV sera and plasma were measured using an ELISA. Primary cardiomyocytes were isolated from neonatal rat ventricular myocardium (NRVMs) and treated for 72 hours with sera or serum-derived exosomes from NF control and SV patients ± sildenafil. qPCR was performed for the targets of interest.
Results: Circulating levels of PDE5 are significantly higher in SV patients (32±7.8 ng/mL) compared to NF (9±3.1 ng/mL) controls (p<0.05; n=3 SV, n=3 NF).Additionally, treatment of NRVMs with SV serum (n=14 SV and n=3 NF) and exosomes (n=6 SV, n=3 NF) recapitulates the pathological gene expression pattern that is seen in the human SV myocardium. Moreover, inhibition of PDE5 in NRVMs prior to exosome or serum treatment prevents these pathologic gene expression changes (n=9 serum, n=3 exosome).
Conclusions: SV circulating factors contribute to myocyte remodeling, and PDE5i attenuates this response. While additional investigation is necessary, these data suggest that in addition to effects on the pulmonary vasculature, PDE5i may be a direct myocardial target of therapy for the treatment of SV.
Article Information
vol. 134 no. Suppl 1 A19517
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Anastacia M Garcia1;
- Stephanie J Nakano1;
- Brian L Stauffer2;
- Carmen C Sucharov2;
- Shelley D Miyamoto1
- 1Pediatric Cardiology, Univ of Colorado Anschutz Med Campus, Aurora, CO
- 2Cardiology, Univ of Colorado Anschutz Med Campus, Aurora, CO
Abstract 18643: Proliferation and Endothelial to Mesenchymal Transition Contribute to Progressive Lesions in a Surgical Model of Pulmonary Vein Stenosis
Rachel D Vanderlaan, Yaqin Yana Fu, Jiaquan Zhu, Rie Montgomery, Haruki Ide, Mauro Lo Rito, Jason Maynes, John Coles, Christopher A Caldarone
Circulation. 2016;134:A18643
Abstract
Introduction: The role of proliferation and endothelial-to-mesenchymal transition (EndMT) is poorly defined in progressive pulmonary vein stenosis (PVS).
Hypothesis: Altered signaling leads to hypercellular (PVS) lesions through proliferation and EndMT, which can be modulated by losartan.
Methods: We used molecular and biochemical techniques to characterize progression of PVS in banded and losartan treated piglets.
Results: Our surgical model of PVS demonstrates progressive hypercellular lesions, with increasing amount of complex lesions between 3 and 7 weeks post banding (3.4% vs 34%, p=0.002). Lesions were rich in mesenchymal cells (α- SMA positive), with increased expression of fibronectin (2.6fold, p=0.05) and collagen 1A1(2.5fold, p=0.05). Banded animals had elevations in PDGFRβ (2.6fold, p=0.001), FGFR2 (3 fold, p<0.05), and HIf1α (2.3 fold, p=0.01) which was associated with increased Ki-67 expression ( 1.5fold, p<0.05). In banded animals, proliferation localized to the intima (7.7% vs 3.2% positive Ki-67 cells, p<0.05) at early timepoints while adventitial proliferation (7.9% vs 3.9% positive Ki-67 cells; P<0.05) was more prominent at later timepoints.
In addition to growth factor signaling, TGFβ1 and AGTR1 expression was elevated (3.7 and 4.0fold, respectively; p<0.05 ). TGFβ1 stimulated PV endothelial cells underwent EndMT with upregulation of Snail ( 2.5fold, p=0.001 and Twist (1.4fold, p=0.07). In banded animals, intimal lesions cells co-expressed CD31 and α-SMA, and there was upregulation of Snail and Twist expression in banded animals compared to shams ( 4.7fold and 2.7fold, respectively; p<0.05), suggesting a role for EndMT.
Losartan ameliorates the PVS phenotype in our model and correlates with a significant reduction in complex lesions in losartan-treated banded animals compared to banded animals (11% vs 34%, p=0.01). This is accompanied by reduced expression of Twist, Snail and TGFβ1 in losartan-treated banded animals ( 2.5, 2.0 and 2.0fold,respectively, p≤0.05), but without significant reductions in Ki 67 expression.
Conclusion: Proliferation and EndMT play a role in development of neointimal lesions in PVS. Losartan primarily targets the contribution of EndMT to PVS lesion development and progression.
Article Information
vol. 134 no. Suppl 1 A18643
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Rachel D Vanderlaan1;
- Yaqin Yana Fu2;
- Jiaquan Zhu3;
- Rie Montgomery3;
- Haruki Ide3;
- Mauro Lo Rito3;
- Jason Maynes4;
- John Coles3;
- Christopher A Caldarone3
- 1Surgery, Univ of Toronto, Toronto, Canada
- 2PEM, Hosp for Sick Children, Toronto, Canada
- 3Cardiovascular Surgery, Hosp for Sick Children, Toronto, Canada
- 4Anesthesia, Hosp for Sick Children, Toronto, Canada
Abstract 16504: Human Gene Profiling Reveals Contribution of Tissue Plasminogen Activator to Intimal Thickening of the Ductus Arteriosus
Junichi Saito, Utako Yokoyama, Munetaka Masuda, Toshihide Asou, Yoshihiro Ishikawa
Circulation. 2016;134:A16504
Abstract
Introduction: Intimal thickening (IT) formation is required to lead complete closure of the ductus arteriosus (DA). The initial step of intimal thickening is disruption of the internal elastic lamina, which is followed by smooth muscle cell (SMC) migration toward luminal side. Although prominent IT is well recognized in humans, gene profiling of IT in the human DA has not been reported. We aimed to identify IT-specific genes using a comprehensive analysis of human DA and investigate the role of the identified gene in endothelial cells and IT formation of the DA.
Methods and Results: Human DA tissues were obtained at the surgery from 6 patients with congenital heart diseases including hypoplastic left heart syndrome and coarctation of the aorta with approval of institutional review board and written informed consents. The tunica media and IT were isolated from the human DA tissues and subjected to DNA microarray analysis. Among total 6,267 genes detected in the tunica media and IT, 12 genes were expressed more than 3-fold in IT than in the tunica media. Notably, expression of tissue plasminogen activator (PLAT) was 3.8-fold greater in IT than in the tunica media (n=6, p<0.001). Next, we examined using fetal rats whether PLAT was highly expressed in the DA compared to the aorta, since the paired aortic tissue could not be obtained from human patients. We obtained the DA and aorta from fetal rats on day 21 of gestation and isolated ECs by fluorescence-activated cell sorting (FACS). Quantitative RT-PCR revealed that expression of PLAT was significantly higher in ECs of the DA than in aortic ECs (2.5-fold, n=8, p<0.05). Immunohistochemistry in human DA and rat fetus demonstrated that PLAT localized in ECs of the DA. We further investigated the role of PLAT using gelatin zymography. When ECs were cultured with plasminogen, plasmin-induced activation of matrix metalloproteinase-2 (MMP-2) which disrupts elastic lamina was markedly enhanced in the rat DA compared to aortic ECs (8.0-fold, n=8-10, p=0.09).
Conclusions: PLAT was identified as an IT-selective gene in the human DA. The data suggests that PLAT activates MMP-2 and may lead disruption of the internal lamina and subsequent IT formation in the DA. Activation of PLAT may be a strategy for DA closure.
Article Information
vol. 134 no. Suppl 1 A16504
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Cardiovascular Rsch Institute, Yokohama City Univ, Yokohama, Japan
- 2Dept of Cardiovascular Surgery, Yokohama City Univ, Yokohama, Japan
- 3Dept of Cardiovascular Surgery, Kanagawa Children’s Med Cntr, Yokohama, Japan
Abstract 20596: Cumulative Hospital-Related Costs Do not Differ Between the Norwood and Hybrid Strategies for Single Ventricle Palliation
Amine Mazine, James M Meza, Anne-Marie Guerguerian, Christoph Haller, Steven M Schwartz, Brian W McCrindle, Glen S Van Arsdell, Osami Honjo, Christopher A Caldarone
Circulation. 2016;134:A20596
Abstract
Introduction: Limited data exist on the health care costs associated with the Norwood and Hybrid strategies for single ventricle palliation. We compared the cumulative hospital-related costs of patients treated with these two strategies.
Methods: We performed a retrospective analysis of 129 consecutive patients with single ventricle physiology who underwent stage 1 palliation (76 Norwood, 53 Hybrid) between 2007 and 2015 at a tertiary pediatric center. Costs associated with inpatient episodes of care from first admission until death or Fontan completion were retrieved from our institution’s Financial Department. Costs are presented in 2016 US dollars (USD). Costs at each stage of single ventricle palliation were calculated and compared pairwise. The effect of surgical strategy on the cost of repeated hospitalizations over time was assessed using linear mixed model regression.
Results: The median number of hospitalizations per patient was 4 (IQR: 2-6) in the Norwood group versus 5 (IQR: 2-8) in the Hybrid group (p=0.55). The median length of stay per hospitalization was 7 (IQR: 1-24) days in the Norwood group versus 6 (IQR:1-20) days in the Hybrid group (p=0.41). There were 179 admissions in the Norwood group (52%) and 134 in the Hybrid group (49%) that involved at least one surgical intervention (p=0.51). Surgical strategy was not significantly associated with the cost of repeated hospitalizations over time (Figure 1A). The median cumulative cost per patient was $220,804 (IQR $155,432—$400,259) versus $237,798 (IQR $156,064—$455,607) in the Norwood and Hybrid groups, respectively (p=0.65). The hybrid strategy was associated with higher interstage costs (p<0.001) and stage 2 costs (p<0.001) (Figure 1B).
Conclusions: There was no difference in cumulative costs over time during the study period between the Norwood and Hybrid strategies. The higher costs during the interstage and stage 2 in the Hybrid group likely reflect the deferral of more complex intervention.
Article Information
vol. 134 no. Suppl 1 A20596
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Amine Mazine1;
- James M Meza1;
- Anne-Marie Guerguerian2;
- Christoph Haller1;
- Steven M Schwartz2;
- Brian W McCrindle3;
- Glen S Van Arsdell1;
- Osami Honjo1;
- Christopher A Caldarone1
- 1Cardiac Surgery, The Hosp for Sick Children, Toronto, Canada
- 2Critical Care Medicine, The Hosp for Sick Children, Toronto, Canada
- 3Cardiology, The Hosp for Sick Children, Toronto, Canada
Abstract 16892: Prenatal Diagnosis Influences Preoperative Status in Neonates With Congenital Heart Disease: an Analysis of the Society of Thoracic Surgeons Congenital Heart Surgery Database (STS-CHSD)
Michael Quartermain, Kevin D Hill, David J Goldberg, Jeffery J Jacobs, Marshall L Jacobs, Sara K Pasquali, George R Verghese, Amelia Wallace, Ross M Ungerleider
Circulation. 2016;134:A16892
Abstract
Background: The early postnatal course for a newborn with critical congenital heart disease (CHD) can be negatively impacted if diagnosis is delayed. Despite this, there continues to be inconsistent evidence regarding the benefits of prenatal diagnosis (PND) in neonates undergoing cardiac surgery. To isolate the impact of a PND on pre-operative morbidity and overcome limitations of previous studies we utilized a large clinical database to assess the effects of PND of CHD on pre-operative status.
Methods: Neonates (<30 days) undergoing heart surgery from 2010-2014 and recorded in the STS-CHSD were included. Multivariable logistic regression was used to evaluate association between PND and a composite measure including nine major preoperative risk factors. Covariates were included to adjust for important patient characteristics (e.g., weight-for-age z-score, genetic syndromes, prematurity), case complexity, and center effects. Centers and patients with excess missing data for relevant covariates were excluded.
Results: Included were 12,899 neonates from 112 centers. Major preoperative risk factors were present in 34% overall. By univariate analysis, PND was associated with a lower overall prevalence of major preoperative risk factors and a lower prevalence for 6 out of 9 of the individual risk factors (Table). After adjusting for potential confounders, preoperative risk factors were less prevalent among neonates with PND diagnosis compared to neonates without PND (adjusted OR = 0.62, 95% CI: 0.57-0.68, p <0.001). A sensitivity analysis excluding neonates with genetic syndromes, non-cardiac anatomic abnormalities and prematurity demonstrated similar findings (adjusted OR = 0.55, 95% CI: 0.49-0.61, p<0.0001).
Conclusions: Among neonates with CHD, a PND is associated with significantly lower rates of pre-operative risk factors for cardiac surgery. Further studies are needed to define the association of PND with longer term clinical outcomes.
Article Information
vol. 134 no. Suppl 1 A16892
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Michael Quartermain1;
- Kevin D Hill2;
- David J Goldberg3;
- Jeffery J Jacobs4;
- Marshall L Jacobs5;
- Sara K Pasquali6;
- George R Verghese7;
- Amelia Wallace8;
- Ross M Ungerleider9
- 1Pediatrics, The Children’s Hosp of Philadelphia, Philadelphia, PA
- 2Pediatrics, Duke Univ, Durham, NC
- 3Pediatrics, Children’s Hosp of Philadelphia, Philadelphia, PA
- 4Surgery, Johns Hopkins All Children’s Heart Institute, St Petersburg, FL
- 5Surgery, Johns Hopkins, Baltimore, MD
- 6Pediatrics, Univ of Michigan, Ann Arbor, MI
- 7Pediatrics, Ann & Robert H. Lurie Children’s Hosp of Chicago, Chicago, IL
- 8DCRI, Duke Clinical Rsch Institute, Durham, NC
- 9Surgery, Wake Forest Univ, Winston-Salem, NC
Abstract 17189: Indications and Adverse Effects of Statin Therapy in Children: A Retrospective Electronic Medical Record Review
Christopher Prendergast, Irene Predazzi, Laura Wiley, Jessica Lilley, Sara Van Driest, Sergio Fazio, Tracy McGregor
Circulation. 2016;134:A17189
Abstract
Introduction: Statins are the most commonly prescribed medications for primary and secondary prevention of coronary artery disease and stroke. Adverse drug reactions (ADRs) ranging from common myalgia to rhabdomyolysis with renal failure can occur. The indications for statin therapy and prevalence of statin ADRs in pediatrics have not been well described.
Hypothesis: Statin ADRs occur less commonly in pediatric patients than in adults.
Methods: Using electronic medical record (EMR) data, we abstracted charts of young subjects for whom statins were prescribed at Vanderbilt University Medical Center. We included 276 subjects with statin therapy initiated ≤21 years. Each record was reviewed manually for therapy indication, age at initiation, drug, dose(s), and reports of ADRs.
Results: The most common indication for statin prescription in children was hypercholesterolemia, followed by renal disease, type 1 diabetes, and heart transplant. Only 10/276 (3.6%) subjects reported ADR to statins leading to a therapeutic change, lower than the 10-25% estimates from observational studies in adults. No pediatric patients were identified with rhabdomyolysis.
Conclusions: ADRs during statin therapy in young patients are infrequent, mostly characterized by mild skeletal muscle symptoms, and rarely result in a change to statin therapy. The risk-to-benefit evaluation of using statin therapy in pediatrics with diverse indications appears favorable with regard to the incidence of skeletal muscle symptoms. However, our analysis does not address other concerns such as hormonal signaling in adolescent patients during times of rapid growth and pubertal development.
Article Information
vol. 134 no. Suppl 1 A17189
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Christopher Prendergast1;
- Irene Predazzi2;
- Laura Wiley3;
- Jessica Lilley4;
- Sara Van Driest5;
- Sergio Fazio2;
- Tracy McGregor6
- 1Pediatric Cardiology, Vanderbilt Univ, Nashville, TN
- 2Knight Cardiovascular Institute, Oregon Health and Sciences Univ, Portland, OR
- 3Biomedical Informatics, Vanderbilt Univ, Nashville, TN
- 4Pediatric Endocrinology, Univ of Mississippi, Jackson, MS
- 5Pediatrics, Vanderbilt Univ, Nashville, TN
- 6Div of Med Genetics and Genomic Medicine, Director Clinical Rsch at Alnylam Pharmaceuticals, Cambridge, MA
Abstract 13524: Examining Variation in Interstage Mortality Rates Across the National Pediatric Cardiology Quality Improvement Collaborative: Do Lower Mortality Centers Have Lower Risk Patients?
Katherine E Bates, Sara K Pasquali, David W Brown, Peter B Manning, Karen Uzark
Circulation. 2016;134:A13524
Abstract
Introduction: Although overall interstage mortality for infants with hypoplastic left heart syndrome has declined within the National Pediatric Cardiology Quality Improvement Collaborative (NPC-QIC), variation in outcomes across centers persists. It remains unclear whether centers with lower mortality rates have lower risk interstage patients or whether differences in the type of interstage care provided may explain this variation. We examined previously established patient risk factors across NPC-QIC centers with higher and lower interstage mortality rates.
Methods: Lower mortality NPC-QIC centers were defined as those with >25 consecutive interstage survivors, and included 7 centers. Higher mortality centers were defined as those with cumulative interstage mortality rates greater than the NPC-QIC historic baseline rate (>10%), and included 4 centers. Patient risk factors were compared between lower and higher mortality centers, accounting for within center clustering.
Results: The 7 lower mortality centers (n=331 patients) had a lower interstage mortality rate of 2.7% compared to 13.3% in the 4 higher mortality centers (n=173 patients); p<0.0001. Post-natal diagnosis was the only risk factor less prevalent in the lower mortality centers (Figure) compared to higher mortality centers (18.4% vs. 31.8%, p=0.04). All other risk factors examined were either similar between the lower and higher mortality centers (including gestational age, anatomic diagnoses, birth weight), or more prevalent in the lower mortality centers (major syndrome- 6.9% vs. 4.0%, p=0.03; major anomalies- 7.3% vs. 4%, p=0.047).
Conclusions: Differences in interstage mortality rates among NPC-QIC centers do not appear to be explained by a lower rate of patient risk factors in lower mortality centers. Further study is necessary to evaluate differences in interstage care practices across centers in order to identify targets for efforts to reduce variation and improve outcomes.
Article Information
vol. 134 no. Suppl 1 A13524
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Congenital Heart Cntr, Univ of Michigan, Ann Arbor, MI
- 2Dept of Cardiology, Boston Children’s Hosp, Boston, MA
- 3Div of Cardiothoracic Surgery, St. Louis Children’s Hosp, St. Louis, MO
Abstract 13178: A Novel, Data-Driven Approach to Classify Critical Left Ventricular Outflow Tract Obstruction Using Pre-Intervention Echocardiographic Measurements: A Report From The Congenital Heart Surgeons’ Society Data Center
James M Meza, Martijn Slieker, Luc Mertens, Eugene H Blackstone, Pirooz Eghtesady, Kamal Pourmoghadam, James K Kirklin, William M DeCampli, Marshall Jacobs, Tara Karamlou, Phillip T Burch, Mohsen Karimi, Jeffrey Pearl, Stephanie Fuller, Christopher Mascio, Brian W McCrindle
Circulation. 2016;134:A13178
Abstract
Objective: Critical left ventricular outflow tract obstruction (LVOTO) has been traditionally classified by aortic and mitral valvar pathology. We aimed to determine if baseline qualitative and quantitative echocardiographic measures alone could define new groups of patients with greater clinical relevance.
Methods: Pre-intervention transthoracic echocardiograms for 651 neonates with Critical LVOTO were interpreted by one pediatric cardiologist according to a standardized protocol. Cluster analysis, with 136 echocardiographic measures, was used to group the patients. Variables defining each group were identified by multinomial regression.
Results: Cluster analysis categorized the 651 neonates into groups of 215 (Group 1), 338 (Group 2), and 98 (Group 3) patients (Panel A). Aortic valve atresia and left ventricular (LV) end diastolic volume were identified as significant discriminating variables. LV size was largest in Group 3 and smallest in Group 2. Aortic atresia was most prevalent in Group 2 and least prevalent in Group 3. The distribution of these and other variables is shown in Panel B. Balloon valvotomy was the first intervention in 9% (19/215), 2% (6/338), and 61% (60/98) (p<0.0001). In those with an initial operation, single ventricle palliation was performed in 90% (176/215), 98% (326/338), and 58% (22/38) (p<0.0001). Overall mortality in each group was 27% (59/215), 41% (138/338), and 12% (12/98) (p<0.0001).
Conclusions: Using a completely data-driven approach, we identified three novel groups, primarily based on baseline LV size, that correlate with management strategy and overall mortality. These groups roughly correspond anatomically with multi-level LV hypoplasia, hypoplastic left heart syndrome, and critical aortic stenosis, respectively. Our analysis suggests that a more useful classification of critical LVOTO may require more detailed measurements, especially of LV size, than a simplistic scheme limited to valvar pathology.
Article Information
vol. 134 no. Suppl 1 A13178
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- James M Meza1;
- Martijn Slieker2;
- Luc Mertens3;
- Eugene H Blackstone4;
- Pirooz Eghtesady5;
- Kamal Pourmoghadam6;
- James K Kirklin7;
- William M DeCampli6;
- Marshall Jacobs8;
- Tara Karamlou9;
- Phillip T Burch10;
- Mohsen Karimi11;
- Jeffrey Pearl12;
- Stephanie Fuller13;
- Christopher Mascio13;
- Brian W McCrindle3
- 1Div of Cardiovascular Surgery, The Hosp for Sick Children, Toronto, Canada
- 2Dept of Pediatric Cardiology, Radboud Univ Med Cntr, Nijmegen, Netherlands
- 3Div of Pediatric Cardiology, The Hosp for Sick Children, Toronto, Canada
- 4Thoracic and Cardiovascular Surgery, Quantitative Health Sciences, The Cleveland Clinic, Cleveland, OH
- 5Section of Pediatric Cardiothoracic Surgery, St. Louis Children’s Hosp, St. Louis, MO
- 6Pediatric Cardiac Surgery, Arnold Palmer Hosp for Children, Orlando, FL
- 7Div of Cardiothoracic Surgery, Univ of Alabama at Birmingham, Birmingham, AL
- 8Div of Cardiac Surgery, Johns Hopkins Sch of Medicine, Baltimore, MD
- 9Pediatric Cardiothoracic Surgery, UCSF Benioff Children’s Hosp, San Francisco, CA
- 10Pediatric Cardiovascular & Thoracic Surgery, Primary Children’s Hosp, Salt Lake City, UT
- 11Cardiac Surgery, Yale-New Haven Children’s Hosp,, New Haven, CT
- 12Pediatric Cardiovascular Surgery, Phoenix Children’s Hosp, Phoenix, AZ
- 13Div of Cardiothoracic Surgery, Children’s Hosp of Philadelphia, Philadelphia, PA
Abstract 20098: Treprostinil Improves Right Ventricular Function in Pediatric Pulmonary Hypertension
Rachel K Hopper, Yan Wang, Valerie DeMatteo, Steven M Kawut, Okan Elci, Rachel Rogers, Laura Mercer-Rosa
Circulation. 2016;134:A20098
Abstract
Introduction: Pulmonary hypertension (PH) is associated with significant morbidity and mortality in children due to right ventricular (RV) failure. Prostacyclin analogs improve outcomes in adult pulmonary arterial hypertension (PAH), however studies of children are limited. We sought to determine the effect of treprostinil on RV function assessed by echocardiogram in children with various forms of PH.
Methods: We conducted a retrospective cohort study of children with PH treated with treprostinil between 1/2001 and 8/2015 at our center. We collected data from baseline, 1-3 months, and 6-12 months after drug initiation. Transthoracic echocardiograms were reviewed offline using a standardized research protocol that included tricuspid annular plane systolic excursion (TAPSE) and RV global longitudinal strain (%, with more negative values indicating better systolic function). Generalized linear/logistic mixed-effects regression models were used to examine changes over time.
Results: Forty-seven subjects were included; 64% were female, 55% were white, and 17% were black. Median age at PH diagnosis was 2.4 months (range: 0 to 21.2). Disease type was idiopathic PAH (38%), PAH associated with congenital heart disease (15%), developmental lung disease (45%), and chronic thromboembolic PH (2%). Subjects received intravenous (68%), subcutaneous (17%), or inhaled (15%) treprostinil. TAPSE and RV strain were reduced at baseline (table 1). Treprostinil was associated with significant improvement in TAPSE (adjusted for growth), qualitative RV function and RV global longitudinal strain. Treprostinil decreased BNP levels, improved functional class assessment and increased 6-minute walk distance (in children able to perform testing).
Conclusions: In children with PH, treprostinil is associated with an early and sustained improvement in RV function as well as clinical markers of PH severity. RV strain may be a sensitive marker of RV function in children with PH.
Article Information
vol. 134 no. Suppl 1 A20098
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Rachel K Hopper1;
- Yan Wang1;
- Valerie DeMatteo1;
- Steven M Kawut2;
- Okan Elci1;
- Rachel Rogers1;
- Laura Mercer-Rosa1
- 1Cardiology, The Children’s Hosp of Philadelphia, Philadelphia, PA
- 2Medicine and Epidemiology, Univ of Pennsylvania, Perelman Sch of Medicine, Philadelphia, PA
Abstract 20320: Late Gadolinium Enhancement at Interventricular Insertion Point Strongly Predicts Systolic and Diastolic Dysfunction of the Systemic Ventricle in Repaired Adult Patients With Complex Congenital Heart Disease
Yohsuke Hayama, Hideo Ohuchi, Jun Negishi, Kanae Noritake, Toru Iwasa, Aya Miyazaki, Etsuko Tsuda, Isao Shiraishi
Circulation. 2016;134:A20320
Abstract
Background: Late gadolinium enhancement (LGE) cardiovascular magnetic resonance (CMR) at interventricular insertion points can often be detected in patients with hypertrophic cardiomyopathy. Some adult patients with congenital heart disease (ACHD) would also show the findings. They were, however, thought to be non-specific, ubiquitous findings, and their clinical importance have not been well analyzed.
Methods: We studied 104 consecutive postoperative adult patients with complex congenital heart disease with biventricular physiology (18-67 years; mean age 32 years, including 55 patients with tetralogy of Fallot, 36 men). Ventricular short-axis images obtained by CMR presenting locations of LGE were analyzed. We calculated the signal-intensity ratio (SIR) of interventricular insertion points to the adjacent blood cavity and averaged them in series of slices. We also measured the end-diastolic, end-systolic ventricular volume and myocardial mass standardized by body surface area (EDVI, ESVI, Mass-I) and ejection fraction (EF) of the left and right ventricle (LV, RV) by CMR. We compared the SIR with clinical profiles, including hemodynamic parameters in cardiac catheterization (for example, end-diastolic ventricular pressure, EDP, pulmonary capillary wedge pressure, PCWP).
Results: Seventy-six patients (72%) had the LGE at interventricular insertion points, located at anterior, posterior or both side of septum in 8, 42 and 26 patients respectively. In univariate analysis, the SIR showed positive correlation with LVEDVI (r = 0.22, p = 0.029), LVESVI (r = 0.29, p = 0.004), LVEDP (r = 0.27, p = 0.010), PCWP (r = 0.24, p = 0.025), QRS duration (r = 0.22, p = 0.030), and negative correlation with LVEF (r = -0.24, p = 0.019). In multivariate analysis, LVESVI (p = 0.003), LVEDP (p = 0.011), QRS duration (p = 0.014), and cardiac index (p = 0.034) were independently correlated with the SIR.
Conclusion: In postoperative complex ACHD with biventricular physiology, the patients often show the LGE at interventricular insertion points. And their elevated signal intensity strongly predicts systolic and diastolic dysfunction of the systemic ventricle.
Article Information
vol. 134 no. Suppl 1 A20320
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Yohsuke Hayama;
- Hideo Ohuchi;
- Jun Negishi;
- Kanae Noritake;
- Toru Iwasa;
- Aya Miyazaki;
- Etsuko Tsuda;
- Isao Shiraishi
- Pediatric Cardiology, National Cerebral and Cardiovascular Cntr, Suita, Japan
Abstract 19399: Failure to Adequately Reduce Tricuspid Valve Size in Hypoplastic Left Heart Syndrome: Tricuspid Valve Repair is an Important Mechanism of Significant Post-Operative Regurgitation
Kandice Mah, Billie-Jean Martin, Silvia Alvarez, Nassiba Alami Laroussi, Ivan M Rebeyka, Jeffrey Smallhorn, Nee Khoo, Timothy Colen
Circulation. 2016;134:A19399
Abstract
Background: Tricuspid valve regurgitation (TR) is associated with morbidity and mortality in hypoplastic left heart syndrome (HLHS). Successful tricuspid valve repair (TVR) may improve outcomes, however 30-50% of patients develop significant post-operative TR, often requiring further surgery. We sought to determine pre-operative factors associated with development of TR after TVR in HLHS.
Methods: Twenty-six HLHS patients requiring TVR for TR between 2005 and 2015 were assessed. 2D echocardiography (2DE) was used pre-op and late post-op (> 6 months) to assess TR grade, vena contracta (VC) size and annulus size. Patients were divided into those with ≤ mild TR (group A) and those with ≥ moderate TR (group B) at late post-op. Pre-op 3D echocardiography (3DE) was used to assess mechanism and location of TR. Surgical notes were reviewed for repair details.
Results: Fourteen patients (54%) had ≤ mild TR (group A) and 12 (46%) had ≥ moderate TR (group B) at late post-op. TVR occurred most commonly with other surgical procedures (2 at Norwood, 8 at Glenn, and 7 at Fontan). On preop 3DE, 13 (52%) had central TR, 7 (28%) had central TR with extension into a commissure, 2 (8%) had anterior-septal TR, and 3 (12%) had mixed commissural TR. The primary mechanism was tethering in 14 (56%) and prolapse in 12 (44%). For surgical repair, 17 (65%) had posterior annuloplasty, 5 (19%) cleft closure, and 4 (16%) other. Types of surgical repair were similar between the 2 groups.
Group A had smaller pre-op 2DE TV annulus Z-score (3.4 vs 5.0, P=0.013) but no difference in pre-op 2DE VC diameter, when compared to group B. Group A pre and post op-comparison showed reduced annulus Z-score (3.4 vs 0.8, P=0.01) and VC diameter (p=0.01), while Group B pre and post op annulus size and VC size showed no reduction. There was no difference between group A and B with respect to TR location or primary mechanism involved. Late post-op VC demonstrated moderate correlation with pre-op TV annulus size (P=0.005; R=0.54) but not with pre-op VC.
Conclusion: TR after valve repair is common. Larger pre op annulus size is related to post-operative TR. Despite surgical repair aimed at reducing TV annulus size, failure to adequately reduce TV size appears to be a mechanism of persistent significant post-operative regurgitation in HLHS.
Article Information
vol. 134 no. Suppl 1 A19399
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Kandice Mah1;
- Billie-Jean Martin2;
- Silvia Alvarez1;
- Nassiba Alami Laroussi1;
- Ivan M Rebeyka2;
- Jeffrey Smallhorn1;
- Nee Khoo1;
- Timothy Colen1
- 1Div of Pediatric Cardiology, Stollery Childrens Hosp, Edmonton, Canada
- 2Dept of Surgery, Div of Cardiac Surgery, Univ of Alberta, Edmonton, Canada
Abstract 19349: Repaired Tetralogy of Fallot: End- Diastolic Pulmonary Artery Forward Flow Differences Defined by Multimodality Imaging
Shelby Kutty, Anne M Valente, Matthew T White, Kelsey Hickey, David A Danford, Andrew J Powell, Tal Geva
Circulation. 2016;134:A19349
Abstract
Background: The presence of pulmonary arterial end-diastolic forward flow (EDFF) in patients with repaired tetralogy of Fallot (TOF) is thought to indicate a non-compliant right ventricle. The purpose of our study was to investigate the associations of EDFF with echocardiogram (Echo) and cardiovascular magnetic resonance (CMR) indices of right and left heart function.
Hypothesis: EDFF is associated with reduced pulmonary regurgitation (PR) and right ventricular (RV) size.
Methods: We retrospectively analyzed 399 patients with repaired TOF who had Echo and CMR within 1 year of each other. EDFF was defined as the presence of forward flow on the main pulmonary artery or right ventricle-to-pulmonary artery conduit pulsed-wave Doppler Echo trace immediately following atrial contraction in at least 3 consecutive cardiac cycles. CMR measurements included comprehensive volumetric and flow indices of the right and left heart. Variables were summarized by presence or absence of EDFF, and differences compared. Logistic regression was used to assess the univariate associations. Multivariable associations with EDFF were investigated and a forward-selection model building procedure was implemented to identify the most parsimonious model.
Results: The median age at TOF repair was 0.7 years (0.1-45), patient age was 18.1 years (0.8-72) and interval between Echo and CMR was 48 days (0-364). Diagnoses consisted of TOF/pulmonary stenosis (73%), TOF/pulmonary atresia (24%), and TOF/atrioventricular canal (3%). EDFF was identified in 122 (31%) patients. Compared with those without EDFF, patients with EDFF were younger (p=0.04); had a larger PR fraction (p<0.0001); and higher RV end-diastolic volume, (p=0.02) stroke volume (p<0.0001) and ejection fraction (p=0.009). There was no significant difference in the right atrial or left ventricular Echo and CMR indices between the 2 groups. On multivariable regression analysis, EDFF was independently associated with a larger RV stroke volume (p<0.0001), and a smaller left ventricular end-diastolic volume (p=0.001).
Conclusion: In this large cohort of repaired TOF patients, multimodality noninvasive imaging findings suggest mechanisms beyond right ventricular noncompliance may be responsible for presence of EDFF.
Article Information
vol. 134 no. Suppl 1 A19349
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Shelby Kutty1;
- Anne M Valente2;
- Matthew T White3;
- Kelsey Hickey3;
- David A Danford1;
- Andrew J Powell3;
- Tal Geva3
- 1DIVISION OF PEDIATRIC CARDIOLOGY, Univ of Nebraska College of Medicine, Omaha, NE
- 2Dept of Cardiology and Pediatrics, Children’s Hosp Boston and Harvard Med Sch, Boston, Boston, MA
- 3DIVISION OF PEDIATRIC CARDIOLOGY and Dept of Pediatrics, Children’s Hosp Boston and Harvard Med Sch, Boston, MA
Abstract 19055: Myocardial Deformation Analysis Reveals Early Cardiac Abnormalities in Patients With Hutchinson Gilford Progeria Syndrome
Fatima I Lunze, Tor Biering-Sørensen, Sheila M Hegde, Steven D Colan, Leslie Smoot, Leslie Gordon, Monica Kleinman, Mark Kieran, Ashwin Prakash
Circulation. 2016;134:A19055
Abstract
Background: Patients with Hutchinson-Gilford Progeria Syndrome (HGPS) demonstrate accelerated aging with premature cardiovascular morbidity and mortality. While left ventricular ejection fraction (LVEF) has been shown to be normal in the absence of significant valve disease, global and regional myocardial deformation has not been previously examined in this population. We used myocardial deformation imaging to evaluate regional ventricular function in patients with HGPS.
Methods: Transthoracic echocardiography with 2-D speckle tracking was used to prospectively evaluate 56 patients with HGPS at a median age of 10.3 (2.2-19.8) years in comparison with 32 age-matched controls. Left ventricular (LV) longitudinal, circumferential and radial strain and, right ventricular (RV) longitudinal strain were calculated using standard techniques.
Results: Despite a normal LVEF (67±5%), HGPS patients showed lower LV global longitudinal and radial strain compared to controls, while global circumferential strain was preserved (Table). Abnormal LV longitudinal strain was confined to the lateral LV free wall with preserved septal deformation. Within the LV, the mid-septal and mid-lateral segments showed the most prominent abnormalities. Right ventricular global longitudinal strain was also lower in patients compared to controls.
Conclusions: In this largest-to-date cohort of HGPS patients, we found abnormalities in LV and RV deformation compared to controls, despite a normal LVEF. We also found a unique pattern of regional variation in LV deformation. Further research is warranted to evaluate the relationship of these abnormalities to clinical outcomes and to determine if deformation parameters can be useful endpoints in clinical trials in this patient population.
Article Information
vol. 134 no. Suppl 1 A19055
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Fatima I Lunze1;
- Tor Biering-Sørensen2;
- Sheila M Hegde2;
- Steven D Colan1;
- Leslie Smoot1;
- Leslie Gordon1;
- Monica Kleinman1;
- Mark Kieran1;
- Ashwin Prakash1
- 1Dept of Cardiology, Boston Children’s Hosp, Boston, MA
- 2Dept of Medicine, Cardiovascular Div, Brigham and Women’s Hosp, Boston, MA
Abstract 18738: Using 3D Printing With Virtual Surgery to Identify Residual Transverse Arch Obstruction in Coarctation Correction
Kevin K Whitehead, Kevin A Gralewski, Yoav Dori
Circulation. 2016;134:A18738
Abstract
Introduction: Transverse arch (tArch) hypoplasia often accompanies coarctation of the aorta (CoA), causing residual arch obstruction after repair. We propose a novel technique for surgical planning using 3D printing and a pulsatile flow phantom in patients with tArch hypoplasia, in order to preoperatively assess the potential correction and quantify residual tArch obstruction.
Methods: Rendered aortic volumes were created by segmentation of two CoA patients with tArch hypoplasia using Mimics and edited in 3-matic (Materialise, Leuven, Belgium). The CoA was virtually repaired but the tArch was not repaired. A rigid-walled 3D model was printed and connected to an MRI-compatible pump programmed to match the patients’ aortic waveform delivered flow of a 40% glycerin-aqueous solution. Descending aorta (dAo) flow was tuned to match the patient-measured inferior vena cava flow. 4D flow MRI sequences were acquired and time-elapse flow pathlines were calculated. Pressures were measured in the ascending aorta, just distal to the tArch, and dAo.
Results: Flow patterns revealed acceleration in the tArch and dAo of both phantoms. Peak tArch velocities were measured to be 2.5 and 3.5 m/s in the mild and moderate hypoplasia (figure) cases, respectively with significant flow skewing in both cases. Pressure gradients were less than 5 mmHg for the mild case and significant (39 mmHg) for the moderate case with some pressure recovery in the dAo (25 mmHg) in the moderate case.
Conclusion: We demonstrate a method using 3D printing to investigate the potential results of a CoA repair in the setting of tArch hypoplasia. Further study is needed to determine the predictive quality of these results.
Article Information
vol. 134 no. Suppl 1 A18738
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Kevin K Whitehead;
- Kevin A Gralewski;
- Yoav Dori
- Pediatrics, Cardiology, Childrens Hosp of Philadelphia, Philadelphia, PA
Abstract 18843: Evaluating Appropriate Use of Pediatric Echocardiogram for Chest Pain in Outpatient Clinics
Reid Chamberlain, Jonathan Pelletier, Sarah Blanchard, Christoph P Hornik, Kevin Hill, Michael J Campbell
Circulation. 2016;134:A18843
Abstract
Introduction: Echocardiography is often used in the evaluation of pediatric chest pain but incidence of uncovered cardiac pathology is low. In 2014, the American College of Cardiology published appropriate use criteria (AUC) for echocardiography in evaluating pediatric chest pain. We sought to evaluate the frequency, diagnostic yield and cost associated with echoes meeting “Rarely Appropriate” criteria.
Methods: Retrospective, single-institution study of all patients 18 years or less with an initial evaluation for chest pain by a pediatric cardiologist (2014-2015). We categorized patients by echo appropriateness based on the AUC. We used multivariable logistic regression to determine factors associated with use of a “Rarely Appropriate” echo. Excess cost was calculated by direct cost estimates for studies and follow-up visits associated with a “Rarely Appropriate” echo.
Results: The cohort included 539 patients, median age 13 years (range 3-18) and 51% female. Retrospective application of the AUC and patient outcomes are summarized in the Figure. Echoes were performed in 71% (380/539) of patients overall and in 36% (60/167) of patients meeting “Rarely Appropriate” criteria. Abnormal echo findings were present in 5% (19/380) and incidental findings in 3% (10/380) overall. There were no abnormal findings (0/60) in the “Rarely Appropriate” subgroup. Provider use of echo in “Rarely Appropriate” patients varied widely from 0-75% across 15 providers (p=0.004). In multivariable analysis, controlling for provider ordering practice by fixed-effect regression, there was no significant association between race, ethnicity, age, sex, or payer status and performance of a “Rarely Appropriate” echo. “Rarely Appropriate” echoes resulted in $280,200 in excess costs ($4,670/patient).
Conclusions: Echo use in patients meeting “Rarely Appropriate” criteria is of little diagnostic utility and contributes to additional cost to the patient and healthcare system.
Article Information
vol. 134 no. Suppl 1 A18843
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Reid Chamberlain1;
- Jonathan Pelletier2;
- Sarah Blanchard2;
- Christoph P Hornik1;
- Kevin Hill1;
- Michael J Campbell1
- 1Pediatric Cardiology, Duke Univ, Durham, NC
- 2Pediatrics, Duke Univ, Durham, NC
Abstract 17989: Early Tricuspid Regurgitation in Hypoplastic Left Heart Syndrome is Not Related to Right Ventricular Function or Mechanical Dyssynchrony
Silvia Alvarez, Nee Khoo, Kandice Mah, Nassiba Alami Laroussi, Edythe Tham, Shelby Kutty, Jeffrey Smallhorn, Timothy Colen
Circulation. 2016;134:A17989
Abstract
Background: Tricuspid regurgitation (TR) is associated with morbidity and mortality in hypoplastic left heart syndrome (HLHS). We have previously demonstrated that TR prior to stage 2 (S2) surgical palliation is related to tricuspid valve (TV) abnormalities, including dilated annulus and increased leaflet prolapse. Right ventricular (RV) dysfunction and mechanical dyssynchrony have been reported as causes for TR. Thus, we hypothesized that TR and abnormal TV parameters are associated with RV dysfunction. This study explored the relationship between TV and RV function using quantitative three dimensional echocardiography (3DE) measure of TV parameters and speckle tracking echocardiography (STE) of RV deformation, in HLHS with and without TR.
Methods and Results: Forty-four HLHS patients with median age of 4.7 months (IQR 3.9-5.3) were prospectively recruited prior to S2 palliation. TV parameters assessed using 3DE, included vena contracta area (VCA), leaflet area, prolapse volume, tethering volume, annular bending angle and papillary muscle angle. RV systolic function was assessed by fractional area change and STE derived longitudinal and circumferential strain, strain rate and mechanical dyssynchrony index (MDI). The group was divided into those with (group A) and those without (group B) significant TR by qualitative assessment. RV functional parameters were compared between the two groups using Mann-Whitney signed rank test and Spearman correlation of TV leaflet and annulus area, prolapse and tethering volume, bending angle and VCA, to longitudinal and circumferential strain, strain rate and MDI were performed. Fourteen patients (32%) had moderate or greater TR (group A). RV function parameters were not different between group A and group B. There was no correlation between all 3DE TV parameters and STE RV deformation parameters.
Conclusion: Contrary to our hypothesis, HLHS RV systolic dysfunction and mechanical dyssynchrony do not play a significant role in early TR. This finding suggests the mechanisms of early TR in HLHS are likely to be secondary to valve and leaflet differences.
Article Information
vol. 134 no. Suppl 1 A17989
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Silvia Alvarez1;
- Nee Khoo1;
- Kandice Mah1;
- Nassiba Alami Laroussi1;
- Edythe Tham1;
- Shelby Kutty2;
- Jeffrey Smallhorn1;
- Timothy Colen1
- 1Div of Pediatric Cardiology, Stollery Children’s Hosp, Edmonton, Canada
- 2Joint Div of Pediatric Cardiology, Children’s Hosp and Med Cntr, Univ of Nebraska/Creighton Univ, Omaha, NE
Abstract 15254: Echocardiographic Variables Immediately Post Right Ventricular Decompression Predict Right Ventricular Growth and Biventricular Circulation in Patients With Pulmonary Atresia Intact Ventricular Septum
Shiraz A Maskatia, Curtis D Tavers, David J Goldberg, Lindsay S Rogers, Andrew C Glatz, Athar M Qureshi, Bryan H Goldstein, Christopher J Petit, Jingning Ao, Ritu Sachdeva
Circulation. 2016;134:A15254
Abstract
Background: Neonates with pulmonary atresia-intact ventricular septum (PA-IVS) who undergo right ventricular (RV) decompression ultimately have two-ventricle (2V) or <2V circulation depending on RV size. We sought to determine the relation between post-decompression echocardiographic parameters, RV growth and 2V circulation.
Methods: Neonates undergoing RV decompression for PA-IVS from 2005-2015 at the 4 member centers of the Congenital Catheterization Research Collaborative were included. Echocardiograms at baseline, first post-decompression, and follow up closest to 1 year post decompression were analyzed. The primary outcomes were RV growth by echocardiogram and 2V circulation.
Results: Of the 81 patients in the study, 11 (14%) had <2V circulation, and 54 (67%) had follow up echocardiograms available. After decompression, tricuspid regurgitation (TR) and RV function improved (Table 1). Post-decompression ≥moderate TR and higher pulmonary valve antegrade velocity were associated with 2V circulation (Table 2). Baseline tricuspid valve z score correlated with larger increase in RV area/BSA (R=0.42, p = 0.005). Patients with ≥moderate TR post decompression had an increase in RV area of 22.3 (7.6-29.7) cc/m2vs 14.3 (6.8-19.3) cc/m2 in those with ≤mild TR (p = 0.049). Those with bidirectional flow at the ASD post-decompression had an increase in RV area of 24.2(14.3-26.6) cc/m2 vs 9.8 (6.8-15.5) cc/m2 in those with right to left flow (p=0.007).
Conclusions: Post-decompression tricuspid regurgitation severity and bidirectional ASD flow post-decompression appear to be associated with RV growth and 2V circulation in patients with PA-IVS following RV decompression
Article Information
vol. 134 no. Suppl 1 A15254
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Shiraz A Maskatia1;
- Curtis D Tavers2;
- David J Goldberg3;
- Lindsay S Rogers4;
- Andrew C Glatz3;
- Athar M Qureshi5;
- Bryan H Goldstein4;
- Christopher J Petit6;
- Jingning Ao2;
- Ritu Sachdeva6
- 1Pediatric Cardiology, Stanford Univ Med Sch, Palo Alto, CA
- 2Pediatrics, Emory Univ Sch of Medicine, Atlanta, GA
- 3Pediatric Cardiology, Univ of Pennsylvania Sch of Medicine, Philadelphia, PA
- 4The Heart Cntr, Cincinnati Children’s Hosp Med Cntr, Cincinnati, OH
- 5Pediatric Cardiology, Baylor College of Medicine, Houston, TX
- 6Pediatric Cardiology, Emory Univ Sch of Medicine, Atlanta, GA
Abstract 14906: The Effect of Shunt Type on Non-invasive Pressure-Volume Loop Measures of Cardiac Mechanics After Stage 2 Palliation: Insights From the Pediatric Heart Network Single Ventricle Reconstruction Trial Public Use Dataset
Shahryar M Chowdhury, Andrew M Atz, Carolyn L Taylor, Sinai C Zyblewski, Scott M Bradley, Minoo N Kavarana, Eric M Graham
Circulation. 2016;134:A14906
Abstract
Introduction: The early survival benefit of the RV to pulmonary artery shunt (RVPAs) over the modified Blalock-Taussig shunt (mBTs) dissipates over time in children with single RV after the Norwood procedure. The objective of this study was to determine if single beat non-invasive pressure-volume loop measures of cardiac mechanics can provide insight into the mechanisms behind these findings.
Methods: Core-lab echocardiogram measures prior to superior cavopulmonary connection (SCPC) and post-operatively at 14 months of age were obtained from the publically available Pediatric Heart Network Single Ventricle Reconstruction trial database. End-systolic elastance (Ees), a measure of contractility, was calculated as (0.9 * SBP/end-systolic volume). Arterial elastance (Ea), a measure of afterload, was calculated as (0.9 * SBP/stroke volume). Ventriculo-arterial coupling was expressed as the ratio of Ea/Ees. Ees and Ea were indexed to BSA. Only patients with paired ventricular volume data pre-SCPC and at 14 months were included in the analysis.
Results: Data from 185 patients were analyzed. Differences between patients with RVPAs vs. mBTs prior to SCPC and at 14 months are reported in the table. There was a greater increase in median Ees (25.5% vs. -4.1%, p < 0.01) and Ea (27.3% vs. 2.2%, p < 0.01) in the mBTs group compared to RVPAs after SCPC. There was no difference in change in Ea/Ees between shunt groups, p = 0.31.
Conclusion: Patients in the RVPAs group displayed greater contractility compared to mBTs patients prior to SCPC. However, at 14 months, there is a trend toward greater contractility in the mBTs group. This was contributed to by a lack of improvement in contractility in the RVPAs group compared to the large increase in contractility in the mBTs group after SCPC. Investigation of the relationship between these changes in contractility and the differences in mid- and long-term mortality between shunt groups is warranted.
Article Information
vol. 134 no. Suppl 1 A14906
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Shahryar M Chowdhury;
- Andrew M Atz;
- Carolyn L Taylor;
- Sinai C Zyblewski;
- Scott M Bradley;
- Minoo N Kavarana;
- Eric M Graham
- Pediatrics, Med Univ of South Carolina, Charleston, SC
Abstract 14546: Aortic Stiffness and Its Relationship to Exercise and Ventricular Volumes After Surgical Reconstruction in Single Ventricle Patients Using Real Time Exercise Cardiac Magnetic Resonance
Mark A Fogel, Esther Kim, Marc Keller, Matthew Harris, Kevin Whitehead, phillip Trusty, Mike Tree, Alan Wei, Ajit Yoganathan
Circulation. 2016;134:A14546
Abstract
Introduction: Aortic reconstruction (recon) in single ventricle (SV) pts create a stiff large vessel which may adversely impact SV afterload & exercise performance.
Hypothesis: SV pts with recon demonstrate evidence of increased afterload & aortic stiffness correlates with exercise performance.
Methods: SV pts after Fontan were studied with real time exercise CMR & metabolic exercise stress test. Aortic pulse wave velocity (PWV) & distensibility (Dis) of the descending aorta at the level of the diaphragm (DAo) were recorded. Significance was P<0.05.
Results: 18 pts who underwent recon & 30 did not (age median [range] 17.4 [12-42] and 17.0 [12.7-25.6] yrs respectively, P=0.33). PWV was greater in recon than in non-recon (median [range] 4.4 [2.3-9.8] vs 3.6 [2.6-6.3] m/s respectively, P=0.006). Significant inverse correlations in recon were found between PWV and end-diastolic, end-systolic and stroke volumes both at rest and at exercise, presumably because of increased afterload (table). Significant inverse correlations also existed in recon between Dis and exercise parameters such as peak O2 pulse (R=0.56, P=0.02), peak oxygen consumption (R=0.63, P=0.008), oxygen consumption at ventillatory anaerobic threshold (R=0.48, P=0.04) and peak work (R=0.54, P=0.02). See graph. Similar correlations were not seen in those with normal aortas.
Conclusion: SV pts with recon demonstrate increased aortic stiffness, increasing afterload on the ventricle & decreasing ventricular volumes including stroke volume at rest & during exercise. At the same time, native DAo stiffness distal to the reconstruction is inversely correlated with exercise performance, presumably to decrease impedance mismatch, maintaining homogeneity of aortic wall compliance & thus not allowing for wasted energy dissipation. This information suggests SV with recon may be at higher risk for heart failure & may be useful in designing better aortic reconstructions to maximize exercise performance.
Article Information
vol. 134 no. Suppl 1 A14546
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- Mark A Fogel1;
- Esther Kim1;
- Marc Keller1;
- Matthew Harris1;
- Kevin Whitehead1;
- phillip Trusty2;
- Mike Tree3;
- Alan Wei3;
- Ajit Yoganathan2
- 1PEDIATRIC CARDIOLOGY, Childrens Hosp Philadelphia, Philadelphia, PA
- 2Bioengineering, GA Institute of Technology, Atlanta, GA
- 3Bioengineering, GA Tech, Atlanta, GA
Abstract 12945: A Novel Index for Quantification of Interventricular Septal Flattening in Pediatric Patients With Right Ventricular Hypertension
Konstantin Averin, Erik Michelfelder, Lindsay Urbinelli, Russel Hirsch
Circulation. 2016;134:A12945
Abstract
Introduction: Systolic flattening of the inter-ventricular septum (IVS) is a marker of elevated right ventricular pressure (RVp). It can be non-invasively quantified by a left ventricular eccentricity index (LVEI), RV to left ventricular (LV) ratio and a novel index – the systolic flattening angle (SFA). Data evaluating the relationship between these indices and invasive RVp in pediatrics are limited.
Methods: Patients referred for right and left heart cardiac catheterizations (CC) were enrolled and underwent echocardiograms after induction of anesthesia. The SFA, RV:LV ratio and LVEI were measured in end-systole. Peak systolic RVp and aortic pressure (pAo) were measured simultaneously during CC. The likelihood of SFA to predict an RVp:pAo ratio of > 0.5 was assessed using receiver-operator curve (ROC) analysis. Bland-Altman plots were used to assess inter-observer agreement.
Results: Forty-one unique subjects were enrolled [56% female, median age 2.7 years (0.7, 7.1) and median weight 12.1kg (6.0, 22.3)]. The median mid-ventricular (MV), apical, and sub-costal LVEI was 1.18 (0.9, 1.7), 1.18 (1.0, 1.7), and 1.13 (1.0, 1.5), respectively. The mean SFA was 8.5±9.6°, the median RV:LV ratio was 0.71 (0.46, 1.23), and the mean RVp:pAo ratio was 0.68 ± 0.5. There was a significant negative correlation (r = -0.75, p <0.001) between SFA and RVp:pAo ratio and a modest correlation with other non-invasive indices (Figure). ROC analysis demonstrated an area under the curve = 0.90 for prediction of RVp:pAo > 0.50 by SFA. An SFA < 10.6 had a sensitivity of 88% and specificity of 79% in predicting RVp:pAo > 0.50. SFA was modestly reproducible with a Bland-Altman plot demonstrating a bias of 4.14 and limits of agreement of -7.8 and 16.1.
Conclusions: SFA has the best correlation with RVp:pAO, good sensitivity and specificity, but relatively high inter-observer variability. Taken together, these non-invasive measures may help minimize the need for invasive assessment of RVp.
Article Information
vol. 134 no. Suppl 1 A12945
Published By:
American Heart Association, Inc.
Online ISSN:
History:
- Originally published November 11, 2016.
Copyright & Usage:
© 2016 by American Heart Association, Inc.
Author Information
- 1Cardiology, Cincinnati Children’s Hosp Med Cntr, Cincinnati, OH
- 2Sibley Heart Cntr, Children’s Healthcare of Atlanta, Atlanta, GA